Abstract
The aim of this study was to characterize the systemic cytokine signature of critically ill COVID-19 patients in a high mortality setting aiming to identify biomarkers of severity, and to explore their associations with viral loads and clinical characteristics. We studied two COVID-19 critically ill patient cohorts from a referral centre located in Central Europe. The cohorts were recruited during the pre-alpha/alpha (November 2020 to April 2021) and delta (end of 2021) period respectively. We determined both the serum and bronchoalveolar SARS-CoV-2 viral load and identified the variant of concern (VoC) involved. Using a cytokine multiplex assay, we quantified systemic cytokine concentrations and analyzed their relationship with clinical findings, routine laboratory workup and pulmonary function data obtained during the ICU stay. Patients who did not survive had a significantly higher systemic and pulmonary viral load. Patients infected with the pre-alpha VoC showed a significantly lower viral load in comparison to those infected with the alpha- and delta-variants. Levels of systemic CTACK, M-CSF and IL-18 were significantly higher in non-survivors in comparison to survivors. CTACK correlated directly with APACHE II scores. We observed differences in lung compliance and the association between cytokine levels and pulmonary function, dependent on the VoC identified. An intra-cytokine analysis revealed a loss of correlation in the non-survival group in comparison to survivors in both cohorts. Critically ill COVID-19 patients exhibited a distinct systemic cytokine profile based on their survival outcomes. CTACK, M-CSF and IL-18 were identified as mortality-associated analytes independently of the VoC involved. The Intra-cytokine correlation analysis suggested the potential role of a dysregulated systemic network of inflammatory mediators in severe COVID-19 mortality.
Similar content being viewed by others
Introduction
COVID-19 is an infectious disease caused by the severe acute respiratory syndrome virus 2 (SARS-CoV-2). Although respiratory failure is the most prominent feature associated with severe COVID-191, it has been demonstrated that systemic hyperinflammation also contributes to negative outcomes, and a distinct immune profile has been reported2,3,4. Several cytokines associated with unfavorable prognosis have been detected5,6,7,8,9,10, and specific anti-cytokine therapies have proven beneficial in severe COVID-1911,12. Despite these advances, cytokine identification as biomarkers has not been consistent across studies, possibly due to differences in population characteristics, detection assays and the time of sampling13. This last factor may be critical as most of the reports analyze samples retrieved at the time of hospital admission6,8,9,14,15, and they do not offer a direct insight into the immune activation landscape of critically ill patients. Moreover, hospital admission criteria are not uniform and depend on healthcare availability and local guidelines. Importantly, the majority of studies focused on relatively healthy cohorts that include non-critically ill patients with low mortality rates and have relied on clinical evaluation to classify for severity and outcomes. In order to develop adequate prognostic tools and/or target candidates, well-defined homogenous cohorts with clear classification endpoints are important.
For this report, we had access to critically ill COVID-19 patient cohorts with a high mortality outcome at two different stages during the pandemic, from a third-level referral center for COVID-19 patients in Croatia. Patient recruitment for the first cohort took place during the period when pre-alpha and alpha SARS-CoV-2 variants of concern (VoC) were dominant and will be referred to as the pre-delta cohort. The second cohort was recruited during the SARS-CoV-2 delta VoC wave in late 2021 and will subsequently be referred to as the delta cohort. From both cohorts, we analyzed serum and bronchoalveolar samples collected at admission to the intensive care unit (ICU) and during their hospitalization. This population was mainly composed of severely ill and/or rapidly deteriorating patients undergoing invasive mechanical ventilation (IMV) with a 30-day post-admission mortality of 70.9% and 72.7% for the pre-delta and the delta cohort respectively. We analyzed the systemic cytokine levels across time, detecting a systemic immune signature associated with higher disease severity and a fatal outcome. Associations with SARS-CoV-2 viral load and clinical characteristics were also investigated, suggesting an early dysregulated immune profile present at ICU admission in non-survivors compared to survivors.
Material and methods
Study participants
The study population included two cohorts. The first cohort (pre-delta cohort) included 54 patients admitted to the COVID-19 Intensive Care Unit (ICU) of the Clinical Hospital Center Rijeka with the diagnosis of acute respiratory distress syndrome (ARDS) defined by the Berlin criteria16 and severe COVID-19 (established by clinical assessment17 and initial viral detection by nasopharyngeal testing) from November 2020 to April 2021. These patients required invasive ventilator support, and ICU specialists followed standardized treatment guidelines. A non-ICU group of eighteen patients (hospitalized oxygen-dependent SARS-CoV-2 positive patients who did not require invasive respiratory support) was included as a control. A second cohort of 33 patients (delta cohort) was used to validate the findings obtained from the first cohort. Patients from the delta cohort were admitted to the ICU between November and December of 2021. The treatment guidelines were maintained across the two cohorts, in which all patients received steroid treatment (methylprednisolone or dexamethasone) in accordance with international guidelines. A more detailed description of the patient cohort was provided in our previous publication18. No power analysis was done due to a lack of reported effect size under matching or similar conditions of high mortality. Sample size was based on patient availability and sample collection was maintained during COVID-19 pandemic waves.
To provide a comparison to critically-ill patients without SARS-CoV-2 infection, serum samples from patients with non-COVID pneumonia and severe sepsis or septic shock were obtained from the randomized controlled trials SISPCT and MAXSEP19,20 of the SepNet Critical Care Trials Group. Patients were selected based on age, comorbidities, and stage of critical illness, to be comparable to COVID-19 cohorts. Serum samples obtained on the day of the start of invasive ventilator support were analyzed and patients were classified according to their 28-day post-admission mortality.
Clinical data and outcomes
Clinical characteristics of the patients from the pre-delta cohort are listed in and in a previous report Ynga-Durand et al.18. Characteristics of the delta cohort and the non-COVID cohort are listed in Table S1 and Table S2, respectively.
Clinical data were obtained from electronic medical records. Rijeka Hospital Medical constituted a highly specialized referral centre for severe COVID-19 cases in Primorsko-goranska, Licko-senjska and Istarska counties in Croatia, and close follow-up of individuals using the hospital information system (IBIS) or via phone calls was maintained up to 60 days. No variables with missing data were included in this study, except for days since symptom onset and lung imaging data.
Samples collection
Serum samples
Serum samples were obtained within the first 36 h after intubation and every two to three days until the 10th day of ICU stay (unless earlier ICU discharge or death occurred). Whole blood samples were transported to the Center for Proteomics of the University of Rijeka for initial processing. Samples were incubated for 30–60 min at room temperature until a blood clot was visible. Serum and blood clot were separated and the serum was centrifuged at 1500 g for 10 min. The supernatant was aliquoted and stored at − 20 °C. The samples were shipped on dry ice to the Helmholtz Center for Infection Research in Braunschweig and stored at −80 °C until analysis.
Bronchoalveolar lavage (BAL) samples
BAL samples were taken at the same time points as the serum samples. 10 mL of sterile saline was instilled in the main right bronchus through the endotracheal tube (ET). The fluid was aspirated until at least 5 mL of aspirate was collected. Afterwards, the samples were initially processed in the Center for Proteomics of the University of Rijeka by filtration through a 100 µm cell strainer and centrifugation at 400 g at 4 °C for 7 min to remove debris and mucous strands. The supernatant was aliquoted and stored at – 80 °C and shipped to the Helmholtz Center for Infection Research in Braunschweig on dry ice.
Quantification of serum cytokines
Serum samples were pre-processed by centrifugation at 800 g and 4 °C for 7 min. Serum proteins were measured using the Bio-Plex Pro™ Human Cytokine Screening Panel, 48-Plex (Bio-Rad, Hercules, USA, 10,000,092,045) following manufacturer’s instructions. The assay was performed using the Bio-Plex 200 system and analyzed with the Bio-Plex Manager™ version 6.2 software (Bio-Rad, Hercules, USA). Measurements below detection limit were set to the lowest standard value, values above detection limit were set to the highest standard concentration. Cytokines that showed levels below detection limit in more than 50% of measured samples were not included in the statistical analysis.
Isolation and quantification of viral RNA from serum and BAL samples
RNA was isolated and quantified as previously described18. In brief, RNA was isolated from 200 µl of serum or BAL using the Innuprep Virus DNA/RNA virus kit (Analytic Jena, Germany 845-KS-4710250). SARS-CoV-2 nucleocapsid protein N2 and the host housekeeping gene RNase P were quantified by reverse-transcriptase quantitative PCR (RT-qPCR) using the TaqPath™ 1-Step RT-qPCR Master Mix (ThermoFisher, Cat A15300). 5 µl of isolated RNA and serially diluted SARS-CoV-2 plasmid controls were used for RNA quantification (Integrated DNA Technologies, Cat # 10,006,625). Viral copy number calculation was performed by OneStep qPCR Software (Thermo Fisher Scientific, Waltham, MA, USA).
SARS-CoV-2 variants were identified using the GSD NovaType II (for pre-delta cohort) and IV (for delta cohort) SARS-CoV-2 RT-PCR assays (PCOV6083T, PCOV6191T, Gold Standard Diagnostics Europe, Dietzenbach, Germany). These assays allow the simultaneous measurement of the mutations K417N, E484K and N501Y or K417N, E484K and L452R in the spike gene. The assay was performed by following the manufacturer’s instructions and using the Light Cycler® 480 (Roche, Basel, Switzerland). Two patients from the pre-delta and one patient from the delta cohort were considered inconclusive due to low viral load.
Statistical analysis
The Shapiro–Wilk test was used to determine normality. Kruskal–Wallis test with Dunn’s correction or unpaired Mann–Whitney test was used for group comparisons where appropriate. Spearman’s rank or Pearson correlation test was used for correlation analysis where appropriate. Data representation was performed using R software v 4.1.2 using the packages heatmaply21, corrplot22, complexHeatmap23, pheatmap24 and upsetR25, and GraphPad Prism v 9.3.0 (GraphPad Software, San Diego, California USA).
Ethics approval
The study protocol was approved by the Institutional Review Board of the Rijeka Clinical Hospital Center (2170-29-02/1-20-2). Written informed consent was waived by the Ethics Committee of the Rijeka Clinical Hospital Center, as all procedures associated to sample collection were part of ICU routine care according to institutional guidelines and the study was performed in a retrospective manner.
Results
Demographic and clinical characteristics of the study population
For the pre-delta cohort, fifty-four patients with severe COVID-19 and ARDS requiring invasive mechanical ventilation, and eighteen hospitalized non-ICU patients requiring supplemental oxygen (but no mechanical ventilation) were included. A summary of the clinical characteristics of the ICU (classified by 30-day post admission survival outcome) and non-ICU population is shown (Table 1). The ICU non-survivor group was significantly older than the ICU survivor group and had a higher ICU severity score at admission (SOFA and APACHE II). Additionally, all non-survivors and 75% of survivors presented with moderate to severe ARDS at their admission to ICU. No significant differences were observed in the occurrence of comorbidities or days on invasive mechanical ventilation.
Detailed demographic data of the delta cohort is listed in Table S1. A comparison of the pre-delta cohort to the delta cohort showed similar characteristics, except for the days under mechanical ventilator support (Table 2). Importantly, none of the pre-delta and only three of the delta (one survivor, two non-survivors) patients had started their vaccinations against SARS-CoV-2. Due to the small number of cases, we have not examined vaccination effects.
Comparison of viral load of pre-alpha, alpha and delta VoC infected patients
We confirmed the VoC identity for the pre-delta cohort and delta cohort samples by variant analysis except for one sample. We measured serum and BAL viral loads of both cohorts at ICU admission (earliest sample available) and during ICU stay. We found that patients from the delta cohort who did not survive had a higher serum and BAL viral load at ICU admission (“earliest”) (Fig. S1a), similar to our previous dataset limited to the pre-delta cohort18 after age-adjustment. We compared BAL and serum viral loads from the earliest sample harvested after ICU admission, and the highest load measured during ICU stay to identify if viral replication was different among detected VoCs. The viral load in pre-alpha VoC infected patients was significantly lower than in alpha infected patients, except for earliest serum measurements. The viral load in delta patients did not significantly differ from either, except in the highest measured burden in BAL which was significantly higher than pre-alpha VoC (Fig. S1b).
Serum cytokine concentration at ICU admission reveals a spectrum of systemic responses in severe COVID-19
To investigate the systemic immune response against SARS-CoV-2 at the time of critical deterioration, we studied serum samples collected at ICU admission and measured 48 cytokine, chemokine and growth factor biomarkers. Based on the 30-day post-admission mortality, the ICU group was divided into survivors and non-survivors. Unbiased patient clustering based on analyte quantification of the pre-delta cohort revealed a spectrum of systemic responses, where the majority of non-ICU patients grouped together showing lower serum concentrations (except for TRAIL) in comparison to ICU survivors and non-survivors (Fig. 1). A similar clustering pattern was observed in the delta cohort (Fig. S2) in which the majority of patients who did not survive had higher analyte levels in comparison to surviving patients.
Cytokine analysis of hospitalized COVID-19 patients. Heatmap of log-transformed cytokine concentrations of samples of the earliest time points. Patients are represented per column and patient conditions are indicated by column annotations. Cytokines are represented by rows. Clustering was performed based on Euclidean distance.
A subset of cytokines are associated to increased systemic inflammation, clinical severity, serum viral loads and mortality
In order to analyze the implications of elevated systemic cytokine levels, we investigated the association of serum analytes concentrations to clinical characteristics at ICU admission. Remarkably, CTACK, M-CSF, IP-10, IL-6, HGF and IL-18 showed a strong positive correlation to C Reactive Protein (CRP), a systemic inflammation biomarker, in comparison to other cytokines (Fig. 2a). Additionally, M-CSF (rS = 0.3918, p = 0.0034) and CTACK (rS = 0.4482, p = 0.0007) showed positive association with the APACHE II score, a clinically validated severity score and mortality estimation tool26 (Fig. 2b).
Cytokine association to clinical marker. (a) Spearman correlation analysis of cytokines to hemoglobin (HB) values, white blood cell count (WBC) and C reactive protein (CRP) was performed. Red indicates positive correlation, blue negative correlation. (b) Waterfall plot of Spearman correlation from cytokines to APACHE II scores. The dotted line indicates values above rS = 0.3 and cytokines with statistically significant correlation (M-CSF (magenta) and CTACK (green)). (c) Correlation of CTACK and M-CSF to SARS-CoV-2 viral load in serum samples of ICU non-survivors (black). Pearson analysis was performed. Linear-regression is shown as well as the 90% CI indicated by the dotted lines. ns = non-significant; * = p < 0.05.
As our previous work has demonstrated that non-survivor patients have higher systemic SARS-CoV-2 loads18, we investigated if cytokine concentrations were associated with higher viral copy numbers. Surprisingly, both M- CSF and CTACK showed a weak but significant correlation to serum SARS-CoV-2 copy numbers at ICU admission in the group of ICU non-survivors (Fig. 2c). The same analysis of the delta cohort revealed a distinct pattern of cytokine correlation to WBC, RBC or CRP (Fig. S3, a) in comparison to the pre-delta cohort. Notably, despite these differences, the positive correlation of CTACK to APACHE II (rS = 0.51938, p = 0.002) (Fig. S3b) and to SARS-CoV-2 viral load in non-survivors (Fig. S3, c) was maintained. This indicates differences in cytokine responses between patients infected with pre-delta and delta VoCs, but also consistent associations across variants analysis.
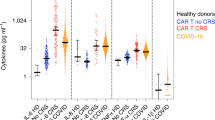
By classifying our cohort according to the patient disease severity and outcome, increased M-CSF, CTACK and IL-18 levels in the non-survivor group were found in comparison to ICU survivors and non-ICU hospitalized patients (Fig. 3a). This finding was validated in the delta cohort (Fig. S4, a). Longitudinal measurements of these three cytokines during ICU stay showed in both cohorts that increased concentrations in non-survivors were found early after ICU admission (Fig. 3b, Fig. S4b). In conjunction, these findings indicate that elevated CTACK, M-CSF and IL-18 may have a role in staging and identifying SARS-CoV-2 disease outcomes at ICU admission despite different VoCs involved. Notably, analysis of samples of critically-ill non-COVID pneumonia patients with severe sepsis collected at ICU admission did not show a significant elevation of CTACK, M-CSF or IL-18 in non-survivors (Fig. S5), arguing that their elevated levels are an exclusive feature of COVID-19 infection.
Analysis of mortality associated cytokines. (a) CTACK, IL-18 and M-CSF showed a significant increase in ICU non-survivors (black triangles) in comparison to ICU survivors (red squares). For analysis, a one-way ANOVA Kruskal–Wallis followed by Dunn’s correction was performed. Box plot showing the median of each group and the 10–90 percentile. (b) Individual samples of all patients were pooled according to their sampling period post-intubation (PI) and analyzed using the Kruskal–Wallis with Dunn’s correction test. The box plot shows the median of each group with the 10–90% percentiles. ns = non-significant; * = p < 0.05; ** = p < 0.01; **** = p < 0.0001.
Critically-ill SARS-CoV-2 patients have contrasting pulmonary functional trajectories according to their survival, and correlates to IL-10 and TNF-beta serum concentration levels
The identification of IL-18 and M-CSF as severity-associated cytokines confirmed previous reports that correlate their increased systemic concentrations to worse outcomes27,28. However, CTACK had not been previously found to be associated with unfavorable clinical outcomes in severe COVID-19. As CTACK has recently been implicated in the pathogenesis of pulmonary fibrosis29, we decided to explore the pulmonary compartment in our cohort. By using non-invasive diagnostic imaging30, we found that around 80% of all pre-delta ICU patients presented fibro-proliferative changes by lung ultrasound sonography (USG) at ICU admission (Fig. S6). Moreover, by examining pulmonary functional data obtained from invasive respiratory monitoring, we found a significantly increased lung compliance in delta infected patients in comparison to pre-delta patients detected at ICU admission (Fig. S7b). When comparing the survivor and non-survivor groups in both cohorts, we identified contrasting functional trajectories depending on the VoC involved. In the pre-delta cohort, lung compliance was similar in survivor and non-survivor groups at admission, and survivors showed a significant improvement after 48 h of specialized intensive care (Fig. 4a). Conversely, delta infected patients showed hardly any improvement over time in both survivors and non-survivors (Fig. S7a) and had better lung compliance at admission in comparison to pre-alpha and alpha VoC (Fig. S7b). Remarkably, by examining the relationship between serum cytokine concentration and gas exchange at 6 h post intubation, we identified that IL-10 and TNF-beta serum levels had a significant positive correlation with PaO2/FiO2 in survivors of the pre-delta cohort (Fig. 4b,c). The delta cohort, however, showed much weaker correlation of cytokines to PaO2/FiO2 results (Fig. S7c). This evidence may suggest that patients that survived severe COVID-19 disease despite low initial lung compliance did not only show early differences in cytokine network regulation, but also in their functional pulmonary trajectories in comparison to those who did not survive. The contrasting findings seen in delta-infected patients may be a reflection of underlying differences in patients’ status at admission to the ICU, or of differences in the VoC afflicting them.
Analysis of cytokines and lung function. (a) Lung compliance was calculated for all patients. For analysis of survivors and non-survivors (left and middle graph) a Friedmann test or for the comparison of survivor to non-survivor (right graph) a one-way ANOVA Kurskal-Wallis followed by Dunn’s correction was performed. Box plots show the median of each group and the 10–90 percentile. Dot plots show the individual values of each patient (red = survivor, blue = non-survivor). The dotted line indicates 50 ml/cmH2O which is the lung compliance of a healthy individual. (b) Heatmap of Spearman correlation analysis of cytokines to the PaO2/FiO2 ratio at 6h post intubation. Red indicates positive correlation, blue negative correlation. (c) Individual correlation plot of PaO2/FiO2 ratio at 6h post intubation to IL-10 and TNF-β concentrations in ICU survivor. ns = non-significant; * = p < 0.05; ** = p < 0.01;*** = p < 0.001; **** = p < 0.0001.
Severe dysregulation of cytokine correlation in ICU non-survivor
Cytokines regulate the inflammatory response via complex networks that balance their levels and ultimately their effects on the host31. To investigate this network in our cohort, we performed a cytokine-to-cytokine correlation analysis in the earliest samples from ICU admission. By comparing correlation heatmaps, a significant cytokine-to-cytokine association was found in survivors, which was almost entirely lost in the non-survivor group (Fig. 5). Importantly, this was also observed in the delta cohort, although to a lesser extent (Fig. S8). These results suggest that a severe dysregulation of the systemic cytokine network in COVID-19 non-survivors was already present at ICU admission. Importantly, the same cytokine correlation analysis in critically ill non-COVID patients with severe sepsis revealed an opposite pattern with an increase of correlation in non-surviving patients (Fig. S9).
Cytokine-to-Cytokine correlation analysis. Cytokine concentrations were log transformed and a parametric Pearson correlation analysis was performed. Rows and columns represent cytokines. Red symbolized positive correlation and blue negative correlation. Cytokines were clustered according to Euclidean distance. The order of cytokines both in the rows and columns are equal between survivor and non-survivor. (a) Correlation heatmap of samples from the first time point (24-36h post intubation. (b) correlation heatmap of samples from the second time point (48-72h after the first sampling). Samples from 10/16 survivor and 20/38 non-survivor were available at the second time point due to earlier release from ICU or passing away from patients.
Discussion
Several serum cytokines have been associated with COVID-19 disease severity and have been proposed as potential biomarkers and/or therapeutic targets32. High IL-6, procalcitonin (PCT) and CRP were associated with fatal outcomes using samples collected at hospital admission in a German COVID-19 cohort with a mortality of around 11%33. By using a similar time point, another group found that IFN-β, IL-13, TNF-β, TGF-α, and IL-18 were associated with mortality14. Likewise, an international study in Europe identified serum HGF and CXCL13 as markers of mortality after confirmation by a validation cohort8. These differences in cytokine identification underline difficulties at comparing heterogeneous, low-mortality populations with inconstant hospitalization criteria across sites. For this reason, we decided to focus on a high-mortality cohort in which sampling occurred at ICU admission due to its temporal association with severe worsening of pulmonary and systemic compromise. This cohort underwent a strict standardized clinical management protocol that did not include immunomodulatory therapies, other than systemic steroid therapy, as recommended by international guidelines34. This led to a patient assortment that allowed a forthright survival classification with minimal treatment selection bias. Additionally, by using a second cohort, which was infected with another VoC, we were able to validate key findings while analyzing differences and similarities across variants. By dividing the ICU groups according to the fatal outcome after a 30-day follow-up, we found three cytokines that were significantly elevated in non-survivors (CTACK, IL-18 and M-CSF) at ICU admission, both in pre-delta and in delta infected patients but not in the non-COVID cohort. Besides association with mortality, we found a weak but significant correlation with serum SARS-CoV-2 viral load for CTACK in non-survivors of both cohorts, which may suggest a relationship between serum mediators and viral-induced pathogenicity, as an important survival determinant18. Remarkably, this cytokine level also positively correlated with APACHE II, a validated prediction tool used in ICU. Our study results are partly overlapping with those by Takashima et al.35, who investigated cytokine responses in a small cohort with a 43% mortality rate. They found that non-survivors had significantly elevated levels of several immune mediators including SDF-1, SCYB16, sCD30, IL-11, IL-18, IL-8, IFN-γ, TNF-α, sTNF-R2, M-CSF, and I-309. On the other hand, TRAIL levels were significantly lower in the cohort on mechanic ventilation than in the hospitalized controls, which was in line with previous reports 36,37, and possibly an indication of protective TRAIL effects.
The mortality-associated cytokines that we identified have various mechanistic and therapeutic significance. M-CSF is a growth factor implicated in steady-state mielopoiesis and monocyte production of proinflammatory cytokines38. A role of M-CSF in lung infection resolution has been reported, as animal models have confirmed its relevance in bacterial pneumonia and mononuclear phagocyte activation39. M-CSF has also been associated with lung damage in COVID-1940,41. IL-18 identification as a severity-associated cytokine brings further evidence of dysregulation in the monocyte/macrophage population. IL-18 is a member of the IL-1 family, mainly produced by macrophages and monocytes in response to several stimuli, including viral infection. By identifying IL-18 association with worse COVID-19 outcomes, our study is in line with previous reports15,27,42, and gives support to the role of monocyte/macrophage dysfunction and myeloid-driven immunopathology as COVID-19 severity determinants9. Interestingly, anti-IL-18 antibodies have been tested in clinical settings and shown to reduce inflammatory markers like CRP but not APACHE II scores, when compared with placebo treated patients43. This shows the relevance of this cytokine but also indicates that IL-18 alone is not the key driver of decease severity. Importantly, by using a cohort of non-COVID-19 patients with sepsis and pneumonia as control, we delineated the specificity of these analytes for severe SARS-CoV-2 disease.
We identified a hitherto undescribed association of systemic CTACK levels with poor prognosis of COVID-19. CTACK has been thought to be exclusively involved in skin-related responses until recently. Its role as a biomarker in idiopathic lung fibrosis (ILF), a rapidly progressive interstitial pneumonia associated with alveolar epithelial injury and abnormal tissue repair without a known cause, has been identified29. One small COVID-19-related study reported an increase of CTACK in COVID-19 patients in comparison to healthy controls but concentrations did not differ among severity degrees44. While fibrotic pulmonary complications have been described as COVID-19 sequelae44,45, no investigation on its relation to acute severe COVID-19 has been performed. In the pre-delta cohort, the majority of ICU patients presented a low lung compliance at ICU admission, as well as a fibroproliferative pattern identified by lung ultrasound. Interestingly, patients infected with the later occurred VoC delta did not show this low lung compliance. These findings may constitute evidence of early fibrosis-like changes within lungs of severely ill patients infected with pre-delta VoCs. Of interest, a transcriptomic tool formulated to predict ILF outcomes was also useful for COVID-1946, suggesting a shared pathophysiology. While an association of cytokine networks to lung fibrosis remains a topic for future investigations, our findings constitute to our knowledge the first report on CTACK association to fatal COVID-19 outcomes.
Finally, we found differences in cytokine-to-cytokine correlation between survivors and non-survivors. Cytokine regulation involves an enhancer-suppressor network that has been proposed to be defective in severe COVID-19, as uncontrolled cytokine overproduction is a key driver of COVID-19 severity47. Our work shows that the loss of cytokine-to-cytokine correlation is present at ICU admission in patients who did not survive, supporting the hypothesis that an early immune dysregulation profile may have a prognostic value or be a therapeutic target, besides the administration of systemic steroids. This finding is supported by a study which also proposed a dysregulated cytokine response at ICU admission to be associated with mortality48. It is remarkable that this disruption of cytokine networks was specific for our COVID-non-survivors and not a feature encountered in non-COVID pneumonia casualties. While our dataset do not allow a cause-effect analysis, it identified novel cytokines as indicators of COVID-19 outcomes.
Conclusion
To conclude our findings, even though pre-delta and delta patients presented differences in clinical and laboratory markers, the cytokine profiles showed similar patterns. The novel mortality-associated cytokine CTACK showed in both cohorts associations to mortality and severity-based markers. Additionally, IL-18 and M-CSF have been found across other studies to be severity/ mortality associated, nevertheless, a clear answer is still not found which cytokines are actually responsible for mortality. Besides those individual cytokines, we report an early loss of cytokine-to-cytokine correlation in the non-survivor groups. These findings might point to the importance of cytokine detection even for Omicron strains of SARS-CoV-2 that have prevailed recently, which would need to be confirmed in independent cohorts.
Limitations
Our study has several limitations. Sampling occurred in late 2020 and early and late 2021, prior to the onset of the omicron variants and prior to the emergence of a basal herd immunity. Hence, it is possible that the immune responses may skew differently in hosts that are primed against SARS-CoV-2 and/or infected with more recent VoC. Since our data were collected on a cohort of mechanically ventilated patients, where PaO2/FiO2 ratios may be affected by FiO2 applied to patients49, the correlation of cytokine to PaO2/FiO2 levels needs to be considered carefully. Similar to other discovery-based cohorts, our sample size was not adequately powered, and it was dependent on patient availability and logistical limitations. In addition, although multiplex assay allows for a broad immune mediator screening, confirmation of our mortality-related cytokines significance in other platforms is desirable in subsequent validation cohorts. Nevertheless, our results provide a direct insight into the systemic cytokine networks at a critical time point in COVID-19 and identify CTACK as a novel mortality-associated cytokine in pre-delta and delta infected patients, which may have important mechanistic and therapeutic implications.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Berlin, D. A., Gulick, R. M. & Martinez, F. J. Severe Covid-19. N. Engl. J. Med. 383(25), 2451–2460 (2020).
Abers MS, Delmonte OM, Ricotta EE, Fintzi J, Fink DL, de Jesus AAA, et al. An immune-based biomarker signature is associated with mortality in COVID-19 patients. JCI Insight. 6(1): (2021).
Balnis, J. et al. Unique inflammatory profile is associated with higher SARS-CoV-2 acute respiratory distress syndrome (ARDS) mortality. Am. J. Physiol. Regul. Integr. Comp. Physiol. 320(3), R250–R257 (2021).
Lucas, C. et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 584(7821), 463–469 (2020).
Bulow Anderberg, S. et al. Increased levels of plasma cytokines and correlations to organ failure and 30-day mortality in critically ill Covid-19 patients. Cytokine. 138, 155389 (2021).
Del Valle, D. M. et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26(10), 1636–1643 (2020).
Herr, C. et al. Distinct patterns of blood cytokines beyond a cytokine storm predict mortality in COVID-19. J. Inflamm. Res. 14, 4651–4667 (2021).
Perreau, M. et al. The cytokines HGF and CXCL13 predict the severity and the mortality in COVID-19 patients. Nat. Commun. 12(1), 4888 (2021).
Vanderbeke, L. et al. Monocyte-driven atypical cytokine storm and aberrant neutrophil activation as key mediators of COVID-19 disease severity. Nat. Commun. 12(1), 4117 (2021).
Youngs, J. et al. Identification of immune correlates of fatal outcomes in critically ill COVID-19 patients. PLoS Pathog. 17(9), e1009804 (2021).
Group WHOREAfC-TW et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: A meta-analysis. JAMA 326(6), 499–518 (2021).
Kyriazopoulou, E. et al. Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: A double-blind, randomized controlled phase 3 trial. Nat. Med. 27(10), 1752–1760 (2021).
Mulchandani, R., Lyngdoh, T. & Kakkar, A. K. Deciphering the COVID-19 cytokine storm: Systematic review and meta-analysis. Eur. J. Clin. Invest. 51(1), e13429 (2021).
Gomez-Escobar, L. G. et al. Cytokine signatures of end organ injury in COVID-19. Sci. Rep. 11(1), 12606 (2021).
Guo, J. et al. Cytokine signature associated with disease severity in COVID-19. Front. Immunol. 12, 681516 (2021).
Force, A. D. T. et al. Acute respiratory distress syndrome: The Berlin definition. JAMA 307(23), 2526–2533 (2012).
Marshall, J. C. et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 20(8), e192–e197 (2020).
Ynga-Durand, M. et al. SARS-CoV-2 viral load in the pulmonary compartment of critically Ill COVID-19 patients correlates with viral serum load and fatal outcomes. Viruses 14(6), 1292 (2022).
Brunkhorst, F. M. et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis-related organ dysfunction in patients with severe sepsis: A randomized trial. JAMA 307(22), 2390–2399 (2012).
Bloos, F. et al. Effect of sodium selenite administration and procalcitonin-guided therapy on mortality in patients with severe sepsis or septic shock: A randomized clinical trial. JAMA Intern. Med. 176(9), 1266–1276 (2016).
Galili, T., O’Callaghan, A., Sidi, J. & Sievert, C. heatmaply: an R package for creating interactive cluster heatmaps for online publishing. Bioinformatics. 34(9), 1600–1602 (2018).
Taiyun Wei V. S. R package 'corrplot': Visualization of a Correlation Matrix. (2021).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32(18), 2847–2849 (2016).
Kolde R. Implementation of heatmaps that offers more control over dimensions and appearance. (2019).
Conway, J. R., Lex, A. & Gehlenborg, N. UpSetR: An R package for the visualization of intersecting sets and their properties. Bioinformatics 33(18), 2938–2940 (2017).
Zou, X. et al. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit. Care Med. 48(8), e657–e665 (2020).
Satis, H. et al. Prognostic value of interleukin-18 and its association with other inflammatory markers and disease severity in COVID-19. Cytokine 137, 155302 (2021).
Liu, Y. et al. Elevated plasma levels of selective cytokines in COVID-19 patients reflect viral load and lung injury. Natl. Sci. Rev. 7(6), 1003–1011 (2020).
Niwamoto, T. et al. Cutaneous T-cell-attracting chemokine as a novel biomarker for predicting prognosis of idiopathic pulmonary fibrosis: A prospective observational study. Respir. Res. 22(1), 181 (2021).
de Almeida Monteiro, R. A. et al. Ultrasound assessment of pulmonary fibroproliferative changes in severe COVID-19: A quantitative correlation study with histopathological findings. Intensive Care Med. 47(2), 199–207 (2021).
Liu, C. et al. Cytokines: From clinical significance to quantification. Adv. Sci. (Weinh). 8(15), e2004433 (2021).
Wahid, B., Rani, N. & Idrees, M. Cytokine storm syndrome in SARS-CoV-2: A review. Z Naturforsch C J Biosci. 77(1–2), 65–69 (2022).
Zobel, C. M. et al. Serum interleukin-6, procalcitonin, and C-reactive protein at hospital admission can identify patients at low risk for severe COVID-19 progression. Front. Microbiol. 14, 1256210 (2023).
Panel C-TG. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines.: National Institutes of Health; [Available from: https://www.covid19treatmentguidelines.nih.gov/.
Takashima, Y. et al. Potential marker subset of blood-circulating cytokines on hematopoietic progenitor-to-Th1 pathway in COVID-19. Front. Med. 11, 1319980 (2024).
Tegethoff, S. A. et al. TNF-related apoptosis-inducing ligand, interferon gamma-induced protein 10, and C-reactive protein in predicting the progression of SARS-CoV-2 infection: A prospective cohort study. Int. J. Infect. Dis. 122, 178–187 (2022).
Mastboim, N. S. et al. An immune-protein score combining TRAIL, IP-10 and CRP for predicting severe COVID-19 disease. Cytokine 169, 156246 (2023).
Chousterman, B. G. & Arnaud, M. Is there a role for hematopoietic growth factors during sepsis?. Front. Immunol. 9, 1015 (2018).
Bettina, A. et al. M-CSF mediates host defense during bacterial pneumonia by promoting the survival of lung and liver mononuclear phagocytes. J. Immunol. 196(12), 5047–5055 (2016).
Chi, Y. et al. Serum cytokine and chemokine profile in relation to the severity of coronavirus disease 2019 in China. J. Infect. Dis. 222(5), 746–754 (2020).
Quartuccio, L. et al. Interleukin 6, soluble interleukin 2 receptor alpha (CD25), monocyte colony-stimulating factor, and hepatocyte growth factor linked with systemic hyperinflammation, innate immunity hyperactivation, and organ damage in COVID-19 pneumonia. Cytokine 140, 155438 (2021).
Coutinho, L. L. et al. Elevated IL-18 predicts poor prognosis in critically ill COVID-19 patients at a Brazilian hospital in 2020–21. Future Microbiol. 17, 1287–1294 (2022).
Hakim, A. D. et al. Efficacy and safety of MAS825 (anti-IL-1beta/IL-18) in COVID-19 patients with pneumonia and impaired respiratory function. Clin. Exp. Immunol. 213(3), 265–275 (2023).
Xu, Z. S. et al. Temporal profiling of plasma cytokines, chemokines and growth factors from mild, severe and fatal COVID-19 patients. Signal Transduct. Target. Ther. 5(1), 100 (2020).
Spagnolo, P. & Oldham, J. M. Fibrotic lung disease: A molecular glimpse into severe Covid-19?. EBioMedicine. 69, 103470 (2021).
Juan Guardela, B. M. et al. 50-gene risk profiles in peripheral blood predict COVID-19 outcomes: A retrospective, multicenter cohort study. EBioMedicine. 69, 103439 (2021).
Montazersaheb, S. et al. COVID-19 infection: An overview on cytokine storm and related interventions. Virol. J. 19(1), 92 (2022).
Shaw, J. A. et al. Immunologic and vascular biomarkers of mortality in critical COVID-19 in a South African cohort. Front. Immunol. 14, 1219097 (2023).
de Heder, V., Soephie, C., Frouke, K., Leo, H. & Angelique, D. M. The effect of oxygen on the PaO2/FiO2-ratio and shunt fraction in patients on mechanical ventilation: A physiological study. Eur. Respir. J. 56(suppl 64), 351 (2020).
Acknowledgements
We thank the physicians and nurses from the Clinical Hospital Center Rijeka, Croatia, as well as all the patients. We thank Christine Falk who helped us in establishing the BioPlex analysis, Martijn Zoodsma and Yang Li for their scientific input and help in analyzing datasets as well as Heiner Wedemeyer and Hortense Slevogt.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research was supported by the Project “Virological and immunological determinants of COVID-19 pathogenesis–lessons to get prepared for future pandemics (KA1-Co-02 “COVIPA”)”, a grant from the Helmholtz Association’s Initiative and Networking Fund. It was funded by the German Scientific Foundation (DFG) through the RESIST Excellence cluster (EXC 2155, project B6), and the Helmholtz Association EU partnering grant PIE-0008. This work has been supported in part by the Croatian Science Foundation under the project IP-CORONA-04-2073 (I.B.).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: H.M., M.Y.-D. and L.Č.-Š.; investigation: H.M., M.Y.-D., I.B., F.K. and M.P.M.; formal analysis: H.M., M.Y.-D. and L. Č.-Š.; resources: A.Š., A.P., I.B, F.K., M.M., I.Ž., F.B. and SepNet; data curation, L.Č.-Š. and A.P.; writing—original draft preparation: H.M. and M.Y.-D.; writing—review and editing: L. Č.-Š.; supervision: L. Č.-Š. and S.J.; funding acquisition: L. Č.-Š. And I.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
LCS received consulting fees by CORAT Therapeutics, DIGID Diagnostics, Dr. Wolff Group and SANOFI Pharma. LCS received speaker’s honoraria by SWIXX Pharma and SANOFI Pharma. LCS has the following patents: EP3655526 and EP22153256.7. LCS has unpaid positions in the HZI Board of Trustees, he is a member of the Vaccine task force of the European Federation of Immunological Societies and is the co-coordinator for the Vaccine group of the German Immunological Society. Other authors have no competing interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maaß, H., Ynga-Durand, M., Milošević, M. et al. Serum cytokine dysregulation signatures associated with COVID-19 outcomes in high mortality intensive care unit cohorts across pandemic waves and variants. Sci Rep 14, 13605 (2024). https://doi.org/10.1038/s41598-024-64384-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64384-y
- Springer Nature Limited