Abstract
This study explores the experiences of Polish caregivers of children with rare disease (CRD) with health care and social services for CRD. A mixed-methods approach was employed, using an open-ended questionnaire with a convenience sample. Quantitative data presented through descriptive statistics, were complemented by thematic analysis applied to qualitative responses. Responses from 925 caregivers of 1002 children with CRD revealed that the duration of the diagnostic journey varied, spanning from 0 to 18 years, with an average time of 1.7 years. Similarly, the average number of physicians consulted before receiving the correct diagnosis was 4.8. The Internet was basic source of information about children’s disease. Although caregivers were to some extent satisfied with the quality of health care for CRD, they complained at the accessibility of health care and social services, physicians’ ignorance regarding RDs, the lack of co-ordinated care and financial and psychological support. To break the cycle of the diagnostic and therapeutic odyssey that may aggravate the condition of CRD, cause parental stress and financial burden there is a need to change our view on CRD from cure to family-oriented care. Multifaceted challenges and needs of CRD families should be prioritized.
Similar content being viewed by others
Introduction
Rare diseases (RDs) are defined in Europe as chronically debilitating or life-threatening conditions with prevalence of less than 50/100000 i.e. 1/20001. Some conditions, however, classified as ultra-rare diseases affect fewer than 1/100000, while hyper-rare diseases affect fewer than 1/1000000002. In fact, according to the Orphanet database 84.5% of all RDs have a prevalence of less than 1/10000003. As 250 new diseases are classified as RDs every year, there are currently more than 10,867 RDs4, and in the European Union (EU) alone between 17.8 and 30.3 million people live with a RDs, while globally there are between 262.9 and 446.2 million sufferers1.
Although over the years clinical breakthroughs have been made in the field of orphan drugs, only between 5 and 10% of RDs have approved drug therapy5. RDs are therefore characterised by high morbidity and mortality, especially among children, as 70% of RDs manifest as paediatric diseases, and 50% of children die before the age of five, and 35% die before their first birthday6.
Due to the multiplicity, complexity and severity of symptoms resulting in physical, cognitive, mental, behavioural and motoric problems, and the increased risk of premature death, RDs affect the entire family7,8,9, and society as a whole10,11. Since RDs have been recognised as a public health priority, they require the integrated care of a range of healthcare professionals12. The EU has therefore urged all Member States to adopt a national policy regarding RDs, and has promoted several initiatives, including the improvement of definition, codification and cataloguing of RDs and orphan drugs, the establishment of European Reference Networks for RDs and the development of a European Platform on Rare Disease Registration13,14. Some countries are still to adopt national plans for RDs, and others’ policies have technically expired15.
Although the number of RD patients in Poland is estimated at between 2.3 and 3 million16, the first national Plan for Rare Diseases was adopted only recently in August 2021. Its established goal is to improve the visibility of RD patients by creating a Polish Rare Diseases Registry and introducing electronic RD patient passports; to improve the diagnostics and treatment of RDs by facilitating access to modern diagnostics using large-scale genomic testing, medicines, high-quality innovative healthcare services and diets to manage the particular nutritional needs of RDs; and to establish Centres of Expertise for Rare Diseases Information Platform: Rare Diseases16. Since the plan is still in consultation, many solutions are yet to be implemented. RD families are therefore still waiting for support mechanisms and struggle for appropriate care.
Significantly, most research on RDs in Poland focuses either on its clinical dimension, i.e. the symptoms, causes and treatment options, or RD patients, but less attention has been paid to the family caregivers of children with RDs (CRD). Caring for CRD affects caregivers’ physical, psychological, emotional and functional health, and may undermine the quality of life of both caregiver and CRD7,8,9. Since one of the most onerous challenges parents face in caring for CRD is related to their encounters with the healthcare system17,18,19,20,21,22,23,24,25,26, this study explores the experiences of Polish caregivers with the healthcare and social services for CRD, by asking the following research questions: 1) What are CRD patents’ experiences with the diagnostic process in their CRD?; 2) How do parents’ perceive health care services for CRD?; 3) What are CRD caregivers’ experiences with the social services?; 4) What are the main needs of CRD caregivers?
Methods
Study design
As part of a larger project that focuses on the challenges and needs of parents who care for CRD, this study specifically delves into experiences of Polish caregivers with the healthcare and social services for CRD. Since to date there is no registry of paediatric RD patients in Poland and the exact number of CRD is unknown, the study was designed as a self-administered, anonymous, computer-assisted online survey on the CRD caregivers experiences with healthcare and social services27.
Ethical considerations
This study was performed in line with the principles of the Declaration of Helsinki28. The study received ethical and research governance approval from the Poznan University of Medical Sciences’ Bioethics Committee (KB – 833/22, 22 October 2022). Before completing the survey all eligible participants signed the informed consent form to participate which explained the purpose of the study and methods used, voluntary, anonymous and confidential character of the survey, and the possibility to withdraw from the study at any time without any implications.
Participants and setting
Study participants were recruited via a convenience sampling, with the support of several RD foundations, patients’ associations and organisations via their webpages and Facebook. Participants were accepted if they were parents or family members who provided care for CRD (below 18 years of age), were able to use electronic devices and participate in the online survey.
The study was conducted between October 13, 2022 and May 28, 2023 among 925 voluntary participants.
Research tool
The data reported here derive from an original questionnaire with both closed-ended and open questions that was designed after a thorough analysis of the literature17,18,19,20,21,22,23,24,25,26. While it is part of a larger study on the experiences of Polish family caregivers of children with a rare disease, this research focuses on the challenges and needs associated with access to the healthcare and social services for CRD.
Because there is no specific tool for the assessment of CRD caregivers’ experiences with healthcare services an ad hoc questionnaire was constructed. Once it was evaluated by a paediatrician who specialises in RDs, a public health specialist and a medical sociologist, it was pre-tested via an online platform with ten caregivers, and then re-evaluated by additional specialists from the same fields which resulted in rephrasing three questions regarding assessment of various healthcare services for CRD.
The questions selected for this study focused on the caregivers’ experiences with the healthcare system, including assistance from government and social institutions, quality of health care, availability of medical specialists’ care, accessibility of medications, financial assistance and medical information, family support from healthcare workers, doctors’ knowledge on RDs, doctors’ communication skills an emotional support, interaction with genetic and psychological clinic. While most questions were explored using closed-ended questions using a 5-Likert scale ranging from 1 (strong dissatisfaction or disagreement) to 5 (high satisfaction or agreement), caregivers were encouraged to develop these issues by answering additional open question regarding theirs experiences with the health care and social services for CRD (“Could you describe, in your own words, your experiences with the health care and social services for children with rare disease?”). In total, 327 caregivers shared their experiences.
Data collection
The survey was distributed via webpages and Facebook by sending a letter of invitation from the research coordinator (JD) to a number of RD foundations, patients’ associations and organisations. Upon receiving permission to post the online questionnaire, all eligible caregivers were invited to share their experiences by completing the surrey using electronic devices (e.g. computers, tablets or smartphones). The study invitation included the online consent form and before completing the survey respondents were requested to select an “I agree” or “I do not agree” checkbox. Two follow-up messages were sent in January and March. Completing the survey took between 15 and 20 min.
Data analysis
Before being transferred to the statistical software JASP (Version 0.18.1), the questionnaire data underwent a thorough check to ensure accuracy, completeness, and consistency.
The quantitative data are presented using descriptive statistics. Additionally, mean and standard deviation (SD) with 95% confidence intervals (CI) for the caregiver’s age, time before the child received the correct diagnosis, and the number of physicians consulted before the child received the correct diagnosis were computed using 5000 bootstrap replicates.
While the classical grounded theory was used for the design of this study29, the qualitative data were analysed using a content and thematic analysis30,31. The qualitative results were selected by employing an inductive approach, which aims at identifying new analytic categories that are not limited to existing theories or research, and classified as thematic categories. Firstly, all responses were read several times for coding purpose, and categorised during familiarisation. Key words, significant phrases and statements describing caregivers’ experiences with the healthcare system were sought. The initial results were assigned preliminary codes with the relevant supporting quotations selected. While the coding was performed by the principal investigator (JD) who is medical sociologist, trained in qualitative research methods, the second researched (DW) helped in the interoperation of the data. Following grounded theory approach during the entire coding process, the researchers remained open to new potential themes and subthemes emerging during the data analysis. A matrix of the codes was then created according to the themes that emerged from caregivers’ responses. These codes were then organised into domains and descriptive results were outlined. The sampling continued until saturation was achieved and no new themes emerged. When the coding was completed both researchers extended notes and discussed generated categories and emerging theory. Any conflicting data was discussed and resolutions were reached within the team. Once agreement had been reached, the final categories were read and analysed using thematic analysis (Supplementary material Table S1).
Results
Characteristics of CRD parents
A total of 925 family caregivers caring for 1002 CRD (see: Supplementary material Table S2) completed the survey, of which 93% were mothers (mean age: 37.4; range: 19–72) (Table 1). 92.1% of caregivers provided care for one CRD and 7.9% for two or more. 67% of caregivers reported a higher level of education and 54.6% reported they were unemployed. 79.8% used no external help in caring for their CRD, and 73.1% received care allowance, i.e. a monthly cash payment granted in Poland to those who renounce paid employment to care permanently for a family member who requires special care (2450 Polish zloty = €565).
CRD parents’ diagnostic experiences
Since only 29.3% of CRD were diagnosed during prenatal testing or newborn screening, many caregivers reported problems with timely diagnosis (Table 2). While the time taken by the diagnostic journey varied, ranging from 0 to 18 years with a median of 1 year and a mean of 1.7 years. Additionally, it provides insights into the number of physicians consulted before receiving the correct diagnosis, with a median of 3 and a mean of 4.8.
Although 54.6% of caregivers identified medical specialists as the main sources of information on their children’s RD, only 7.7% identified their general practitioner. For 88% of parents the Internet was the basic source of information about their children’s disease.
Caregivers’ perspective on the health and social service for CRD
Although most caregivers evaluated five dimensions of the Polish healthcare system for CRD rather positively, the majority expressed dissatisfaction with its organization (Table 3). In fact, while more than half of caregivers were satisfied with the quality of healthcare services for their CRD (58% vs 35.2% dissatisfied), doctors’ communication skills (54% vs 35.1%), interaction with genetic clinics (50.7% vs 26.3%) and doctors’ empathy (50.2% vs 37.5%), still nine dimensions of healthcare services were assessed negatively, and most parents reported disappointing experiences with the Polish healthcare system for CRD. In particular, caregivers complained about the lack of financial help (66% dissatisfied vs % 17.5% satisfied), the lack of support from government and social institutions (65.4% vs 20.8%) and the access to medications for CRD (40.2% vs 36.4%). Caregivers criticised the lack of information regarding their children’s disease from physicians (65.2% vs 29.1%), including practical information on the way to deal with the disease (49.5% vs 38.4), and those provided by the system (56% vs 38.3%). They were also dissatisfied with the availability of specialist care (60.9% vs 32%), support from healthcare workers (51.1% vs 37.5%) and doctors’ empathy (48.6% vs 37.5%). These quantitative data were further supported by textual findings from the qualitative findings described below.
Parental experiences with the healthcare and social services for children with rare diseases
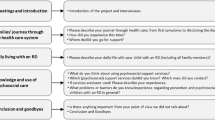
The thematic analysis of the open question identified two major themes: 1. experiences with the healthcare system, and 2. experiences with the government and social services. Both themes were categorised into two main domains: challenges and needs (Fig. 1).
Challenges and needs related to navigating the healthcare system
The first theme, with 15 associated sub-themes and representative quotations [Q] is summarised in Table 4. The first six sub-themes related to CRD caregivers’ struggle with the healthcare services.
Diagnostic odyssey
Caregivers were burdened by the diagnostic process (Q1–Q5). It was framed as a ‘waste of time’ (Q3, Q4) leading to misdiagnosis (Q2, Q3). The diagnostic journey was also described as ‘the most traumatic experiences’ in a child’s disease (Q5), either due to doctors’ lack of interest (Q1, Q2) or intuitive or accidental nature of the diagnostic process (Q3–Q5).
Therapeutic odyssey
Caregivers struggled to receive appropriate treatment for their CRD (Q6–Q8). While they complained that delays in treatment resulted from doctors’ reluctance to care for CRD (Q6–Q7), parents stressed that it fell to them to find such treatment and cover it from a private funds (Q6–Q8).
Lack of specialised care
Parents found it very challenging to find a specialist for their CRD, either due to a lack of doctors (Q9, Q11), protracted waiting lists for medical specialists (Q9, Q11) or the necessity to travel great distances (Q10).
Lack of integrated care/holistic approach
Parents complained at the lack of integrated care (Q12–Q14), poor care pathways and communication between specialists whom they visited separately and had to repeat the information all over again (Q13, Q14).
Cross-border health care
Since some parents were unable to find treatment in Poland (Q17–Q18), they had to look for healthcare services abroad (Q15–Q18). Caregivers suggested that this was a result both of doctors’ lack of knowledge about their child’s disease (Q15, Q17, Q18), and lack of interest or willingness to provide such care (Q16).
Lack of psychological support for CRD parents
Caregivers were burdened by the lack of emotional support from healthcare providers (Q19–Q22). Some complained at the scant support at the time of diagnosis (Q19, Q20). Others suggested that they had never received any support (Q19, Q21, Q22). Many parents therefore felt abandoned and neglected (Q19, Q22).
Another four sub-themes referred to the difficulties experienced in interacting with doctors.
Physicians’ ignorance of RDs
One of the greatest challenges parents reported facing was related to healthcare professionals’ lack of knowledge regarding RDs (Q23–Q26). In the face of doctors’ ignorance parents had to become experts in their child’s disease (Q23–Q26). Caregivers reported at the same time that doctors’ ignorance resulted in a lack of understanding of the needs of parents (Q23, Q24) and empathy (Q24, Q25).
Lack of communication with doctors
Parents complained at doctors’ communication skills and poor interaction (Q27–Q29). They criticised doctors for speaking in an overly formal manner, like ‘robots’ (Q27), devoting too little time to caregivers, and failing to engage in meaningful communication (Q27, Q28). Caregivers also expressed dissatisfaction with the amount of information received and suggested that they had to seek it out themselves (Q28, Q29).
Doctors’ attitudes: paternalism
Caregivers reported paternalistic attitudes among doctors (Q30–Q33) and suggested that doctors acted as though they knew everything better than parents did and ignored caregivers’ ‘gut instincts’ and suggestions (Q30, Q31). Some parents reported being treated as though they were ‘mad’ or ‘overprotective parents’ (Q30–Q33).
Lack of empathy from doctors
Parents complained at healthcare professionals’ lack of empathy and compassion (Q30–Q33), and suggested that they cared neither for CRD (Q30, Q31) nor caregivers’ problems and needs (Q32). Parents also reported that such coldness resulted in mistreatment (Q30, Q31).
Another five sub-themes referred to caregivers’ needs related to healthcare services for CRD.
Psychological/emotional support for CRD parents
Parents expressed the need for psychological support (Q37–Q39). While stressing that a child’s disease affects the entire family (Q39), caregivers emphasised that emotional and psychological support is required as early as at the time of diagnosis (Q37–Q39).
Information on RDs
Parents reported the need for information on the RD their child had been diagnosed with (Q40–Q42). They expected ‘materials and knowledge’ on the disease itself, (Q40, Q42) and practical information about where they might seek institutional help (Q42). Courses teaching parents how to care for their RD child were also requested (Q42).
Improved diagnostics
Another need referred to early diagnosis, which would help parents cope better with the stress (Q43–Q45). While prompt diagnosis was defined as ‘a priority’ (Q43), parents expressed the need for better access to modern diagnostics using large-scale genomic testing (Q44), and stressed the prohibitive expense of covering it from private funds (Q44, Q45).
Co-ordinated care
Caregivers hoped for improved co-ordination of care for their CRD (Q46–Q48). In discussing the psychosocial consequences of fragmented care (Q46, Q47) they stressed the urgent need for improved co-operation between specialists (Q46–Q48). The need for an holistic approach towards CRD and their caregivers was also emphasised (Q48).
Access to innovative therapies
Caregivers were also hoping for a cure for their children (Q49–Q50). While some parents expressed hope for effective gene therapy (Q49), others described their struggle to secure experimental therapies (Q50).
Caregivers perception of the government and social services for CRD
The second theme referring to parents’ experiences with the government and social services, with 11 associated sub-themes and representative quotations, is summarised in Table 5.
Lack of support for caregivers
In describing the health policy towards RDs parents stressed that they felt abandoned (Q1–Q3). They complained at the lack of institutional support (Q1, Q2) and that no one cared about needs of either CRD (Q2, Q3) or parents (Q1, Q2).
Lack of information
Caregivers felt abandoned by the government and social institutions and stressed the extent to which they felt ill-supported in securing information on medical and social services for their children, including rehabilitation, re-imbursement and system of jurisprudence (Q4–Q6). They emphasised that, when seeking practical easy-to-understand information, parents had to rely more on other parents than social institutions (Q4, Q5).
Lack of re-imbursement (medication, rehabilitation, services)
Parents complained that the lack of re-imbursement meant that caregiving imposed a substantial economic burden on caregivers and reduced treatment available (Q7–Q10). They described long waiting lists (Q8), high costs of personal expenditure, including genetic testing (Q9), special foods (Q7) and rehabilitation equipment (Q10).
The disability jurisprudence system
Parents reported problems with the Polish system of disability jurisprudence (Q11–Q14) which was described as being in ‘a deplorable state’ (Q11) and ‘a mockery’ (Q13). They complained at the protracted procedures required to claim disability benefits (Q11) and described ignorance of doctors in the pension commission, who had no knowledge of RDs (Q12, Q14).
Lack of systemic care
Caregivers emphasised that there was no systemic care for RD families (Q15–Q18). They complained at fragmented care and lack of co-ordination between healthcare providers and services (Q15–Q17). While parents criticised the accessibility of health care and social services (Q15–Q18), they descried the system as ‘unsupportive’ and ‘destructive’ (Q15). Some parents therefore left the country (Q18).
Finally, caregivers reported six main unmet needs.
Access to medical treatment
Parents hoped for enhanced accessibility to modern RD treatments (Q19–Q21). In stressing that provision of medical care to CRD is often neglected (Q19) they expressed the wish it would take less time to receive treatment (Q20). They also believed that National Health Fund should cover all costs, including treatment abroad (Q21).
Financial support
Caregivers described difficulties in procurement of medications and healthcare services (Q19–21) and they expressed the need for financial assistance and hoped for re-imbursement for medications, appointments and rehabilitation (Q22). Among other needs they mentioned equipment for rehabilitation, specialised food items (Q22, Q24) and psychological support (Q25).
Respite care and personal assistants for those with disabilities
Parents expressed the wish for much-needed respite care that would enable them to rest and take time for themselves (Q26–Q28). Money was the problem for some caregivers (Q26) and they also wished for personal assistants for those with disabilities, who would support them in the performance of basic daily activities and decisions regarding care (Q28).
Residential care homes for disabled adults
Some caregivers anticipated challenges relating to transitioning from paediatric to adult care and one of the most important supportive care needs was the organisation of residential care homes (Q29–30). Parents hoped that such facilities would provide health care for their growing children (Q29, Q30) and company in order to enable them to live life to the best of their potential (Q30).
Care allowance
Since until recently the right to care benefits in Poland depended on the caregivers’ giving up paid work, parents suggested that it should be legal to receive a care allowance and at the same time take up employment without restrictions (Q31–Q34). They also believed that parents who wish to work should not be deprived of the benefit (Q31, Q32). Caregivers also stressed that benefits stemming from professional activity far outstrip financial income and guarantees better care for their children (Q34, Q35) and emphasised the psychological aspects of work as a coping resource (Q33, Q34).
Discussion
While several previous studies on the experiences of caregivers, namely parents, of CRDs have been conducted in Poland, including Huntington disease32,33,34 or Prader-Willi syndrome35, most often they focuses either on the challenges and needs related to caring for such a child, caregivers’ burden or social functioning of a family whose member experiences RD. However, few data are available on the experiences of CRD caregivers with the healthcare system in Poland20. This study is therefore, one of the few Polish studies that highlights the family caregivers’ interactions with healthcare and social service for CRD. This is of key importance because, while Poland adopted its first Plan for Rare Diseases only recently, it is yet to be implemented this study shows that many parents struggle with the diagnostic and therapeutic odyssey their children face, and feel neglected by the system.
Thus, even though this study shows that some dimensions of healthcare services for CRD were assessed positively, most caregivers reported negative experiences with Polish healthcare system and were dissatisfied with the way it is organized. However, also previous studies demonstrated that although Polish parents of persons with Huntington disease reported many challenges and negative feelings resulting from caregiving, their perception of burden was mostly influenced by negative experiences with the healthcare system, as 9.1% declared having had positive experiences, while almost 42% described their encounters negaively20,32. What is equally important, is that caregivers enrolled in our study also reported difficulties in accessing professional care, complained over lack of resources required for providing care, and expressed the need for support system for CRD families.
While CRD visit doctors more frequently and wait much longer for diagnoses than others17,18,19,20,21,22,23,25,26, they are also several times more likely to be hospitalised, and the average length of their hospitalisation is longer24,25. During hospital stays they also face more difficulties and are more dependent on co-ordinated care involving large, multi-disciplinary teams. Finally, CRD parents report greater reliance on health care, as their children often use a wide variety of primary, secondary and tertiary health services19,20,24,25.
This research confirms that medical dealings for many CRD parents are very confusing, chaotic and expensive, and often become a protracted diagnostic odyssey17,18,19,20,21,22,23,25,26. Libura et al.36 showed, however, that more than 60% of those with RDs in Poland have received at least one misdiagnosis, averaging 3.5 misdiagnoses, and almost one quarter have waited ten or more years for their diagnoses.
Simultaneously, although caregivers enrolled in this survey reported that one of the reasons for this is the lack of access to modern diagnostic techniques that use large-scale genomic testing, they also suggested that such delays are caused by a lack of knowledge about RDs among doctors and other healthcare workers8,17,18,19,20,21,22,23,26,37. This is in line with previous research showing that Polish doctors and nurses have insufficient knowledge of RDs and feels unprepared to deal with patients with RDs37,38. In fact, parents often reported knowing more about their children’s disease than doctors and they were burdened by the necessity to take the role of “expert caregiver”, especially since it was frequently unacknowledged by the patronising healthcare professionals who treated them with little emapthy8,21,25,26. This study also confirms that, when faced with information deficits, poor communication skills and lack of empathy from doctors, most parents sought information from web-based sources22,23,25.
While many caregivers also reported that their children received misdiagnoses or late diagnoses, they also had to consult a number of specialists before the final diagnosis was made20,21,22. This is important because research has demonstrated that the diagnostic odyssey is a great emotional and physical stress for the entire family and may impede adaptation to the disease and the quality of life7,8,9. It also results in unnecessary medication, hospitalisations and uncomfortable and painful treatment, including surgeries that may aggravate the condition of CRD and cause a financial burden17,18,19,20,21,22,23,24,25,26. Teutsch et al.24, for example, demonstrated that, while only 51% of Australian RD families had private health insurance, they spent on average AU$31,000 (US$21,500) annually per child, mainly, on travel costs, medical appointments, medications and medical and assistive equipment. A recent study conducted in France, Germany, Italy, Spain, the UK and the US also estimated the annual direct medical costs in the case of Huntington’s disease at €12,663, indirect medical costs at €2984 and indirect costs at €47,57611. Another study estimated the direct healthcare costs of Dravet syndrome per three months as €6043 ± €5825 per patient. They also suggest that total indirect costs were €4399 ± €4989 in mothers and €391 ± €352 in fathers10.
This study also supports previous research showing that a diagnosis was not always followed by appropriate care8,17,18,20,25,26. While some parents reported being denied treatment for their CRD, most caregivers were ill-informed, either by the specialists or social institutions, about psychosocial care and support available to RD families. While most parents were unaware of psychosocial care services, many reported that there being no such offers available17,20,25. Many caregivers reported that doctors focus mainly on medical care but neglect children’s and caregivers’ emotional and psychosocial needs. Although parents expected practical information on the management of the symptoms and treatment, and socio-legal and organisational issues related to the care allowance and re-imbursement system, they were rarely informed about such offers and did not know whom to turn to for such help. They felt alone in their struggle with the system26 and turned to online-support groups23,25.
Finally, this study confirms that one of the biggest challenges experienced by Polish CRD parents is related to navigating the healthcare and social system8,17,18,19,20,21,22,23,24,25,26,32. Caregivers reported problems in timely diagnoses and access to specialists, as well as their struggle with a lack of co-ordinated care for CRD, and were burdened by the necessity to take on role of co-ordinator of their children’s care8. Since the governmental list of chronic diseases contains only a few RDs, many parents reported problems with socio-legal and organisational care, i.e. access to government support systems and social services. They specified the many challenges to funding for medications, therapy and rehabilitation, which had to be covered from personal funds, denting family finances8,10,19,25. CRD carers therefore felt neglected by the system and described their caregiving as a ‘lonely journey’8,20,23,25,26.
This, research also shows that according to CRD parents Polish healthcare system often focuses on children and clinical dimension of disease, but often neglects caregivers emotional and psychological needs. While most caregivers enrolled in this study complained over lack of psychological support for CRD families, they also emphasized the need for holistic approach towards RD families and stressed that emotional and psychological support should be available to them from the time of diagnosis through entire disease trajectory and should include entire family.
Strength and limitations
The unquestionable strengths of this study are that, since there is scarcity of studies describing the experiences of Polish caregivers of CRD with the healthcare and social services, it helps in identifying actions required from the government, medical and social institutions to improve healthcare for CRD families. Another strength is that it included a large sample of caregivers of children with a variety of (ultra)rare diseases. Since many caregivers acknowledged that this survey gave them the opportunity to be heard for the very first time it might also have a therapeutic value.
This study had, however, some limitations Firstly, while 925 caregivers of 1002 CRD responded, the estimated number of CRD cases in Poland is much higher, so the results cannot be extrapolated to the entire population of caregivers of CRD in the country. Nevertheless, it should be acknowledged that although the first National Plan for Rare Diseases was adopted in Poland in 2021, there is still no registry of persons with RD, and the exact number of paediatric RD patients is unknown. Furthermore, none of the RD foundations, patients’ associations, and organizations involved in the study were able to provide the number of paediatric RD patients with a given condition in Poland. Secondly, since this study was designed as an online survey, there is a risk that it failed to reach caregivers in remote locations with no access to the internet or those who felt uncomfortable using social media platforms and electronic devices. Thirdly, not all caregivers are members of (online) support groups, associations or organisations that helped in the recruitment process. Fourthly, because this survey focussed on experiences of caregivers of children with RDs, the results may be unrepresentative of the experiences of caregivers providing care over adult persons with RD who often face different challenges and express different needs. Fifthly, even though the questionnaire used in this survey was consulted with three external experts in paediatrics, public health and medical sociology and was pre-tested in a pilot study with ten caregivers, it was not validated. A further limitation includes method of qualitative data collection since only one open question was asked without triangulating it against other sources, i.e. caregivers’ interviews or Facebook posts. Moreover, since only 327 participants provided qualitative data there is a potential participation bias related to the possibility that only dissatisfied caregivers shared their experiences by answering additional open question regarding caregivers’ experiences with the health care and social services for CRD. In fact, even though many participants were somehow satisfied with various dimensions of healthcare services for their CRD, of all responses provided only nine were positive, but all of them referred to parents’ perspective on the impact of their child’s disease on caregivers’ personal growth or emotional relationship with CRD, and not to respondents’ experiences with healthcare system. Since only 57 fathers completed the survey there is also a possible gender bias. Lastly, even though qualitative were translated with the help of bilingual translator, still there is a risk of misinterpretation of language nuances inherent in participants’ experiences and that situational context may be lost.
Conclusions
In summary, this study highlights that the diagnostic and therapeutic journey that befalls their children means that CRD parents face many challenges with the healthcare system and express numerous unmet needs. As it shows that there is a urgent need to change our perspective on RDs from cure to family-oriented care, some important policy implications therefore emerged from this study. Although they have been also recommended globally, they are particularly relevant in countries like Poland, where health and social policy for RDs is in progress and national Plan for Rare Diseases is still to be implemented:
-
1.
There is an urgent need for further exploration into challenges and unmet needs described by caregivers that hinder access to health care and social services for their CRD.
-
2.
In particular, in order to assure timely and accurate diagnoses it is crucial to improve and facilitate access to modern diagnostics using large-scale genomic testing.
-
3.
Since health care for CRD is fragmented and lacks co-ordination between medical specialists, healthcare providers and services, there is a need for integrated care for entire RD families that would consist of multidisciplinary team of specialists, including geneticists, neurologists, psychiatrists, dieticians, clinical psychologists, nurses, physiotherapists and speech therapists.
-
4.
To facilitate the management and organisation of care for CRD rare disease co-ordinators, similar to cancer care co-ordinators that were introduced in Poland in 2015, should be organised, so that they would inform, educate and guide RD families through the healthcare system and help to organise an RD person’s care.
-
5.
Although several Polish research and health institutes and clinical hospitals are members of the European Reference Networks (ERNs), including the ERN-RND and the ERN-EYE which are dedicated to rare neurological diseases and rare eye diseases, because due to their rarity and complexity RDs often require extensive consultation, diagnostics and treatment, including surgery, often unavailable in Poland, there is a need to further develop international collaborative actions that enhance the accessibility of cross-border health care.
-
6.
Since obtaining an RD diagnosis has a strong emotional impact on the entire family, tracking their mental health symptoms and supporting families with CRD should be a goal of health care and social services from the time of diagnosis through the entire trajectory of the disease. There is also a need to improve accessibility to patient advocacy and support groups.
-
7.
As well as psychosocial support CRD families require financial support in access to genetic testing, modern medicines, specialised foods, rehabilitation and assistive equipment.
-
8.
As well as the existing education programmes in university curricula in molecular biology, clinical genetics and diagnostics all healthcare professionals should also be trained in genetic testing and counselling to improve their understanding not only of the nature of RDs, but also their psycho-social impact on the family.
-
9.
Healthcare professionals should recognise CRD parents as experts in their children’s disease and in the field of care.
Data availability
The datasets generated during the study are available from the corresponding author on reasonable request.
Abbreviations
- CDR:
-
Children with rare diseases
- RD:
-
Rare disease
References
Nguengang Wakap, S. et al. Estimating cumulative point prevalence of rare diseases: Analysis of the Orphanet database. Eur. J. Hum. Genet. 28(2), 165–173. https://doi.org/10.1038/s41431-019-0508-0 (2020).
Smith, C. I. E., Bergman, P. & Hagey, D. W. Estimating the number of diseases - the concept of rare, ultra-rare, and hyper-rare. iScience 25(8), 104698. https://doi.org/10.1016/j.isci.2022.104698 (2022).
Crooke, S. T. A call to arms against ultra-rare diseases. Nat. Biotechnol. 39(6), 671–677. https://doi.org/10.1038/s41587-021-00945-0 (2021).
Haendel, M. et al. How many rare diseases are there?. Nat. Rev. Drug Discov. 2020(2), 77–78. https://doi.org/10.1038/d41573-019-00180-y (2020).
Fermaglich, L. J. & Miller, K. L. A comprehensive study of the rare diseases and conditions targeted by orphan drug designations and approvals over the forty years of the Orphan Drug Act. Orphanet J. Rare Dis. 18(1), 163. https://doi.org/10.1186/s13023-023-02790-7 (2023).
Mazzucato, M. et al. Estimating mortality in rare diseases using a population-based registry, 2002 through 2019. Orphanet J. Rare Dis. 18(1), 362. https://doi.org/10.1186/s13023-023-02944-7 (2023).
Bonner, N. et al. Rare diseases, are caregivers just as affected as patients?. Value Health 20(9), 562. https://doi.org/10.1016/j.jval.2017.08.928 (2017).
Currie, G. & Szabo, J. “It is like a jungle gym, and everything is under construction”: The parent’s perspective of caring for a child with a rare disease. Child Care Health Dev. 45(1), 96–103. https://doi.org/10.1111/cch.12628 (2019).
Boettcher, J., Boettcher, M., Wiegand-Grefe, S. & Zapf, H. Being the pillar for children with rare diseases. A systematic review on parental quality of life. Int. J. Environ. Res. Public Health 18(9), 4993. https://doi.org/10.3390/ijerph18094993 (2021).
Strzelczyk, A. et al. Burden-of-illness and cost-driving factors in Dravet syndrome patients and carers: A prospective, multicenter study from Germany. Eur. J. Paediatr. Neurol. 23(3), 392–403. https://doi.org/10.1016/j.ejpn.2019.02.014 (2019).
Rodríguez-Santana, I. et al. Economic burden of Huntington disease in Europe and the USA: Results from the Huntington’s disease burden of illness study. Eur. J. Neurol. 30(4), 1109–1117. https://doi.org/10.1111/ene.15645 (2023).
Schieppati, A., Henter, J.-I., Daina, E. & Aperia, A. Why rare diseases are an important medical and social issue. Lancet 371(9629), 2039–2041 (2008).
Héon-Klin, V. European reference networks for rare diseases: What is the conceptual framework?. Orphanet J. Rare Dis. 12(1), 137. https://doi.org/10.1186/s13023-017-0676-3 (2017).
Stawowczyk, E. et al. Reimbursement status and recommendations related to orphan drugs in European countries. Front. Pharmacol. 10, 1279. https://doi.org/10.3389/fphar.2019.01279 (2019).
Hedley, V., Bottarelli, V., Weinman, A. & Taruscio, D. Shaping national plans and strategies for rare diseases in Europe: Past, present, and future. J. Community Genet. 12(2), 207–216. https://doi.org/10.1007/s12687-021-00525-4 (2021).
Ministerstwo Zdrowia. 2021. Uchwała nr 110 Rady Ministrów z dnia 24 sierpnia 2021 r. w sprawie przyjęcia dokumentu Plan dla Chorób Rzadkich. https://isap.sejm.gov.pl/isap.nsf/download.xsp/WMP20210000883/O/M20210883.pdf. Accessed 2 Dec 2023.
Anderson, M., Elliott, E. J. & Zurynski, Y. A. Australian families living with rare disease: Experiences of diagnosis, health services use and needs for psychosocial support. Orphanet J. Rare Dis. 8, 22. https://doi.org/10.1186/1750-1172-8-22 (2013).
Black, N., Martineau, F. & Manacorda, T. 2015. Diagnostic odyssey for rare diseases: exploration of potential indicators. Policy Innovation Research Unit. http://piru.lshtm.ac.uk/assets/files/Rare%20diseases%20Final%20report.pdf. Accessed 30 Nov 2023.
Carmichael, N., Tsipis, J., Windmueller, G., Mandel, L. & Estrella, E. “Is it going to hurt?”: The impact of the diagnostic odyssey on children and their families. J. Genet. Couns. 24(2), 325–335. https://doi.org/10.1007/s10897-014-9773-9 (2015).
Domaradzki, J. Family caregivers’ experiences with healthcare services - a case of Huntington disease. Psychiatr. Pol. 50(2), 375–391. https://doi.org/10.12740/PP/59103 (2016).
Bauskis, A., Strange, C., Molster, C. & Fisher, C. The diagnostic odyssey: Insights from parents of children living with an undiagnosed condition. Orphanet J. Rare Dis. 17(1), 233. https://doi.org/10.1186/s13023-022-02358-x (2022).
Llubes-Arrià, L. et al. Emotional experience of the diagnostic process of a rare disease and the perception of support systems: A scoping review. J. Clin. Nurs. 31(1–2), 20–31. https://doi.org/10.1111/jocn.15922 (2022).
Ashtari, S. & Taylor, A. D. The Internet knows more than my physician: Qualitative interview study of people with rare diseases and how they use online support groups. J. Med. Internet Res. 24(8), e39172. https://doi.org/10.2196/39172 (2022).
Teutsch, S. et al. Australian children living with rare diseases: health service use and barriers to accessing care. World J. Pediatr. 19(7), 701–709. https://doi.org/10.1007/s12519-022-00675-6 (2023).
Witt, S., Schuett, K., Wiegand-Grefe, S., Boettcher, J. & Quitmann, J. Living with a rare disease - experiences and needs in pediatric patients and their parents. Orphanet J. Rare Dis. 18(1), 242. https://doi.org/10.1186/s13023-023-02837-9 (2023).
Baumbusch, J., Mayer, S. & Sloan-Yip, I. Alone in a crowd? Parents of children with rare diseases’ experiences of navigating the healthcare system. J. Genet. Couns. https://doi.org/10.1007/s10897-018-0294-9 (2018).
Nowak, J. K. & Walkowiak, J. Study designs in medical research and their key characteristics. J. Med. Sci. 92(4), e928. https://doi.org/10.20883/medical.e928 (2024).
Sawicka-Gutaj, N. et al. Publication ethics of human studies in the light of the Declaration of Helsinki – a mini-review. J. Med. Sci. 91(2), e700. https://doi.org/10.20883/medical.e700 (2022).
Glaser, B.G., Strauss, A.L. The discovery of grounded theory: Strategies for qualitative research. 4th edn. Aldine (2009).
Fereday, J. & Muir-Cochrane, E. C. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int. J. Qual. Methods 5(1), 80–92. https://doi.org/10.1177/160940690600500107 (2006).
Chapman, A. L., Hadfield, M. & Chapman, C. J. Qualitative research in healthcare: An introduction to grounded theory using thematic analysis. J. R. Coll. Phys. Edinb. 45(3), 201–205. https://doi.org/10.4997/jrcpe.2015.305 (2015).
Domaradzki, J. Caring for patients with Huntington disease – a survey of caregivers’ experiences and views. J. Pre Clin. Clin. Res. 9(2), 133–139. https://doi.org/10.5604/18982395.1186494 (2015).
Bartoszek, A. et al. Exploring the reliability and validity of the Huntington’s disease quality of life battery for carers (HDQoL-C) within a polish population. Int. J. Environ. Res. Public Health 16(13), 2323. https://doi.org/10.3390/ijerph16132323 (2019).
Modrzejewska-Zielonka, E. et al. Huntington’s disease progression and caregiver burden. Eur. Neurol. 85(5), 398–403. https://doi.org/10.1159/000524146 (2022).
Kowal, K., Skrzypek, M. & Kocki, J. Experiencing illness as a crisis by the caregivers of individuals with Prader-Willi syndrome. PLoS One 17(9), e0273295. https://doi.org/10.1371/journal.pone.0273295.4 (2022).
Libura, M. et al. Choroby rzadkie w Polsce: Stan obecny i perspektywy. Uczelnia Łazarskiego (2016).
Walkowiak, D. & Domaradzki, J. Are rare diseases overlooked by medical education? Awareness of rare diseases among physicians in Poland: An explanatory study. Orphanet J. Rare Dis. 16, 400. https://doi.org/10.1186/s13023-021-02023-9 (2021).
Walkowiak, D. & Domaradzki, J. Needs assessment study of rare diseases education for nurses and nursing students in Poland. Orphanet J. Rare Dis. 15, 167. https://doi.org/10.1186/s13023-020-01432-6 (2020).
Acknowledgements
We thank all caregivers who gave their valuable time to share their experiences and completed the survey. We also thank representatives of RD foundations, patients’ associations and organisations for their assistance in recruiting families via their webpages and Facebook: achromatopsja.pl, Alkaptonuria, Blackfan Diamond Anemia Polska, Choroba Gauchera, Chorzy na rdzeniowy zanik mięśni (SMA), Cri du Chat Polska, Delecja 18q. Zespół de Grouchy’ego, Dolnośląskie Koło Przyjaciół Dzieci z Fenyloketonurią, DRAVET.PL – Grupa wspierająca rodziców i opiekunów, Dystrofia Mięśniowa Duchenne’a, Forum Sarkoidoza – Poland, FOXG1 syndrome Poland, Fundacja MATIO, Fundacja Parent Project Muscular Dystrophy, Fundacja Pomocy Chorym na Zanik Mięśni, Fundacja Pomocy Chorym na Zanik Mięśni im. Piotra Karlińskiego, Fundacja Saventic – choroby rzadkie, Fundacja SMA, glikogenoza, Grupa wsparcia dla chorych na stwardnienie rozsiane i ich bliskich, Grupa wsparcia dla osób z Chorobą Fabry’ego, Hemofilia Polska – Polskie Stowarzyszenie Chorych na Hemofilię, Jesteśmy Pod Ścianą Foundation, Małe Fenylaki, Mowat-Wilson syndrome Polska, Mukowiscydoza, Najrzadsze i rzadkie choroby genetyczne świata – Grupa Wsparcia, Ogólnopolskie Stowarzyszenie Pomocy Osobom z Zespołem Retta, Polskie Stowarzyszenie Pomocy Osobom z Zespołem Pradera-Williego, Polskie Towarzystwo Chorób Nerwowo-Mięśniowych, Rodzice dzieci z CZD, Rodzice niepełnosprawnych dzieci – dyskusja na każdy temat, Rodzinamuko, Rzadkie choroby metaboliczne – grupa wsparcia, Specjaliści, Lekarze, Terapeuci, Rodzice – Zespół Coffin-Siris, Stowarzyszenie Chorych na Mukopolisacharydozę (MPS) i Choroby Rzadkie, Stowarzyszenie Ehlers-Danlos Polska, Stowarzyszenie Marfan Polska, Stowarzyszenie na Rzecz Dzieci z Zaburzeniami Genetycznymi GEN, Stowarzyszenie Osób z Wrodzoną Łamliwością Kości (O.I) – Polska, Stowarzyszenie Rodzin z Chorobą Fabry’ego, Stowarzyszenie Rodzin z Chorobą Gauchera, Stowarzyszenie Zespołu Williamsa, Stowarzyszenie 22q11 Polska, Stwardnienie guzowate TSC, Syndrom Collins’a Treachera w Polsce, Wrodzona łamliwość kości, Wyjątkowa dziewczynka – Zespół Kabuki, Wyjątkowi! Wady i choroby genetyczne, Zespół Churga-Strauss ZChS – Polska, Zespół Jouberta, Zespół KABUKI Niikawa-Kuroki POLSKA, Zespół Klinefeltera – grupa wsparcia dla dorosłych i rodziców dzieci z ZK, Zespół Noonan – wyjątkowe dzieci = nasze Noonanki, Zespół Silvera-Russella, Zespół Smith-Magenis Polska, Zespół Sotosa Polska, Zespół Turnera – Wyjątkowe Dziewczynki – Kobiety, Zespół Wolfa-Hirschhorna, Choroba Wilsona, Ziarniniak Wegenera. Finally, we would like to express our gratitude to Mr. Robert France for his assistance with the language editing of the manuscript.
Author information
Authors and Affiliations
Contributions
JD conceptualised and supervised the study. JD and DW designed the study, had full access to all data in the study and prepared the tables. JD collected and analysed the data, conducted the literature search and drafted the manuscript for publication. Both authors approved the final draft and accept the responsibility for submitting it for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Domaradzki, J., Walkowiak, D. Invisible patients in rare diseases: parental experiences with the healthcare and social services for children with rare diseases. A mixed method study. Sci Rep 14, 14016 (2024). https://doi.org/10.1038/s41598-024-63962-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-63962-4
- Springer Nature Limited