Abstract
Coronary artery disease is a leading cause of morbidity and mortality worldwide. It occurs due to a combination of genetics, lifestyle, and environmental factors. Premature coronary artery disease (PCAD) is a neglected clinical entity despite the rising number of cases worldwide. This study aimed to investigate the risk factors of premature coronary artery disease. In this study, we searched articles that had studied the risk factors of premature coronary artery diseases from January 2000 to July 2022 in Saudi Arabia in Web of Science, Pub Med, Scopus, Springer, and Wiley databases. The final analysis is based on seven articles. The smoking prevalence was 39%, diabetes mellitus 41%, hypertension 33%, overweight and obesity 18%, family history of coronary artery disease (CAD) 19%, dyslipidemia 37%, and the prevalence range of low-density lipoprotein cholesterol was 33.8–55.0%. The results revealed a mortality prevalence of 4% ranging from 2 to 8% which is similar to the prevalence in older patients which was 2–10%. Smoking, diabetes mellitus, hypertension, family history of CAD, dyslipidemia, and overweight/obesity are significantly and positively associated with premature coronary artery diseases. The health authorities should design and implement an intensive and effective prophylactic plan to minimize the subsequent impact of PCAD on the young population. In addition, early diagnosis of PCAD has great value in providing timely treatment, managing the patients, and minimizing the burden of the disease.
Similar content being viewed by others
Introduction
An alarming estimate by health organizations and authorities shows that cardiovascular diseases (CVD) might be the leading cause of death worldwide in 20301,2. Around one-third of the mortality rate globally in 2020 was due to cardiovascular diseases3,4. Although Coronary artery diseases (CAD) are expected to occur more frequently in the elderly population, recent reports highlighted that 10% of patients less than 45 years old are also affected by CAD5. This is called Premature coronary artery disease (PCAD) which occurs below the age of 45 to 55 years6,7.
In North America, an increase in the incidence of Myocardial infarction (MI) was observed in younger patients recently8,9. The increase in the incidence of myocardial infarction was the consequence of predisposing risk factors leading to premature coronary artery diseases. Some of these risk factors are common with coronary artery disease (CAD) affecting the elderly populations as well as premature coronary artery disease while others are not10.
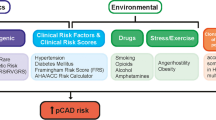
Several traditional risk factors have been identified to be associated with premature coronary artery diseases including smoking, physical inactivity, overweight/obesity, metabolic disorders, diabetes mellitus, and hypertension while multiple nontraditional risk factors including heterozygous familial hypercholesterolemia (HeFH), inflammation, prothrombotic states and ethnicity11. Early detection and identification of risk factors are of great value in reducing the impact of premature coronary artery diseases and their consequences.
Worldwide, CAD is the most common cause of mortality and loss of Disability Adjusted Life Years (DALYs), and the burden falls in low and middle-income countries. CAD caused about 7 million deaths and 129 million DALYs annually12. In 2015 CAD accounted for 8.9 million deaths and 164.0 million DALYs. PCAD is a leading public health challenge resulting in years of productive life loss and an intensifying burden on health systems13,14.
In Saudi Arabia, it has been found that admitted patients with acute coronary syndrome (ACS) were 10 years younger than similar patients in other countries and were mostly diabetic or hypertensive15,16,17. We aimed in this systematic review and meta-analysis to evaluate the prevalence of various premature coronary artery disease risk factors in Saudi Arabia. This systematic review and meta-analysis will help health authorities design prophylactic strategies against a hidden threat to protect the younger population.
Methods
Data search strategy
The studies were searched from the Web of Science, PubMed, Scopus, Springer, and Wiley databases from January 2000 to July 2022. The specific keywords have been used in the search strategy in different combinations: “coronary artery disease,” “coronary heart disease,” “vascular disease,” “atherosclerosis,” “smoking”, “diabetes mellitus”, “risk factors,” and “Saudi Arabia.” We assigned two co-authors to evaluate the literature by excluding irrelevant articles by reading the titles and abstracts. In addition, if any unclear abstracts correlated to our objectives, the full article was retrieved and studied thoroughly. After exclusion, the remaining relevant articles were evaluated by another co-author for final eligibility.
Inclusion and exclusion criteria
Any Studies that evaluate patients with PCAD or compare PCAD to healthy subjects in Saudi Arabia. The cut-off age of Premature coronary disease is different according to various studies but mostly mention less than 45 and 55 years6,7. All articles published were in the English language. The duplicate studies, brief communications, case reports, letters to editors, and systematic reviews, were excluded from the study.
Data extraction
Information from the eligible articles, after filtration, was arranged in a table (Table 1). The information from each article was: first author, sample size, age of patients, study design, and outcomes. The prevalence of traditional and nontraditional was extracted from eligible studies including smoking, hypertension, diabetes mellitus, dyslipidemia, family history of CAD, obesity, and drug abuse.
Quality assessment of the studies
The Newcastle–Ottawa Scale (NOS), Table 2, which assesses selection bias, comparability of exposed and control participants, and outcome evaluation, was used to evaluate the quality of non-randomized research. Each criterion was given a star rating of 1 or 0 stars. For observational studies, the overall star rating ranged from 0 to 9 stars. The NOS instrument assesses three areas: study group selection (maximum 4 stars); study group comparability (maximum 2 stars), and outcome assessment (max 3 stars). The quality was evaluated independently by two authors, and disagreements were settled by discussion. A study with a score of 7–9 or 10 is good quality, a score of 4–6 is fair quality, and a score of 0–3 is poor quality.
Table 2 summarizes the quality assessment scores for the included studies. Five studies scored three stars. For the remaining studies, the reasons for not receiving a full quality score for the selection section were that there was no demonstration that the outcome of interest was not present at the start of the study or that the control group was not selected from the general community. Five studies controlled the outcomes and for additional factors (e.g., age), so they scored two stars, while 2 studies controlled the outcomes and scored only one star. All studies reported the ascertainment of the outcome, but they did not describe the follow-up period, so they scored only one star.
Statistical analysis
The statistical evaluations were carried out utilizing the Comprehensive Meta-Analysis version 3 (Biostat Inc. USA). The prevalence of different risk factors was calculated along with a 95% confidence interval. The significance level was established at a p-value less than 0.05. The Cochrane chi-squared test was used to assess article heterogeneity; a P value of 0.05 or higher indicates the presence of heterogeneity. I2 value was calculated to determine the effect of heterogeneity on the meta-analysis. The pooled studies did exhibit moderate to high levels of heterogeneity, as indicated by I2 values > 50% and P < 0.05. If I2 < 50% and P > 0.05, a fixed-effects design was used; otherwise, a random-effects design was utilized. To evaluate the robustness of this meta-analysis, a sensitivity analysis was conducted. Egger’s test was conducted to evaluate publication bias. This latter was further assessed by the visual inspection of the symmetry in funnel plots.
Results
Initial 32606 articles were screened. 32583 articles, then, were excluded by reading the title and abstract. The excluded studies involved the following: Unrelated articles, litter to editors, congress articles, review articles, systematic reviews, and case reports. The remaining 23 full‐text articles were further examined in depth for eligibility. Finally, 7 articles were eligible to be included. Figure 1 shows the flow chart that was followed for eligibility according to the PRISMA guidelines17. Table 1 illustrates the characteristics of the studies that were included in the systematic review; two of the studies were retrospective case-control studies, two retrospective studies, two case-control studies, and one cross-sectional study. All the studies were from patients presenting to hospitals18,19,20,21,22,23,24.
Prevalence of risk factors
The prevalence range percentage of risk factors are shown in table 3. Seven studies mentioned smoking as a risk factor for PCAD in Saudi Arabia18,19,20,21,22,23,24. The range of smoking prevalence was from 29 to 52%.
Seven studies mentioned DM as a risk factor for PCAD in Saudi Arabia18,19,20,21,22,23,24. The range of DM prevalence was from 34 to 49%.
Seven studies mentioned hypertension as a risk factor for PCAD in Saudi Arabia. The range of hypertension prevalence was from 24 to 45%. One study reported hypertension prevalence of patients less than 40 years was 28%24.
Two studies reported overweight and obesity as risk factors for PCAD in Saudi Arabia18,22. The range of overweight and obesity prevalence was from 5 to 62%.
Four studies reported a family history of PCAD as a risk factor for PCAD in Saudi Arabia19,20,22,23. The family history of CAD prevalence ranged from 7 to 49%.
Two studies reported Drug abuse and Amphetamine-type stimulants (ATS) as a risk factor for PCAD in Saudi Arabia21,22. One study mentioned drug abuse in general as a risk factor with a prevalence of 3.0%22 while another study specified Amphetamine-type stimulants (ATS) as a risk factor with a prevalence of 5.8%21.
The different studies have mentioned various cutoff points in defining hypercholesterolemia. levels of total cholesterol > 5.2 mmol/L and > 6.2 mmol/L were used as a cutoff point25,26.
Four studies reported dyslipidemia in general as a risk factor for PCAD in Saudi Arabia18,22,23,24. The range of dyslipidemia prevalence was from 22 to 60%. One study reported dyslipidemia prevalence in patients less than 40 years was 32% and from 41 to 55 years was 39%24.
Two studies reported increased Low‐density lipoprotein cholesterol (LDL) as a risk factor for PCAD in Saudi Arabia19,20. The range of Low‐density lipoprotein cholesterol (LDL) prevalence was from 33.8 to 55.0%. Only one study mentioned decreased High‐density lipoprotein cholesterol (HDL) as a risk factor for PCAD in Saudi Arabia20. The prevalence was 52.8%. One study mentioned Hypertriglyceridemia as a risk factor for PCAD in Saudi Arabia20, and the prevalence was 7.7%. The present study results showed a mortality prevalence ranging from 0 to 9.2% which is similar to the prevalence in older patients from 2 to 10%18,19,20,21,22,23,24.
Smoking
All studies reported the prevalence of smoking among patients with PCAD. The heterogeneity (Chi2 = 7295.69, p < 0.00001, I2= 100%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 39% (95% CI 29–52%) (Figure 2).
Diabetes mellitus
All studies reported the prevalence of DM among patients with PCAD. The heterogeneity (Chi2 = 37.60, P < 0.00001, I2 = 79%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 41% (95% CI 34–49%) (Figure 3).
Hypertension
All studies reported the prevalence of hypertension among patients with PCAD. The heterogeneity (Chi2 = 125.70, p < 0.0001, I2 = 93%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 33% (95% CI 24–45%) (Figure 4).
Overweight and obesity
Two studies reported the prevalence of overweight and obesity among patients with PCAD. The heterogeneity (Chi2 = 121.41, p < 0.00001, I2 = 98%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 18% (95% CI 5–62%) (Figure 5).
Family history of coronary artery disease (CAD)
Three studies reported the prevalence of family history of CAD among patients with PCAD. The heterogeneity (Chi2 = 148.13, p < 0.00001, I2 = 98%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 19% (95% CI 7–49%) (Figure 6).
Dyslipidemia
Three studies reported the prevalence of dyslipidemia among patients with PCAD. The heterogeneity (Chi2 = 25.37, p < 0.00001, I2 = 88%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 37% (95% CI 22–60%) (Figure 7).
Mortality
Three studies reported the prevalence of mortality among patients with PCAD. The heterogeneity (Chi2 = 112.84, p < 0.00001, I2 = 96%) was high, so a random effect model was used. The forest plot analysis showed a pooled estimated prevalence of 4% (95% CI 2–8%) (Figure 8).
Discussion
Coronary artery disease is a leading cause of morbidity and mortality worldwide. Premature coronary artery diseases have been correlated with multiple risk factors worldwide. Some of these factors are due to a sedentary lifestyle while some are genetically predisposed risk factors (modifiable and non-modifiable risk factors)27,28,29,30,31. Epidemiological data about Premature coronary artery diseases in Saudi Arabia are limited. To our surprise was the observation that although there is a long list of nontraditional risk factors significantly contributing to increased cardiovascular risk at younger ages, we did not find any report addressing the magnitude of these factors in PCAD. The list includes a group of factors that are categorized into lipid, inflammatory and prothrombotic markers.
To the best of our knowledge, this meta-analysis is the first to systematically identify several risk factors associated with PCAD, some are traditional while others are not, with a high prevalence of smoking, dyslipidemia, obesity, diabetes, and hypertension. There is a lack of studies correlating risk factors and PCAD in the Middle East. Therefore, we compared our findings with North American studies regarding PCADs.
Around 5–10 % of all acute myocardial infarction (AMI) cases occur in patients less than 45 years32,33. The percentages in Middle East countries are higher (11%) than in Western Europe (2.7%), North America (4%), and Africa (9%)34,35. Different types of smoking have been introduced and they are available in the market including traditional smoking, electronic smoking, and pipe (Shisha smoking). As a primary risk factor, smoking plays a major role in premature coronary atherosclerosis and in accelerating atherosclerosis by increasing the oxidation of low-density lipoprotein (LDL) and damaging coronary endothelial vasodilation36. In this context, many studies revealed that smoking was significantly associated with an increased risk of PCAD compared to a healthy population37.
In this meta-analysis, we analyzed 7 studies. The pooled estimated prevalence of smoking was 39% among Saudi patients, which is way lower than in USA patients with PCAD (60.8%)38. In addition, it is lower than what was reported in a study conducted in the United Arab Emirates, which reported a high prevalence of smoking associated with PCAD (70–90%)39. These dismal results need to be well evaluated by higher authorities to find solutions to this issue.
International Diabetic Federation (IDF) declared that the diabetes prevalence among Saudi adults is 17.6% which is considered one of the highest rates worldwide40. We found that the pooled estimated prevalence of diabetes among PCAD patients was 41% while diabetes prevalence in USA PCAD patients was lower (23.8%)38. Nevertheless, diabetes prevalence in PCAD patients was lower than in those with CAD (52–62%)18,19,22. It was reported that patients with diabetes have a two- to four-fold higher risk of developing coronary disease than people without diabetes41.
Indeed, diabetic patients exhibit an increased risk for the development of atherosclerotic CAD for many reasons, including metabolic factors, like hyperglycemia, dyslipidemia, and insulin resistance, which lead to endothelial cell, vascular smooth muscle dysfunction, impaired platelet function and abnormal coagulation42.
Our meta-analysis showed that the pooled estimated prevalence of hypertension in PCAD was 33% which is lower than the prevalence in the USA (52.8%)38 and the prevalence in CAD patients (36–68.7%)18,19,22. This could be due to arteriosclerosis (age-related disease) which increased the prevalence in older patients. High blood pressure can lead to CAD due to the added force on the artery walls. Over time, this can damage these blood vessels and lead to more plaque buildup. The narrowed artery limits or blocks the flow of blood to the heart muscle, which means it might not get enough oxygen43.
Based on two studies, the pooled estimated prevalence of overweight and obesity was 18%. In comparison to a study performed in the USA, they found that obesity (BMI > 30 kg/m2) prevalence in PCAD was 47.1% which is higher than what we found38.
In our study, the pooled estimated prevalence of a family history of CAD was 19%. In the USA, the prevalence was 39.8% which is higher than our findings38. This could be due to ethnic differences between the two populations. On the other hand, the prevalence of a family history of PCAD was higher than those with CAD (0.5–9.4%)19,22. These results highlight the importance of genetic and biomarker studies to understand the underlying mechanism.
Regarding dyslipidemia, the pooled estimated prevalence was around 37% which is lower than what was reported in the USA population (46.4%)38. These results suggest the need for extensive studies in predisposing genetic factors affecting lipid profiles. Nevertheless, lifestyle cannot be overlooked as an important contributor in this regard due to the high prevalence of physical inactivity and sedentary lifestyle in our region (overall prevalence of physical inactivity was 32.3%, and even higher in women 35.5%)44. Another systematic review in Saudi Arabia reported a worrying prevalence of physical inactivity in women ranging from 53.2 to 98.1%45.
The prevalence of drug abuse in PCAD was from 3.0 to 5.8%21,22. In a study performed in the USA detecting the correlation between Substance abuse and premature atherosclerotic cardiovascular diseases, they found a prevalence of alcohol was 31.8%, cocaine at 12.9%, amphetamine at 2.9%, and cannabis at 12.5%46. Thus, regarding amphetamine, our results are higher than those found in the USA which is a warning sign to be carefully considered.
Regarding mortality rate, the astonishing findings show that our results showed an estimated pooled prevalence of 4% (2–8%), which is similar to the prevalence in older patients (2–10%)18,19,20,21,22,23,24. This result should be the focus of extensive research, as well as legislators’ concerns.
In this regard, one cannot neglect the gender differences in risk factors in CAD or PCAD patients which need to be extensively evaluated. Last but not least, we found recently a high prevalence of lack of knowledge and unhealthy lifestyle practices of PCAD and its risk factors among the Saudi population where more intervention and awareness of health care providers to reduce its detrimental impact is of great value47.
Strengths and limitations
In the present study, we performed a search in major databases. The main strong item of this article is the fair quality of the included studies. Although unpublished articles and local articles published in non-indexed journals have not been included in our study, the funnel plots did not show a publication bias. Furthermore, the main findings were validated by sensitivity analysis, which demonstrated the strong reliability of this meta-analysis.
One of the main difficulties is the large differences between studies in design, as well as in the cutoff point of risk factors. These differences present a significant limitation when comparing the results of different studies and consequently make pooled analysis more complicated. Hence, considerable heterogeneity, which is expected in meta-analysis studies, can alter the interpretability of results. Consequently, the findings of the present work must be analyzed with attentiveness. In addition, the lack of extensive and controlled studies was a limiting factor. Furthermore, a lack of studies concerning genetic differences as well as biomarkers affecting PCAD was also noticed. Also, all the eligible studies that have been included did not differentiate between males and females regarding risk factors that need to be considered in future studies. Also, none of the studies mentioned the occupation of the patients which we believe is an important risk factor that might contribute to premature coronary artery disease.
Conclusions
The majority of the patients with premature coronary artery disease in Saudi Arabia are smokers, have dyslipidemia, diabetic and are overweight/obese. Smoking, diabetes mellitus, hypertension, family history of CAD, dyslipidemia, and overweight/obesity are significantly and positively associated with premature coronary artery diseases in Saudi Arabia. The other risk factors such as drug abuse and hypertriglyceridemia are associated with PCAD but to a lesser extent. We found an alarmingly high mortality rate of PCAD similar to CAD. The health authorities should design and implement an intensive and effective prophylactic plan to minimize the subsequent impact of PCAD on the young population. In addition, early diagnosis of PCAD has great value in providing timely treatment, managing the patients, and minimizing the burden of the disease.
Data availability
The data may be provided on reasonable request to the corresponding author.
References:
World Health Organization. A Vital Investment. World Health 2005; 202.
Beaglehole, R. & Bonita, R. Global public health: A scorecard. Lancet 372, 1988–1996 (2008).
Mathers, C. D. & Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(2011–2030), e442 (2006).
WHO|cardiovascular diseases (CVDs). World Health Organization; Available at: http://www.who. int/mediacentre/factsheets/f s317/en/.
Mohammad, A., Jehangeer, H. & Shaikhow, S. Prevalence, and risk factors of premature coronary artery disease in patients undergoing coronary angiography in Kurdistan, Iraq. BMC Cardiovasc. Disord. 15(1), 155 (2015).
Achari, V. & Thakur, A. Association of major modifiable risk factors among patients with coronary artery disease–a retrospective analysis. JAPI 52, 103–108 (2004).
Panwar, R. B. et al. Atherothrombotic risk factors & premature coronary heart disease in India: A case-control study. Indian J. Med. Res. 134(1), 26–32 (2011).
Arora, S. et al. Twenty-year trends, and sex differences in young adults hospitalized with acute myocardial infarction: The ARIC community surveillance study. Circulation 139, 1047–1056 (2019).
Gupta, A. et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 64, 337–345 (2014).
El-Aziz, T., Hussein, Y. M., Mohamed, R. H. & Shalaby, S. M. Renin–angiotensin system genes polymorphism in Egyptians with premature coronary artery disease. Gene. 498(2), 270–275 (2012).
Collet, J.-P. et al. Long-term evolution of premature coronary artery disease. J Am Coll Cardiol. 74, 1868–1878 (2019).
Vedanthan, R., Seligman, B. & Fuster, V. Global perspective on acute coronary syndrome: a burden on the young and poor. Circ Res. 114, 1959–1975. https://doi.org/10.1161/CIRCRESAHA.114.302782 (2014).
Ralapanawa, U. & Sivakanesan, R. Epidemiology and the Magnitude of Coronary Artery Disease and Acute Coronary Syndrome: A Narrative Review. J Epdemiol. Glob. Health. 11(2), 169–177. https://doi.org/10.2991/jegh.k.201217.001 (2021).
Zhang, G. et al. Burden of ischaemic heart disease and attributable risk factors in China from 1990 to 2015: Findings from the global burden of disease 2015 study. BMC Cardiovasc. Disord. 18, 18. https://doi.org/10.1186/s12872-018-0761- (2018).
Soofi, M. & Youssef, M. Prediction of 10-year risk of hard coronary events among Saudi adults based on the prevalence of heart disease risk factors. J. Saudi Heart Assoc. 27(3), 152–159 (2015).
Alhabib, K. F. et al. Baseline characteristics, management practices, and in-hospital outcomes of patients with acute coronary syndromes: Results of the Saudi project for assessment of coronary events (SPACE) registry. J. Saudi Heart Assoc. 23(4), 233–239 (2011).
Simera, I., Moher, D., Hoey, J., Schulz, K. & Altman, D. A catalogue of reporting guidelines for health research. Eur. J. Clin. Invest. 40(1), 35–53 (2010).
Al-Murayeh, M., Al-Masswary, A., Dardir, M., Moselhy, M. & Youssef, A. Clinical presentation, and short-term outcome of acute coronary syndrome in native young Saudi population. J. Saudi Heart Assoc. 24(3), 169–175 (2012).
Al-Shahrani, M. et al. Differences in clinical nature and outcome among young patients suffering from an acute coronary syndrome. J. Blood Med. 2(12), 1011–1017 (2021).
Al-Khadra, A. Clinical profile of young patients with acute myocardial infarction in Saudi Arabia. Int. J. Cardiol. 91(1), 9–13 (2003).
Alghamdi, M., Alqahtani, B. & Alhowti, S. Cardiovascular complications among individuals with amphetamine-positive urine drug screening admitted to a tertiary care hospital in Riyadh. J. Saudi Heart Assoc. 28(3), 129–135 (2016).
Sakr, H. et al. Clinical profiles, and outcomes of acute ST-segment elevation myocardial infarction in young adults in a tertiary care centre in Saudi Arabia. Saudi Med. J. 42(11), 1201–1208 (2021).
Abazid, R. et al. Visceral adipose tissue influences coronary artery calcification in young and middle-aged groups using computed tomography angiography. Avicenna J. Med. 5(3), 83–88 (2015).
Al-Saif, S. et al. Age and its relationship to acute coronary syndromes in the Saudi Project for Assessment of Coronary Events (SPACE) registry: The SPACE age study. J. Saudi Heart Assoc. 24(1), 9–16 (2012).
Al-Kaabba, A. et al. Prevalence and correlates of dyslipidemia among adults in Saudi Arabia: Results from a national survey. J. Endocr. Metab. Dis. 2(4), 89–97 (2012).
Basulaiman, M. et al. Hypercholesterolemia and its associated risk factors of Saudi Arabia, 2013. Ann. Epidemiol. 24(11), 801–808 (2014).
Cho, S. et al. The additive value of multiple biomarkers in the prediction of premature coronary artery disease. Acta Cardiol. 70(2), 205–210 (2015).
Upadhyay, R. K. Emerging risk biomarkers in cardiovascular diseases and disorders. J. Lipids. 2015, 971453 (2015).
Montgomery, J. & Brown, J. Metabolic biomarkers for predicting cardiovascular disease. Vasc. Health Risk Manag. 9, 37 (2013).
Rubin, J. & Borden, W. Coronary heart disease in young adults. Curr. Atherosler. Rep. 14(2), 140–149 (2012).
Alkhawam, H. et al. Coronary artery disease in Young Adults. Am. J. Med. Sci. 350(6), 479–483 (2015).
Egred, M., Viswanathan, G. & Davis, G. K. Myocardial infarction in young adults. Postgrad. Med. J. 81, 741–745 (2005).
Tuzcu, E. et al. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: Evidence from intravascular ultrasound. Circulation 103, 2705–2710 (2001).
Gehani, A. et al. Association of risk factors with acute myocardial infarction in Middle Eastern countries: The INTERHEART Middle East study. Eur. J. Prev. Cardiol. 21, 400–410 (2014).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 364, 937–952 (2004).
Barua, R. S., Ambrose, J. A., Srivastava, S., DeVoe, M. C. & Eales-Reynolds, L. J. Reactive oxygen species are involved in smoking-induced dysfunction of nitric oxide biosynthesis and upregulation of endothelial nitric oxide synthase: An in vitro demonstration in human coronary artery endothelial cells. Circulation 107(18), 2342–2347. https://doi.org/10.1161/01.CIR.0000066691.52789.BE (2003).
Poorzand, H. et al. Risk factors of premature coronary artery disease in Iran: A systematic review and meta-analysis. Eur. J. Clin. Invest. 49(7), e13124. https://doi.org/10.1111/eci.13124 (2019).
Zeitouni, M. et al. Risk factor burden and long-term prognosis of patients with premature coronary artery disease. J. Am. Heart Assoc. 9(24), e017712 (2020).
Jamil, G. et al. Risk factor assessment of young patients with acute myocardial infarction. Am. J. Cardiovasc. Dis. 3, 170–174 (2013).
IDF. IDF Middle East and North Africa Region, 2015, http://www.idf.org/membership/mena/saudi-arabia.
Ali, M. K., Narayan, K. M. & Tandon, N. Diabetes & coronary heart disease: Current perspectives. Indian J. Med. Res. 132(5), 584–97 (2010).
Al-Nozha, M. M., Ismail, H. M., Al, O. M. & Nozha,. Coronary artery disease and diabetes mellitus. J. Taibah Univ. Med. Sci. 9(10), 330–338 (2016).
Rosendorff, C. Hypertension and coronary artery disease: A summary of the American Heart Association scientific statement. J. Clin. Hypertens (Greenwich). 9(10), 790–795. https://doi.org/10.1111/j.1751-7176.2007.tb00006.x (2007).
Kahan, D. Adult physical inactivity prevalence in the Muslim world: Analysis of 38 countries. Prev. Med. Rep. 2, 71–75 (2015).
Alshaikh, M., Filippidis, F., Baldove, J., Majeed, A. & Rawaf, S. Women in Saudi Arabia, and the prevalence of cardiovascular risk factors: A systematic review. J. Environ. Public Health 2016, 7479357 (2016).
Mahtta, D. et al. Recreational substance use among patients with premature atherosclerotic cardiovascular disease. Heart 107(8), 650–656 (2021).
Al-Khlaiwi, T. et al. High prevalence of lack of knowledge and unhealthy lifestyle practices regarding premature coronary artery disease and its risk factors among the Saudi population. BMC Public Health 23(1), 908. https://doi.org/10.1186/s12889-023-15834-1 (2023).
Acknowledgements
We thank the Researchers Supporting Project number (RSP-2024 R47), King Saud University, Riyadh, Saudi Arabia.
Funding
King Saud University, Riyadh, Saudi Arabia (RSP-2024 R47).
Author information
Authors and Affiliations
Contributions
T.A.K.: research design, writing and editing the manuscript; N.B., data checking and analysis, S.S.H., H.A.K., literature review, checking, analysis, S.A.M., writing and editing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Khlaiwi, T., Habib, S.S., Bayoumy, N. et al. Identifying risk factors and mortality rate of premature coronary artery disease in young Saudi population. Sci Rep 14, 12727 (2024). https://doi.org/10.1038/s41598-024-62970-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62970-8
- Springer Nature Limited