Abstract
Comparison of the three methods standing-on-a-stool (SS), one knee kneeling on a stretcher (KS), and kneeling at the same height as the patient’s bed on the kneeling stool (KK) to evaluate the yielded of highest CPR quality and rescuer comfortability. A prospective randomized cross-over study which compares the three different rescuer positions for their effectiveness of chest compression. Conducted at a tertiary care between 19 and 22 Aug 2022. Emergency personnel aged 18 years or older, who completed the AHA-approved BLS course. The chest compression data was obtained by the ALIVE AED manikin® and AED reporting system. The information on the CPR quality and post-test questionnaires assessing the participants’ preference, satisfaction and modified Borg’s scale score was collected. The three methods shown no statistically significant difference in adequate chest compression depth (percentage). KK was not superior than SS at chest compression rate (P = 0.05). The adequate full chest recoil achieved with KK and KS were significantly higher than that of SS. However, there were no statistical difference between the three methods in the modified Borg’s scale score. Based on the satisfying score, the rescuers preferred KK to either SS (p 0.007) or KS (p 0.012). The three methods shown no statistically significant difference in adequate chest compression depth (percentage). Still, both KK and KS provided more adequate chest recoil, so we would recommend using these two methods in the ED.
Clinical trial registry: This study was retrospective registration in thaiclinicaltrials.org (TCTR20230119002, 19/1/2023).
Similar content being viewed by others
Introduction
High-quality cardiopulmonary resuscitation (CPR) is essential for improving the survival of Out of Hospital Cardiac Arrest (OHCA); in emphasizing high-quality CPR, the compression depth should be at least 5 cm but not exceed 6 cm for adult cardiac arrest patients. The chest should be released and allowed to recoil completely before initiating another compression, and the compression rate should be at least 100–120 compressions per minute. It is crucial to ensure that no interruptions occur while performing chest compression1,2,3.
The layperson and hospital staff may learn basic life support (BLS) in various programs, enabling them to become BLS providers and feel confident in emergencies situation4,5,6. However, the American Heart Association (AHA) guidelines and the European Resuscitation Council (ERC) guidelines do not provide any details about the rescuer’s position and posture during in-hospital cardiac arrest, especially in emergency department (ED) on stretcher that is different from the practice in BLS lesson except for the using a rigid backboard on the patients' backs. According to the literature review, kneeling positions were effective on a hard floor or on a wide patient bed (with space for kneeling beside the patient). Stand-on-a-stool is an effective method that shows non-inferiority to kneeling beside the patient; the principle is that the rescuer's knees are equally close to the patient's bed7,8,9. Standing on a stool has some disadvantages; this method can cause low back pain and imbalance10,11, and kneeling is impossible in the ED.
As a result, we developed an innovation that can simulate a rescuer in a kneeling position, the kneeling stool. Suppose stability is one of the reasons for effective chest compression. In that case, we included another method in which the rescuer placed one dominant knee on the bed and performed the chest compression because this posture is simple and brings the rescuer’s knee level with the patient’s bed. Hence, we aimed to demonstrate which of the three methods: stand-on-a-stool (SS), one knee kneeling on a stretcher (KS), and kneeling at the height as the patient’s bed on the kneeling stool (KK), was the best way to improve CPR quality and rescuer comfortability.
Methods
Trial design and setting
This study is a crossover, open-label, single-centered, randomized controlled trial conducted at Chiang Mai University Hospital, a tertiary care, university-based hospital between 19 AUG 2022 and 22 AUG 2022 to compare the effectiveness of chest compression in three different rescuer positions: kneeling on the kneeling stool (intervention), stand-on-a-stool, and one knee kneeling on a stretcher and standing on a step stool.
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki, and the study protocol received exempt approval from the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University (study code: EME-2564-08366). This study followed the Consolidated Standards of Reporting Trials (CONSORT) 2010 statement with extension to randomized crossover trials. Each participant provided written, informed consent before enrollment.
Participant
We recruited emergency personnel aged 18 years or older, including nurses, doctors, paramedics, and nurse aids who completed the AHA-approved BLS course. All participants were enrolled through wide announcements at the hospital and given written informed consent. Additionally, participant data including age, height, BMI, occupation, and work experience were recorded.
Trial protocol and intervention
As a crossover design, each participant planned to perform three methods (SS = A, KS = B, and KK = C) which random sequences resulting in three periods. Finally, six patterns were generated: ABC, BAC, CBA, CAB, ACB, and BCA.
All participants were randomly assigned to do a different sequence (6 sequences) for three postures (Fig. 1). We considered the risk of a carry-over effect from the previous period. Based on previous study of different resting methods in hand-only CPR, 2-min compression followed by 8-min of 10-s pause after 60-s compression was no significant difference in CPR quality indicators, including chest compression depth, compression with a depth of 5 cm or more, and chest compression rate. Additionally, physiological measures of rescuer fatigue, including heart rate, blood pressure, and pulse pressure, showed no difference12. In our study, participants only performed chest compressions for two minutes instead of the ten minutes as in the aforementioned study. This meant that a ten-minute break was sufficient for resting and avoiding any carry-over effects. Thus, we planned that each participant did the chest compressions for two minutes, then took a break of at least ten minutes as a washout period. Furthermore, repeat until all three poses are completed. Quality of chest compression data was obtained by the ALIVE BLS manikin® (Siamtool Engineering Co., Ltd.), capable of measuring compression depth, rate, recoil, and chest compression fraction. Participants answered the post-test questionnaire about preferability, satisfaction and modified Borg’s scale score.
For kneeling on a stand at the same height as the patient's bed, our innovation aimed to allow participants to do the chest compressions in a kneeling position beside the patient, which was the kneeling stool. The kneeling stool size was 70 × 80 × 80 cm, with a cushion pad for participant support. The innovative material structure was made of stainless steel (Figs. 2, 3). We limit the height of the bed in the method of SS no more than 20 cm from the knee because a prior study indicated that would reduce the quality of CPR8.
Outcome
High-quality CPR parameters included rate, depth, adequate depth, adequate full chest recoil, and chest compression fraction. So, this study's primary outcome was to compare the effectiveness of chest compression between three methods: rate, depth, adequate depth, and full chest recoil percentage. A secondary outcome was the participant preference, feeling of safety, confidence, and tiredness using the modified Borg's scale score.
Sample size
The study size estimation was based on the pilot data of 6 BLS-certified rescuers who worked in the ED. All rescuers were randomized in 3 × 3 fashions (three-intervention and three-period), mimicking an actual intended crossover study. Study size estimation via power calculation was done using Monte Carlo simulation of a linear mixed model using parameters estimated from our pilot data dataset. (Supplementary Fig. 1) Three independent components were included in the model: methods (representing the treatment effect), periods (representing the period effect), and the interaction term of methods and periods (representing the sequence effect). We calculated based on adequate chest compression depth parameters in our pilot data that showed method SS, KS, and KK were 80.5 ± 27.1%, 89 ± 23.6%, and 63.8 ± 41%, respectively. Parameters in the linear mixed model for the effect size of 10% were as follows: intercept, method KS’s coefficient, method KK’s coefficient, period 2’s coefficient, period 3’s coefficient, the interaction term of method KS and period 2, the interaction term of method KS and period 3, the interaction term of method KK and period 2, the interaction term of method KK and period 3, random-effect of method parameter, random-effect of period parameter, and observation-level error were 133%, 40%, 69%, − 58%, − 5.5%, 51%, 5%, 70%, − 31%, 51%, 11%, and 38%, respectively. We simulated power for level-2 (number of total patients included) study sizes with an alpha error of 0.05 and set the number of simulations at 1000 replications. Given our assumptions, we estimated that we would achieve more than 90% statistical power to detect the difference in the estimated interaction parameters (the sequence effect) with at least 50 participants. To account for the anticipated 20% of missing data or censored observations, we would include 63 participants.
Data analysis
Baseline characteristics were summarized as number, percentage, mean, standard deviation, median, and interquartile range (IQR) as appropriate. Data visualization demonstrated the normal distribution of continuous variables, and the categorical variable was determined using Fisher’s exact test. To account for correlated data in a crossover design, we used multilevel models with random effects incorporated with an interaction term of methods and periods to compare the difference of continuous variables among the three methods. If missing data were observed, multiple imputation methods would be used to handle the missing data before proceeding to regression analysis. The Stata version 16 (Stata Corp LLC, College Station, TX, USA) was used to analyze all statistical data. Statistical significance was specified at two-sided p < 0.05.
Ethics approval
Research Ethics Committee of the Faculty of Medicine, Chiang Mai University approved the research protocol on 6 Sep 2021 (study code: EME-2564-08366).
Result
A total of 69 participants were eligible for inclusion The mean age of the study participants was 29.5 ± 7.6 years, and there were 51 females (73.9%). The mean weight and height were 60.6 ± 14.8 kg, and 163.6 ± 7 cm, respectively (Table 1). There is no missing data.
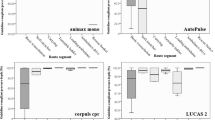
The three methods had no statistically significant differences in adequate chest compression depth (Table 2). In a group of compression depth of less than 5 cm, mean differences (MD) of KK vs SS, KS vs SS, and KK vs KS were − 4.6 cm (95% CI − 17.2 to 7.9 cm, p 0.468), 5.7 cm (− 6.6 to 18 cm, p 0.362), and − 10.4 cm (− 22.9 to 2.2 cm, p 0.105), respectively. In a group of compression depth of 5–6 cm, mean differences of KK vs SS, KS vs SS, and KK vs KS were 5.6 cm (95% CI − 6.7 to 17.8 cm, p 0.372), − 3 cm (− 15.2 to 9.2 cm, p 0.625), and 8.6 cm (− 3.6 to 20.8 cm, p 0.167), respectively. In a group of compression depth of greater than 6 cm, mean differences of KK vs SS, KS vs SS, and KK vs KS were 0.2 cm (95% CI − 11.8 to 12.2 cm, p 0.978), − 4 cm (− 15.9 to 8 cm, p 0.516), and 4.1 cm (− 7.9 to 16.1 cm, p 0.502), respectively. For compression rate, KS vs. SS (MD 2.6 times/min, 95% CI − 2.7 to 7.9 times/min, p 0.332) and KK vs. KS (MD 2.7 times/min, − 2.6 to 8 times/min, p 0.321) were no evidence of difference. KK had a different trend but was not better than SS for chest rate (MD 5.3 times/min, 0 to 10.6 times/min, p 0.05). For adequate full chest recoil percentage, KK was statistically better than SS (MD 22.6%, 7.7 to 37.6%, p 0.003). Also, KS was better than SS (MD 37.2%, 21.8 to 52.6%, p < 0.001). However, there were no statistical differences between the three methods in the modified Borg’s scale score. Based on the satisfying score, the rescuer preferred when performing KK to SS (MD 1.4 points, 0.4 to 2.4 points, p 0.007) or KS (MD 1.4 points, 0.3 to 2.5 points, p 0.012).
Discussion
This study demonstrated that a rescuer could perform high-quality CPR using any chest compression method if the rescuer's knee height was equal to the level of the patient's bed. However, the SS method has some limitations in fully recoiling. As in the previous study, it is unclear whether this was due to an incomplete recoil; we suspect it was caused by an unstable position13,14. Also, our study found no statistically significant difference in adequate chest compression depth (percentage). Although KK tended to have a slightly higher chest compression rate than SS, compression rates among all methods were still within the recommended range. KK and KS increased the adequate chest recoil percentage, whereas SS produced a surprisingly low rate of adequate chest recoil.
A previous study revealed that the efficiency of chest compression was diminished when the bed was 20 cm higher than the knee of the rescuer8. However, this depends on the stepstool and the rescuer's height15. Chest compression on a step stool (stand-on-a-stool or SS) demonstrated effective quality in chest compression depth and was not inferior to floor chest compression7. Our study discovered that adequate chest compression was achieved when the rescuer's knee was at the same level as the patient's bed; however, the SS approach cannot adjust the level of the rescuer's knee to the bed level, resulting in insufficient chest recoil. Chest recoil is essential to high-quality CPR because it allows more blood to refill the heart to fill between chest compressions adequately. Following OHCA, the ideal Chest compression rate and chest compression dept combination are linked to a positive neurologic outcome3.
Our study examined the impact of rescuer position on chest compression quality in a controlled experimental setting. However, real-world CPR scenarios involve additional factors such as compressor changes and interrupted for rhythm analysis, defibrillation, and breathing (in cases without intubation), which contribute to low chest compression fraction or "no flow time" aspects not addressed in our study. While a high ratio in chest compression fraction is crucial for CPR quality, our study did not explore how different CPR positions might affect this aspect. Future research should consider these real-world factors to better understand their impact on CPR quality.
Kneeling CPR is the typical technique provided in BLS courses worldwide while standing CPR is unfamiliar and may initially result in inferior quality. Our research also indicated that standing CPR was associated with poorer quality. In real-world practice, we, therefore, proposed using a kneeling stool. Chest compression on the floor compared to kneeling on the patient’s bed is not different16,17,18. One study suggests that kneeling was the optimal position for CPR since it optimized the time the chest was compressed effectively and reduced back pain10. From our post-test questionnaire, most participants preferred the KK because this posture felt stable and familiar, like kneeling on the floor, and they believed that it reduced low back pain compared to the standing posture. If the kneeling stool (KK) was available, most participants preferred to try it. Comparable to the benefit, there may have some disadvantages, including an impediment when changing the rescuer's position, limited space to perform some procedures, and the inability to adjust the height. But our study suggests that three methods may be used to achieve high-quality CPR. Still, we recommend KK and KS because both methods were better at achieving adequate full chest recoil when compared with SS. If CPR is prolonged for more than 2 min, kneeling is better than stand-on-a-stool posture10.
Limitation
This study had some main limitations. First, the primary outcome was chest compression depth while, the manikin could only report rate of adequate depth of compression (less than, greater than or equal to 5–6 cm) which was not the actual depth of the compression. Second, our study utilized manikins which may have affected the rescuer's sensation as it may not have felt the same as when performing chest wall compressions with real people. Furthermore, due to being simulated, the experience gave no stress and tension unlike the real-life situations. Therefore, scenario-based practice and simultaneous data collection of high-quality chest compression may be used in further study.
Third, we estimated the sample size to account for the percentage of adequate chest compression depth. However, there were many CPR quality indicators. Future research may consider calculating the sample size based on various effectiveness endpoints of chest compressions, including considering multiplicity from the perspective of multi-group comparisons. Fourth, we designed a washout period of at least ten minutes between each period to allow participants to take a break before moving on to the next period based on a previous study of 2-min compression followed by an 8-min 10-s pause after 60-s compression that revealed no significant difference in CPR quality indicators. The duration of the washout period varied for each participant but was not recorded. Thus, the duration between periods could be recorded in the future study. In addition, it may be considered if the washout period is lengthened to several hours or days. Lastly, Our study did not address real-world CPR situations involving factors such as changing compressors every 2 min, interrupted compressions for rhythm analysis, defibrillation, providing breaths (in cases without intubation), and during intubation, which may contribute to no-flow time.
Conclusion
The three methods had no statistically significant differences in adequate chest compression depth (percentage). Still, both kneeling on the kneeling stool (KK) and one knee kneeling on a stretcher (KS) achieved better adequate chest recoil, so we recommend using these two methods for high-quality CPR in the ED.
Data availability
The datasets are available from the corresponding author upon reasonable request.
References
Iwami, T., Kitamura, T., Kiyohara, K. & Kawamura, T. Dissemination of chest compression-only cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Circulation 132, 415–422 (2015).
Rao, P. & Kern, K. B. Improving community survival rates from out-of-hospital cardiac arrest. Curr. Cardiol. Rev. 14, 79–84 (2018).
Duval, S. et al. Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA Cardiol. 4, 900 (2019).
Hsu, S.-C., Kuo, C.-W., Weng, Y.-M., Lin, C.-C. & Chen, J.-C. The effectiveness of teaching chest compression first in a standardized public cardiopulmonary resuscitation training program. Medicine 98, e14418 (2019).
Bielec, G., Klajman, P. & Pęczak-Graczyk, A. Effectiveness of basic life support instruction in physical education students: A pilot study. Teach. Learn. Med. 26, 252–257 (2014).
Jiang, L., Min, J., Yang, F. & Shao, X. The optimal chest compression point on sternum based on chest-computed tomography: A retrospective study. Hong Kong J. Emerg. Med. 27, 197–201 (2020).
Oh, J. H., Kim, C. W., Kim, S. E., Lee, S. J. & Lee, D. H. Comparison of chest compressions in the standing position beside a bed at knee level and the kneeling position: a non-randomised, single-blind, cross-over trial: Table 1. Emerg. Med. J. 31, 533–535 (2014).
Cho, J., Oh, J. H., Park, Y. S., Park, I. C. & Chung, S. P. Effects of bed height on the performance of chest compressions. Emerg. Med. J. 26, 807–810 (2009).
Lewinsohn, A., Sherren, P. B. & Wijayatilake, D. S. The effects of bed height and time on the quality of chest compressions delivered during cardiopulmonary resuscitation: a randomised crossover simulation study. Emerg. Med. J. 29, 660–663 (2012).
Foo, N.-P., Chang, J.-H., Lin, H.-J. & Guo, H.-R. Rescuer fatigue and cardiopulmonary resuscitation positions: A randomized controlled crossover trial. Resuscitation 81, 579–584 (2010).
Hasegawa, T., Okane, R., Ichikawa, Y., Inukai, S. & Saito, S. Effect of chest compression with kneeling on the bed in clinical situations. Jpn. J. Nurs. Sci. 17, 12314 (2020).
Dong, X. et al. Different resting methods in improving laypersons hands-only cardiopulmonary resuscitation quality and reducing fatigue: A randomized crossover study. Resusc. Plus 8, 100177 (2021).
Mirwanti, R. The impact of CPR position (kneeling, footstool and standing beside bed) on cardiopulmonary resuscitation quality: A literature review. Padjadjaran Acute Care Nurs. J. 1, 28846 (2020).
Edelson, D. P., Call, S. L., Yuen, T. C. & Hoek, T. L. V. The impact of a step stool on cardiopulmonary resuscitation: A cross-over mannequin study. Resuscitation 83, 874–878 (2012).
Lee, D. H., Kim, C. W., Kim, S. E. & Lee, S. J. Use of step stool during resuscitation improved the quality of chest compression in simulated resuscitation: Effect of step stool on chest compression. Emerg. Med. Australas. 24, 369–373 (2012).
Kim, J. A. et al. A randomized, controlled comparison of cardiopulmonary resuscitation performed on the floor andon a moving ambulance stretcher. Prehosp. Emerg. Care 10, 68–70 (2006).
Sebbane, M. et al. Chest compressions performed by ED staff: A randomized cross-over simulation study on the floor and on a stretcher. Am. J. Emerg. Med. 30, 1928–1934 (2012).
Mygind-Klausen, T. et al. In a bed or on the floor? The effect of realistic hospital resuscitation training: A randomised controlled trial. Am. J. Emerg. Med. 36, 1236–1241 (2018).
Acknowledgements
We would like to thank Miss Rudklao Sairai and colleagues, the Research Unit of the Department of Emergency Medicine, Faculty of Medicine, Chiang Mai University, for supporting this study. We would like to thank Dr. Phichayut Phinyo for serving as a statistical consultant in this research.
Funding
This work was supported by Faculty of Medicine, Chiang Mai University (grant number MC022-65) on 5 May 2022.
Author information
Authors and Affiliations
Contributions
NC contributed to the conceptualization, methodology, formal analysis, investigation, data curation, writing—original draft, writing—review and editing, visualization. PL contributed to the conceptualization, methodology, investigation, writing—original draft, writing—review and editing, funding acquisition. TT contributed to the conceptualization, methodology, software, validation, formal analysis, investigation, data curation, writing—original draft, writing—review and editing. BW contributed to the conceptualization, methodology, validation, formal analysis, investigation, resources, writing—original draft, writing—review and editing, supervision, project administration. This manuscript has been read and finally approved by all the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Charungwatthana, N., Laohakul, P., Tangsuwanaruk, T. et al. Effectiveness of innovative chest compression on the emergency department stretcher by an alternative method: a randomized controlled crossover trial. Sci Rep 14, 12284 (2024). https://doi.org/10.1038/s41598-024-62845-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62845-y
- Springer Nature Limited