Abstract
Metabolism of praziquantel (PZQ), a racemic mixture and the only drug approved to treat S. mansoni infection, is mediated by genetically polymorphic enzymes. Periodic school-based mass drug administration (MDA) with PZQ is the core intervention to control schistosomiasis. However data on the impact of pharmacogenetic variation, nutrition, and infection status on plasma PZQ exposure is scarce. We investigated genetic and non-genetic factors influencing PZQ plasma concentration and its metabolic ratios (trans-4-OH-PZQ/PZQ and cis-4-OH-PZQ/PZQ). Four hundred forty-six school children aged 7–15 years from four primary schools in southern Ethiopia who received albendazole and PZQ preventive chemotherapy through MDA campaign were enrolled. Genotyping for common functional variants of CYP3A4 (*1B), CYP3A5 (*3, *6), CYP2C19 (*2, *3, *17), CYP2C9 (*2, *3), and CYP2J2*7 was performed. Plasma concentrations of PZQ, trans-4-OH-PZQ, and cis-4-OH-PZQ were quantified using UPLCMS/MS. Carriers of CYP2C19 defective variant alleles (*2 and *3) had significantly higher mean PZQ plasma concentration than CYP2C19*1/*1 or *17 carriers (p = 0.005). CYP2C19*1/*1 and CYP2C19*17 carriers had higher trans-4-OH-PZQ/PZQ and cis-4-OH-PZQ/PZQ metabolic ratios compared with CYP2C19*2 or *3 carriers (p < 0.001). CYP2J2*7 carriers had lower mean PZQ plasma concentration (p = 0.05) and higher trans-4-OH-PZQ/PZQ and cis-4-OH-PZQ/PZQ metabolic ratios. Male participants had significantly higher PZQ concentration (p = 0.006) and lower metabolic ratios (p = 0.001) than females. There was no significant effect of stunting, wasting, S. mansoni or soil-transmitted helminth infections, CYP3A4, CYP3A5, or CYP2C9 genotypes on plasma PZQ or its metabolic ratios. In conclusion, sex, CYP2C19 and CYP2J2 genotypes significantly predict PZQ plasma exposure among Ethiopian children. The impact of CYP2C19 and CYP2J2 genotypes on praziquantel treatment outcomes requires further investigation.
Similar content being viewed by others
Introduction
Globally, about 250 million people are currently infected with schistosomiasis, and 800 million are at risk of infection in endemic areas, mainly in tropical and sub-tropical regions1,2,3. Over 90% of the disease burden is from Sub-Saharan African (SSA) countries4. In Ethiopia, approximately 38.3 million people live in schistosomiasis-endemic areas5. Schistosomiasis was first reported in the country in 19346, and children in high transmission areas are the most affected. Repeated exposure to contaminated water with infectious cercariae leads to chronic schistosomiasis, especially in children7. In Ethiopia, schistosomiasis remains among the significant causes of morbidity in children8. Chronic schistosomiasis can lead to several health complications, including malnutrition, anemia, impaired childhood development, fatigue, exercise intolerance, and poor cognitive function9,10,11.
Preventive chemotherapy using mass praziquantel (PZQ) administration, targeting school-aged children, is the cornerstone prevention and control strategy recommended by the World Health Organization (WHO) to control schistosomiasis and interrupt transmission in endemic regions12. PZQ has been used in large-scale mass drug administration (MDA) programs worldwide since 198412. The standard recommended dosage for treating schistosomiasis is 40 mg/kg body weight. However, this standard dosage resulted in varying treatment outcome (efficacy and safety) findings in SSA among pre-school and school-aged children13. Variability in drug response may result from various factors, including genetic variations, nutrition, environmental factors, and type of disease14.
Genetic variations influence variability in drug exposure and treatment response of various infectious diseases15,16,17. However, data on the importance of genetic variation for variability in PZQ plasma exposure between populations and individuals is scarce18,19,20,21. Assessing the importance of genetic and non-genetic factors that influence variation in PZQ exposure in genetically diverse populations of Africa, where the disease is most prevalent, is imperative22 to optimize treatment23. Recent studies highlighted the significant contribution of genetic variations on PZQ plasma concentration and treatment outcomes20,24 and the need for pharmacogenetic studies of PZQ, especially in the African continent19.
Praziquantel, a racemic mixture of the biologically active enantiomer (R-PZQ) and distomer (S-PZQ)18,19, is metabolized in the liver by CYP enzymes, including CYP1A2, CYP3A4, CYP3A5, CYP2C9, CYP2C19 and CYP2D619,25. The two major metabolites in humans are trans-4-OH-PZQ and cis-4-OH-PZQ18,19,25,26. The CYP enzymes are genetically polymorphic, showing broad inter-individual variability in enzyme activity, which may affect PZQ plasma concentration27. In this study, we assessed the effect of genetic variations on plasma concentrations of PZQ and its major metabolites (trans- and cis-4-OH PZQ) among school children who received mass PZQ and albendazole (ALB) in two rural districts in Southern Ethiopia.
Methods
Study design, area, and population
This prospective observational pharmacogenetics-pharmacokinetics study was conducted to investigate the effect of genetic variations on plasma concentrations of PZQ and its major metabolites. The study was conducted in two rural districts in southern Ethiopia in January 2019. The two districts, Hawella Tula and Wondo Gennet, are located around the shore of Lake Hawassa and are known for their high endemicity of schistosomiasis and soil-transmitted helminths5,28.
The study population consisted school children who were eligible for PZQ and ALB combination preventive chemotherapy for the control of schistosomiasis and soil-transmitted helminths as per the WHO and the Ethiopian NTD preventive chemotherapy guidelines. A total of 446 schoolchildren aged 7–15 years attending four primary schools-Bushulo, Kidus Pawulos, Finchawa, and Wosha-located in the two study districts were enrolled in this study. All children attending the study schools were eligible for PZQ and ALB preventive chemotherapy.
Ethical considerations
Prior to the study initiation, permission to conduct the study was obtained from regional, zonal, and woreda Health and Education offices. The study received ethics approval from Southern Nations, Nationalities and Peoples Region Health Bureau ethical clearance committee (Ref no 902-6-19/14966), The Ethiopia National Research Ethics Review Committee (Ref no MoSHE//RD/141/9848/20), and The Swedish Ethics Review Authority (Ref No 2020-00845). Study participants and their guardians/parents were informed about the study and data collection processes, and children whose parents/guardians gave written informed consent were enrolled in the study. The study was conducted according to the guidelines of the Declaration of Helsinki. Informed consent from parents/guardians and assent from participants who were > 12 years of age were obtained.
Data collection and preventive chemotherapy
Socio-demographic characteristics, including sex, age, and clinical data such as body weight, height, nutritional status, and infection status, were collected using a case record form through interviews before MDA. School-based MDA with PZQ and ALB 400 mg was given as preventive chemotherapy through an MDA campaign led by the national NTD control public health program coordinators. The study team had no role in the MDA planning, implementation, and administering of the drugs. The dosing of PZQ was based on the WHO dose pole based on height (corresponding to 40 mg/kg body weight)29. All children attending primary schools in the two rural districts received MDA irrespective of their infection status. The nutritional status of the participants was assessed by converting the height for age Z score (HAZ) for stunting and BMI for age Z score (BAZ) for wasting using WHO Anthro Plus software30.
Stool and blood samples collection
Two weeks before MDA, stool samples were collected for microscopic examination for screening and diagnosis of S. mansoni and soil transmitted helminths infection using Kato-Katz technique. On the MDA Day, whole blood samples for genotyping were collected in EDTA-containing vacutainer tubes from 446 participants and stored at −80 °C. Two hours post-dose, blood samples were collected from each participant in the heparinized tube and centrifuged at 1000 rpm for 10 min, and plasma samples were stored at −80 °C until analysis. Both whole blood and plasma samples were packed with dry ice and shipped to Karolinska Institutet, Stockholm, Sweden, for laboratory analysis.
Quantification of plasma PZQ, trans-and cis-4-OH-PZQ concentration
Reference standards such as rac-PZQ, trans-4-OH-PZQ, and cis-4-OH-PZQ and their respective internal standards rac-PZQ-d11, trans-4-OH-PZQ-d5, and cis-4-OH-PZQ-d5 were purchased from Toronto Research Chemicals (Toronto, Ontario, Canada). Acetonitrile, methanol, and formic acid of mass spectrometry (MS) grade were purchased from Merck (Darmstadt, Germany). Ultra-pure MilliQ water was prepared using a Milli-Q water purification system (Merck Millipore, Massachusetts, USA). Blank plasma was kindly supplied by the blood bank of the Karolinska University Hospital Huddinge (Stockholm, Sweden).
The plasma sample preparation procedure for quantification of PZQ, trans-4-OH-PZQ and cis-4-OH-PZQ was adapted from Nyla et al.25 with slight modification. Briefly, 100 µL of plasma sample was added to 300 µL of internal standard solution consisting of 50 ng/mL of rac-PZQ-d11, trans-4-OH-PZQ-d5 and cis-4-OH-PZQ-d5 in a 50:50 mixture (v:v) of acetonitrile: methanol. The mixture was vortexed for 3 min, followed by centrifugation for 20 min at 3220g at 4 °C. Then, 75 µl of the supernatant was diluted with 75 µL MilliQ water and 5 µL was injected into the UPLC-MS/MS system. Standards and quality control (QC) samples were prepared in the same manner by adding 10 µL standard and QC 10× concentrated solutions to 90 µL blank plasma and precipitating as above.
The UPLC–MS/MS method of quantification of the analytes was done as described previously20,31. The calibration curves were constructed within the range of 2.4 to 2500 ng/mL for PZQ and cis-4-OH-PZQ, and from 24 to 25,000 ng/mL for trans-4-OH-PZQ, since the levels of trans-4-OH-PZQ were very high in the samples. About 7–9 calibration points were injected twice before and after the samples. The QC samples were injected every 20 samples. The analytes were quantified using the analyte to internal standard integrated peak area ratio with the Mass Lynx application manager Target Lynx (Waters). Trans-4-OH-PZQ d5 was used as an internal standard also for cis-OH-PZQ since their retention times were similar. Quality control samples at 9.8, 78.1, and 1250 ng/mL were injected at regular intervals during each analysis.
CYP3A4, CYP3A5, CYP2C19, CYP2C9 and CYP2J2 genotyping
Genomic DNA was extracted from whole-blood samples using QIAamp DNA MidiKit (QIAGEN GmbH, Hilden, Germany) as per the manufacturer’s protocol. The purity and quantity of the extracted DNA were measured using NanoDrop 2000 (Thermo Scientific, Saveen Warner, Sweden). Genotyping for the common functional variant alleles in genes coding for CYP enzymes relevant for PZQ disposition was performed using allelic discrimination TaqMan genotyping assays (Applied Biosystems, CA, USA) as previously discussed20,31.
Briefly, genotyping was performed for CYP3A4 (*1B), CYP3A5 (*3, *6), CYP2C19 (*2, *3, *17), CYP2C9 (*2, *3), and CYP2J2 (*7) as described previously20,31. Genotyping for CYP3A5*7 was not done as previous studies reported its absence in the Ethiopian population17,32. The allelic discrimination reactions were performed using TaqMan® genotyping assays (Applied Biosystems®, CA, USA) with the following ID numbers for the (SNPs): C__11711730_20 for CYP3A4*1B (− 392A > G, rs2740574), C__26201809_30 for CYP3A5*3 (c.6986A4G, rs776746), C__30203950_10 for CYP3A5*6 (g.14690G4A, rs10264272), C__25986767_70 for CYP2C19*2 (rs4244285), C__2,7861809_10 for CYP2C19*3 (rs4986893), C__469857_10 for CYP2C19*17 (rs12248560), C__25625805_10 for CYP2C9*2 (rs1799853), C__27104892_10 for CYP2C9*3 (rs1057910) and C_9581699_80 for CYP2J2 *7.
The genotyping was performed on Applied Biosystems® 7500 Real-Time PCR Systems (Applied Biosystems, United States). The final volume of the PCR mixture was 10 μL, consisting of 5μL TaqMan fast advanced master mix (Applied Biosystems, United States), 3.5 μL deionized water, 0.5 μL 20× drug metabolizing genotype assay mix and 1 μL genomic DNA. The thermal cycler condition involves an initial step at 60 °C for 30 s, hold stage at 95 °C for 10 min, followed by PCR stage for 40 cycles of 95 °C for 15 s, 60 °C for 1 min and after reading stage with 60 °C for 30 s.
Study outcomes
The study outcomes were praziquantel, trans- and cis-4-OH-PZQ, metabolic ratios (trans-4-hydroxy-praziquantel/praziquantel and cis-4-hydroxy-praziquantel/praziquantel) concentrations and the effect of CYP3A4, CYP3A5, CYP2C19, CYP2C9 and CYP2J2 genotypes as well as non-genetic factors on the plasma concentrations.
Statistical data analysis
Baseline socio-demographic, clinical, and laboratory parameters were described using means and standard deviations (SD) or medians and interquartile range (IQR) for continuous variables and as percentages for categorical variables. The Chi-square test was used to compare the genotype and allele frequencies between the observed and expected according to the Hardy–Weinberg equilibrium.
The plasma concentration data was converted to log10 values before statistical analysis. Independent sample t-tests or One-way ANOVA was used to compare the log-plasma PZQ, trans-4-OH-PZQ, and cis-4-OH-PZQ concentrations as well as the metabolic ratios (trans-4-OH-PZQ/PZQ and cis-4-OH-PZQ/PZQ) across the different CYP450 genotypes. Then, the arithmetic means of the log-transformed PZQ, trans-4-OH-PZQ, cis-4-OH-PZQ, trans-4-OH-PZQ/PZQ, and cis-4-OH-PZQ/PZQ concentrations were anti-logged to obtain their respective geometric means (GM) and standard deviations (SD).
A Univariate analysis followed by a multivariate linear regression analysis was performed to identify predictors of PZQ, trans-4-OHPZQ, and cis-4-OH-PZQ plasma concentrations and metabolic ratios. Variables age, sex, baseline S. mansoni infection status, Soil-Transmitted Helminths (STH) infection, S. mansoni–STH co-infection, anemia status, HAZ, BAZ, and the CYP450 genotypes were tested in the linear regression analysis. Variables with p-value < 0.2 from the univariate analysis were included in the multivariate analysis. In all the analyses, p-values were two-sided, and p < 0.05 was considered statistically significant. Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) software for Windows version 24 (SPSS, IBM Corp, Armonk, NY, USA).
Result
Socio-demographic characteristics
A total of 446 school children who received the standard PZQ and ALB preventive chemotherapy through MDA to control schistosomiasis and soil-transmitted helminths participated in this study. The median age of the participants was 11 years (IQR = 8–13). Female participants were 51.6%. The proportions of participants with stunting and wasting were 21.9% and 9.3%, respectively. Only 4.3% of the participants were anemic at baseline assessment, as presented in Table 1.
Genotypes and alleles frequencies
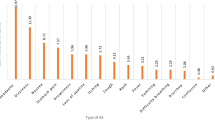
There were no significant differences between the observed and expected genotype frequencies according to the Hardy Weinberg Equilibrium. The highest allele frequency was observed for CYP3A5*3 (48.5%) followed by CYP3A4*1B (40.4%), and the lowest allele frequency was 1.6% for CYP2C9*2 (Table 2).
Effect of CYP genotypes on PZQ concentration and metabolic ratios
For assessing the effect of CYP genotypes on PZQ plasma concentration, its major metabolites, and respective metabolic ratios, we categorized all genotypes as extensive metabolizers (*1/*1) and carriers of defective variant allele (intermediate or slow metabolizers) except for CYP2C19 genotype. CYP2C19 genotype was categorized as extensive and ultra-rapid metabolizers (*1/*1, *17 carriers), intermediate and slow metabolizers (*2, *3 carriers). The geometric means of PZQ, trans-4-OH PZQ/PZQ and cis-4-OH PZQ/PZQ among the different genotype groups are summarized in Table 3. The overall geometric means ± SDs of PZQ, trans-4-OH PZQ and Cis-4-OH PZQ, were 221.7 ± 5.6 ng/mL, 4406.2 ± 2.7 ng/mL and 220.0 ± 3.8 ng/mL, respectively. PZQ plasma concentrations were significantly associated with CYP2C19 and CYP2J2 genotypes. Likewise, CYP2C19 and CYP2J2 genotypes had significant association with the metabolic ratios both trans-4-OH PZQ/PZQ and cis-4-OH PZQ/PZQ.
Predictors of praziquantel plasma concentration
To identify predictors of PZQ plasma concentration, we analyzed log10 converted concentration data using univariate and multivariate linear regression. Variables with p-value ≤ 0.2 in the univariate analysis, such as sex, wasting, CYP2C19 and CYP2J2 genotypes, were included in the multivariate analysis (Table 4). Sex and CYP2C19 remained significant predictors of PZQ plasma concentration in the multivariate analysis. Male participants had a mean increase in concentration of 0.27 ng/ml (95% CI,0.12 – 0.42). Likewise, carriers of CYP2C19 (*2, *3) had an increase in mean PZQ plasma concentration of 0.27 ng/ml (95% CI 0.08–0.46 and p = 0.005) compared to CYP2C19 *1/*1, or *17 carriers.
Predictors of trans-4-OH-PZQ/PZQ metabolic ratio
We used univariate and multivariate linear regression analysis to assess predictors of trans-4-OH-PZQ/PZQ. In the univariate analysis, sex, wasting, CYP2C19, and CYP2J2 genotypes had p-values ≤ 0.2 and were included in the multivariate model. In the multivariate analysis, sex and CYP2C19 genotype were significant factors predicting trans-4-OH-PZQ/PZQ. Male participants had a mean decrease of trans-4-OH-PZQ/PZQ metabolic ratio by 0.15 ng/ml (95% CI −0.23 to −0.06) compared to female participants. Similarly, CYP2C19*2 or *3 carriers had significantly lower mean trans-4-OH-PZQ/PZQ metabolic ratios than CYP2C19 *1/*1, or *17 carriers (Table 5).
Predictors of cis-4-OH-PZQ/PZQ
In the univariate analysis, sex, S. mansoni infection status, CYP2C19, and CYP2J2 genotypes had p-values ≤ 0.2 and were included in the multivariate model. In the multivariate analysis, sex, CYP2C19, and CYP2J2 genotype remained significant predictors of cis-4-OH-PZQ/PZQ metabolic ratio. In the multivariate model, sex, CYP2J2 and CYP2C19 genotypes were significant predictors of cis-4-OH-PZQ/PZQ metabolic ratio. CYP2C19 (*1, *17) and CYP2J2*7 carriers had higher cis-4-OH-PZQ/PZQ metabolic ratio compared to CYP2C19 (*2, *3) carriers and CYP2J2*1/*1 genotype (p < 0.001 and 0.038) respectively (Table 6).
Discussion
Schistosomiasis remains a major problem in Sub-Saharan Africa, and millions of children living in endemic countries receive periodic school-based mass praziquantel administration to control and halt transmission. Genetically polymorphic CYP enzymes metabolize PZQ, but the impact of genetic variations on drug exposure, particularly in black Africans, the most genetically diverse population, is not well explored. We investigated the effect of genetic variations on plasma concentrations of PZQ, its major metabolites (trans-4-OH PZQ, Cis-4-OH PZQ), and metabolic ratios (trans-4-OH PZQ/PZQ and Cis-4-OH PZQ/PZQ) among school children who received mass PZQ and ALB administration.
There are several notable findings from this study: First, there was a significant association of CYP2C19 and CYP2J2 genotypes with PZQ plasma concentration and trans-4-OH PZQ/PZQ and Cis-4-OH PZQ/PZQ metabolic ratios. Carriers of defective CYP2C19 variant alleles (*2 or *3) had significantly higher PZQ plasma concentration and lower metabolic ratio than CYP2C19 extensive metabolizers. On the other hand, CYP2J2*7 carriers had a borderline lower PZQ plasma concentration and significantly higher cis-4-OH PZQ/PZQ metabolic ratio. Second, sex significantly predicted PZQ plasma concentration and trans-4-OH PZQ/PZQ and Cis-4-OH PZQ/PZQ metabolic ratios. Male participants had higher PZQ plasma concentration and lower trans-4-OH PZQ/PZQ and Cis-4-OH PZQ/PZQ metabolic ratios compared to females. No significant effect of having infection by S. mansoni or soil-transmitted helminths, or nutritional status (stunting, wasting) or CYP3A4, CYP3A5, or CYP2C9 genotype on plasma praziquantel concentration or its metabolic ratio was observed. This is the first study to explore the impact of genetic and non-genetic factors, including S. mansoni and soil-transmitted helminth infection status in Ethiopian children.
In humans, praziquantel is metabolized primarily by CYP2C19 to 4-OH PZQ, the major metabolite, and to some extent by CYP1A2, CYP3A4, CYP3A5, and CYP2C919,20,25. Genes coding for these metabolizing enzymes are genetically polymorphic. Thus, investigating the effect of genetics on PZQ exposure is important, especially in the genetically diverse SSA population20,21, and variations in treatment outcomes have been reported13. Moreover, the African continent contributes more than 90% of the global disease burden4, and Preventive chemotherapy through MDA campaigns periodically without prior diagnosis to all at-risk children living in endemic areas. The genotype and allele frequencies of CYP3A4*1B, CYP3A5 (*3,*6), CYP2C9 (*2,*3), CYP2C19 (*2,*3,*17), and CYP2J2*7 observed in our study were similar with those of previous studies conducted in Ethiopian population32,33,34.
In addition to exploring the impact of genotype in relevant enzymes involved in the intricate metabolic pathway of praziquantel, we investigated the role of CYP2J2 genotype, which has not been previously examined in this context. It is noteworthy that albendazole, co-administered with praziquantel in school-based MDA programs as per the WHO recommendations in endemic areas, is primarily metabolized by CYP2J235,36. With our study participants receiving both praziquantel and albendazole as part of preventive chemotherapy, we aimed to evaluate any potential impact of CYP2J2 genotype. Drug interactions could potentially affect the relationship between genotype and plasma concentrations of co-administered drugs, necessitating further investigation. Furthermore, the relevance of the CYP2J2 enzyme for praziquantel metabolism has not been previously explored. Our finding of a significant impact of CYP2J2 genotype on praziquantel plasma concentration could be attributed to its influence on albendazole metabolism, potentially altering the absorption, metabolism, and transport of praziquantel. Alternatively, CYP2J2 may directly affect praziquantel metabolism, although this aspect requires further investigation.
Our study found a significant association between CYP2C19 genotype and PZQ plasma concentration; a higher PZQ concentration was observed among children carrying defective alleles CYP2C19 (*2 or *3) compared to those with wild type (CYP2C19 *1/*1)) or CYP2C19 *17 carriers. Likewise, the CYP2C19 genotype was also significantly associated with trans 4-OH-PZQ/PZQ and cis 4-OH-PZQ/PZQ) metabolic ratios. CYP2C19 extensive metabolizers had lower metabolic ratios compared to those carrying defective CYP2C19 alleles variant allele (*2 or *3). Similar findings were reported among S. mansoni-infected Tanzanian children who received praziquantel therapy, where the CYP2C19 genotype was significantly associated with PZQ plasma concentration and the trans 4-OH-PZQ/PZQ metabolic ratio20. However, the study in Tanzania did not assess cis-OH-PZQ/PZQ as we did in this study. This finding strengthens the previous evidence that CYP2C19 is a major metabolic pathway for the formation of major PZQ metabolites such as trans-and cis 4-OH-PZQ20,25,37. Furthermore, these findings indicate the relevance of the CYP2C19 genotype in determining praziquantel plasma exposure among children receiving PZQ MDA. However, the relevance of CYP2C19 genotype for the safety and efficacy of praziquantel needs to be investigated.
Our study also found a borderline association between CYP2J2 genotype (p = 0.05) and PZQ plasma concentration, where higher PZQ plasma concentrations were observed among CYP2J2 *1/*1 genotypes compared to CYP2J2 *7 carriers. CYP2J2 genotype was significantly associated with both trans-4-OH-PZQ/PZQ and cis 4-OH-PZQ/PZQ) the metabolic ratios, being higher among CYP2J2 *7 carriers than the wild type (CYP2J2 *1/*1). The CYP2J2 *7 variant allele is reported to be associated with increased enzyme activity34, which is in line with our findings. A recent study reported the contribution of CYP2J2 genotype for PZQ metabolism though not statistically significant31. The significant association of CYP2J2 genotype with variability in PZQ plasma concentration in our study may indicate the contribution of CYP2J2 enzyme for PZQ metabolism. CYP2J2 metabolizes structurally diverse compounds that are also metabolized by CYP3A4, but with differences in regioselectivity35,38. In addition to its role in endogenous metabolism, recent studies highlighted the importance of CYP2J2 for metabolizing various drugs, including anti-malarial and anti-tuberculosis that are widely used in Africa39,40. For the first time, our result indicates CYP2J2 genotype plays an important role in inter-individual variability in PZQ and its metabolites exposure.
Our study also found significant sex differences in PZQ and its metabolite exposure. Male participants had significantly higher PZQ plasma concentration and lower trans-4-OH PZQ/PZQ and cis-4-OH PZQ/PZQ metabolic ratios than females. This observation aligns with previous research indicating higher CYP enzyme activity among females compared to males41,42. Consistent with these findings, our study suggests that females displayed lower PZQ plasma concentrations, implying enhanced enzyme activity. Sex differences in drug metabolism stem from a range of biological factors, including variations in hormone levels, enzyme expression, body weight, body mass index (BMI), fat distribution, and other physiological disparities between males and females43,44. These differences can lead to variations in drug absorption, distribution, metabolism, and elimination within the body, thereby resulting in distinct pharmacokinetic profiles between males and females.
Although CYP3A4, CYP3A5, and CYP2C9 enzymes were identified as relevant for the metabolism of PZQ in previous studies18,19,25,26, our study found no significant association between CYP3A4, CYP3A5, and CYP2C9 genotypes and PZQ plasma concentration, and its metabolic ratios. This finding further suggests that CYP2C19 is a major metabolic pathway for the formation of major PZQ metabolites in humans. In addition, our study identified the CYP2J2 genotype as another possible pathway for PZQ metabolism.
Conclusion
We conclude that plasma concentrations of PZQ and its metabolic ratio display wide inter-individual variability, partly due to pharmacogenetic variations and sex differences. CYP2C19 and CYP2J2 genotypes significantly predict PZQ plasma concentration and its metabolic ratios -trans 4-OH-PZQ/PZQ and Cis 4-OH-PZQ/PZQ. CYP2J2 genotype is significantly associated with PZQ and its major metabolites exposure; therefore, CYP2J2 could be another important pathway for PZQ metabolism in humans. This study highlights the importance of pharmacogenetic variation for PZQ pharmacokinetics. The impact of genetic variations on PZQ treatment outcomes requires further investigations.
Data availability
All relevant data are included in the manuscript; further enquiries can be directed to the corresponding author.
References
Olveda, U. & Bilharzia, D. Pathology, diagnosis, management and control. Trop. Med. Surg. https://doi.org/10.4172/2329-9088.1000135 (2013).
Hotez, P. J. et al. The Global Burden of Disease Study 2010: Interpretation and implications for the neglected tropical diseases. PLoS Negl. Trop. Dis. 8, e2865 (2014).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
Hotez, P. J. & Kamath, A. neglected tropical diseases in sub-Saharan Africa: Review of their prevalence, distribution, and disease burden. PLOS Negl. Trop. Dis. 3, e412 (2009).
Leta, G. T. et al. National mapping of soil-transmitted helminth and schistosome infections in Ethiopia. Parasites Vectors 13, 437 (2020).
Kloos, H. et al. Schistosomiasis in Ethiopia. Soc. Sci. Med. 26, 803–827 (1988).
Colley, D. G. et al. Human schistosomiasis. Lancet 383, 2253–2264 (2014).
Jember, T. H. Challenges of schistosomiasis prevention and control in Ethiopia: Literature review and current status. JPVB 6, 80–86 (2014).
King, C. H. & Dangerfield-Cha, M. The unacknowledged impact of chronic schistosomiasis. Chronic Illn. 4, 65–79 (2008).
Ezeamama, A. E. et al. Cognitive deficits and educational loss in children with schistosome infection—A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 12, e0005524 (2018).
Schistosomiasis. https://www.who.int/news-room/fact-sheets/detail/schistosomiasis. Accessed 12 Oct 2020 (2020).
WHO. Investing to Overcome the Global Impact of Neglected Tropical Diseases: Third WHO Report on Neglected Tropical Diseases. (World Health Organization, 2015).
Kabuyaya, M., Chimbari, M. J. & Mukaratirwa, S. Efficacy of praziquantel treatment regimens in pre-school and school aged children infected with schistosomiasis in sub-Saharan Africa: A systematic review. Infect. Dis. Poverty. https://doi.org/10.1186/s40249-018-0448-x (2018).
Wilkinson, G. R. Drug metabolism and variability among patients in drug response. N. Engl. J. Med. 352, 2211–2221 (2005).
Ngaimisi, E. et al. Importance of ethnicity, CYP2B6 and ABCB1 genotype for Efavirenz pharmacokinetics and treatment outcomes: A parallel-group prospective cohort study in two sub-Saharan Africa populations. PLOS ONE. 8, e67946 (2013).
Maganda, B. A. et al. CYP2B6*6 genotype and high efavirenz plasma concentration but not nevirapine are associated with low lumefantrine plasma exposure and poor treatment response in HIV-malaria-coinfected patients. Pharmacogenom. J. 16, 88–95. https://doi.org/10.1038/tpj.2015.37 (2016).
Mugusi, S. et al. Impact of population and pharmacogenetics variations on Efavirenz pharmacokinetics and immunologic outcomes during anti-tuberculosis co-therapy: A parallel prospective cohort study in two sub-Sahara African populations. Front. Pharmacol. 11, 113 (2020).
Olliaro, P., Delgado-Romero, P. & Keiser, J. The little we know about the pharmacokinetics and pharmacodynamics of praziquantel (racemate and R-enantiomer). J. Antimicrob. Chemother. 69, 863–870 (2014).
Zdesenko, G. & Mutapi, F. Drug metabolism and pharmacokinetics of praziquantel: A review of variable drug exposure during schistosomiasis treatment in human hosts and experimental models. PLOS Negl. Trop. Dis. 14, e0008649 (2020).
Mnkugwe, R. H. et al. Effect of pharmacogenetics variations on praziquantel plasma concentrations and schistosomiasis treatment outcomes among infected school-aged children in Tanzania. Front. Pharmacol. 12, 712084 (2021).
Zdesenko, G., Mduluza, T. & Mutapi, F. Pharmacogenetics of praziquantel metabolism: Evaluating the cytochrome P450 genes of Zimbabwean patients during a schistosomiasis treatment. Front. Genet. 13, 122 (2022).
Rajman, I. et al. African genetic diversity: Implications for cytochrome P450-mediated drug metabolism and drug development. EBioMedicine. 17, 67–74 (2017).
Dandara, C. et al. African Pharmacogenomics Consortium: Consolidating pharmacogenomics knowledge, capacity development and translation in Africa. AAS Open Res. https://doi.org/10.12688/aasopenres.12965.1 (2019).
Bustinduy, A. L. et al. Population pharmacokinetics and pharmacodynamics of praziquantel in Ugandan children with intestinal schistosomiasis: Higher dosages are required for maximal efficacy. mBio https://doi.org/10.1128/mBio.00227-16 (2016).
Nleya, L. et al. The effect of ketoconazole on praziquantel pharmacokinetics and the role of CYP3A4 in the formation of X-OH-praziquantel and not 4-OH-praziquantel. Eur. J. Clin. Pharmacol. 75, 1077–1087 (2019).
Wang, H. et al. Metabolic profiling of praziquantel enantiomers. Biochem. Pharmacol. 90, 166–178 (2014).
Bains, R. K. African variation at cytochrome P450 genes evolutionary aspects and the implications for the treatment of infectious diseases. Evol. Med. Public Health 2013, 118–134 (2013).
Gebreyesus, T. D. et al. Prevalence, intensity, and correlates of schistosomiasis and soil-transmitted helminth infections after five rounds of preventive chemotherapy among school children in southern Ethiopia. Pathogens https://doi.org/10.3390/pathogens9110920 (2020).
Montresor, A. et al. The WHO dose pole for the administration of praziquantel is also accurate in non-African populations. Trans. R. Soc. Trop. Med. Hyg. 99, 78–81 (2005).
WHO. WHO Anthro Survey Analyser and Other Tools. https://www.who.int/tools/child-growth-standards/software. Accessed 7 June 2022 (2015).
Barry, A. et al. Effect of pharmacogenetic variations on praziquantel plasma concentration and safety outcomes among school children in Rwanda. Sci. Rep. https://doi.org/10.1038/s41598-023-28641-w (2023).
Gebeyehu, E. et al. Sex and CYP3A5 genotype influence total CYP3A activity: High CYP3A activity and a unique distribution of CYP3A5 variant alleles in Ethiopians. Pharmacogenom. J. 11, 130–137. https://doi.org/10.1038/tpj.2010.16 (2011).
Bedada, W. et al. Effects of Khat (Catha edulis) use on catalytic activities of major drug-metabolizing cytochrome P450 enzymes and implication of pharmacogenetic variations. Sci. Rep. 8, 12726. https://doi.org/10.1038/s41598-018-31191-1 (2018).
Ahmed, J. H. et al. CYP2J2∗7 genotype predicts risk of chemotherapy-induced hematologic toxicity and reduced relative dose intensity in Ethiopian breast cancer patients. Front. Pharmacol. 10, 481 (2019).
Lee, C. A. et al. Identification of novel substrates for human cytochrome P450 2J2. Drug Metab. Dispos. 38, 347–356 (2010).
Wu, Z. et al. CYP2J2 and CYP2C19 are the major enzymes responsible for metabolism of albendazole and fenbendazole in human liver microsomes and recombinant P450 assay systems. Antimicrob. Agents Chemother. 57, 5448 (2013).
Li, X.-Q. et al. Identification of human cytochrome P450s that metabolise anti-parasitic drugs and predictions of in vivo drug hepatic clearance from in vitro data. Eur. J. Clin. Pharmacol. 59, 429–442 (2003).
Solanki, M. et al. Cytochrome P450 2J2: Potential role in drug metabolism and cardiotoxicity. Drug Metab. Dispos. 46, 1053–1065 (2018).
Obach, R. S. Linezolid metabolism is catalyzed by cytochrome P450 2J2, 4F2, and 1B1. Drug Metab. Dispos. 50, 413–421 (2022).
Chamboko, C. R. et al. Human cytochrome P450 1, 2, 3 families as pharmacogenes with emphases on their antimalarial and antituberculosis drugs and prevalent African alleles. Int. J. Mol. Sci. 24, 3383 (2023).
Scandlyn, M. J., Stuart, E. C. & Rosengren, R. J. Sex-specific differences in CYP450 isoforms in humans. Exp. Opin. Drug Metab. Toxicol. 4, 413–424 (2008).
Sileshi, T. et al. Correlation of N-acetyltransferase 2 genotype and acetylation status with plasma isoniazid concentration and its metabolic ratio in Ethiopian tuberculosis patients. Sci. Rep. 13, 11438. https://doi.org/10.1038/s41598-023-38716-3 (2023).
Whitley, H. P. & Lindsey, W. Sex-based differences in drug activity. AFP 80, 1254–1258 (2009).
Soldin, O. & Mattison, D. Sex differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 48, 143–157 (2009).
Acknowledgements
We are grateful for the support and facilitation from the departments of health and education at regional, zonal and district offices. We also acknowledge the study participants, parents/guardians, and teachers at Bushulo, Kidus Pawulos, Finchawa and Wosha primary schools for their participation. We are also grateful for the technical assistance and support from Hawassa University Hospital management and laboratory professionals during blood sample collection and storage. We appreciate the unreserved support from the clinical trial and pharmacovigilance team of EFDA and south branch staff members during the conduct of this study.
Funding
Open access funding provided by Karolinska Institute. This study was funded by the European and Developing Countries Clinical Trials Partnership (EDCTP) 2 program supported by the European Union and the Swedish International Development Cooperation Agency (SIDA) as part of the Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa (PROFORMA) project (Grant number CSA2016S-1618).
Author information
Authors and Affiliations
Contributions
T.D.G., E.M., H.G., and M-L.D., E.A, designed the study; T.D.G., A.B., E.M. and E.A. participated in protocol development; T.D.G, participated in the sample collection; T.D.G., R.H.M., A.B., N.F. and E.A. participated in DNA extraction and genotyping; T.D.G., N.F, R.H.M., A.B., M-L.D and E.A. participated in the pharmacokinetics analysis (quantification of plasma concentration of PZQ and its major metabolites); T.D.G., N.F., R.H.M., A.B., H.G., E.M., M-L.D and EA participated in formal data analysis and interpretation; T.D.G. and N.F. wrote the original draft; T.D.G., N.F., A.B., R.H.M., E.M., H.G., M-L.D and EA reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gebreyesus, T.D., Makonnen, E., Telele, N.F. et al. CYP2C19 and CYP2J2 genotypes predict praziquantel plasma exposure among Ethiopian school-aged children. Sci Rep 14, 11730 (2024). https://doi.org/10.1038/s41598-024-62669-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62669-w
- Springer Nature Limited