Abstract
In prior investigations, a correlation was established between patient outcomes in locally advanced non-small cell lung cancer (LA-NSCLC) following thoracic irradiation and parameters, such as pre/post-treatment neutrophil-to-lymphocyte ratio (NLR) and NLR change (ΔNLR). However, these parameters could potentially be influenced by radiation-related variables, such as gross tumor volume (GTV). The primary aim of this study was to elucidate the factors impacting post-treatment NLR and ΔNLR and to further assess their prognostic relevance. In this retrospective study, a cohort of 188 LA-NSCLC patients who underwent thoracic radiation between 2012 and 2017 was assessed. The calculation of pre/post-treatment NLR involved the use of absolute neutrophil and lymphocyte counts. ΔNLR was defined as the difference between post- and pre-treatment NLR values. To assess the relationships between various variables and overall survival (OS), local progression-free survival (LPFS), and distant metastasis-free survival (DMFS), the Kaplan–Meier technique and Cox proportional hazards regression were employed. Additionally, Spearman’s rank correlation analysis was carried out to investigate correlations between the variables. The analysis revealed that both post-treatment NLR (r = 0.315, P < 0.001) and ΔNLR (r = 0.156, P = 0.032) were associated with GTV. However, OS, LPFS, and DMFS were not independently correlated with pre/post-treatment NLR. ΔNLR, on the other hand, exhibited independent associations with OS and DMFS (HR = 1.054, P = 0.020, and P = 0.046, respectively). Elevated ΔNLR values were linked to poorer OS (P = 0.023) and DMFS (P = 0.018) in the Kaplan–Meier analysis. Furthermore, when stratifying by GTV, a higher ΔNLR remained to be associated with worse OS and DMFS (P = 0.047 and P = 0.035, respectively) in the GTV ≤ 67.41 cm3 group, and in the GTV > 67.41 cm3 group (P = 0.028 and P = 0.042, respectively), highlighting ΔNLR as the sole independent predictive factor for survival and metastasis, irrespective of GTV.
Similar content being viewed by others
Introduction
Patients with unresectable, locally advanced non-small cell lung cancer (LA-NSCLC) significantly benefit from immunomaintenance treatment after chemoradiotherapy1,2,3. The effects of radiation on the body’s inflammatory state have noticeably attracted scholars’ attention because immunotherapy has been used more frequently as it may alter its effectiveness4. As one of the important markers of inflammation, neutrophil-to-lymphocyte ratio (NLR) has been widely studied, and it has been proven to have a predictive value for the prognosis5,6,7,8. As the immune state is not static and can be changed by radiotherapy and chemotherapy, the dynamic changes of NLR may provide more information compared to a single time-point NLR. However, few studies have concentrated on the impact of dynamic changes of NLR on prognosis. Besides, the prognostic significance of NLR remains controversial. Research has shown that higher pre-treatment NLR, post-treatment NLR, and NLR change (ΔNLR) were independent predictors of poor survival9. However, another study revealed that ΔNLR was correlated with overall survival (OS) and progression-free survival (PFS). While post-treatment NLR was solely a standalone predictor of PFS, baseline NLR was not associated with prognosis10. Therefore, the predictive significance of the dynamic change of NLR on the prognosis still needs further investigation. It is noteworthy that the abovementioned studies did not profoundly assess the influential factors of post-treatment NLR and ΔNLR. For instance, gross tumor volume (GTV) may affect post-treatment NLR and ΔNLR, and a larger baseline GTV was reported to be related to worse OS11. Further research is required to determine whether post-treatment NLR and ΔNLR are independent prognostic variables. The present research aimed to assess the influential factors of post-treatment NLR and ΔNLR and further explore their prognostic significance.
Methods
Patients
The study enrolled 188 patients with unresectable LA-NSCLC, including histologically-confirmed stage III, who were treated with radiotherapy at our hospital between 2012 and 2017. Prior to commencement, approval was granted by the Medical Ethics Committee of Cangzhou Hospital of Integrated Traditional Chinese and Western Medicine of Hebei Province (China). All experiments were performed in accordance with relevant guidelines and regulations. In addition, informed consent was obtained from participants and/or their legal guardians. The inclusion criteria were summarized as follows: age > 18 years, patients with non-small cell lung cancer (including squamous cell carcinoma, adenocarcinoma, or large cell carcinoma), patients with disease stage IIIA, IIIB, or IIIC (according to the eighth edition of the American Joint Committee on Cancer), and patients who had received conventionally fractionated radiotherapy and completed the course of treatment. Patients with second primary cancer, those with pleural effusion, those who had previously undergone surgery or radiation, and those who had received targeted treatment or consolidation immunotherapy were excluded from the study.
Data collection and calculation of specific variables
The electronic medical records were used to collect information on the following variables: age, sex, performance status score, smoking status, pathology, staging, treatment method, tumor (T) stage, lymph node (N) stage, presence or absence of positron emission tomography/computed tomography scans, absolute neutrophil count (ANC), absolute lymphocyte count (ALC). ANC and ALC from all 188 patients were collected before radiotherapy and after completion of the full radiotherapy protocol.
The pre-treatment ANC was divided by the pre-treatment ALC to calculate the pre-treatment NLR. Similarly, the post-treatment ANC was divided by the post-treatment ALC to determine the post-treatment NLR. The ΔNLR was derived by subtracting the pre-treatment NLR from the post-treatment NLR.
The radiation therapy (RT) method, radiation dosage, GTV, clinical target volume (CTV), planning target volume (PTV), mean lung dose, and mean heart dose data were extracted from the radiotherapy plan.
Radiotherapy
Three-dimensional conformal radiation therapy (3D-CRT), intensity-modulated radiation therapy (IMRT), and volumetric modulated arc therapy (VMAT) were the radiotherapy modalities used in the whole cohort, with a median dosage of 60 (range, 50–66) Gy.
Statistical analysis
The following clinical outcomes were evaluated in this study: OS, local progression-free survival (LPFS), and distant metastasis-free survival (DMFS). OS was computed from the moment of diagnosis to the final follow-up or the time of death from any cause. LPFS was defined as the time from diagnosis to local progression or death from any cause. DMFS was defined as the time from diagnosis to distant metastasis or death from any cause.
Both univariate and multivariate Cox proportional hazards regression analyses were conducted to assess the association between potential prognostic variables and outcomes. Variables with P value < 0.1 in the univariate analysis were subsequently included in the multivariate regression analysis. A stepwise forward method was utilized to compute the results of the multivariate analysis. As a result of the regression coefficients, hazard ratios (HRs) were obtained. The assessment of OS, LPFS, and DMFS was conducted using Kaplan–Meier analysis. ΔNLR was divided into two groups for Kaplan–Meier analysis. Potential associations between post-treatment NLR, ΔNLR, and other prognostic markers were assessed by calculating Spearman’s rank correlation coefficient. The standard distribution test was conducted for the two groups of ΔNLR stratified by GTV. Normally distributed data were analyzed by t-test. Abnormally distributed data were analyzed by the non-parametric test. Patients received intensity-modulated radiation therapy was performed as a subgroup to analysis in order to overcome the hetero geneity of the study population. Statistical analysis was carried out using SPSS 26.0 software (IBM, Armonk, NY, USA). P < 0.05 was considered statistically significant.
Results
Patients’ characteristics
Totally, 188 patients were finally involved in this study. The median follow-up time was 46.5 months, with a maximum follow-up time of 112.8 months. Regrettably, 70.74% of patients passed away. Table 1 lists patients’ characteristics. Besides, 66.0% of patients underwent brain magnetic resonance imaging and PET examination for tumor staging. Stage IIIA (54.3%), IIIB (41.5%), or IIIC (4.2%) was used to classify all patients. Moreover, 42.6% of tumors were found in the left lung and 57.4% in the right lung.
The relationship between variables
The median pre-treatment NLR was 2.10 (range, 0.09–10.62). The median post-treatment NLR was 4.80 (range, 0.22–33.91). The median ΔNLR was 2.60 (range, − 6.61–25.98). In the whole cohort, the median GTV was 67.41 (range, 5.39–326.0) cm3. Post-treatment NLR and GTV were linearly and positively associated together, according to the Spearman rank correlation (r = 0.315, P < 0.001) (Fig. 1A). After grouping post-treatment NLR according to the median GTV (67.41 cm3), the average post-treatment NLR of 4.99 (3.16 ± 0.33) in the GTV ≤ 67.41 cm3 group was significantly lower than that (6.85, 4.94 ± 0.51) in the GTV > 67.41 cm3 group (P = 0.002, Fig. 1B). Furthermore, ΔNLR and GTV exhibited to have a linear positive association together, according to the Spearman rank correlation (r = 0.156, P = 0.032, Fig. 1C). After grouping △NLR according to the median GTV (67.41 cm3), the mean ΔNLR in the GTV ≤ 67.41 cm3 group was 2.79 (3.01 ± 0.31), which was significantly lower than that in the GTV > 67.41 cm3 group (3.89, 4.79 ± 0.49) (P = 0.048, Fig. 1D).
The relationship between post-treatment NLR, ΔNLR and GTV (A) Spearman’s correlation coefficients for post–treatment NLR and GTV, (B) After grouping post–treatment NLR according to the median of GTV, (C) Spearman’s correlation coefficients for ΔNLR and GTV, (D) After grouping ΔNLR according to the median of GTV.
The association of variables with prognosis
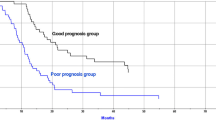
With median durations of 25.3, 20.4, and 36.1 months, the 5-year OS, LPFS, and DMFS rates were 24.4, 28.3, and 31.8%, respectively. A larger GTV was strongly correlated with OS, LPFS, and DMFS based on the results of univariate analysis. OS and DMFS were significantly correlated with the increased post-treatment NLR and ΔNLR. However, pre-treatment NLR was found irrelevant to OS, LPFS, or DMFS (Table 2). The results of multivariate analysis indicated that a larger GTV was associated with worse OS, LPFS, and DMFS, while a greater ΔNLR indicated a significant correlation with worse OS and DMFS. It is also noteworthy that multivariate analysis did not reveal any associations between post-treatment NLR and OS or DMFS (Table 3). For further research, Kaplan–Meier analysis was used to dichotomize ΔNLR; a greater ΔNLR was linked to worse OS (P = 0.023, Fig. 2A) and DMFS (P = 0.018, Fig. 3A). Median values of OS and DMFS in the low ΔNLR group (27.2 months, 95% confidence interval (CI): 22.2–32.2 and 43.8 months, 95%CI 34.7–52.9 months, respectively) were higher than those in the high post-treatment NLR group (20.7 months, 95%CI 15.7–25.8 and 26.2 months, 95% CI 23.2–29.2 months, respectively).
In the univariate analysis and Kaplan–Meier analysis, GTV was utilized as a stratification factor since the association between ΔNLR and GTV could affect the prognostic function of ΔNLR. After using GTV as a stratification factor in the univariate analysis, a significant association was identified between ΔNLR and OS (HR = 1.058, P = 0.007). ΔNLR was correlated with OS in the GTV ≤ 67.41 cm3 group (P = 0.047, Fig. 2B) and the GTV > 67.41 cm3 group (P = 0.028, Fig. 2C) when ΔNLR was dichotomized on the Kaplan–Meier analysis. After incorporating GTV as a stratification factor in the univariate analysis, the association between ΔNLR and DMFS remained significant (HR = 1.057, P = 0.031). When ΔNLR was dichotomized for the Kaplan–Meier analysis, ΔNLR was correlated with DMFS in both the GTV ≤ 67.41 cm3 (P = 0.035, Fig. 3B) and GTV > 67.41 cm3 groups (P = 0.042, Fig. 3C).
In the subgroup analysis of patients received intensity-modulated radiation therapy, The results of univariate analysis (S Table 1) and multivariate analysis (S Table 2) were similar to those of the whole population.
Discussion
In the present research, the determinants of post-treatment NLR and ΔNLR in patients with thoracic radiotherapy-treated LA-NSCLC were investigated. After incorporating the covariates, the prognostic significance of pre-treatment NLR, post-treatment NLR, and ΔNLR was subsequently evaluated. It was found that GTV was associated with post-treatment NLR and ΔNLR. In the multivariate analysis, ΔNLR was regarded as an independent predictor of OS and DMFS after GTV addition. Besides, there was no statistically significant difference between pre-treatment NLR, post-treatment NLR, and prognosis.
Inflammation and the growth and metastasis of tumors are tightly connected12,13,14, and it is more important to explore the impact of inflammatory status on prognosis with the widely application of immunotherapy in lung cancer. NLR has been widely studied as one of the important markers of inflammation. However, the predictive value of NLR for the prognosis of LA-NSCLC needs further exploration especially in the era of immunotherapy. In NSCLC patients with stage II and stage III who received radical intensity-modulated radiation therapy, prior research has shown that a lower baseline NLR indicates higher rates of PFS and OS15. Conversely, baseline NLR was confirmed to have no association with OS in III NSCLC patients, of whom 115 (35%) patients underwent surgical resection, followed by chemotherapy or chemoradiotherapy, and the remaining 217 (65%) patients received synchronous CRT16. Furthermore, baseline NLR was not associated with prognosis in stage IIB-IIIC NSCLC patients receiving radical radiotherapy17. Similarly, pre-treatment NLR and OS, LPFS, and DMFS were not correlated together in the present research (P = 0.464, 0.654, and 0.821, respectively). This result was not surprising because the immune state is dynamic, which can be changed by radiotherapy or chemotherapy. It is broadly accepted that radiotherapy is one of the main treatment methods for LA-NSCLC, which can not only directly kill tumor cells, but also impact the body's immune system18. Relevant studies have revealed that radiation can reduce the number of peripheral blood immune cells, especially lymphocytes. Lymphocytes are more sensitive to radiation, in which 50% lethal dose is as low as 2 Gy19, and 0.5 Gy can cause DNA damage20,21. Thus, the number of lymphocytes can be significantly reduced by radiotherapy22,23. Therefore, post-treatment NLR and ΔNLR may provide more information on the prognosis than pre-treatment NLR, and further determining its predictive value is more meaningful. Post-treatment NLR and ΔNLR were previously found as independent predictors of poor survival in NSCLC patients following radical radiation therapy9. Besides, NLR at four months after radiotherapy was also associated with OS6. Consistently, the data of stage III NSCLC patients treated with radiation therapy and chemotherapy were related to the post-treatment NLR7. High postoperative NLR was an independent unfavorable prognostic factor in patients with LA-NSCLC who were treated with surgery after chemoradiotherapy with or without postoperative adjuvant chemotherapy24. In patients receiving concomitant chemoradiotherapy, ΔNLR was reported as a standalone predictor of OS and PFS10. Further research revealed that PFS and OS in Kaplan–Meier survival analysis were correlated with post-treatment NLR and ΔNLR. Additionally, the results of multivariate analysis indicated that post-treatment NLR could only be utilized as an independent predictor of PFS, whereas ΔNLR was noted as an independent predictor of PFS and OS25.
To some extent, the abovementioned studies suggest that the post-treatment NLR and the ΔNLR after treatment are associated with prognosis. It is worth noting that the majority of the prognostic indicators used in the aforementioned studies are OS and PFS. The body’s immune status may be highly correlated with DMFS. Furthermore, previous investigations did not consider putative post-treatment NLR and ΔNLR determinants (e.g., GTV size), which may affect the outcomes. In earlier trials, a significant baseline GTV was linked to poorer OS and PFS26,27,28. Hence, it is necessary to explore the predictive significance of post-treatment NLR and ΔNLR excluding the influence of GTV and add DMFS as a prognostic indicator. This study was revealed that GTV was a standalone unfavorable prognostic factor for OS, LPFS, and DMFS; of note, a larger GTV was associated with higher values of post-treatment NLR and △NLR. This could be attributed to the more extensive radiation range of the larger GTV group. A more extensive radiation range signifies more exposure of immune cells and a more significant reduction in the number of lymphocytes. Therefore, the prognostic significance of pre-treatment NLR, post-treatment NLR and ΔNLR after GTV addition remains to be further verified. It is noteworthy that although the univariate analysis showed that post-treatment NLR was associated with OS and DMFS, no statistically significant difference was found in the results of the multivariate analysis. Additionally, ΔNLR remains a separate prognostic factor for OS and DMFS when GTV is taken into account in the multivariate analysis. Furthermore, ΔNLR exhibited to have no association with LPFS. The conjecture is that GTV is more closely correlated with local control, and the severity of compromised immune system is associated with the distant metastasis of the tumor. The Kaplan–Meier survival analysis also supported these results. These results indicate that ΔNLR is more closely correlated with prognosis, especially it discovered the connection of ΔNLR and DMFS which different from other studies. This result suggests that the immune status of the body is crucial for controlling of the systemic tumors, and it is very meaningful especially in the era of immunotherapy. It is well known that although immune maintenance therapy after radiochemotherapy has improved the efficacy, The 12-, 24- and 36- month OS rates with durvalumab were 83.1, 66.3, and 57.0%1,2,3, and there is significant population heterogeneity. Therefore, it is necessary to further stratify and develop more accurate treatment methods. The results of this study .indicating that ΔNLR may serve as a stratified indicator to assist clinical differentiation of beneficiary populations and the development of more accurate treatment decisions.
Because of the significant heterogeneity of the population and the majority of people receiving intensity-modulated radiation therapy (81.9%), we performed subgroup analysis. However, the results indicate that ΔNLR is also correlated with OS and DMFS whicn similar to those of the whole population.
Although the present research established the association between ΔNLR and GTV, and it also confirmed the prognostic value of ΔNLR in stage LA-NSCLC, there are some limitations that should be pointed out. Firstly, this research inherently involved selection bias owing to its retrospective design. Secondly, NLR might be influenced by potential confounding factors (e.g., possible infection and chemotherapy regimen). Thirdly, the potential variations in salvage therapies may have inadvertently influenced the outcomes. Finally, this was a single-center study, and findings should be verified externally in future research.
Conclusions
In conclusion, post-treatment NLR and ΔNLR were found to be associated with GTV. The impact of ΔNLR on survival and metastasis remained noticeable when GTV was analyzed. Furthermore, there was no statistically significant difference between pre-treatment NLR, post-treatment NLR, and prognosis. Further research should be conducted to clarify the prognostic significance of ΔNLR.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Antonia, S. J. et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N. Engl. J. Med. 377(20), 1919–1929 (2017).
Gray, J. E. et al. Three-year overall survival with durvalumab after chemoradiotherapy in stage III NSCLC-update from PACIFIC. J. Thorac. Oncol. 15(2), 288–293 (2020).
Faivre-Finn, C. et al. Four-year survival with durvalumab after chemoradiotherapy in stage III NSCLC-an update from the PACIFIC trial. J. Thorac. Oncol. 16(5), 860–867 (2021).
Ohri, N. et al. Who benefits the most from adjuvant durvalumab after chemoradiotherapy for non-small cell lung cancer? An exploratory analysis. Pract. Radiat. Oncol. 11(2), e172 (2021).
Scilla, K. A. et al. Neutrophil-lymphocyte ratio is a prognostic marker in patients with locally advanced (Stage IIIA and IIIB) non-small cell lung cancer treated with combined modality therapy. Oncologist 22(6), 737–742 (2017).
Thor, M. et al. Are unsatisfactory outcomes after concurrent chemoradiotherapy for locally advanced non-small cell lung cancer due to treatment-related immunosuppression?. Radiother. Oncol. 143, 51–57 (2020).
Palomar-Abril, V. et al. Dynamic evaluation of neutrophil-to-lymphocyte ratio as prognostic factor in stage III non-small cell lung cancer treated with chemoradiotherapy. Clin. Transl. Oncol. 22(12), 2333–2340 (2020).
Łochowski, M. et al. Prognostic value of neutrophil-to-lymphocyte, platelet-to-lymphocyte and lymphocyte-to-monocyte ratio ratios in patients operated on due to non-small cell lung cancer. J. Thorac. Dis. 11(8), 3377–3384 (2019).
Punjabi, A. et al. Neutrophile lymphocyte ratio and absolute lymphocyte count as prognostic markers in patients treated with curative-intent radiotherapy for non-small cell lung cancer. Clin. Oncol. 33(8), e331–e338 (2021).
Guo, M. et al. Prognostic value of delta inflammatory biomarker-based nomograms in patients with inoperable locally advanced NSCLC. Int. Immunopharmacol. 72, 395–401 (2019).
Kwinta, M. et al. The prognostic value of volumetric changes of the primary tumor measured on Cone Beam-CT during radiotherapy for concurrent chemoradiation in NSCLC patients. Radiother. Oncol. 146, 44–51 (2020).
Shadab, A. et al. Divergent functions of NLRP3 inflammasomes in cancer: A review. Cell Commun. Signal. 21(1), 232 (2023).
Jiao, Z. Y. & Zhang, J. Interplay between inflammasomes and PD-1/PD-L1 and their implications in cancer immunotherapy. Carcinogenesis 44, 795–808. https://doi.org/10.1093/carcin/bgad072 (2023).
Li, X. et al. The immunological and metabolic landscape in primary and metastatic liver cancer. Nat. Rev. Cancer 21(9), 541–557 (2021).
Li, Y. et al. Higher aorta dose increased neutrophil-to-lymphocyte ratio resulting in poorer outcomes in stage II–III non-small cell lung cancer. Thorac. Cancer. 14(6), 555–562 (2023).
Tong, Y. S., Tan, J., Zhou, X. L., Song, Y. Q. & Song, Y. J. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J. Transl. Med. 15(1), 221 (2017).
Ozkan, E. E., Kaymak Cerkesli, Z. A. & Erdogan, M. Predictive value of immune-inflammation indices in metabolic response and outcome after curative radiotherapy in patients with non-small cell lung cancer. Clin. Respir. J. 14(9), 849–856 (2020).
Yin, X. et al. Is a higher estimated dose of radiation to immune cells predictive of survival in patients with locally advanced non-small cell lung cancer treated with thoracic radiotherapy?. Radiother. Oncol. 159, 218–223 (2021).
Nakamura, N., Kusunoki, Y. & Akiyama, M. Radiosensitivity of CD4 or CD8 positive human T-lymphocytes by an in vitro colony formation assay. Radiat. Res. 123, 224–227 (1990).
Heylmann, D., Rödel, F., Kindler, T. & Kaina, B. Radiation sensitivity of human and murine peripheral blood lymphocytes, stem and progenitor cells. Biochim. Biophys. Acta (BBA) Rev. Cancer 1846, 121–129 (2014).
Sellins, K. S. & Cohen, J. J. Gene induction by gamma-irradiation leads to DNA fragmentation in lymphocytes. J. Immunol. 139, 3199–3206 (1987).
Kobzeva, I. et al. Effect of radiation therapy on composition of lymphocyte populations in patients with primary breast cancer. J. Pers. Med. 13(9), 1399 (2023).
Paganetti, H. A review on lymphocyte radiosensitivity and its impact on radiotherapy. Front. Oncol. 13, 1201500 (2023).
Tsudaka, S. et al. Prognostic significance of neutrophil-to-lymphocyte ratio in locally advanced non-small-cell lung cancer treated with trimodality therapy. Ann. Surg. Oncol. 28(9), 4880 (2021).
Wang, D. et al. The post-treatment neutrophil-to-lymphocyte ratio and changes in this ratio predict survival after treatment of stage III non-small-cell lung cancer with conventionally fractionated radiotherapy. Future Oncol. 16(9), 439–449 (2020).
Nygard, L. et al. A competing risk model of first failure site after definitive chemoradiation therapy for locally advanced non-small cell lung cancer. J. Thorac. Oncol. 13, 559–567 (2018).
Edith, M. T. et al. Concurrent daily cisplatin and high-dose radiation therapy in patients with stage III non-small cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 102(3), 543–551 (2018).
Zhou, R. et al. Radiation dose, local disease progression, and overall survival in patients with inoperable non-small cell lung cancer after concurrent chemoradiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 100(2), 452–461 (2018).
Author information
Authors and Affiliations
Contributions
X.Y. and H.C. wrote the manuscript, and they contributed to data collection and anslysis. L.X., H.L., W.G., H.Y., J.Z., K.F. and W.L. provided the enrolled cases. Y.S. designed the study and provided administrative support. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, X., Chen, H., Sun, Y. et al. Prognostic value of neutrophil-to-lymphocyte ratio change in patients with locally advanced non-small cell lung cancer treated with thoracic radiotherapy. Sci Rep 14, 11984 (2024). https://doi.org/10.1038/s41598-024-62662-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62662-3
- Springer Nature Limited