Abstract
This study aimed to examine the interaction between diet quality indices (DQIs) and smoking on the incidence of hypertension (HTN), stroke, cardiovascular diseases, and all-cause mortality. We prospectively followed 5720 participants and collected dietary data via a validated food frequency questionnaire to calculate DQI-international (DQI-I) and DQI-revised (DQI-R). Considering an interaction analysis, we classified participants based on diet quality (median: higher/lower) and smoking status. Over 9 years of follow-up, higher diet quality scores were associated with a lower risk of stroke and mortality. While current smokers had a higher risk of stroke and mortality but had a lower risk of developing HTN. Compared to the current smokers with lower diet quality, nonsmokers with higher diet quality according to the DQI-I [HR 0.24; 95% CI (0.08, 0.66)], and DQI-R [HR 0.20; 95% CI (0.07, 0.57)] had a lower risk of stroke. Moreover, the lower risk of mortality was more evident in nonsmokers with higher DQI-I [HR 0.40; 95% CI (0.22–0.75)] and DQI-R scores [HR 0.34; 95% CI (0.18–0.63)] compared to nonsmokers with lower diet quality. While higher DQI-I and DQI-R scores were associated with a lower risk of stroke and mortality, this beneficial effect may be negated by smoking.
Similar content being viewed by others
Introduction
Non-communicable diseases (NCDs), particularly cardiovascular diseases (CVDs), represent the predominant global cause of mortality1. Iran has a high prevalence rate of CVD (> 9000 cases per 100,000 individuals), accounting for almost half of the mortalities and contributing to 20–23% of the overall disease burden2. Notably, hypertension (HTN) has emerged as the leading contributor to CVDs incidence, affecting one in every four Iranians3,4. While smoking and poor diet are recognized as the primary contributors to mortality risk5, it has been shown that CVDs can be managed through dietary and lifestyle behaviors6,7.
Smoking contributes to nearly 25% of annual stroke incidents and approximately 15% of stroke-related mortality8,9. Cigarette smoking has a pronounced effect on males, adults ranging from 18 to 44 years old, individuals with lower socioeconomic status, and residents of developing nations10,11. Evidence suggests that smokers with poorer nutritional status have a twofold higher risk of developing CVDs12,13. Smokers often adopt unhealthy dietary habits, like lower intake of fruits and vegetables and higher consumption of fats and alcohol14,15. The mutually influencing disease-causing mechanisms common to both smoking and poor diet quality can interact progressively, indicating the higher potential risk of NCDs over time16. Meanwhile, the optimal method for considering associations and interactions among dietary components is to assess overall diet quality17. Dietary quality indices (DQIs) offer a thorough approach to assessing dietary behaviors with an emphasis on dietary variety, dietary moderation, balanced nutrient intake, and diverse food choices18.
Several studies have individually examined the impact of dietary factors or smoking on health risks. Still, there is a notable gap in research exploring how these factors might interact and influence health outcomes. Previous studies have indicated that a higher score on the DQIs is linked to lower levels of inflammatory markers, which are known risk factors for CVDs19. Furthermore, a higher score on these indices has been associated with higher levels of high-density lipoprotein-cholesterol (HDL-C), which is a protective factor against CVDs20. However, few studies have explored the relationship between these indices and the risk of CVDs. Additionally, while smoking is a well-known risk factor for CVD incidence, some studies have suggested a lower risk of HTN among smokers21. Besides, studies examining the diets of smokers predominantly focused on individual dietary components rather than assessing overall dietary patterns22,23. To the best of our knowledge, there are no studies investigating the interaction between a high-quality diet as a protective factor and smoking as a risk factor for CVDs risk, particularly in the Middle East and North Africa (MENA) region.
Considering the conflicting results and limited available data, this study can contribute to shaping more effective recommendations and dietary guidelines for the management of CVDs outcomes. Hence, this study was conducted to investigate the associations between diet quality, smoking, and their interactions with the incidence of HTN, stroke, CVDs, and all-cause mortality.
Results
The mean age ± SD of the participants recruited for the study of cardiovascular events was 46.42 years, and 44.8% were men. The baseline characteristics of the study participants based on diet quality and smoking status are reported in Table 1. In the total population, the mean ± SD of DQI-I and DQI-R were 63.41 ± 7.98 and 71.20 ± 12.61, respectively. Based on both DQI-I and DQI-R, individuals with higher vs. lower diet quality showed a higher proportion of men, and had higher mean age, education level, FBS, TG, SBP levels, and energy intake. Individuals with higher DQI-I had lower levels of HDL-C and employment rate. Also, those with higher DQI-R had higher BMI and higher physical activity levels compared with those with lower DQI-R. Compared to non-smokers, current smokers had significantly a higher percentage of men and TG levels, while mean age, BMI, physical activity, and HDL-C levels were significantly lower in the current smokers compared to non-smokers. Moreover, the energy intake was higher, and both quality diet scores were lower for current smokers than non-smokers.
Supplementary Table S1 displays the baseline characteristics of the study participants recruited for the study of HTN. The mean age ± SD of the participant's age was 38.25 years, and 42.6% were men. The total population had the mean ± SD of DQI-I and DQI-R of 62.43 ± 8.03 and 70.00 ± 12.81, respectively. Considering the DQI-I and DQI-R, participants with higher diet quality, had a higher percentage of men, higher mean age and BMI, higher physical activity and education level, higher energy intake, and exhibited higher levels of FBS, TC, TG, and SBP. According to the DQI-I, participants with higher diet quality had a lower HDL-C level. Compared to non-smokers, current smokers were more likely to be male, had a higher age, higher physical activity level, higher levels of TC, TG, SBP, and higher energy intake, however, they had lower HDL-C, lower scores of DQI-I and its components including variety and moderation, and also lower DQI-R score and its moderation score.
After a mean follow-up of 9.0 years, 357 cases of CVDs (7.1%), 54 cases of stroke (1.1%), and 131 cases of mortality (2.6%) were ascertained. Also, considering the HTN outcome, 1032 cases of HTN (18%) were recorded after a mean follow-up period of 7.8 years. Our results indicated the robust accuracy of the multivariable models in predicting the incidence of the investigated outcomes. The Harrel’s C index scores for the associations between smoking and HTN (0.792), smoking and stroke (0.880), smoking and CVDs (0.823), smoking and mortality (0.847), DQI-I and HTN (0.791), DQI-I and stroke (0.895), DQI-I and CVDs (0.823), DQI-I and mortality (0.846), DQI-R and HTN (0.791), DQI-R and stroke (0.895), DQI-R and CVDs (0.823), and DQI-R and mortality (0.849) signify their predictive capability. Considering the interaction between diet quality and smoking, the multivariable models exhibited good predictive power concerning the incidence of HTN (DQI-I = 0.791, DQI-R = 0.791), stroke (DQI-I = 0.887, DQI-R = 0.887), CVDs (DQI-I = 0.823, DQI-R = 0.823), and all-cause mortality (DQI-I = 0.849, DQI-R = 0.851).
Table 2 represents the HR and 95% CI for cardiovascular events, all-cause mortality, and HTN across quartiles of DQIs. The higher DQI-I and DQI-R scores were associated with a higher risk of total cardiovascular events in the crude model but after accounting for covariates in model 1 and model 2, the associations became non-significant. The hazard of stroke decreased significantly across quartiles of DQI-I and DQI-R in both adjusted models. Compared with those in the first quartile of DQI-I and DQI-R, the fully adjusted HRs (95% CIs) were 0.37 (0.17, 0.82) and 0.33 (0.15, 0.72), respectively. The hazard of the all-cause mortality also decreased across the quartiles of DQI-I and DQI-R in the adjusted models; the fully adjusted HR (95% CI) in those in the highest quartile compared to first quartile was 0.57 (0.34, 0.97) for DQI-I and 0.51 (0.30, 0.86) for DQI-R. The hazard of HTN increased significantly across quartiles DQI-I (P trend = 0.001) and DQI-R (P trend = 0.003) in the unadjusted model but by inclusion of covariates in models 1 and 2 the associations became non-significant.
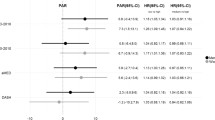
Figure 1 indicates the hazard ratio for incidence of CVDs, stroke, mortality, and HTN in current smokers compared with non-smokers. In the crude model, the risk of all-cause mortality was significantly higher in the current smokers than non-smokers [HR 1.87, 95% CI (1.19–2.93)]; the association remained significant in the final adjusted model [HR 2.11; 95% CI (1.30–3.45)]. A significantly increased risk of stroke was also observed in the current smokers than the non-smokers after accounting for all potential covariates [HR 2.32; 95% CI (1.06–5.10)]. The risk of HTN was significantly lower in the current smokers compared to non-smokers in the fully adjusted model [HR 0.77; 95% CI (0.62–0.96)].
Table 3 displays the HR (95% CI) for cardiovascular events, all-cause mortality, and HTN based on the combined effects of diet quality and smoking status. No significant interaction (P interaction > 0.05) was noted among the studied groups concerning cardiovascular events, all-cause mortality, and HTN. Compared to current smokers with poor diet quality, the hazard (95% CI) of stroke was 0.23 (0.08, 0.63) in adjusted model 1 and 0.24 (0.08, 0.66) in the adjusted model 2 in non-smokers with good diet quality based on DQI-I. A lower risk of stroke was also observed in non-smokers with good diet quality based on DQI-R compared to current smokers with poor diet quality in the adjusted models. The risk of all-cause mortality was significantly lower in both non-smokers’ groups with higher or lower diet quality compared to the current smokers with poor diet quality in the crude model and after adjusting for potential covariates. The hazard of HTN was not significantly different across the combined groups.
Discussion
The current study revealed that a high-quality diet was linearly associated with a lower risk of stroke and mortality. Compared to non-smokers, current smokers had an higher risk of stroke, CVDs, and mortality, and a lower risk of HTN. Additionally, non-smokers with higher diet quality had a lower risk of stroke compared to current smokers with lower diet quality. Non-smokers experience a lower risk of mortality than current smokers with lower diet quality. Notably, the lower risk for stroke and all-cause mortality was more pronounced in non-smokers with higher diet quality than in those with lower diet quality.
The similarities in the associations between the DQI-I and the DQI-R with the studied outcomes are likely attributable to similarities in their food and nutrient components. In general, higher DQI-I and the DQI-R scores indicate a healthier diet, characterized by a variety of food choices, adequate intake of fruits, vegetables, grains, and micronutrients, and suitable percentages of total energy intake for total fat, saturated fats, and high-calorie foods. Additionally, the DQI-R considers moderation of alcohol consumption, which makes it valuable in populations where alcohol use is either excessive or contraindicated. Although both indices evaluate an approximately equal number of dietary components, the DQI-I encompasses a broader spectrum of dietary aspects compared to the DQI-R. In contrast to the DQI-R, the DQI-I assesses the adequacy of fiber, protein, and vitamin C intake, as well as the balance in ratios between macronutrients and fatty acids.
Despite the limited number of studies examining the link between diet quality, as assessed by the DQIs, and the incidence of CVDs and all-cause mortality, our findings contribute additional evidence supporting the role of overall diet quality in the prevention of CVDs outcomes. In a study conducted within the framework of the Korean National Health and Nutrition Examination Surveys, it was observed that, based on DQI-I, individuals with CVDs exhibited a lower diet quality in comparison to those without CVDs24. Abdurahman et al. reported that a lower DQI-I score was linked to a higher risk of metabolic syndrome and its components, particularly hypertriglyceridemia, and reduced HDL-C levels among obese adults25. A cross-sectional study conducted by Shiraseb et al. revealed an inverse association between the DQI-I score and serum inflammatory biomarkers19. However, a cross-sectional study by Daneshzad et al. revealed no significant association between DQI-I score and cardiovascular disease risk factors in type 2 diabetic women, possibly due to low statistical power. Of note, it has been suggested that different ratings of DQIs for evaluating diet quality in different populations, such as diabetic patients, be created26.
Current smokers seem to exhibit a lower risk of HTN compared to non-smokers. Previous studies suggest that the lower risk of HTN in current smokers is attributed to higher levels of physical activity and lower weight of smokers. Khodamradi et al., following a 20-year follow-up, implied that the lower risk of HTN among smokers may be linked to their increased participation in work-related activities21. Besides, smoking can impact the hypothalamus, leading to appetite suppression, reduced dietary intake, and elevated catecholamine levels. This results in higher energy consumption in peripheral tissues and, ultimately, a lower body weight for smokers27. However, smoking causes a temporary increase in blood pressure, which returns to normal levels after 20 min of smoking10. According to data from the CARDIA (Coronary Artery Risk Development in Young Adults) study, the detrimental effects of smoking on blood pressure changes and pulse pressure (as calculated by subtracting DBP from SBP) are more pronounced than those of blood pressure levels alone. Notably, cigarette smoking can cause stiffness in large elastic arteries, like the aorta. This stiffness disrupts the ability of vessels to adjust to pressure changes during systole and diastole. Although there was no significant difference between blood pressure levels in current and non-smokers, the acute increase in blood pressure coupled with the progression of atherosclerosis may amplify the likelihood of unfavorable outcomes for smokers28.
The risk of stroke in comparison to other CVDs events, was significantly higher among current smokers. Findings from the Atherosclerosis Risk in Communities (ARIC) study indicate relative risks for lacunar and cardioembolic strokes in current smokers of 2.30 and 1.94, respectively29. In addition, Kawachi et al. demonstrated that, within the framework of the Nurse's Health Study, nurses who smoke are almost three times more likely to experience a stroke30. The elevated risk associated with smoking and stroke is attributed to factors like increased atherosclerotic plaque formation, heightened thrombosis, reduced cerebral perfusion, facilitation of aneurysm formation and rupture, structural damage to the arterial wall, carboxyhemoglobinemia, heightened platelet aggregability, and elevated fibrinogen levels31. Additionally, in animal models, a constituent of environmental tobacco smoke like 1,3-butadiene, can accelerate atherosclerosis, further linking smoking to CVDs risk10.
Previous studies have presented contrasting perspectives regarding the interaction effects of diet and smoking on health outcomes. One perspective suggests that, due to smokers' weakened nutritional and clinical status, a healthy diet is expected to have more pronounced effects on smokers than non-smokers32. In addition, in alignment with our study's results, smoking emerged as an effect modifier in the association between diet quality and NCDs. In other words, smoking might diminish the potential beneficial impact of a high-quality diet. Geng et al. reported an increased risk of CVDs mortality in individuals who were genetically prone to smoking and who also had lower DASH (dietary approach to stop hypertension) scores7. Moreover, Margetts et al. suggested that the risk of oxidative damage is elevated in smokers due to a combination of insufficient nutrient intake and the impact of smoking on nutrient metabolism33. Of note, smoking and a low-quality diet contribute to CVDs development through shared pathways like endothelial dysfunction and inflammation34. While increased TG and decreased HDL-C levels are the main characteristics of metabolic syndrome in smokers35, previous studies have established a direct association between adherence to a high-quality diet, assessed by the DQI-I, and higher serum HDL-C levels20. A recent study by Noruzzadeh et al. suggests that among current smokers, individuals with higher diet quality experience a lower risk of all-cause mortality compared to current smokers with lower diet quality36. Additionally, the study found that this lower risk associated with higher diet quality was more pronounced among former smokers36. Although some studies emphasize the essential role of nutrition in overall health, they suggest that diet may not influence the relationship between smoking and disease. Li and colleagues suggested that the severity of asthma symptoms in smokers was not influenced by the quality of their diet37. In contrast, a high-quality diet, as measured by the Alternative Healthy Eating Index 2010, was linked to a decrease in the severity of asthma symptoms in nonsmokers37. Millen et al. suggested that smokers who adopt heart-healthy dietary modifications may have certain advantages, but their risk of CVDs and all-cause mortality remains higher compared to non-smokers who also follow a heart-healthy diet6. Of note, DQIs are a measure of overall dietary quality in the general population, but considering the specific health condition of smokers, different ratings of DQIs or other dietary indices designed to correct these conditions may be more suitable in preventing CVDs incidence and all-cause mortality. It is crucial to acknowledge that our results may be susceptible to residual confounding from smoking-related factors, including smoking intensity and duration.
This study has notable strengths, including an extended follow-up duration, an investigation of the combined impact of diet quality and smoking, the use of validated and reproducible FFQ to collect dietary data, and control for various potentially confounding variables. Nevertheless, this study has considerable limitations. Like all observational studies, it may be susceptible to measurement bias. Additionally, due to the lack of available data, alcohol consumption was not incorporated as a food component in the computation of the DQI-R. Last, as an observational study, it cannot fully eliminate the impact of all potential residual confounding variables.
Based on our findings, it appears that smoking may counteract the benefits of a high-quality diet within the general population. Furthermore, existing literature suggests that the dietary habits of current smokers could influence their mortality risk. Given the limitations of this study, future studies could explore the interaction between diet quality and smoking across diverse populations. Employing alternative interaction indices like the relative excess risk due to interaction (RERI) and synergy index (SI) may provide deeper insights into their combined impact on health outcomes. Furthermore, employing restricted cubic splines (RCS) analysis to assess the relationship between smoking intensity (measured by the number of cigarettes per day) and duration (pack-years) and health-related outcomes could yield more precise estimates of the impact of smoking on health risks. Given the observed interaction between higher diet quality and smoking regarding health outcomes, future nutrition studies should acknowledge smoking as a significant confounding variable. Also, considering the detrimental impact of smoking on overall mortality and the incidence of CVDs, strategies such as smoking cessation programs, smoking reduction initiatives, and the implementation of smoking bans in public areas can prove effective in alleviating the smoking-related burden of diseases.
In conclusion, following a high-quality diet can be associated with a lower risk of stroke and all-cause mortality, however, these beneficial effects may be eliminated by the adverse impact of smoking. Further research in different populations is warranted to examine the individual and combined effects of dietary quality indices and smoking on the risk of NCDs.
Methods
Study population
The current investigation was carried out within the Tehran Lipid and Glucose Study (TLGS) outline. The TLGS is an ongoing population-based research initiative designed to identify risk factors for NCDs and advocate for healthier lifestyles. Since 1999, six examinations, involving 15,005 participants who undergo routine physical examinations, laboratory tests, and updates to their medical histories every three years, have been conducted38.
In the third examination of the TLGS (2006–08), 3686 individuals were chosen at random for dietary assessment. In the subsequent fourth examination (2009–2011), 7956 individuals were randomly selected and participated in the dietary assessment. For the present study, participants with complete dietary intake data from the third examination and those newly enrolled in the fourth examination were considered. Notably, participants from the third examination who exhibited under-reporting or over-reporting of energy intake (≤ 800 kcal/day and ≥ 4200 kcal/day, respectively) were excluded (n = 233). However, if their energy intake fell within the normal range at the fourth examination (n = 100), their dietary data from the fourth examination were considered baseline dietary data. After excluding individuals with over- or under-reports of energy intake in the fourth examination (n = 502), a total of 8914 participants with complete dietary intake data were included.
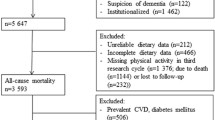
For the HTN outcome, exclusions were made for individuals aged < 18 years (n = 1270), individuals with any type of CVDs (n = 408), history of cancer (n = 35), pregnant or lactating women (n = 154), individuals with missing data on HTN status (n = 52), and those who were hypertensive at baseline (n = 1276). It is worth noting that some participants may belong to more than one exclusion category. Additionally, 299 participants were lost to follow-up, resulting in 5720 participants remaining for the final analysis of the HTN incident (Fig. 2).
Concerning the incidence of CVDs, and all-cause mortality, among the 5532 individuals aged ≥ 30 years, exclusions were made for those with any type of CVD (n = 383), a history of cancer (n = 32), pregnancy or lactation (n = 70) at the baseline of the study. Of note, some participants may belong to more than one exclusion category. Ultimately, a total of 5048 participants, free of CVDs were included in the study (Fig. 2) and were followed up until March 20, 2018, for the analysis of CVDs, and all-cause mortality.
Dietary assessment
Nutrition specialists collected dietary intake data by employing a validated semi-quantitative food frequency questionnaire (FFQ) comprising 168 items39. This questionnaire assessed the frequency of participants' food consumption over the preceding year, categorizing responses into daily, weekly, or monthly frequencies. To ensure accuracy and consistency in the data analysis, portion sizes originally expressed in household measurements were converted into grams. The nutritional values of the food items were determined using the United States Department of Agriculture (USDA) food composition table (FCT)40. In instances where local foods were not listed in the USDA FCT, the Iranian FCT41 was utilized.
Demographic and clinical measurements
To obtain demographic information, including age, sex, medication intake, and social and economic status, face-to-face interviews were conducted by trained interviewers using a standardized questionnaire. Annual phone follow-ups were carried out by the research team to monitor new medical incidents. In cases requiring further information, a physician conducted additional inquiries through home visits or reviews of medical records.
The participants' physical activity levels were assessed using the validated modifiable activity questionnaire (MAQ)42. This questionnaire, divided into leisure and work-related sections, assessed the duration and frequency of various activities undertaken in the past year. The total physical activity was computed in metabolic equivalent minutes per week (MET-min/week).
Blood pressure was measured using a calibrated mercury sphygmomanometer, following a 15-min rest period. A trained doctor recorded two blood pressure readings at 30-s intervals, and the average of these readings was considered the individual's blood pressure.
The height and weight of the participants were measured using a standardized procedure. To ensure accuracy, participants removed their shoes and wore light clothing during the measurements. A stadiometer was utilized for height measurements, while a calibrated weighing scale was used to record weight. Body mass index (BMI) was calculated by dividing individuals’ weight in kilograms by the square of their height in meters.
Laboratory analyses were conducted utilizing kits provided by Pars Azmon Inc. Participants' venous blood samples were obtained during a fasting period of 12–14 h, between 7:00 and 9:00 a.m. The measurement of serum HDL-C involved the isolation of apoB-containing lipoproteins through phosphotungstic acid precipitation. Serum triglyceride (TG) and total cholesterol (TC) levels were determined using an enzymatic colorimetric method, employing cholesterol esterase and cholesterol oxidase for TG, and glycerol phosphate oxidase for TC. Fasting blood sugar (FBS) was measured using the glucose oxidase technique and an enzymatic colorimetric method. Samples were analyzed only when they met internal quality control standards. The coefficients of variation were 2.2% for serum glucose, 2% (intra-assay) and 0.5% (inter-assay), for TC, and 1.6% (intra-assay), and 0.6% (inter-assay) for TG.
Also, a premature family history of CVDs was defined as the occurrence of any CVDs incidents in first-grade female family members aged < 65 years, or first-grade male family members aged < 55 years43.
Exposure definition
Current and non-smokers
Participants who smoke daily or occasionally, or who have quit smoking for less than a year, are considered current smokers44. Non-smokers are defined as individuals who have quit smoking for more than a year or have no smoking history.
Dietary Quality Index-International (DQI-I)
To calculate the DQI-I, we utilized the approach outlined by Kim et al.45. This method evaluates four primary components: 1) Variety in the intake of food groups, encompassing meat, poultry, fish, eggs, dairy, vegetables, fruits, grains, and legumes, as well as diversity within protein sources (scored on a scale of 0–20 points); 2) Adequacy in the consumption of 8 dietary components including vegetables, fruits, grains, fiber, protein, and micronutrients including iron, calcium, and vitamin C (scored on a scale of 0–40 points); 3) Moderation in the consumption of total fat, saturated fats, cholesterol, sodium, and free-calorie foods (scored on a scale of 0–30 points); and 4) Overall balance in the ratio of macronutrients (carbohydrate: protein: fat) and fatty acids (polyunsaturated fats: monounsaturated fats: saturated fats), (scored on a scale of 0–10 points). Scores can range from 0 to 100, with higher scores indicative of a higher level of diet quality.
Dietary Quality Index-Revised (DQI-R)
The DQI-R comprises ten elements, four of which align with the original DQI (total fat, saturated fat, cholesterol, and calcium). Additionally, the DQI-R assesses grain, fruit, vegetable, iron, dietary moderation, and dietary diversity. Each element is assigned a rating on a scale from 0 to 10, contributing to a maximum cumulative score of 100. The moderation component involves managing simple sugars, discretionary fat, sodium, and dietary alcohol, while diversity encompasses a variety of grains, fruits, vegetables, meats, and dairy products in the diet46.
Outcome definition
The studied outcomes involve CVDs, HTN, and all-cause mortality. CVDs were described as a combined measure involving incidents of coronary heart disease, stroke, or death due to cardiovascular causes. Events related to coronary heart disease included confirmed cases of myocardial infarction (determined by diagnostic electrocardiogram, and biomarkers), possible myocardial infarction (identified by positive electrocardiogram findings, symptoms or signs of a heart attack, and absence of biomarkers; or positive electrocardiogram findings and uncertain biomarkers), and coronary heart disease confirmed through angiography. Stroke was characterized by the presence of newly developed neurological impairment lasting at least 24 h.
According to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines, HTN was diagnosed if an individual’s systolic blood pressure (SBP) was ≥ 140 mmHg, diastolic blood pressure (DBP) was ≥ 90 mmHg, or if they were on medication for HTN management47.
In the case of all-cause mortality, an authorized local physician collected information from hospital records or death certificates. A committee, comprising key professionals including a chief researcher, an internist, an endocrinologist, a cardiologist, an epidemiologist, and the individual responsible for compiling outcome data, evaluated the results obtained.
Statistical analyses
The statistical analysis was performed utilizing IBM SPSS Statistics (Version 26.0, IBM Corp., Armonk, NY, USA). The characteristics of the study population are reported as percentages for categorical variables, means ± standard deviation (SDs) for normally distributed variables, and medians (interquartile ranges) for non-normally distributed variables. Comparisons between the groups, including those with higher and lower diet quality or current and non-smokers, were performed using the chi-square test for categorical variables, independent sample t-test for normally distributed continuous variables, and the Mann‒Whitney U test for non-normally distributed variables. Our study did not encounter missing data.
Cox proportional hazard regression was employed to explore the associations of DQI quartiles and smoking status (non-smokers vs current smokers) with the incidence of HTN, stroke, CVDs, and all-cause mortality. The duration of follow-up was calculated from the enrollment date in the study until the occurrence of the first CVDs or mortality event or until the last follow-up date. Additionally, for the incidence of HTN, the follow-up duration was defined as the midpoint between the date of the follow-up visit where HTN was initially identified and the last follow-up visit preceding the diagnosis.
Additionally, an interaction analysis was conducted based on the joint classification of DQIs (median; higher/lower) and smoking status (current smokers/non-smokers). For the interaction analysis, four groups were created: 1) current smokers with lower diet quality, 2) current smokers with higher diet quality, 3) non-smokers with lower diet quality, and 4) non-smokers with higher diet quality. The hazard ratios (HRs) and their associated 95% confidence intervals (CIs) for each outcome were determined across the categories considering “current smokers with poor diet quality” as a reference group. Variables that had significant associations with CVDs and HTN according to the univariate analysis (P < 0.05), were included in the statistical analyses as confounding factors. Model 1 was adjusted for sex, age, SBP, FBS, serum TC, serum TG, serum HDL-C, energy intake, BMI, and physical activity. Additionally, Model 2 was adjusted for medication use, employment status, education level, and family history of premature CVDs. The fitness of the multivariable models was determined using Harrel’s C index48. To obtain P values for interactions, smoking status, diet quality status, and their interaction terms were included in the unadjusted Cox model. The results include HR (95% CI) for each comparison. The proportional hazards assumption was checked using the graph of the log(−log(survival)) versus the log of survival time, and the assumption was satisfied (lines in the plots were parallel). All P values were derived from two-sided tests, and values less than 0.05 were considered to indicate statistical significance.
Ethics approval and consent to participate
The study followed the Declaration of Helsinki by obtaining informed consent from participants and receiving approval from the Ethics Committee of the Iran University of Medical Sciences (IR.IUMS.REC.1402.138).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Allen, L. et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob. Health 5, e277–e289 (2017).
Sarrafzadegan, N. & Mohammmadifard, N. Cardiovascular disease in iran in the last 40 years: Prevalence, mortality, morbidity, challenges and strategies for cardiovascular prevention. Arch. Iran Med. 22, 204–210 (2019).
Oori, M. J. et al. Prevalence of HTN in Iran: Meta-analysis of published studies in 2004–2018. Curr. Hypertens. Rev. 15, 113–122. https://doi.org/10.2174/1573402115666190118142818 (2019).
Li, Y., Cao, G.-Y., Jing, W.-Z., Liu, J. & Liu, M. Global trends and regional differences in incidence and mortality of cardiovascular disease, 1990–2019: Findings from 2019 global burden of disease study. Eur. J. Prev. Cardiol. 30, 276–286 (2023).
Sun, J. et al. Association of the American Heart Association’s new “Life’s Essential 8” with all-cause and cardiovascular disease-specific mortality: Prospective cohort study. BMC Med. 21, 1–13 (2023).
Millen, B. E. et al. Dietary patterns, smoking, and subclinical heart disease in women: Opportunities for primary prevention from the Framingham Nutrition Studies. J. Am. Diet. Assoc. 104, 208–214. https://doi.org/10.1016/j.jada.2003.11.007 (2004).
Geng, T. et al. The association of genetic susceptibility to smoking with cardiovascular disease mortality and the benefits of adhering to a DASH diet: The Singapore Chinese Health Study. Am. J. Clin. Nutr. 116, 386–393. https://doi.org/10.1093/ajcn/nqac128 (2022).
Boehme, A. Smoking cessation and secondary stroke prevention. Neurology 89, 1656–1657. https://doi.org/10.1212/wnl.0000000000004530 (2017).
Girot, M. Smoking and stroke. Press Med. 38, 1120–1125. https://doi.org/10.1016/j.lpm.2008.12.018 (2009).
Shah, R. S. & Cole, J. W. Smoking and stroke: The more you smoke the more you stroke. Expert Rev. Cardiovasc. Ther. 8, 917–932. https://doi.org/10.1586/erc.10.56 (2010).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364, 937–952. https://doi.org/10.1016/s0140-6736(04)17018-9 (2004).
Stamler, J., Rains-Clearman, D., Lenz-Litzow, K., Tillotson, J. L. & Grandits, G. A. Relation of smoking at baseline and during trial years 1–6 to food and nutrient intakes and weight in the special intervention and usual care groups in the Multiple Risk Factor Intervention Trial. Am. J. Clin. Nutr. 65, 374s–402s. https://doi.org/10.1093/ajcn/65.1.374S (1997).
Dallongeville, J., Marécaux, N., Fruchart, J. C. & Amouyel, P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: A meta-analysis. J. Nutr. 128, 1450–1457. https://doi.org/10.1093/jn/128.9.1450 (1998).
Morabia, A., Bernstein, M. S. & Antonini, S. Smoking, dietary calcium and vitamin D deficiency in women: A population-based study. Eur. J. Clin. Nutr. 54, 684–689. https://doi.org/10.1038/sj.ejcn.1601074 (2000).
Alavi, S. S. et al. Exercise training attenuates cardiac vulnerability and promotes cardiac resistance to isoproterenol-induced injury following hookah smoke inhalation in male rats: Role of klotho and sirtuins. Cardiovasc. Toxicol. 22, 501–514. https://doi.org/10.1007/s12012-022-09733-x (2022).
Mangoni, A. A., Sherwood, R. A., Swift, C. G. & Jackson, S. H. Folic acid enhances endothelial function and reduces blood pressure in smokers: A randomized controlled trial. J. Intern. Med. 252, 497–503. https://doi.org/10.1046/j.1365-2796.2002.01059.x (2002).
Hu, F. B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13, 3–9. https://doi.org/10.1097/00041433-200202000-00002 (2002).
Williams, J. et al. Diet quality of adolescents in rural Sri Lanka based on the Diet Quality Index-International: Findings from the “Integrating Nutrition Promotion and Rural Development” project. Public Health Nutr. 22, 1735–1744. https://doi.org/10.1017/s1368980019000430 (2019).
Shiraseb, F. et al. The association between diet quality index-international and inflammatory markers in Iranian overweight and obese women. Front. Nutr. 10, 1164281. https://doi.org/10.3389/fnut.2023.1164281 (2023).
Asghari, G. et al. Dietary quality among Tehranian adults in relation to lipid profile: Findings from the Tehran Lipid and Glucose Study. J. Health Popul. Nutr. 31, 37–48. https://doi.org/10.3329/jhpn.v31i1.14747 (2013).
Khodamoradi, F. et al. The effects of smoking on metabolic syndrome and its components using causal methods in the Iranian population. Int. J. Prev. Med. 12, 118. https://doi.org/10.4103/ijpvm.ijpvm_45_21 (2021).
Clark, M. L., Butler, L. M., Koh, W. P., Wang, R. & Yuan, J. M. Dietary fiber intake modifies the association between secondhand smoke exposure and coronary heart disease mortality among Chinese non-smokers in Singapore. Nutrition 29, 1304–1309. https://doi.org/10.1016/j.nut.2013.04.003 (2013).
Dauchet, L. et al. Association between the frequency of fruit and vegetable consumption and cardiovascular disease in male smokers and non-smokers. Eur. J. Clin. Nutr. 64, 578–586. https://doi.org/10.1038/ejcn.2010.46 (2010).
Cho, I. Y. et al. Assessment of dietary habits using the diet quality index-international in cerebrovascular and cardiovascular disease patients. Nutrients https://doi.org/10.3390/nu13020542 (2021).
Abdurahman, A. et al. Association of diet quality and food insecurity with metabolic syndrome in obese adults. Int. J. Prev. Med. 12, 138. https://doi.org/10.4103/ijpvm.IJPVM_191_19 (2021).
Daneshzad, E., Larijani, B. & Azadbakht, L. Diet quality indices and cardiovascular diseases risk factors among diabetic women. J. Sci. Food Agric. 99, 5926–5933. https://doi.org/10.1002/jsfa.9867 (2019).
Zhu, P., Pan, X. F., Sheng, L., Chen, H. & Pan, A. Cigarette smoking, diabetes, and diabetes complications: Call for urgent action. Curr. Diabet. Rep. 17, 78. https://doi.org/10.1007/s11892-017-0903-2 (2017).
Luehrs, R. E. et al. Cigarette smoking and longitudinal associations with blood pressure: The CARDIA study. J. Am. Heart Assoc. 10, e019566. https://doi.org/10.1161/jaha.120.019566 (2021).
Ohira, T. et al. Risk factors for ischemic stroke subtypes: The Atherosclerosis Risk in Communities study. Stroke 37, 2493–2498. https://doi.org/10.1161/01.Str.0000239694.19359.88 (2006).
Kawachi, I. et al. Smoking cessation and decreased risk of stroke in women. JAMA 269, 232–236 (1993).
Luo, J. et al. Cigarette smoking and risk of different pathologic types of stroke: A systematic review and dose-response meta-analysis. Front. Neurol. 12, 772373. https://doi.org/10.3389/fneur.2021.772373 (2021).
Bodner, C. et al. Antioxidant intake and adult-onset wheeze: A case-control study. Aberdeen WHEASE Study Group. Eur. Respir. J. 13, 22–30. https://doi.org/10.1183/09031936.99.13102299 (1999).
Margetts, B. M. & Jackson, A. A. Interactions between people’s diet and their smoking habits: The dietary and nutritional survey of British adults. BMJ 307, 1381–1384. https://doi.org/10.1136/bmj.307.6916.1381 (1993).
Ramotowski, B., Gurbel, P. A., Tantry, U. & Budaj, A. Smoking and cardiovascular diseases: paradox greater than expected?. Pol. Arch. Intern. Med. 129, 700–706. https://doi.org/10.20452/pamw.14931 (2019).
Slagter, S. N. et al. Associations between smoking, components of metabolic syndrome and lipoprotein particle size. BMC Med. 11, 195. https://doi.org/10.1186/1741-7015-11-195 (2013).
Norouzzadeh, M. et al. Cigarette smoking and cardiovascular disease incidence and all-cause mortality: The modifying role of diet quality. BMC Public Health 24, 1021. https://doi.org/10.1186/s12889-024-18468-z (2024).
Li, Z. et al. Longitudinal study of diet quality and change in asthma symptoms in adults, according to smoking status. Br. J. Nutr. 117, 562–571. https://doi.org/10.1017/s0007114517000368 (2017).
Azizi, F., Zadeh-Vakili, A. & Takyar, M. Review of rationale, design, and initial findings: Tehran lipid and glucose study. Int. J. Endocrinol. Metab. 16, e84777. https://doi.org/10.5812/ijem.84777 (2018).
Esfahani, F. H., Asghari, G., Mirmiran, P. & Azizi, F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J. Epidemiol. 20, 150–158. https://doi.org/10.2188/jea.je20090083 (2010).
Satija, A. & Hu, F. B. Cardiovascular benefits of dietary fiber. Curr. Atheroscler. Rep. 14, 505–514. https://doi.org/10.1007/s11883-012-0275-7 (2012).
Azar, M. & Sarkisian, E. Food Composition Table of Iran: National Nutrition and Food Research Institute (Shaheed Beheshti University, 1980).
Momenan, A. A. et al. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Arch. Iran Med. 15, 279–282 (2012).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140, e596–e646. https://doi.org/10.1161/cir.0000000000000678 (2019).
Wang, J. et al. Association between life-course cigarette smoking and metabolic syndrome: A discovery-replication strategy. Diabetol. Metab. Syndr. 14, 11. https://doi.org/10.1186/s13098-022-00784-2 (2022).
Kim, S., Haines, P. S., Siega-Riz, A. M. & Popkin, B. M. The Diet Quality Index-International (DQI-I) provides an effective tool for cross-national comparison of diet quality as illustrated by China and the United States. J. Nutr. 133, 3476–3484. https://doi.org/10.1093/jn/133.11.3476 (2003).
Newby, P. K. et al. Reproducibility and validity of the Diet Quality Index Revised as assessed by use of a food-frequency questionnaire. Am. J. Clin. Nutr. 78, 941–949. https://doi.org/10.1093/ajcn/78.5.941 (2003).
Chobanian, A. V. et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 289, 2560–2572. https://doi.org/10.1001/jama.289.19.2560 (2003).
Harrell, F. E. Jr., Califf, R. M., Pryor, D. B., Lee, K. L. & Rosati, R. A. Evaluating the yield of medical tests. JAMA 247, 2543–2546 (1982).
Acknowledgements
We express our gratitude to the participants in the TLGS for their enthusiastic support and acknowledge the valuable assistance provided by the staff of the Research Institute for Endocrine Sciences, TLGS unit.
Funding
This work was funded by the Iran University of Medical Sciences, Tehran, Iran. This grant has been awarded for completion of a master's thesis.
Author information
Authors and Affiliations
Contributions
M.N.: Conceptualization, Methodology, Formal analysis, Investigation, Writing—Original Draft F.T.: Methodology, Formal analysis, Validation, Investigation H.F.N.: Investigation, Writing—Review & Editing N.M.: Investigation, Writing—Review & Editing S.T.R.: Conceptualization, Supervision P.M.: Resources, Project administration F.A.: Resources, Project administration.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Norouzzadeh, M., Teymoori, F., Farhadnejad, H. et al. The interaction between diet quality and cigarette smoking on the incidence of hypertension, stroke, cardiovascular diseases, and all-cause mortality. Sci Rep 14, 12371 (2024). https://doi.org/10.1038/s41598-024-62616-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62616-9
- Springer Nature Limited