Abstract
Optimal fluid management during major surgery is of considerable concern to anesthesiologists. Although crystalloids are the first choice for fluid management, the administration of large volumes of crystalloids is associated with poor postoperative outcomes. Albumin can be used for fluid management and may protect renal function. However, data regarding the effects of albumin administration on kidney function are conflicting. As such, the present study aimed to investigate the effect of albumin administration on renal function in patients undergoing major surgery and compare its effects with those of crystalloid fluid. The Embase, Medline, Web of Science, Cochrane Library, and KoreaMed databases were searched for relevant studies. The primary endpoint of the meta-analysis was the incidence of postoperative kidney injury, including acute kidney injury and renal replacement therapy. Twelve studies comprising 2311 patients were included; the primary endpoint was analyzed in four studies comprising 1749 patients. Perioperative albumin levels in patients undergoing major surgery did not significantly influence kidney dysfunction (p = 0.98). Postoperative fluid balance was less positive in patients who underwent major surgery and received albumin than in those who received crystalloids. Owing to the limitations of this meta-analysis, it remains unclear whether albumin administration during major surgery is better than crystalloid fluid for improving postoperative renal function.
Similar content being viewed by others
Introduction
The amount and type of intravenous fluid administered during major surgery are associated with perioperative outcomes and may affect patient prognosis1. Crystalloids and colloids are commonly used for fluid management in major surgical procedures. Although crystalloids are preferred for intravascular fluid management, large-volume intravascular crystalloid administration is associated with poor postoperative outcomes including delayed gastrointestinal function, multiple organ failure, morbidity, and mortality2,3. Albumin is the principal plasma protein and plays a central role in maintaining plasma oncotic pressure4; as such, it is used for fluid management in patients undergoing major surgery. According to Lazzareschi et al., albumin was used intraoperatively in approximately 15% of major non-cardiac surgeries in the United States between January 2014 and June 20205. Other functions of albumin include the binding and transport of molecular substances and ligands, redox reactions, regulation of acid–base balance, capillary permeability, vascular integrity, and participation in apoptosis and homeostasis6.
Albumin can increase oncotic pressure and, consequently, preserve intravascular volume and renal perfusion pressure better than crystalloid fluids7. Albumin has also been hypothesized to improve renal function by affecting renal blood flow autoregulation by decreasing oxidative stress, endotoxemia, and endothelial stabilization8. However, results of studies investigating albumin administration vary, and conflicting conclusions have been drawn. Some studies have shown that administering albumin during the perioperative period in patients undergoing major surgery may prevent kidney injury9,10, whereas others have reported either a detrimental effect of albumin on the kidney, or no association with kidney function11,12. Considering the lack of consensus data, the effects of albumin administration on the kidneys during major surgeries remain uncertain.
As such, we aimed to compare the effect of albumin with that of crystalloid fluid administration on renal function in patients undergoing major surgery. This meta-analysis included randomized controlled trials (RCTs) in which albumin was administered during the perioperative period to adult patients undergoing major surgery.
Results
Description of studies
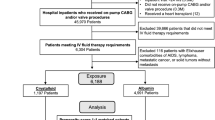
The initial literature search retrieved 1296 studies, and 2 were identified from other sources. A flow-diagram illustrating the study selection process is presented in Fig. 1. Of 25 potentially eligible studies, six were not RCTs, 1 was a pediatric study, 1 was a duplicate, 1 was retracted, 2 did not use albumin, and 2 had different study designs. Ultimately, therefore, 11 RCTs13,14,15,16,17,18,19,20,21,22,23,24 and 1 non-randomized control trial fulfilled the study inclusion criteria. Data regarding kidney dysfunction were obtained from the articles or via e-mail from the authors of these studies. The 6 studies for which kidney dysfunction data could not be collected19,20,21,22,23,24 included 278 patients, comprising 12.03% of the total number of patients across all studies fulfilling the study inclusion criteria. One study reported data regarding acute kidney injury (AKI) and renal replacement therapy (RRT)14.
Study characteristics
Characteristics of the 12 included studies are summarized in Table 1.
Five studies described the use of albumin at a concentration ≥ 20%14,15,18,19,24, whereas seven used albumin at a concentration ≤ 5%13,16,17,20,21,22,23. Seven studies included patients who underwent cardiac surgery14,15,16,17,20,22,23. Other surgery types included those for upper gastrointestinal cancer, pelvic exenteration, cystectomy, and renal transplantation.
Four studies did not use synthetic colloids15,16,19,22, and six did not indicate whether synthetic colloids were used13,17,18,20,21,24; for these, it was assumed that none were used. In one study, synthetic colloids were used intra-and postoperatively, but there was no difference in the volume of synthetic colloids used between the albumin and control groups14. One study used synthetic colloids during the postoperative period, and the amount of synthetic colloids administered in the albumin group was lower than that administered in the control group23.
In one study, albumin was used in the control group, albeit with a lower volume than that in the albumin group22.
Risk of bias in the included studies
Two reviewers independently assessed the methodological quality of the studies using the Risk of Bias (ROB) tool recommended by the Cochrane Collaboration. Disagreements were resolved through discussion and consensus with another reviewer (YJ Choi).
The Cochrane tool was used to determine risk of bias, which was evaluated as “low”, “high” or “some concern”, as shown in Fig. 2.
Kidney dysfunction
Six studies reported kidney dysfunction in patients in whom albumin was administered during major surgeries. Four of the six studies reported data regarding the incidence of AKI (n = 84)13,14,15,16. Bisgaard et al. defined AKI based on the Risk, Injury, and Failure; and Loss; and End-stage kidney disease (RIFLE) criteria. Lee et al. defined AKI in accordance with the Acute Kidney Injury Network (AKIN) criteria. The criteria for AKI were not clearly defined in the study by Marelli et al. A study by Pesonen et al. defined AKI as an increase in postoperative creatinine levels to at least twice the preoperative level. Four patients required RRT in three of six studies14,17,18, which was too small a sample for meaningful statistical analysis; therefore, RRT data were excluded from the comparison between the two groups. Four studies reported creatinine data17,18,23,24; however, changes creatinine levels over 48 h or 7 days for individual patients could not be obtained; therefore, creatinine data were excluded.
Albumin administration did not significantly affect kidney function compared with crystalloid administration (albumin, 40/874 [4.58%] versus [vs.] crystalloid, 44/875 [5.03%]; odds ratio [OR] 0.99 [95% confidence interval (CI) 0.41 − 2.42]; I2 = 54%, p = 0.98) (Fig. 3A).
In the subgroup analysis according to different albumin concentrations (i.e., iso-oncotic and hyper-oncotic), studies using ≤ 5%13,16 and > 20%14,15 albumin were classified into the iso-oncotic and hyper-oncotic groups, respectively. Administration of albumin at both iso-oncotic and hyperoncotic concentrations did not significantly affect the incidence of kidney dysfunction when compared with the effect of crystalloid administration (iso-oncotic group, albumin, 24/723 [3.32%] vs. crystalloid, 18/723 [2.49%], OR 1.33 [95% CI 0.72 − 2.46], I2 = 0%, p = 0.36; hyperoncotic group, albumin, 16/151 [10.60%] vs. crystalloid, 26/152 [17.11%], OR 1.00 [95% CI 0.10 − 9.58], I2 = 58%, p = 1.00) (Fig. 3B).
Mortality and intensive care unit stay
Three14,16,17 and six13,14,17,19,20,22 studies reported mortality and intensive care unit (ICU) stay, respectively, in patients who underwent major surgery and were administered albumin. Albumin administration did not significantly influence mortality (albumin, 5/871 [0.57%] vs. crystalloid, 4/873 [0.46%]; OR 1.19 [95% CI 0.27 − 5.25]; I2 = 11%, p = 0.82) (Fig. 4A). The pooled mean difference (MD) of the ICU stay was -0.04 (95% CI − 1.22 to 1.14; I2 = 0%, p = 0.95) between the albumin and crystalloid groups (Fig. 4B).
Other outcomes
Secondary outcome data, including the studies, number of participants, risk ratio or MD, and p-values, are summarized in Table 2.
Intraoperative and postoperative fluid balance
Among the included studies investigating patients who underwent major surgery and received albumin, five and five reported results on intraoperative and postoperative fluid balance, respectively. Albumin administration did not significantly influence intraoperative fluid balance (MD − 517.63 [95% CI − 1112.07 to 76.80]; I2 = 94%, p = 0.09). Compared with crystalloids, albumin administration significantly lowered postoperative fluid balance (MD − 657.46 [95% CI − 1257.24 to − 57.68]; I2 = 97%, p = 0.03).
Intraoperative and postoperative blood loss
Four and seven studies reported intra- and postoperative blood loss, respectively, in patients who underwent major surgery and albumin therapy. Compared with crystalloid, albumin administration did not significantly affect intraoperative (MD 29.35 [95% CI − 134.06 to 192.77]; I2 = 66%, p = 0.72) and postoperative (MD − 16.06 [95% CI − 156.84 to 124.72]; I2 = 97%, p = 0.82) blood loss.
Intraoperative and postoperative red blood cell transfusion
Eight and six studies reported on intraoperative and postoperative red blood cell (RBC) transfusions, respectively, in patients who underwent major surgery and were administered albumin. Intraoperative RBC transfusion was significantly higher in patients who received albumin than in those who received crystalloids (MD 0.37 [95% CI 0.07 to 0.67]; I2 = 80%, p = 0.01). In contrast, the volume of postoperative RBC transfusions did not significantly differ between patients who received albumin versus those who received crystalloids (MD -0.45 [95% CI − 1.29 to 0.39]; I2 = 90%, p = 0.29).
Lowest hemoglobin level
Six studies reported nadir perioperative hemoglobin levels. Compared with the crystalloid group, the nadir hemoglobin level was significantly lower in the albumin group (MD − 1.29 [95% CI − 2.12 to − 0.46]; I2 = 95%, p = 0.002).
Postoperative pulmonary edema
Five studies reported on postoperative pulmonary edema. Albumin administration did not significantly influence postoperative pulmonary edema in the albumin and crystalloid groups (albumin, 9/243 [3.70%] vs. crystalloid, 13/244 [5.33%]; OR 0.70 [95% CI 0.28 − 1.74]; I2 = 0%, p = 0.45).
Sensitivity analysis and publication bias
Sensitivity analysis was performed to evaluate the influence of synthetic colloids by excluding studies in which synthetic colloids were used or those in which their use was not described. As reported in Table 1, synthetic colloids did not influence kidney dysfunction. Based on Egger’s test performed to evaluate publication bias in this meta-analysis, the funnel plot displayed no obvious asymmetry (Fig. 2). Furthermore, Egger’s test indicated no evidence of publication bias in studies addressing the kidney dysfunction endpoint (t = 1.85, p = 0.138). The quality of evidence for kidney dysfunction, mortality, and ICU stay was low, high, and high, respectively. The overall quality of evidence for the other outcomes, assessed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) criteria, is presented in Table 2.
Discussion
This meta-analysis synthesized evidence from RCTs comparing the effects of crystalloid versus albumin administration on renal function in patients who underwent major surgery, with results revealing no association. Several meta-analyses of mortality following the administration of crystalloids and albumin under various clinical conditions have been conducted25,26. Although individual studies have reported the effects of albumin administration on kidney function during major surgery, no meta-analysis has been performed and the effects of albumin administration on the kidneys during the perioperative period remain undefined.
The incidence of mortality in the broad population of patients undergoing major surgery is approximately 1–4%, suggesting that mortality is a relatively insensitive outcome27. In contrast, the incidence of morbidity is usually much higher than that of mortality, and morbidity can provide results that are more sensitive to meta-analyses than mortality as an outcome28,29. Moreover, postoperative kidney injury is a continual medical concern that significantly influences prognosis. Therefore, this study aimed to understand the effects of albumin administration on kidney function in patients undergoing major surgery.
In a retrospective observational study involving patients receiving albumin-containing fluids for fluid bolus therapy, the use of hyperosmolar albumin resulted in less volume, less sodium and chloride, and fewer adverse outcomes than the use of iso-oncotic albumin30. Previously, Wiedermann et al. reported that hyperoncotic albumin reduced the probability of AKI by 76% and suggested that albumin exhibits renoprotective properties31. In contrast, Schortgen et al. reported the possibility of harmful effects on renal function and poorer outcomes with hyperosmolar albumin32. However, results of the present study contradict those reported in these two studies, and may be explained by differences in patient condition(s) in the pooled studies. The present review included studies that focused on patients who underwent surgery. Wiedermann et al. included not only studies that focused on patients who underwent surgery, but also those that focused on patients with cirrhosis (one study on patients who underwent surgery and six on patients with cirrhosis). Albumin administration improves kidney function and prevents AKI in patients with cirrhosis33. Furthermore, in contrast to the present study, in which studies using a mixture of iso-oncotic and hyper-oncotic albumin were pooled, Wiedermann et al. used only hyper-oncotic albumin. To verify the results of the study by Wiedermann et al., it is necessary to carefully and cautiously analyze the effects of hyperoncotic albumin on kidney function. Schortgen et al. selected patients already in a state of multiple organ failure and severe hemodynamic instability. These patients may have advanced multiple organ failure and hemodynamic instability; therefore, their physical conditions were different from those of patients who underwent major surgery. Furthermore, there were differences at baseline, with the crystalloid group including significantly more medical patients and a lower volume of fluid than the albumin group. In a retrospective study by Kim et al., no significant association was observed between hyperoncotic albumin levels and AKI in patients who underwent major abdominal surgery34. In contrast, in a retrospective study by Udeh et al., hyperoncotic albumin in postoperative shock appeared to be associated with AKI35.
Although there was no significant difference in blood loss volume between patients administered albumin versus crystalloids during major surgery in our study, the volume of RBC transfusions was higher in the albumin group. This could, in part, be explained by lower perioperative hemoglobin levels in the albumin versus crystalloid group. Other studies reported no difference in blood loss between the albumin and crystalloid groups; however, hemoglobin level was lower in the albumin group36,37. Albumin has a greater and longer-lasting plasma volume expansion effect than crystalloid fluid38. In this meta-analysis, we speculated that, despite no significant difference in blood loss between patients administered albumin versus crystalloids during major surgery, those receiving albumin underwent a significantly higher volume of RBC transfusions than those receiving crystalloids due to the overestimated blood loss caused by hemodilution resulting from the administered albumin. A recent network meta-analysis reported that an albumin priming strategy resulted in lower postoperative hemoglobin counts than crystalloids, despite no significant difference in postoperative blood loss in on-pump cardiac surgery39. This study showed that albumin priming resulted in more perioperative RBC transfusions than crystalloid priming. Albumin is known to cause more hemodilution than crystalloids. In a study by Arya et al., the crystalloid group was infused with a volume three times that of the albumin group and the immediately measured hemoglobin level was lower in the crystalloid group than in the albumin group. However, over time, the measured hemoglobin levels were lower in the albumin group than in the crystalloid group40. Caution is necessary when interpreting these results because the cause of low hemoglobin levels elicited by albumin administration and RBC transfusion has not been established.
In our meta-analysis, there was no statistically significant difference in intraoperative fluid balance between the albumin and crystalloid groups among patients who underwent major surgery. However, our results should be interpreted with caution. This is because the study by Gallagher, which was the only of the five studies to report a greater amount of intraoperative fluid in the albumin group than in the crystalloid group, excluded a portion of blood loss when calculating fluid balance.
Another review reported that the albumin group exhibited a less positive fluid balance than the crystalloid group in critically ill patients41,42. Albumin can efficiently maintain intravenous fluids because its molecular weight is larger than that of crystalloid fluids43. Yanase et al. reported that fluid bolus therapy using albumin had a more sustained effect than crystalloids on mean arterial, central venous, and perfusion pressures in patients undergoing cardiac surgery44. It has been reported that the volume of fluid required to achieve the same resuscitation endpoint is lower in the albumin group than in the crystalloid group45,46. Nevertheless, there is still controversy as to whether albumin versus crystalloid is beneficial. During resuscitation for septic shock, the volume of fluid required when albumin and crystalloid fluids were administered in a blinded fashion was similar between the two groups47,48.
In our meta-analysis, the crystalloid group exhibited a significantly higher postoperative positive fluid balance than the albumin group. Xu et al. reported that perioperative fluid infusion was lower in the albumin group than crystalloid group49. Positive perioperative fluid balance adversely affects renal function and patient prognosis50. Firth et al. reported that fluid-extended animals exhibit increased renal venous pressure, resulting in elevated interstitial pressure and reduced renal blood flow compared with fluid-depleted animals51. In a meta-analysis, although there was a trend toward lower volumes of albumin administered compared with crystalloids in ICU patients, which was not statistically significant, the central venous pressure was significantly higher with albumin than with crystalloids52. Additionally, Nishimoto et al. reported that the higher the positive fluid balance, the higher the incidence of AKI53. Nishimoto et al. reported that an increase in the probability of AKI is associated with an increase in the intraoperative fluid balance > 40 ml/kg. However, some of the studies included in the present meta-analysis reported a mean intraoperative fluid balance < 40 ml/kg, assuming a mean adult weight of 60 kg. Furthermore, in the study by Nishimoto et al., the expected probabilities of postoperative AKI were 0.05 and 0.17 when the intraoperative fluid balance was 50 ml/kg and 100 ml/kg, respectively. However, among the studies included in the present meta-analysis, the study with the largest difference in mean intraoperative fluid balance between the albumin-administered and crystalloid groups was 21 ml/kg, assuming an average adult weight of 60 kg. This explains the observed (in the present meta-analysis) lack of any significant difference in kidney dysfunction and the presence of a significant difference in intraoperative fluid balance between the albumin and crystalloid groups.
The present meta-analysis had several limitations. The effect of albumin administration on kidney function based on albumin concentration is ambiguous because this meta-analysis included both iso-oncotic and hyper-oncotic albumin studies. However, in the subgroup analysis, the effects of iso-oncotic and hyper-oncotic albumin on kidney function were not different.
In addition, the effect of albumin may be influenced by additional conditions such as the timing of albumin administration or other clinical factors in patients who undergo major surgery. Zhang et al. reported that administration of albumin in the ICU after cardiac surgery decreased mortality54. The authors suggested that albumin administration may be beneficial for ICU patients with hypovolemia, an inflammatory state, capillary leakage, vasodilation, and a high degree of vascular permeability after cardiac surgery. Our study found no significant impact of administered albumin compared with crystalloids on mortality in patients undergoing major surgery. However, due to its low incidence, definitive conclusions regarding the effects of albumin on mortality cannot be drawn. Vincent et al.55 reported that albumin could potentially improve morbidity when used to treat hypovolemia secondary to trauma and surgery.
Moreover, there was a risk of bias in the population or type of surgery, and the low level of evidence was due to the inconsistent AKI criteria based on RIFLE and AKIN used in the included studies. In this meta-analysis, the primary endpoint was analyzed in only four studies involving approximately 1700 patients. One of the four studies included approximately 80% of the patients. Furthermore, the primary endpoint was analyzed in patients who underwent heterogeneous major surgeries, including cardiac and non-cardiac procedures. Epidemiologically, postoperative AKI after cardiac and non-cardiac surgery is a common cause of renal hypoperfusion, inflammation, oxidative stress, exogenous and endogenous toxins, ischemia, and reperfusion injury56,57. We investigated the incidence of AKI in a heterogeneous population undergoing major surgery and found that, except for cardiac surgery, other major surgeries had similar rates of AKI58. Therefore, in this meta-analysis, a search was performed to identify major surgeries, including cardiac and noncardiac procedures. Many clinical studies investigating postoperative AKI have been published, mainly using the KDIGO, RIFLE, and AKIN criteria; however, to date, there has been no clear gold standard for postoperative AKI59. Therefore, despite the lack of a consistent definition of AKI, we included all studies with AKI data. Owing to the risk of bias in the population or type of surgery, and the lack of a consistent definition of AKI in this meta-analysis, future high-quality randomized controlled trials are necessary to determine the efficacy of administered albumin on kidney function in patients undergoing major surgery.
In conclusion, this meta-analysis has important policy implications for fluid management during major surgical procedures. Results of this meta-analysis suggested that kidney function may not be affected by albumin, and no clear advantage of albumin over crystalloid fluid administration during major surgery was observed. However, owing to the limitations of this meta-analysis, a larger trial investigating the effects of albumin on kidney function in patients undergoing major surgery should be conducted. In addition, albumin is expensive compared to crystalloid fluids; hence, the medical and economic burden is high. Albumin should be used cautiously during major surgeries until more conclusive studies are completed.
Method
Institutional review board approval was not required for this systematic review and meta-analysis. The systematic review was performed according to the Cochrane Review Methods and a previously registered protocol (PROSPERO, registration number CRD42021259805), and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (i.e., “PRISMA) statement.
Identification of relevant studies
Query searches identified relevant studies in the Embase, Medline, Web of Science, Cochrane Library, and KoreaMed databases that were published from inception up to December 31, 2022. The detailed search strategy is illustrated in Fig. 1.
A systematic search for relevant published trials was performed without language restrictions. In addition, the reference lists of relevant review articles were also searched for potentially eligible studies.
Studies fulfilling the following criteria were considered to be eligible: RCTs; a population of patients who underwent major surgery, defined as any cardiac, thoracic, major vascular, intra-abdominal, or retroperitoneal procedure; perioperative administration of intervention fluid (albumin: 4–5%, 20%, or 25% human albumin) vs. control (crystalloid fluid: 0.9% normal saline, Ringer’s acetate solution, PlasmaLyte, or Hartmann’s solution); and reported kidney-related clinical outcomes as primary or secondary outcomes.
Studies with patient populations < 18 years of age, and those including minor surgeries, defined as invasive procedures not requiring a large surgical incision that would be expected to result in significant bleeding60, were excluded.
Types of outcome measures
A review of relevant articles identified AKI, RRT, and changes in serum creatinine levels as parameters of postoperative kidney injury. In cases in which both AKI and RRT data were described in the article, AKI data were selected as the primary outcome.
Data collection and analysis
Full-text copies of all relevant studies were independently assessed based on predefined inclusion criteria. Two authors (KS Lee and YJ Choi) independently extracted the data and YJ Won verified accuracy. The extracted data included trial design features, perioperative laboratory values, intraoperative fluid volumes, complications (AKI, RRT, and pulmonary edema), mortality, and length of ICU stay. The methodological quality across statistically pooled outcomes was evaluated using the GRADE guidelines61.
Risk of bias in included studies
The risk of bias was analyzed using the Cochrane Risk of Bias Tool (ROB v2.0), which has five domains: bias arising from the randomization process; bias due to deviations from intended interventions; bias due to missing outcome data; bias in the measurements of the outcome; and bias in the selection of the reported results. Each domain classifies studies into “low,” “some concern,” and “high” risk of bias. Two authors (KS Lee and YJ Won) independently evaluated the methodological quality and risk of bias. Any disagreements were discussed with another author (YJ Choi).
Statistical analysis
Review Manager version 5.4 (Cochrane Collaboration, Oxford, United Kingdom) was used for data analysis and synthesis. Results expressed as median and interquartile range were calculated as mean and standard deviation using the methods described by Wan et al. 62. Depending on the reported effect size measures, pooled risk ratios, MD, and 95% CI were calculated. A random-effects approach (inverse variance or Mantel–Haenszel) was selected to allow for expected heterogeneity across studies because data collected from different study designs and surgeries would not satisfy the assumption of a fixed-effects meta-analysis. The degree of heterogeneity among the studies was based on I-squared statistics, with ranges of 0–50%, 50–75%, and 75–100% considered to be low, moderate, and high degrees of heterogeneity, respectively. A sensitivity analysis was performed by removing studies that used synthetic colloids or did not mention the use of synthetic colloids in the meta-analysis to determine whether synthetic colloids could alter the results. A funnel plot was used to evaluate potential publication bias, and Egger’s test was performed to evaluate funnel plot asymmetry using STATA Release 17 (StataCorp LLC, College Station, TX, USA).
Data availability
All data generated or analysed during this study are included in this published article.
References
Holte, K. & Kehlet, H. Fluid therapy and surgical outcomes in elective surgery: A need for reassessment in fast-track surgery. J. Am. Coll. Surg. 202, 971–989. https://doi.org/10.1016/j.jamcollsurg.2006.01.003 (2006).
Peng, J. S. et al. Restrictive intraoperative fluid rate is associated with improved outcomes in cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann. Surg. Oncol. 29, 163–173. https://doi.org/10.1245/s10434-021-10556-3 (2022).
Colantonio, L. et al. A randomized trial of goal directed vs standard fluid therapy in cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. J. Gastrointest. Surg. 19, 722–729. https://doi.org/10.1007/s11605-015-2743-1 (2015).
Gounden, V., Vashisht, R. & Jialal, I. StatPearls (2023).
Lazzareschi, D. V. et al. Intraoperative use of albumin in major noncardiac surgery: Incidence, variability, and association with outcomes. Ann. Surg. 278, e745–e753. https://doi.org/10.1097/SLA.0000000000005774 (2023).
Bihari, S., Bannard-Smith, J. & Bellomo, R. Albumin as a drug: its biological effects beyond volume expansion. Crit. Care Resusc. 22, 257–265 (2020).
Zdolsek, M. & Hahn, R. G. Kinetics of 5% and 20% albumin: A controlled crossover trial in volunteers. Acta Anaesthesiol. Scand. 66, 847–858. https://doi.org/10.1111/aas.14074 (2022).
Garcia-Martinez, R., Noiret, L., Sen, S., Mookerjee, R. & Jalan, R. Albumin infusion improves renal blood flow autoregulation in patients with acute decompensation of cirrhosis and acute kidney injury. Liver Int. 35, 335–343. https://doi.org/10.1111/liv.12528 (2015).
Iglesias, J. et al. Albumin is a major serum survival factor for renal tubular cells and macrophages through scavenging of ROS. Am. J. Physiol. 277, F711-722. https://doi.org/10.1152/ajprenal.1999.277.5.F711 (1999).
Wiedermann, C. J. & Joannidis, M. Nephroprotective potential of human albumin infusion: A narrative review. Gastroenterol. Res. Pract. 2015, 912839. https://doi.org/10.1155/2015/912839 (2015).
Kingeter, A. J. et al. Association between albumin administration and survival in cardiac surgery: A retrospective cohort study. Can. J. Anaesth. 65, 1218–1227. https://doi.org/10.1007/s12630-018-1181-4 (2018).
Ryhammer, P. K. et al. Colloids in cardiac surgery-friend or foe?. J. Cardiothorac. Vasc. Anesth. 31, 1639–1648. https://doi.org/10.1053/j.jvca.2017.02.001 (2017).
Bisgaard, J. et al. Goal-directed therapy with bolus albumin 5% is not superior to bolus ringer acetate in maintaining systemic and mesenteric oxygen delivery in major upper abdominal surgery: A randomised controlled trial. Eur. J. Anaesthesiol. 37, 491–502. https://doi.org/10.1097/EJA.0000000000001151 (2020).
Lee, E. H. et al. Effect of exogenous albumin on the incidence of postoperative acute kidney injury in patients undergoing off-pump coronary artery bypass surgery with a preoperative albumin level of less than 4.0 g/dl. Anesthesiology 124, 1001–1011. https://doi.org/10.1097/ALN.0000000000001051 (2016).
Marelli, D. et al. Does the addition of albumin to the prime solution in cardiopulmonary bypass affect clinical outcome? A prospective randomized study. J. Thorac. Cardiovasc. Surg. 98, 751–756 (1989).
Pesonen, E. et al. Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: A randomized clinical trial. JAMA 328, 251–258. https://doi.org/10.1001/jama.2022.10461 (2022).
Skhirtladze, K. et al. Comparison of the effects of albumin 5%, hydroxyethyl starch 130/0.4 6%, and Ringer’s lactate on blood loss and coagulation after cardiac surgery. Br. J. Anaesth. 112, 255–264. https://doi.org/10.1093/bja/aet348 (2014).
Abdallah, E., El-Shishtawy, S., Mosbah, O. & Zeidan, M. Comparison between the effects of intraoperative human albumin and normal saline on early graft function in renal transplantation. Int. Urol. Nephrol. 46, 2221–2226. https://doi.org/10.1007/s11255-014-0785-z (2014).
Fiorica, J. V. et al. Concentrated albumin infusion as an aid to postoperative recovery after pelvic exenteration. Gynecol. Oncol. 43, 265–269. https://doi.org/10.1016/0090-8258(91)90033-2 (1991).
Gallagher, J. D. et al. Effects of colloid or crystalloid administration on pulmonary extravascular water in the postoperative period after coronary artery bypass grafting. Anesth. Analg. 64, 753–758 (1985).
Rasmussen, K. C. et al. Impact of albumin on coagulation competence and hemorrhage during major surgery: A randomized controlled trial. Medicine (Baltimore) 95, e2720. https://doi.org/10.1097/MD.0000000000002720 (2016).
Sade, R. M. et al. A prospective randomized study of hydroxyethyl starch, albumin, and lactated Ringer’s solution as priming fluid for cardiopulmonary bypass. J. Thorac. Cardiovasc. Surg. 89, 713–722 (1985).
Scott, D. A. et al. A comparison of albumin, polygeline and crystalloid priming solutions for cardiopulmonary bypass in patients having coronary artery bypass graft surgery. Perfusion 10, 415–424. https://doi.org/10.1177/026765919501000605 (1995).
Shah, R. B., Shah, V. R., Butala, B. P. & Parikh, G. P. Effect of intraoperative human albumin on early graft function in renal transplantation. Saudi J. Kidney Dis. Transpl. 25, 1148–1153. https://doi.org/10.4103/1319-2442.144246 (2014).
Xu, J. Y. et al. Comparison of the effects of albumin and crystalloid on mortality in adult patients with severe sepsis and septic shock: A meta-analysis of randomized clinical trials. Crit. Care 18, 702. https://doi.org/10.1186/s13054-014-0702-y (2014).
Cochrane Injuries Group Albumin R. Human albumin administration in critically ill patients: Systematic review of randomised controlled trials. BMJ 317, 235–240. https://doi.org/10.1136/bmj.317.7153.235 (1998).
Heeney, A., Hand, F., Bates, J., Mc Cormack, O. & Mealy, K. Surgical mortality—An analysis of all deaths within a general surgical department. Surgeon 12, 121–128. https://doi.org/10.1016/j.surge.2013.07.005 (2014).
O’Connor, M. E., Kirwan, C. J., Pearse, R. M. & Prowle, J. R. Incidence and associations of acute kidney injury after major abdominal surgery. Intensive Care Med. 42, 521–530. https://doi.org/10.1007/s00134-015-4157-7 (2016).
Hobson, C. et al. Cost and mortality associated with postoperative acute kidney injury. Ann. Surg. 261, 1207–1214. https://doi.org/10.1097/SLA.0000000000000732 (2015).
Bannard-Smith, J. et al. Haemodynamic and biochemical responses to fluid bolus therapy with human albumin solution, 4% versus 20%, in critically ill adults. Crit. Care Resusc. 17, 122–128 (2015).
Wiedermann, C. J., Dunzendorfer, S., Gaioni, L. U., Zaraca, F. & Joannidis, M. Hyperoncotic colloids and acute kidney injury: A meta-analysis of randomized trials. Crit. Care 14, R191. https://doi.org/10.1186/cc9308 (2010).
Schortgen, F., Girou, E., Deye, N., Brochard, L. & Group, C. S. The risk associated with hyperoncotic colloids in patients with shock. Intensive Care Med. 34, 2157–2168. https://doi.org/10.1007/s00134-008-1225-2 (2008).
Garcia-Tsao, G., Parikh, C. R. & Viola, A. Acute kidney injury in cirrhosis. Hepatology 48, 2064–2077. https://doi.org/10.1002/hep.22605 (2008).
Kim, H. J. et al. Association between 20% albumin use and acute kidney injury in major abdominal surgery with transfusion. Int. J. Mol. Sci. 24, 2333. https://doi.org/10.3390/ijms24032333 (2023).
Udeh, C. I. et al. Acute kidney injury in postoperative shock: Is hyperoncotic albumin administration an unrecognized resuscitation risk factor?. Perioper. Med. (Lond.) 7, 29. https://doi.org/10.1186/s13741-018-0110-y (2018).
Huang, C. J. et al. Clinical beneficial effects of using crystalloid only in recipients of living donor liver transplantation. Int. J. Environ. Res. Public Health 14, 1418. https://doi.org/10.3390/ijerph14111418 (2017).
Jones, S. B., Whitten, C. W., Despotis, G. J. & Monk, T. G. The influence of crystalloid and colloid replacement solutions in acute normovolemic hemodilution: A preliminary survey of hemostatic markers. Anesth. Analg. 96, 363–368. https://doi.org/10.1097/00000539-200302000-00012 (2003).
Hahn, R. G. Understanding volume kinetics. Acta Anaesthesiol. Scand. 64, 570–578. https://doi.org/10.1111/aas.13533 (2020).
Wang, T. et al. Effects of albumin and crystalloid priming strategies on red blood cell transfusions in on-pump cardiac surgery: A network meta-analysis. BMC Anesthesiol. 24, 26. https://doi.org/10.1186/s12871-024-02414-y (2024).
Arya, V. K., Nagdeve, N. G., Kumar, A., Thingnam, S. K. & Dhaliwal, R. S. Comparison of hemodynamic changes after acute normovolemic hemodilution using Ringer’s lactate versus 5% albumin in patients on beta-blockers undergoing coronary artery bypass surgery. J. Cardiothorac. Vasc. Anesth. 20, 812–818. https://doi.org/10.1053/j.jvca.2005.04.012 (2006).
Dubois, M. J. et al. Albumin administration improves organ function in critically ill hypoalbuminemic patients: A prospective, randomized, controlled, pilot study. Crit. Care Med. 34, 2536–2540. https://doi.org/10.1097/01.CCM.0000239119.57544.0C (2006).
Martensson, J. et al. Small volume resuscitation with 20% albumin in intensive care: Physiological effects : The SWIPE randomised clinical trial. Intensive Care Med. 44, 1797–1806. https://doi.org/10.1007/s00134-018-5253-2 (2018).
Bunn, F. & Trivedi, D. Colloid solutions for fluid resuscitation. Cochrane Database Syst. Rev. 2012, CD001319. https://doi.org/10.1002/14651858.CD001319.pub5 (2012).
Yanase, F. et al. A comparison of the hemodynamic effects of fluid bolus therapy with crystalloids vs. 4% albumin and vs. 20% albumin in patients after cardiac surgery. Heart Lung 50, 870–876. https://doi.org/10.1016/j.hrtlng.2021.07.014 (2021).
Finfer, S. et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N. Engl. J. Med. 350, 2247–2256. https://doi.org/10.1056/NEJMoa040232 (2004).
Investigators, S. S. et al. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Med. 37, 86–96. https://doi.org/10.1007/s00134-010-2039-6 (2011).
Perel, P., Roberts, I. & Ker, K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD000567.pub6 (2013).
Hahn, R. G. Volume kinetics for infusion fluids. Anesthesiology 113, 470–481. https://doi.org/10.1097/ALN.0b013e3181dcd88f (2010).
Xu, H. et al. Perioperative albumin supplementation is associated with decreased risk of complications following microvascular head and neck reconstruction. J. Oral Maxillofac. Surg. 79, 2155–2161. https://doi.org/10.1016/j.joms.2021.04.030 (2021).
Weinberg, L. et al. Associations of fluid amount, type, and balance and acute kidney injury in patients undergoing major surgery. Anaesth. Intensive Care 46, 79–87. https://doi.org/10.1177/0310057X1804600112 (2018).
Firth, J. D., Raine, A. E. & Ledingham, J. G. Raised venous pressure: A direct cause of renal sodium retention in oedema?. Lancet 1, 1033–1035. https://doi.org/10.1016/s0140-6736(88)91851-x (1988).
Martin, G. S. & Bassett, P. Crystalloids vs. colloids for fluid resuscitation in the Intensive Care Unit: A systematic review and meta-analysis. J. Crit. Care 50, 144–154. https://doi.org/10.1016/j.jcrc.2018.11.031 (2019).
Nishimoto, M. et al. Positive association between intra-operative fluid balance and post-operative acute kidney injury in non-cardiac surgery: The NARA-AKI cohort study. J. Nephrol. 33, 561–568. https://doi.org/10.1007/s40620-019-00688-x (2020).
Zhang, Z. et al. Effect of albumin administration on post-operation mortality, duration on ventilator, and hospital stay on patients in cardiac intensive care: An observational study. Trop. J. Pharm. Res. 18, 1339–1345 (2019).
Vincent, J. L., Navickis, R. J. & Wilkes, M. M. Morbidity in hospitalized patients receiving human albumin: A meta-analysis of randomized, controlled trials. Crit. Care Med. 32, 2029–2038. https://doi.org/10.1097/01.ccm.0000142574.00425.e9 (2004).
Djordjevic, A., Susak, S., Velicki, L. & Antonic, M. Acute kidney injury after open-heart surgery procedures. Acta Clin. Croat 60, 120–126. https://doi.org/10.20471/acc.2021.60.01.17 (2021).
Prowle, J. R. et al. Postoperative acute kidney injury in adult non-cardiac surgery: Joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative. Nat. Rev. Nephrol. 17, 605–618. https://doi.org/10.1038/s41581-021-00418-2 (2021).
Grams, M. E. et al. Acute kidney injury after major surgery: A retrospective analysis of veterans health administration data. Am. J. Kidney Dis. 67, 872–880. https://doi.org/10.1053/j.ajkd.2015.07.022 (2016).
Chen, L.-S. & Singh, R. J. Utilities of traditional and novel biomarkers in the management of acute kidney injury. Crit. Rev. Clin. Lab. Sci. 57, 215–226. https://doi.org/10.1080/10408363.2019.1689916 (2020).
Brilakis, E. S. et al. Incidence and clinical outcome of minor surgery in the year after drug-eluting stent implantation: Results from the Evaluation of Drug-Eluting Stents and Ischemic Events Registry. Am. Heart J. 161, 360–366. https://doi.org/10.1016/j.ahj.2010.09.028 (2011).
Guyatt, G. et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 64, 383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026 (2011).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14, 135. https://doi.org/10.1186/1471-2288-14-135 (2014).
Acknowledgements
This paper supported by a Korea University grant (K2409171).
Author information
Authors and Affiliations
Contributions
K.S.L: contribution to the conception of the article, interpretation, and analysis of data, and drafting of the article. J.E.K: contribution to the conception of the article, search, interpretation, and analysis of data of the article. G.K: contribution to analysis of date of the article. Y.J.W: contribution to search, interpretation, and analysis of data, and revising the article for content. Y.J.C: contribution to the design of the article, interpretation of data and revising the article for content. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, K.S., Kim, J.E., Kang, G. et al. The effect of human albumin administration on postoperative renal function following major surgery: a systematic review and meta-analysis. Sci Rep 14, 16599 (2024). https://doi.org/10.1038/s41598-024-62495-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-62495-0
- Springer Nature Limited