Abstract
Lymphocyte subsets are the most intuitive expression of the body’s immune ability, and the lymphocyte-to-monocyte ratio (LMR) also clearly reflect the degree of chronic inflammation activity. The purpose of this study is to investigate their predictive value of lymphocyte subsets and LMR to neoadjuvant therapy (NAT) efficacy in breast cancer patients. In this study, lymphocyte subsets and LMR were compared between breast cancer patients (n = 70) and benign breast tumor female populations (n = 48). Breast cancer patients were treated with NAT, and the chemotherapy response of the breast was evaluated using established criteria. The differences in lymphocyte subsets and LMR were also compared between pathological complete response (pCR) and non-pCR patients before and after NAT. Finally, data were analyzed using SPSS. The analytical results demonstrated that breast cancer patients showed significantly lower levels of CD3 + T cells, CD4 + T cells, CD4 + /CD8 + ratio, NK cells, and LMR compared to benign breast tumor women (P < 0.05). Among breast cancer patients, those who achieved pCR had higher levels of CD4 + T cells, NK cells, and LMR before NAT (P < 0.05). NAT increased CD4 + /CD8 + ratio and decreased CD8 + T cells in pCR patients (P < 0.05). Additionally, both pCR and non-pCR patients exhibited an increase in CD3 + T cells and CD4 + T cells after treatment, but the increase was significantly higher in pCR patients (P < 0.05). Conversely, both pCR and non-pCR patients experienced a decrease in LMR after treatment. However, this decrease was significantly lower in pCR patients (P < 0.05). These indicators demonstrated their predictive value for therapeutic efficacy. In conclusion, breast cancer patients experience tumor-related immunosuppression and high chronic inflammation response. But this phenomenon can be reversed to varying degrees by NAT. It has been found that lymphocyte subsets and LMR have good predictive value for pCR. Therefore, these markers can be utilized to identify individuals who are insensitive to NAT early on, enabling the adjustment of treatment plans and achieving precise breast cancer treatment.
Similar content being viewed by others
Introduction
Metastasis is the main cause of death in breast cancer, which is the most common malignant tumor in women and is ranked second in mortality among female malignancies1. Currently, neoadjuvant therapy (NAT) is commonly recommended for advanced breast cancer, as it can effectively lower the tumor stage, reduce metastasis, and increase the chances of surgery as well as breast preservation2. However, the efficacy of NAT varies from individual to individual, making it challenging for clinicians to determine its effectiveness timely and effectively. If the therapeutic effect cannot be assessed promptly, it may cause delays in surgical opportunities and tumor progression, ultimately reducing patients’ survival rates. Although Miller-Payne grading system can be used as a gold standard for postoperative pathological evaluation, it can only be obtained from postoperative specimens, which has a certain delay. After chemotherapy, tumor cells undergo degeneration, necrosis, and the formation of granulation tissue or scar tissue due to hyperplasia, which occupy the original tumor bed. Therefore, in some cases, the mass may not show a significant reduction in size on imaging examination. Ultrasound and other imaging evaluation methods, although capable of assessing treatment response in a timely manner, may encounter limitations in such cases. Consequently, it is crucial to explore a simpler, more timely, and accurate method for evaluating the therapeutic effect. In the past, researchers have been looking for new predictive markers. The relationship between immune cells and tumor cells has been extensively studied with the deepening of research on tumor immunology. It has been found that there are significant immunosuppression and immune disorders in patients with malignant tumors such as lung cancer, esophageal cancer, gastric cancer, colon cancer and gastric cancer, with decreased levels of CD3 + T cells, CD4 + T cells, CD8 + T cells, NK cells and other immune effector cells3,4. Immune dysfunction weakens the body’s ability to recognize mutated cells and tumor cells, allowing them to escape from the killing effect of immune system and metastasize from the primary site. In addition, for the special population of patients with malignant tumors, researchers have discovered the dual effects of chemotherapy on the immune function of the body. On one hand, chemotherapy, as a systemic treatment method, kills tumor cells while also killing some normally functioning immune cells, inhibiting the differentiation of immune cells. On the other hand, chemotherapy indirectly reduces the inhibitory effect of tumor cells on the immune system after killing tumor cells5,6. Therefore, we speculate that for individuals sensitive to chemotherapy, the tumor burden of the patient decreases after receiving chemotherapy, leading to weaken tumor-related immunosuppressive effect, which may restore the patient’s immune function. However, for patients who are not sensitive to chemotherapy, there is no significant increase in various immune indicators after treatment, and even a decrease may occur, because chemotherapy not only cannot effectively kill tumor cells but may further damage the immune system. Certain studies suggest that pre-existing immune responses may enhance the effectiveness of traditional chemotherapy drugs. Li et al.7 has reported a correlation between lymphocytes and the therapeutic response and prognosis of certain tumor patients receiving NAT. Therefore, we speculate that monitoring the lymphocyte subsets in the body may be a novel approach to assess treatment effectiveness.
In addition, inflammatory cells have been discovered in the majority of solid tumors, including colon, stomach, and liver cancers8,9. Tumor-related systemic inflammation is not only an important factor promoting tumorigenesis and progression but also an independent factor affecting prognosis10,11. Previous studies has demonstrated a 40%-50% reduction in the risk of colorectal cancer associated with the use of nonsteroidal anti-inflammatory drugs (NSAIDs)12. The lymphocyte-to-monocyte ratio (LMR) is one of the evaluation indicators for the degree of systemic inflammatory response13. Studies have shown that breast cancer patients with high LMR before NAT have significantly prolonged disease-free survival (DFS), and high LMR patients have lower recurrence rates and better survival rates after NAT14,15. After effective chemotherapy, the tumor burden decreases and the tumor-related inflammatory response weakens. Therefore, we speculate that LMR can also be used as an effective predictor of NAT efficacy. Moreover, lymphocyte subsets and LMR can be directly obtained from peripheral venous blood, which has the advantages of simplicity, real-time detection, and low cost. The aim of this study is to further explore the predictive value of lymphocyte subsets and LMR for the efficacy of breast cancer patients receiving NAT, providing reference for clinical treatment planning.
Data and methods
General information
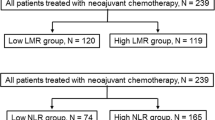
Collected from August 2022 to May 2023 in the First Affiliated Hospital of Chongqing Medical University, female patients with breast cancer who underwent NAT were included in the case group. At the same time, a control group consisting of 48 female individuals with histologically confirmed breast fibroadenoma was included in the study. The inclusion criteria for the case group were: (1) female patients aged 18–80 years; (2) no acute or chronic inflammation, other tumors, and autoimmune diseases such as hyperthyroidism and rheumatoid arthritis; (3) complete clinical and postoperative pathological data. The exclusion criteria were: (1) pregnant or breastfeeding patients; (2) prior steroid, immunosuppressive or immunoenhancement drug treatment; (3) prior anti-inflammatory drug treatment; (4) patients with chemotherapy contraindications; (5) patients who were assessed as having no response or tumor progression during treatment and required a change in treatment regimen. According to the inclusion and exclusion criteria, a total of 70 patients were included in the case group, with an average age of 52.73 ± 9.90 years. Among them, 38 (54.3%) were postmenopausal. 6 cases (8.6%) had tumor size ≤ 2 cm, 49 cases (70.0%) had tumor size > 2 cm and ≤ 5 cm, and 15 cases (21.4%) had tumor size > 5 cm. 62 cases (88.6%) had lymph node metastasis. According to the eighth edition of the AJCC TNM staging system, ≤ II stage in 24 cases (34.3%) and ≥ III stage in 46 cases (65.7%). Furthermore, based on the different expression statuses of hormone receptor and HER-2 receptor, the case group patients were divided into hormone receptor-positive group, HER-2 receptor-positive group, and triple-negative group. Patients who were hormone receptor-positive and HER-2 receptor-negative were included in the hormone receptor-positive group, with a total of 21 cases (30.0%); patients who were HER-2 receptor-positive regardless of hormone receptor status were included in the HER-2 receptor-positive group, with a total of 36 cases (51.4%); and patients who were negative for both hormone receptor and HER-2 receptor were included in the triple-negative group, with a total of 13 cases (18.6%). Based on a Ki-67 expression cut-off of ≤ 20%, Ki-67 low expression (≤ 20%) in 21 cases (30.0%), and high expression (> 20%) in 49 cases (70.0%). Out of the total patients, 28 (40.0%) achieved pCR while 42 (60.0%) did not. In the control group of 48 benign breast tumor female subjects, the average age was 49.23 ± 11.34 years. Among them, postmenopausal in 19 cases (39.6%). Tumor size ≤ 2 cm in 12 cases (25.0%), tumor size > 2 cm and ≤ 5 cm in 25 cases (52.1%), and tumor size > 5 cm in 11 cases (22.9%). There were no significant differences in age, menstrual status, and tumor size between the two groups (P ≥ 0.05), indicating good comparability between the two groups. This study was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University. Data collection began on October 13, 2023.
Treatment method
Both hormone receptor-positive and triple-negative subtypes patients received the TAC neoadjuvant chemotherapy regimen, which included intravenous infusion of 75 to 80 mg/m2 of docetaxel or 175 mg/m2 of paclitaxel on day 1; intravenous infusion of 90/50 mg/m2 of epirubicin or pirarubicin on day 1; and intravenous infusion of 600 mg/m2 of cyclophosphamide on day 1. And HER-2 receptor-positive group patients received a neoadjuvant therapy regimen that included targeted agents (AC-THP regimen), which was an addition of trastuzumab and pertuzumab to the TAC regimen. Three weeks constituted one cycle, and the patients were evaluated for clinical efficacy every two cycles. Patients either continued with the current chemotherapy regimen if the treatment was effective or underwent a change in chemotherapy regimen or surgery if the treatment was ineffective or the tumor progressed. Surgical treatment was performed two weeks after the completion of the prescribed cycle of NAT.
Ethical approval
The studies involving human participants were reviewed and approved by the institutional ethics committee of the First Affiliated Hospital of Chongqing Medical University, and all experiments were performed in accordance with relevant guidelines and regulations. As this was a retrospective non-interventional study, written informed consent was not required from participants in accordance with national legislation and institutional requirements, and the application for exempted informed consent for the study has been approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University.
Detection method
Lymphocyte subset detection
Case group patients were drawn peripheral venous blood 2 ml before NAT and after 6 cycles of NAT prior to surgery. With heparin as anticoagulant, 100 μl was taken from each sample, added 20 μl of monoclonal antibodies CD3, CD4, CD8, CD16, CD19, and CD56-fluorescently labeled single clones, and incubated in the dark for 30 min. Then phosphate buffered saline (PBS) 3 ml was added for washing, centrifuged at 1500 r/min for 5 min, and washed again with PBS 1 ml. The proportion of CD3 + T cells, CD3 + CD4 + T cells, CD3 + CD8 + T cells, CD3 + CD4 − CD8 − T cells, CD3 + CD4 + CD8 + T cells, CD3 − CD16 + CD56 + NK cells, CD3 + CD16 + CD56 + NKT cells, and CD19 + B cells was detected by flow cytometry. Monoclonal antibodies and flow cytometers were purchased from BD Biosciences (USA), and the operation was carried out according to the instructions of the reagent. Control group patients were also sampled prior to pathological biopsy, using the same method as the case group.
Routine blood test
Case group patients were draw 5 ml venous blood before NAT and surgery and put it into an anticoagulant tube for inspection. The centrifuge was set to a speed of 1500 r/min with a radius of 15 cm, spun for 10 min. Mindray BC5180 automated hematology analyzer and supporting reagents were used to detect lymphocyte and monocyte counts. The test was repeated three times, and the average value of the three tests was used as the final result. Collected lymphocyte and monocyte counts data were used to calculate the LMR value. (LMR = lymphocyte count/monocyte count).
Criteria for efficacy evaluation
NAT efficacy was evaluated using the Miller-Payne grading system for breast cancer treatment response. It was divided into grades 1–5. Grade 5 was considered a pathological complete response (pCR). Pathological efficacy evaluation was completed by a senior pathologist and then reviewed by a higher-level pathologist.
Statistical method
Data analysis was carried out using SPSS 25.0 statistical software. Quantitative data that meet the normal distribution were expressed as the mean ± standard deviation (x ± s), and the independent sample t-test was used for group comparison. Quantitative data that did not meet the normal distribution were expressed as M (P25, P75), and the Wilcoxon (Mann–Whitney U) test was used for group comparison. Multiple group comparisons were performed using the Kruskal–Wallis test (KW test). Qualitative data were expressed as n (%), and the chi-square test or KW test was used for group comparison. Statistically significant indicators in univariate analysis were included in the multivariate analysis model, and binary logistic regression was used for multivariate analysis. The receiver operating characteristic (ROC) curve was used to evaluate the predictive value of each index for NAT efficacy, and the Youden index was used to determine the optimal cutoff value. When P < 0.05, the difference was considered statistically significant.
Results
Comparison of lymphocyte subsets and LMR levels in the control and case groups
Univariate analysis results showed that there were no significant differences in age, menstrual status, and tumor size between the two groups (P ≥ 0.05). The levels of CD3 + T cells, CD4 + T cells, CD4 + /CD8 + ratio, NK cells, and LMR were lower in the case group compared to the control group, with statistically significant differences (P < 0.05). There were no significant differences in CD8 + T cells, CD3 + CD4 − CD8 − T cells, CD3 + CD4 + CD8 + T cells, NKT cells, and CD19 + B cells between the two groups (P ≥ 0.05) (Table 1).
Comparison of lymphocyte subsets and LMR levels in the pCR and non-pCR groups before NAT
The levels of CD4 + T cells, NK cells, and LMR were lower in the non-pCR group compared to the pCR group before NAT, with statistically significant differences (P < 0.05). There were no significant differences in CD3 + T cells, CD8 + T cells, CD4 + /CD8 + ratio, CD3 + CD4 − CD8 − T cells, CD3 + CD4 + CD8 + T cells, NKT cells, and CD19 + B cells between the two groups (P ≥ 0.05) (Table 2).
Comparison of different clinical features in the pCR and non-pCR groups before NAT
There was a significant difference in Ki-67 expression level between the pCR group and non-pCR group before NAT (P < 0.05). However, there were no significant differences in TNM staging, lymph node metastasis, and molecular typing between the two groups (P ≥ 0.05) (Table 3).
Comparison of changes in lymphocyte subsets and LMR in the pCR and non-pCR groups after NAT
We denoted the magnitude of change in lymphocyte subsets and LMR before and after NAT as Delta-lymphocyte subsets and Delta-LMR. After NAT, significant differences were observed in the dCD3 + T cells, dCD4 + T cells, dCD8 + T cells, dCD4 + /CD8 + ratio, and dLMR between the non-pCR group and pCR group (P < 0.05). In both groups, the levels of CD3 + T cells and CD4 + T cells increased after treatment. However, these increases were significantly higher in the pCR group compared to the non-pCR group. The level of CD8 + T cells decreased in the pCR group after treatment, while it increased in the non-pCR group. The change trend of CD4 + /CD8 + ratio was opposite to that of CD8 + T cells. More specifically, the level of CD4 + /CD8 + ratio increased in the pCR group after treatment, while it decreased in the non-pCR group. Additionally, both groups exhibited a decrease in LMR after NAT, but the decrease was significantly higher in the non-pCR group. However, no significant differences were observed dCD3 + CD4 − CD8 − T cells, dCD3 + CD4 + CD8 + T cells, dNK cells, dNKT cells, and dCD19 + B cells levels between the two groups (P ≥ 0.05) (Table 4).
Logistic multivariate analysis of factors influencing NAT efficacy
In the multifactorial logistic regression model, the independent variables included lymphocyte subset indexes and LMR before NAT, which were found to be statistically significant in univariate analysis. After adjusting for the effect of Ki-67 level, the model indicated that CD4 + T cells and LMR before NAT served as independent predictors of pCR (OR 1.119, 95% CI 1.031–1.213, P = 0.007; OR: 2.169, 95% CI 1.336–3.519, P = 0.002) (Table 5). Following this, Delta-lymphocyte subsets and Delta-LMR with significant differences in univariate analysis were included as independent variables in a multivariate logistic regression model. After adjusting for the effect of Ki-67 level, the results showed that dCD3 + T cells, dCD8 + T cells, and dLMR were also independent predictors of pCR (OR 1.101, 95% CI 1.019–1.191, P = 0.015; OR 0.892, 95% CI 0.821–0.968, P = 0.006; OR 1.960, 95% CI 1.004–3.827, P = 0.049) (Table 6).
ROC curve reveals the predictive value of lymphocyte subsets and LMR for NAT efficacy
ROC curve analysis showed that the AUCs of CD4 + T cells and LMR before NAT were 0.678 (95% CI 0.548–0.808) and 0.707 (95% CI 0.583–0.831), with sensitivities of 46.4% and 50.0%, specificities of 85.7 and 85.6%, respectively. The AUCs of dCD3 + T cells, dCD8 + T cells, and dLMR were 0.639 (95% CI: 0.507–0.770), 0.701 (95% CI: 0.568–0.833), 0.676 (95% CI 0.546–0.806), respectively. Their sensitivities were 71.4, 83.3, 67.9, and specificities were 52.4, 57.1, 69.0%, respectively (Table 7; Fig. 1). When the lymphocyte subsets indicators dCD3 + T cells and dCD8 + T cells were used together for diagnosis, the AUC was 0.739 (95% CI: 0.617–0.861), with a sensitivity of 64.3% and a specificity of 73.8% (Table 8; Fig. 2). Hence, CD4 + T cells, LMR before NAT, and dCD3 + T cells, dCD8 + T cells, dLMR were significantly correlated with pCR and possess predictive value. Moreover, utilizing lymphocyte subset indicators in combination further improved their predictive capability.
Discussion
In recent years, research has shown that the occurrence, progression, and metastasis of tumors are closely related to the immune status and inflammatory response in the tumor host16. A decrease in the body’s immune surveillance function and the immune cytotoxic function allows abnormal proliferative cells and tumor cells to achieve immune escape, promoting the formation and progression of malignant tumors, including breast cancer17,18. The most direct indicator of the body’s immune ability is the number of lymphocytes. According to different surface markers and differentiation antigens, lymphocytes are divided into different subsets. CD3 antigen is found on mature T lymphocytes, making it a general indicator for T lymphocytes and strength of cellular immune response. Mature T lymphocytes further express CD4 or CD8 antigens on their surface. CD4 + T cells can directly secrete cytokines such as IFN-α, TNF-γ, IL-2, which have anti-tumor effects, and also activate immune effector cells such as CD8 + T cells and NK cells to indirectly exert anti-tumor effects19. CD8 + T cells not only release granzyme and perforin to kill tumor cells, but also differentiate into cytotoxic T lymphocytes (CTL) to directly play an anti-tumor effect. Under normal conditions, most of the interior of CD8 + T cells are made up of CTL, and a few are suppressor T lymphocytes (Ts), which can inhibit the body’s immune response20. The dynamic balance within the T cell subsets is reflected by the CD4 + /CD8 + ratio. A decrease in this ratio indicates that the lymphatic system inside the patient is in a disordered state, and the anti-tumor ability of the immune system is reduced21. CD3 + CD4 − CD8 − T cells are a rare T lymphocyte subset that exerts anti-tumor effects through mechanisms such as the Fas/FasL pathway, cytokine secretion, and expression of tumor necrosis factor-associated apoptosis-inducing ligand (TRAIL)22,23. CD3 + CD4 + CD8 + T cells are a small subset of lymphocytes that has received relatively little research attention. Currently, there are two mainstream views regarding the role of CD3 + CD4 + CD8 + T cells. One view is that CD3 + CD4 + CD8 + T cells are highly cytotoxic as they express numerous cytotoxic-related immune molecules such as CRTAM, CD244, granzyme B, perforin, and IFN-γ24; Another view is that CD3 + CD4 + CD8 + T cells have immunosuppressive properties as they express IL-10 and IFN-γ, which reduce T-cell proliferation25,26. CD19 + B cells are a type of inhibitory B lymphocyte that can increase the expression of regulatory T cells to inhibit the activation of CD4 + T cells and promote immune escape in tumors27. NK cells are non-specific immune cells derived from bone marrow large granular lymphocytes. They have the ability to directly kill tumor cells through nonspecific killing without specific sensitizing antigens for activation28. NKT cells are unique immune cells that have both NK cells functions and T cell characteristics. They can recognize glycolipid antigens presented by CD1d molecules on tumor cells and exert tumor-killing effects by relying on CD95/CD178 molecules29. In this study, breast cancer patients had significantly reduced levels of CD3 + T cells, CD4 + T cells, CD4 + /CD8 + ratio, and NK cells, confirming that the transition of a tumor from benign to malignant can lead to significant immunosuppression. This suggests that the specific and non-specific killing effects of immune cells are impaired in these patients. It is possible that tumor cells inhibit lymphocyte differentiation and proliferation by secreting immunosuppressive factors such as TGF-β and IL-10, which leads to an imbalance in lymphocyte subsets30. Furthermore, the decrease in CD4 + /CD8 + ratio observed in breast cancer patients further revealed the presence of an immunological disorder. Previous studies have demonstrated that low CD4 + /CD8 + ratio is a crucial indicator of the severity and poor prognosis of malignant tumors, with a lower ratio indicating a higher risk of tumor metastasis and recurrence31. However, the occurrence of malignant tumors is not determined by a single factor. As early as Rudolf Virchow’s research, it was found that there were white blood cells in tumor tissue. When the body’s repair function was disordered due to a tumor, it stimulated the body to produce an inflammatory response that created a favorable microenvironment for tumor cells, accelerating their growth. This initialized the hypothesis of “relationship between inflammation and cancer”32. Monocytes, as a type of inflammatory cells, not only secrete inflammatory factors such as IL-1, IL-6, IL-10, and TNF-α to promote tumor microangiogenesis, but also assist in the adhesion of tumor cells to endothelial cells, thereby promoting breast cancer metastasis33. Monocytes are recruited to the peritumor tissue and differentiate into tumor associated macrophages (TAMs). TAMs contribute to tumor cells migration and invasion by reshaping the extracellular matrix and releasing mediators like VEGF, PDGF, and EGF. These mediators induce a hypoxic microenvironment and facilitate the formation of tumor microvessels34,35. TAMs also express IDO and IL-10 to play immunosuppressive roles36. In this study, we found that breast cancer patients had significantly lower LMR compared to benign breast tumor individuals, indicating that chronic inflammation might be a risk factor for breast cancer. Previous studies have shown that a lower LMR is indicative of a higher tumor burden in patients. Additionally, a low LMR prior to treatment is significantly linked to unfavorable DFS and overall survival (OS)37. Therefore, the immune system and inflammatory response are crucial factors in the occurrence and progression of breast cancer. Tumor cells originate from genetic mutations, leading to disruption in the body’s repair mechanisms that stimulates chronic inflammation. The presence of tumor cells also causes tumor-associated immunosuppression. Additionally, abnormality in immune function reduces the elimination of chronic inflammation. Ultimately, the prolonged presence of immunosuppression and chronic inflammation promotes tumor progression in turn, which forms a vicious circle. A deeper comprehension of the intricate relationships between these three factors is currently a hot topic in breast cancer research. And understanding these interactions can lay the groundwork for breaking the vicious cycle, consequently leading to more precise and effective treatment options for breast cancer in the future.
Currently, NAT is the preferred initial treatment for locally advanced breast cancer (LABC). Recent studies indicated that attaining a pCR after NAT leads to a more favorable prognosis and increased survival rates compared to those without pCR38,39. Therefore, early prediction of NAT efficacy is crucial in assessing drug sensitivity, selecting subsequent treatment regimens, and improving overall survival quality. Previous research has shown that effective treatment can rectify immune disorders, restore immune function, and alleviate chronic inflammation in patients with malignant tumors, despite their suppressed immune function40. In this study, 70 breast cancer patients underwent NAT. Among them, 28 achieved pCR, while 42 did not. Prior to NAT, notable disparities in lymphocyte subsets were observed between the two groups. Individuals in the pCR group exhibited significantly elevated levels of CD4 + T cells and NK cells in comparison to the non-pCR group. A possible mechanism is that the higher levels of T cells before NAT can help induce anti-tumor immunity during chemotherapy. Chemotherapy can stimulate the body’s immune response to the tumor. A more robust immune system function prior to chemotherapy is associated with a more intense immune response. This, in turn, enhances the effectiveness of chemotherapeutic drugs41,42. Denkert et al.43 discovered that the presence of tumor-infiltrating lymphocytes (TILs) is associated with increased response rates in breast cancer patients receiving NAT, and the enrichment of TILs can improve chemotherapy sensitivity. CD4 + T cells are one of the major components of TILs44. In addition, Verma et al.45 found that elevated NK cells in peripheral blood may be associated with favorable therapeutic effects of chemotherapy on breast cancer patients, possibly through mechanisms such as promoting NKG2D expression and the presence of Granzyme B( +)/perforin( +) cells. This study also discovered a positive correlation between high LMR prior to NAT and increased pCR rates. This suggests that individuals with lower levels of chronic inflammation before NAT are more likely to exhibit a heightened pathological response rate. Previous studies have found that TAMs can predict the sensitivity of radiotherapy and chemotherapy. This is because TAMs can not only release chemotherapy resistance factors, making breast cancer cells insensitive to chemotherapy, but also exhibit increased release of VEGF under radiation exposure, thus reducing radiotherapy sensitivity46. Ni et al.47 analyzed 542 LABC patients and found that high LMR before NAT is a significant favorable factor for NAT response and prognosis. This study’s multivariate analysis further demonstrated that high levels of CD4 + T cells and LMR before NAT are independent predictors of better pathological response rates. Additionally, high Ki-67 expression predicts tumor cell proliferation activity, and chemotherapeutic agents have stronger killing effects on proliferating cells. Consistent with previous studies, we found a correlation between high Ki-67 expression and a high pCR rate, suggesting that Ki-67 is also a factor related to NAT efficacy48.
Chemotherapy, as a systemic treatment approach, exhibits cytotoxic effects on tumor cells. However, due to the limitations in drug selectivity, it inevitably leads to collateral damage to the normal immune system of the body. Nevertheless, once the tumor cells are effectively eliminated by the chemotherapy drugs, their inhibitory effect on the immune system diminishes accordingly. Concurrently, the inflammatory stimulation within the tumor microenvironment also decreases49,50. Therefore, the role of chemotherapy in the immune status and chronic inflammation of the body is worth further research and exploration. Different from previous studies, our research also focuses on the changes in lymphocyte subsets and LMR before and after NAT, denoted as Delta-lymphocyte subsets and Delta-LMR. These dynamic quantitative indicators allow for a clearer representation of the changes brought about by NAT, while avoiding biases caused by inconsistent baseline characteristics among patients. The findings of this study found significant differences in the levels of dCD3 + T cells, dCD4 + T cells, dCD8 + T cells, dCD4 + /CD8 + ratio, and dLMR between pCR and non-pCR patients after NAT. To be more specific, the pCR group showed a significant increase in CD3 + T cells, CD4 + T cells, and CD4 + /CD8 + ratio compared to the non-pCR group. This indicate that after effective treatment, the tumor burden in the patients is significantly alleviated. As a result, the suppressive effect of tumor cells on the immune system is weakened, leading to a gradual recovery of immune function and normal production of CD3 + T cells and CD4 + T cells. In contrast, the non-pCR group exhibited a decrease in CD4 + /CD8 + ratio after treatment. This suggests that for chemotherapy-insensitive patients, not only do chemotherapy drugs damage the immune system but their tumor burden is not effectively reduced. During tumor progression, immune suppressive factors continue to be released, disrupting the homeostasis within lymphocyte subsets. Consequently, there is an increased dominance of lymphocytes with suppressive effects, causing a shift in the CD4 internal Th1/Th2 balance towards Th2. Additionally, there are an enhancement of activity and an increase in the number of Ts cells characterized by the CD8 + phenotype51,52. Simultaneously, the increased Ts cells have a regulatory inhibitory effect on CD4 + T cells, hindering their expression and maturation. As a result, the surface expression of CD4 antigen on lymphocytes decreases and the reactivity of CD8 + T cells increases. However, during this process, the body is in an immunosuppressed state, and the increased number of CD8 + T cells is dominated by Ts cells, further exacerbating the suppressive effects on CD4 + T cells53,54. Therefore, an increase in CD8 + T cells proportion and a decrease in CD4 + /CD8 + ratio were observed after NAT among patients with high tumor burden in the non-pCR group. During this period, the body experiences severe immune disorders, hindering its ability to effectively exert anti-tumor effects. Furthermore, this study revealed that following NAT, there was a decline in LMR for both the pCR and non-pCR groups. However, the decrease in LMR was notably greater in the non-pCR group than in the pCR group, and this difference was statistically significant. One possible reason is that chemotherapy drugs such as taxanes have been found to increase serum levels of IL-2, IL-6, GM-CSF, IFN-α, TNF-γ, and PGE2, these factors not only stimulate the proliferation of immune effector cells to exert anti-tumor effects but also trigger an inflammatory response in the body. This leads to the proliferation of monocytes and macrophages, which further intensify the inflammatory reaction by engulfing or phagocytosing antigenic substances55,56, resulting in a decrease in post-treatment LMR. However, patients who achieved pCR experienced immune function restoration, enhancing the inhibitory effect on this exacerbated inflammatory response. As a result, although the LMR might decrease in these patients, the extent of decrease was much lower compared to non-pCR patients. Our additional ROC curve analysis showed that dCD3 + T cells, dCD8 + T cells, and dLMR had good predictive value for treatment efficacy. Early identification of patients with poor therapeutic effects is key to subsequent treatment decisions. For these patients, their immune function remains suppressed and chronic inflammation is constantly activated, which further promotes tumor proliferation. As a result, even after completing the scheduled NAT cycle, they may fail to achieve ideal pathological complete remission.
Past research demonstrated a close correlation between the occurrence of tumors and the immune status of the organism, with immune cells participating in various pathways involved in the initiation and progression of tumors. In previous studies on patients with malignant neoplasms such as lung cancer, esophageal cancer, colorectal cancer, and gastric cancer, researchers have detected decreased levels of CD3 + T cells, CD4 + T cells , NK cells, and CD4 + /CD8 + ratio in peripheral blood4,57,58,59,60. The commonality among these findings reveals a prevalent state of immunosuppression in patients with malignant tumors, suggesting that changes in immune cell populations may be intimately associated with tumor burden in the body. This study examines the correlation between immune status, chronic inflammation, and NAT in breast cancer patients. It demonstrates the significance of lymphocyte subsets and LMR in forecasting the effectiveness of NAT in breast cancer. The aim is to provide clinicians with new prediction methods and reference criteria for NAT efficacy, which can improve prediction accuracy and provide more support for precise breast cancer treatment. Early identification of patients with poor treatment efficacy and timely adjustment of their treatment plan may improve the overall prognosis. However, this study still has some limitations. Firstly, it is a small-sample, single-center study. To confirm the conclusions drawn in this study, there is a need for large-sample, multi-center clinical studies. Secondly, venous blood samples were collected and analyzed only before NAT and prior to surgery in this study. However, immune damage and chronic inflammation are persistent processes, and dynamic monitoring of venous blood may provide a clearer understanding of these chronic processes. Additionally, long-term follow-up allows for the collection of subsequent survival data from patients, enabling the investigation of the correlation between lymphocyte subsets, LMR, and long-term prognosis among patients receiving NAT.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72(1), 7–33 (2022).
Liu, S. V., Melstrom, L., Yao, K., Russell, C. A. & Sener, S. F. Neoadjuvant therapy for breast cancer. J. Surg. Oncol. 101(4), 283–291 (2010).
Chraa, D., Naim, A., Olive, D. & Badou, A. T lymphocyte subsets in cancer immunity: Friends or foes. J. Leukoc. Biol. 105(2), 243–255 (2019).
Wang, Q. et al. Changes in T lymphocyte subsets in different tumors before and after radiotherapy: A meta-analysis. Front. Immunol. 12, 648652 (2021).
Zitvogel, L., Apetoh, L., Ghiringhelli, F. & Kroemer, G. Immunological aspects of cancer chemotherapy. Nat. Rev. Immunol. 8(1), 59–73 (2008).
Apetoh, L., Tesniere, A., Ghiringhelli, F., Kroemer, G. & Zitvogel, L. Molecular interactions between dying tumor cells and the innate immune system determine the efficacy of conventional anticancer therapies. Cancer Res. 68(11), 4026–4030 (2008).
Li, Y. et al. Clinicopathological and prognostic significance of high circulating lymphocyte ratio in patients receiving neoadjuvant chemotherapy for advanced gastric cancer. Sci. Rep. 8(1), 6223 (2018).
Allavena, P., Garlanda, C., Borrello, M. G., Sica, A. & Mantovani, A. Pathways connecting inflammation and cancer. Curr. Opin. Genet. Dev. 18(1), 3–10 (2008).
Mantovani, A., Allavena, P., Sica, A. & Balkwill, F. Cancer-related inflammation. Nature 454(7203), 436–444 (2008).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, inflammation, and cancer. Cell 140(6), 883–899 (2010).
Roxburgh, C. S. D. & McMillan, D. C. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. Lond. Engl. 6(1), 149–163 (2010).
Rodríguez, L. A. G. & Huerta-Alvarez, C. Reduced risk of colorectal cancer among long-term users of aspirin and nonaspirin nonsteroidal antiinflammatory drugs. Epidemiol. Camb. Mass. 12(1), 88 (2001).
Lee, K. H. et al. The prognostic and predictive value of tumor-infiltrating lymphocytes and hematologic parameters in patients with breast cancer. BMC Cancer 18(1), 938 (2018).
Ni, X. J. et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PloS One 9(11), e111886 (2014).
Marín Hernández, C. et al. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin. Transl. Oncol. 20(4), 476–483 (2018).
Ramirez, M. F. et al. Innate immune function after breast, lung, and colorectal cancer surgery. J. Surg. Res. 194(1), 185–193 (2015).
Höchst, B. & Diehl, L. Antigen shedding into the circulation contributes to tumor immune escape. Oncoimmunology 1(9), 1620–1622 (2012).
Gu-Trantien, C. et al. CD4+ follicular helper T cell infiltration predicts breast cancer survival. J. Clin. Invest. 123(7), 2873–2892 (2013).
Kurozumi, S. et al. Significance of evaluating tumor-infiltrating lymphocytes (TILs) and programmed cell death-ligand 1 (PD-L1) expression in breast cancer. Med. Mol. Morphol. 50(4), 185–194 (2017).
Appay, V., Douek, D. C. & Price, D. A. CD8+ T cell efficacy in vaccination and disease. Nat. Med. 14(6), 623–628 (2008).
Zacharakis, N. et al. Immune recognition of somatic mutations leading to complete durable regression in metastatic breast cancer. Nat. Med. 24(6), 724–730 (2018).
Chen, J., Hu, P., Wu, G. & Zhou, H. Antipancreatic cancer effect of DNT cells and the underlying mechanism. Pancreatology 19(1), 105–113 (2019).
Lee, J. et al. Allogeneic human double negative T cells as a novel immunotherapy for acute myeloid leukemia and its underlying mechanisms. Clin. Cancer Res. 24(2), 370–382 (2018).
Mucida, D. et al. Transcriptional reprogramming of mature CD4+ helper T cells generates distinct MHC class II-restricted cytotoxic T lymphocytes. Nat. Immunol. 14(3), 281–289 (2013).
Das, G. et al. An important regulatory role for CD4+CD8 alpha alpha T cells in the intestinal epithelial layer in the prevention of inflammatory bowel disease. Proc. Natl. Acad. Sci. U. S. A. 100(9), 5324–5329 (2003).
Van Kaer, L., Rabacal, W. A. S., Scott Algood, H. M., Parekh, V. V. & Olivares-Villagómez, D. In vitro induction of regulatory CD4+CD8α+ T cells by TGF-β, IL-7 and IFN-γ. PloS One 8(7), e67821 (2013).
Tadmor, T., Zhang, Y., Cho, H. M., Podack, E. R., Rosenblatt, J. D. The absence of B lymphocytes reduces the number and function of T-regulatory cells and enhances the anti-tumor response in a murine tumor model. Cancer Res. 60(5), 609–19 (2011).
Roberti, M. P., Mordoh, J. & Levy, E. M. Biological role of NK cells and immunotherapeutic approaches in breast cancer. Front. Immunol. 3, 375 (2012).
Wingender, G., Krebs, P., Beutler, B. & Kronenberg, M. Antigen-specific cytotoxicity by invariant NKT cells in vivo is CD95/CD178-dependent and is correlated with antigenic potency. J. Immunol. 185(5), 2721–2729 (2010).
Vahidi, Y., Faghih, Z., Talei, A. R., Doroudchi, M. & Ghaderi, A. Memory CD4+ T cell subsets in tumor draining lymph nodes of breast cancer patients: A focus on T stem cell memory cells. Cell. Oncol. Dordr. 41(1), 1–11 (2018).
Xu, T. et al. The predictive and prognostic role of stromal tumor-infiltrating lymphocytes in HER2-positive breast cancer with trastuzumab-based treatment: A meta-analysis and systematic review. J. Cancer 8(18), 3838–3848 (2017).
Balkwill, F. & Mantovani, A. Inflammation and cancer: Back to virchow?. Lancet Lond. Engl. 357(9255), 539–545 (2001).
Evani, S. J., Prabhu, R. G., Gnanaruban, V., Finol, E. A. & Ramasubramanian, A. K. Monocytes mediate metastatic breast tumor cell adhesion to endothelium under flow. FASEB J. 27(8), 3017–3029 (2013).
Jézéquel, P. et al. Validation of tumor-associated macrophage ferritin light chain as a prognostic biomarker in node-negative breast cancer tumors: A multicentric 2004 national PHRC study. Int. J. Cancer 131(2), 426–437 (2012).
Watari, K. et al. Tumor-derived interleukin-1 promotes lymphangiogenesis and lymph node metastasis through M2-type macrophages. PloS One 9(6), e99568 (2014).
Galdiero, M. R. et al. Tumor associated macrophages and neutrophils in cancer. Immunobiology 218(11), 1402–1410 (2013).
Hu, R. J., Liu, Q., Ma, J. Y., Zhou, J. & Liu, G. Preoperative lymphocyte-to-monocyte ratio predicts breast cancer outcome: A meta-analysis. Clin. Chim. Acta Int. J. Clin. Chem. 484, 1–6 (2018).
Boughey, J. C. et al. Tumor biology and response to chemotherapy impact breast cancer-specific survival in node-positive breast cancer patients treated with neoadjuvant chemotherapy: Long-term follow-up from ACOSOG Z1071 (Alliance). Ann. Surg. 266(4), 667–676 (2017).
Klein, J. et al. Locally advanced breast cancer treated with neoadjuvant chemotherapy and adjuvant radiotherapy: A retrospective cohort analysis. BMC Cancer 19(1), 306 (2019).
Lim, J. A. et al. The effect of propofol and sevoflurane on cancer cell, natural killer cell, and cytotoxic T lymphocyte function in patients undergoing breast cancer surgery: An in vitro analysis. BMC Cancer 18(1), 159 (2018).
Zitvogel, L., Apetoh, L., Ghiringhelli, F. & Kroemer, G. Immunological aspects of cancer chemotherapy. Nat. Rev. Immunol. 8(1), 59–73 (2008).
Korkaya, H., Liu, S. & Wicha, M. S. Breast cancer stem cells, cytokine networks, and the tumor microenvironment. J. Clin. Invest. 121(10), 3804–3809 (2011).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19(1), 40–50 (2018).
Ruffell, B. et al. Leukocyte composition of human breast cancer. Proc. Natl. Acad. Sci. U. S. A. 109(8), 2796–2801 (2012).
Verma, C. et al. Natural killer (NK) cell profiles in blood and tumour in women with large and locally advanced breast cancer (LLABC) and their contribution to a pathological complete response (PCR) in the tumour following neoadjuvant chemotherapy (NAC): Differential restoration of blood profiles by NAC and surgery. J. Transl. Med. 4(13), 180 (2015).
Anfray, C., Ummarino, A., Andón, F. T. & Allavena, P. Current strategies to target tumor-associated-macrophages to improve anti-tumor immune responses. Cells 9(1), 46 (2019).
Ni, X. J. et al. An elevated peripheral blood lymphocyte-to-monocyte ratio predicts favorable response and prognosis in locally advanced breast cancer following neoadjuvant chemotherapy. PloS One 9(11), e111886 (2014).
Denkert, C. et al. Ki67 levels as predictive and prognostic parameters in pretherapeutic breast cancer core biopsies: A translational investigation in the neoadjuvant GeparTrio trial. Ann. Oncol. 24(11), 2786–2793 (2013).
Wang, L. X. et al. Interleukin-7-dependent expansion and persistence of melanoma-specific T cells in lymphodepleted mice lead to tumor regression and editing. Cancer Res. 65(22), 10569–10577 (2005).
Galluzzi, L., Buqué, A., Kepp, O., Zitvogel, L. & Kroemer, G. Immunological effects of conventional chemotherapy and targeted anticancer agents. Cancer Cell 28(6), 690–714 (2015).
Janneh, O. et al. Intracellular accumulation of efavirenz and nevirapine is independent of P-glycoprotein activity in cultured CD4 T cells and primary human lymphocytes. J. Antimicrob. Chemother. 64(5), 1002–1007 (2009).
Yuan H. et al. Destructive impact of T-lymphocytes, NK and Mast cells on basal cell layers: implications for tumor invasion. BMC Cancer 13, 258 (2013).
Olkhanud, P. B. et al. Tumor-evoked regulatory B cells promote breast cancer metastasis by converting resting CD4+ T cells to T-regulatory cells. Cancer Res. 71(10), 3505–3515 (2011).
Mamessier, E. et al. Human breast cancer cells enhance self tolerance by promoting evasion from NK cell antitumor immunity. J. Clin. Invest. 121(9), 3609–3622 (2011).
Tsavaris, N., Kosmas, C., Vadiaka, M., Kanelopoulos, P. & Boulamatsis, D. Immune changes in patients with advanced breast cancer undergoing chemotherapy with taxanes. Br. J. Cancer 87(1), 21–27 (2002).
Liu, G., Chen, X. T., Zhang, H. & Chen, X. Expression analysis of cytokines IL-5, IL-6, IL-8, IL-17 and VEGF in breast cancer patients. Front. Oncol. 12, 1019247 (2022).
Liu, A. et al. A clinical nomogram based on absolute count of lymphocyte subsets for predicting overall survival in patients with non-small cell lung cancer. Int. Immunopharmacol. 114, 109391 (2023).
Li, N. et al. Prognostic and predictive significance of circulating biomarkers in patients with advanced upper gastrointestinal cancer undergoing systemic chemotherapy. Front. Oncol. 13, 1195848 (2023).
Gao, C., Tong, Y. X., Zhu, L., Dan Zeng, C. D. & Zhang, S. Short-term prognostic role of peripheral lymphocyte subsets in patients with gastric cancer. Int. Immunopharmacol. 115, 109641 (2023).
Mei, Z. et al. Tumour-infiltrating inflammation and prognosis in colorectal cancer: Systematic review and meta-analysis. Br. J. Cancer 110(6), 1595–1605 (2014).
Acknowledgements
The authors thank all the patients who participated in this study.
Funding
This study was supported by the Research Fund of the First Affiliated Hospital of Chongqing Medical University.
Author information
Authors and Affiliations
Contributions
Conceptualization: H.Z.; Data Curation: H.Z., Y.-W.L.; Formal Analysis: H.Z., Y.L., Y.-G.L.; Methodology: H.Z., Y.L., Y.-W.L., Y.-G.L.; Project Administration: H.Z., X.C.; Supervision: X.C.; Validation: H.Z., Y.L., X.C.; Visualization: H.Z., X.C.; Writing—Original Draft Preparation: H.Z.; Writing—Review and Editing: H.Z., Y.L., Y.-W.L., Y.-G.L., X.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, H., Li, Y., Liu, YW. et al. Predictive value of lymphocyte subsets and lymphocyte-to-monocyte ratio in assessing the efficacy of neoadjuvant therapy in breast cancer. Sci Rep 14, 12799 (2024). https://doi.org/10.1038/s41598-024-61632-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61632-z
- Springer Nature Limited