Abstract
The coronavirus disease (COVID-19) pandemic has significantly affected the sleep health of healthcare workers (HCWs); however, no studies have assessed this effect in primary HCWs. This cross-sectional, web-based study explored the prevalence and factors associated with sleep disorders among primary HCWs during the first COVID-19 outbreak in Shanghai from 12 July to 15 August 2022. Sociodemographic and work-related characteristics, various sleep dimensions, and exposure to patients with COVID-19 were assessed. They were screened for common mental disorders (depression, burnout, and stress). Overall, 313 primary HCWs were recruited. At least one sleep dimension in 84% of respondents deteriorated compared with that observed pre-pandemic; sleep quality (decline of 66%) and daytime sleepiness (increase of 56%) were the most affected domains. After excluding 145 primary HCWs with pre-pandemic ‘poor sleep’, depression (odds ratio [OR] 3.08; 95% confidence interval [CI] 1.59–5.98), weekly burnout symptoms (OR 2.57; 95% CI 1.32–5.03), and high psychological stress (OR 4.51; 95% CI 2.09–9.72) were associated with poor sleep patterns during the pandemic. After adjusting for significant differences between groups, for every 1-point increase in the Perceived Stress Scale score, an associated 12% increased risk of poor sleep (adjusted OR 1.12; 95% CI 1.05–1.21; p = 0.002) was observed. Most primary HCWs showed significant worsening of sleep quality, with increases in daytime sleepiness during the first wave of the COVID-19 pandemic in Shanghai. HCWs with high stress levels were at greater risks of sleep disorders.
Similar content being viewed by others
Introduction
Public health emergencies often deprive healthcare workers (HCWs) of sleep, in terms of time and quality, contributing to psychological problems such as generalised anxiety disorder and depression1. This problem may have been magnified among primary HCWs because they were responsible for the screening and diagnosis of patients with coronavirus disease (COVID-19) and providing frequent non-hospital/home care to the majority of patients with COVID-19. During the pandemic, HCWs also continued working despite the initial moments of collapse in the healthcare system2. Several primary care practitioners assumed new positions and responsibilities that eventually led to poor sleep health. A recent study reported that during the COVID-19 pandemic, < 6 h of sleep per day for general practitioners was a risk factor for an alteration in one’s mental health3. Sleep deprivation and burnout are not only linked to patient-related medical errors but also can lead to chronic depression, substance abuse, and suicide among medical professionals4,5. Notably, owing to the recurrent outbreaks of COVID-19, primary HCWs compared with other HCWs in China are being affected by sleep disorders for various reasons such as stress from the high risk of contracting the infection and transmitting it to their close contacts and changing professional obligations3. Some studies have found increased sleep disturbance and burnout rates among frontline HCWs only a few weeks after the response against COVID-19 was initiated6,7. In 2022, the COVID-19 Omicron variant caused the most severe and widespread outbreak in Shanghai since the pandemic began, causing a 3-month strict lockdown and massive COVID-19 testing and surveillance. That period was essentially Shanghai’s first wave of the pandemic. Furthermore, the impact of this pandemic in Shanghai on the sleep quality and psychological well-being of frontline primary HCWs, who are the mainstay of the fight against the epidemic, could be persistent.
To our knowledge, no study has explicitly focused on changes in the sleep patterns of primary HCWs during the epidemic period in China. Most studies have investigated the impact of pandemics on frontline staff in different roles in acute care and hospitals8,9. The duration of the COVID-19 pandemic is unknown, and primary HCWs in community hospitals are considered a significant force in the long-term response to the epidemic through their role as ‘gatekeepers’, which also means this group is the most vulnerable to sleep disorders. Identifying subgroups of primary HCWs susceptible to sleep disorders and identifying their characteristics are necessary to improve sleep quality and reduce the incidence of mental illness in this group. Good sleep may be associated with improved vaccination outcomes10. Similarly, reduced sleep, especially shorter than 7–9 h, may increase the risk of upper respiratory tract infections and related potential health outcomes such as metabolic syndrome, coronary heart disease, hypertension, diabetes, and impaired neurobehavioral performance11. In China, repeated outbreaks require primary HCWs to constantly switch roles, potentially affecting their sleep patterns and mental health. Thus, this observational cross-sectional study aimed to describe changes in multiple aspects of sleep among primary HCWs in Shanghai, China during the first wave of the COVID-19 epidemic in 2022.
Results
Survey population
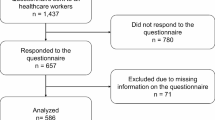
We distributed 557 questionnaires, and 375 primary HCWs (response rate of 67.3%) responded; 59 primary HCWs were excluded because they did not meet the inclusion criteria (non-Shanghai area questionnaires) and three were excluded because they answered fewer than two questions. A total of 313 qualified questionnaires were eligible for analysis.
The median age of our sample (313 respondents) was 37 years (interquartile range [IQR] 32–42 years), and the majority of our respondents were females (77.6%). The proportion of Shanghai-origin respondents was 62.3%. Over three-quarters of respondents (77.6%) were married and 67.1% were the primary caretaker for at least one child. The sample mainly included physicians (40.9%) and nurses (39.3%). Regarding job level, the majority of the respondents (91.4%) had junior and mid-level titles. Table 1 lists the roles of the primary HCWs who participated in this study. Furthermore, 262 (83.7%) survey respondents reported having two or more frontline workplaces during the pandemic. The top five job locations were enclosed communities (71.2%), outpatient clinics (55.0%), quarantine hotels (46.0%), inpatient wards (36.7%), and Fangcang shelter hospitals (8.0%, they are large-scale temporary hospitals built in public venues).
Sleep patterns before and during the outbreak
Before the pandemic, most primary HCWs experienced good (‘Often’, ‘Usually’, or ‘Always’) sleep regularity (69.3%), quality (53.4%), timing (86.6%), efficiency (53.7%), and duration (73.3%). Half (48.9%) of the respondents reported ‘often’ staying awake throughout the day. However, the proportion of respondents with regular healthy sleep patterns decreased significantly during the pandemic (p < 0.001; Fig. 1).
Figure 2 shows the proportion of respondents who reported the largest change in sleep patterns; nearly a third (32.3%) complained of sleeping later than the pre-pandemic time. Over four-fifths of primary HCWs (84.0%) showed a decline in at least one sleep dimension from the pre-pandemic levels, and over two-thirds (69.3%) showed a reduction in at least two dimensions; 16.3% of the individuals showed a decline in all six domains (Fig. 3).
‘Sleep quality’ and ‘daytime sleepiness’ had the most significant deterioration from the pre-pandemic levels. As the pandemic continued, more than half of the primary HCWs in this study (55.3%) experienced varying degrees of decline in ‘sleep quality’. The proportion of HCWs who ‘often’ had good sleep quality decreased from 53.4 to 18.2%, showing a reduction of 65.9% (p < 0.001). Before the pandemic, 51.1% of the survey respondents had already experienced chronic excessive daytime sleepiness, and this proportion reached a staggering 79.6% during the pandemic, showing an increment of 55.7% (p < 0.001). Additionally, 48.2% of the participants reported an increase in daytime sleepiness frequency during the pandemic.
After excluding 145 (46.3%) HCWs with composite sleep health score (CSHS) < 4 before the pandemic, we divided the remaining 168 HCWs into the intra-pandemic good sleep group (n = 58, 34.5%) and poor sleep group (n = 110, 65.5%) for a comparative analysis. Table 2 shows the basic information of the primary HCWs with good and poor intra-pandemic sleep behaviours. No differences were observed in sex, medical roles, and ranking levels between the groups (p > 0.05). Participants with poor intra-pandemic sleep behaviours had significantly lower CSHS than those with good sleep habits (p < 0.001). Primary HCWs with high Perceived Stress Scale (PSS) scores (p < 0.001), especially scores > 28 (odds ratio [OR] 4.51; 95% confidence interval [CI] 2.09–9.72), had a higher likelihood of developing poor sleep patterns. Furthermore, those with weekly burnout symptoms had considerably increased odds of poor sleep during the pandemic (OR 2.57; 95% CI 1.32–5.03; Table 3) After adjusting for significant differences between groups, a multivariable analysis was conducted. We found that a higher PSS score was the only factor independently associated with increased risk of poor sleep during the pandemic (adjusted odds ratio [aOR] 1.12; 95% CI 1.05–1.21).
The respondents who reported pre-pandemic insomnia (OR 2.50; 95% CI 0.89–7.03), caffeinated beverage intake ‘often’ within 12 h of bedtime (OR 2.37; 95% CI 0.96–5.84). and prolonged viewing of electronic device screens ‘often’ at night (OR 1.71; 95% CI 0.90–3.25) tended to sleep poorly, but this was not statistically significant. Furthermore, no significant statistical differences were observed in the pre-pandemic CSHS score, anxiety, depression, or sleep apnoea between those with good and poor pandemic sleep behaviours (Table 3).
Impact of the pandemic on primary HCWs’ lives and careers
The respondents’ opinions of the impact of COVID-19 are summarised in Table 4. Self-reported pandemic adjustments in job requirements were almost universal (98.4% of respondents), and challenging situations were also frequently reported (97.8%); 89.4% of respondents were assigned SARS-CoV-2 nucleic acid testing and night duties. Over two-thirds (70.3%) of respondents were concerned about closure-induced difficulties in the case of unexpected sickness and lack of access to medical care for themselves or for family.
Over a fifth (23.3%) of respondents showed positive results when screened for depression. The average PSS score was 35.4 ± 11.1, and 81.5% of respondents scored at least 29 points, which indicates moderate-to-severe stress. Additionally, about one-fifth (20.8%) of respondents ‘often’ took caffeinated beverages 12 h before bedtime, and more than half (57.2%) of the participants would frequently view electronic devices for prolonged periods at night.
Moreover, 85.7% of the respondents with children (n = 210) reported a loss of resources for childcare due to the epidemic. Over half (55.2%) of respondents changed their residence because of concerns about children or older adults being affected by COVID-19.
Contact with patients or colleagues with confirmed COVID-19 status
Over half (58.8%) of the respondents reported weekly or daily exposure to patients with COVID-19; 229 (73.2%) respondents stated that their colleagues had been diagnosed with COVID-19. A significantly higher proportion (p < 0.001) of nurses (95/123,77.2%) than physicians (84/128, 65.6%) were diagnosed with COVID-19.
Discussion
To our knowledge, this study is the first to investigate multidimensional sleep patterns in primary HCWs during the first wave of the 2022 COVID-19 pandemic in Shanghai. Other studies in China have generally focused on sleep as a secondary component of overall mental health3 or specific provider groups, such as HCWs from tertiary medical centres12, intensive care unit practitioners13, nurses14, and anaesthesiologists15. Benedict et al.5 investigated the sleep patterns of HCWs and non-HCWs using various sleep dimensions. However, sleep disturbances were more prevalent among frontline HCWs than among non-frontline and non-medical staff16. Primary HCWs play a critical role in the early identification and containment of the pandemic. Regarding overall sleep health, the frontline group should be the most considered17. According to our findings, the COVID-19 outbreak significantly influenced the sleep health (six dimensions) of primary HCWs. Sleep quality and daytime sleepiness were the most strongly affected aspects. Individuals with sleep disturbances had self-reported depression, weekly burnout symptoms, and high psychological stress (moderate-to-severe).
Our study included a larger group of primary HCWs with poor sleep habits than that in other studies18. The pre-pandemic and mid-pandemic rates of poor sleep health (46.3% and 78.6%, respectively) were considerably higher in our study than those reported in another study in the early stages of the COVID-19 outbreak in China19. The continuation of the pandemic may be having an adverse impact on the sleep health of primary HCWs. Similar to our findings, pandemic-related rates of depression20 and burnout21 among primary HCWs have been routinely reported to be more than 50%, while provider stress levels have been observed to exceed 80%.
As expected, high stress, burnout, and depression were not directly related to sex or medical roles, but they directly affected holistic sleep patterns. A possibility of the reciprocal influence of psychological factors on sleep disturbances may exist. On the one hand, the stress associated with a high risk of viral infection, perceived physical isolation, need for constant awareness of infection control protocols, and concerns about the well-being of family members may lead to depression and altered sleep patterns. On the other hand, poor sleep can result in daytime weariness, burnout, impairment of daily performance, and increased risk of crucial errors at work, all of which affect the psychological condition of HCWs22. Furthermore, a downward trend was observed in sleep-related disorders among primary HCWs in one to four sleep dimensions. In contrast, a sharp increase in such disorders was noted when more than five dimensions were involved. This phenomenon could be explained by a significant breakthrough effect when several sleep dimensions interact substantially.
Our findings contradict numerous previous conclusions that females, nurses, and frontline HCWs were the most consistently affected by COVID-193,5,18,23. We did not observe significant differences between sexes, medical roles, or levels. A potential explanation is that almost all of the primary HCWs were involved in frontline roles with an equal workload during the peak time of the outbreak. Furthermore, many appeals were made to ensure that females and nurses receive increased attention and care during the pandemic, which may have increased the workload of male primary HCWs. Our research showed that mental health (stress, burnout, and depression) had a more robust association with sleep behaviour than that observed with job role or sex. Notably, providers with a high PSS score were disproportionately affected by sleep loss, indicating that focusing on psychological ailment interventions to improve sleep patterns may be particularly fruitful.
Ongoing public health crises can have immediate and long-term effects on the sleep and mental health of frontline primary HCWs; hence, it is important to establish proactive systems to assess and monitor the psychological well-being of various professionals in primary care and provide psychological support18,24,25. Although providers experiencing psychological stress may contract COVID-1926, the addition of poor sleep health to emotional stress has been associated with reduced immunity and poor vaccine response27. One study also revealed that insufficient sleep before and during the pandemic was related to an increased risk of COVID-1928. Regrettably, studies on earlier pandemics have suggested that the mental health impact on frontline primary HCWs was long lasting. However, the duration of any effect on provider sleep patterns is uncertain, and interventions should be provided to promote sleep health since it can be modified via self-management methods and organisational and work environment adjustments18,29. Longitudinal studies are required to examine the impact of the pandemic on sleep behaviour over time and to determine the elements that can predict the occurrence of sleep disorders.
This research had several limitations. First, participation was voluntary, which may have introduced an unpredictable bias owing to the self-selection of survey respondents. The risk of bias is particularly high when the response rate is low (67.3%), although this constraint is inherent to the approach employed and has been reported in other studies based on telematic surveys30. Second, a disadvantage of the convenience sample method was that it resulted in a limited sample size; hence, the sample lacked the statistical power to allow the evaluation of data from underrepresented healthcare positions, such as logistic staff and social workers. In reality, almost all (88%) of the studies included in large-sample systematic review and 89% of the studies in another large systematic review assessing mental health or sleep disorders related to pandemics were cross-sectional and employed convenience sampling31,32 Third, the variable selection process based on univariate p-values is commonly used in the literature to determine which variables to include in a logistic regression model; however, this may lead to overfitting and increased false positive rates. The implications of this approach may have consequences on the interpretation of the results and the generalizability of the findings.
In conclusion, during the first wave of the COVID-19 outbreak in 2022 in Shanghai, primary HCWs experienced a deterioration in various sleep parameters, with self-reported ‘sleep quality’ and ‘daytime sleepiness’ being the most strongly affected domains. Self-reported depression, weekly burnout symptoms, and high psychological stress were associated with poor sleep health during the COVID-19 pandemic. Furthermore, high stress was associated with higher odds of poor sleep health among the HCWs during the onset of the COVID-19 pandemic.
Methods
Study design
This anonymous, cross-sectional survey was performed via the Tencent questionnaire website (Tencent questionnaire: http://wj.qq.com). Written informed consent was obtained from each participant before the study began. This study was approved by the Ethics Committee of Shanghai Tianlin Community Health Center (Approval No: 2022-003) and in accordance with the Declaration of Helsinki. All the data were collected without any personal identifiers. In this study, medical personnel were asked to join a WeChat group where they were briefed on the purpose, nature, and administrative procedures of the study. The members of the group accepted the invitation to complete the survey anonymously.
Sample size was calculated using the following formula: N = u × P × (1 − P)/δ2, with u = 1.96 and its associated 95% confidence interval. According to a previous study, P represents a 15% prevalence rate with a 5% expected error rate. The least sample size was calculated as N = 1.96 × 0.15 × (1–0.15)/0.052 = 100.
The survey included all primary HCWs (general practitioners, nurses, pharmacists, medical technicians, administrative staff, and logistics staff) in Shanghai community hospitals. Participants residing outside Shanghai area were excluded from the survey. Respondents who replied to fewer than two questions were disqualified. The survey questionnaire (ID: 10511743) was filled by scanning a pre-generated quick response (QR) code. The QR code was first sent by email to the person in charge of the target community hospital, who then sent it to the respondents via a mass email. The survey was opened between 12 July and 15 August 2022. No personalised invitations were made as this survey was designed to capture a target sample size, and participation was entirely voluntary.
The COVID-19 epidemic in Shanghai had been effectively controlled in the period during which the survey link was open. However, as stringent management measures continued, the workload of primary HCWs on the frontline remains heavy.
Survey content
The questionnaire contained questions on basic demographic information—survey respondents’ role, age, household location (Shanghai or non-Shanghai), sex, fertility, relationship status, and sleep patterns. The respondents also reported information on how the pandemic had changed the content and location of their jobs, children’s education in the household, and family responsibilities (see Supplementary Information 1 for details).
Referring to the study by Benedict et al.5, we used the CSHS to measure good or poor sleep patterns before and during the pandemic. The CSHS is a widely used multi‐dimensional indicator of sleep health, with higher values indicating good sleep health5,33,34,35. The CSHS, a newer assessment tool compared with the previously predominant Pittsburgh Sleep Quality Index, which mainly relies on individual subjective evaluations, may attempt to offer a more comprehensive perspective on an individual’s sleep health by incorporating both subjective reports and objective measurements. A 6-point Likert scale (1 = never; 2 = rarely; 3 = sometimes; 4 = often; 5 = usually; 6 = always) was used to quantify the frequency of sleep patterns before and during the pandemic, with higher scores indicating a higher frequency of healthy sleep patterns. The CSHS is the total sleep health score (maximum of 36 points) divided by the dimensions of the questions answered (maximum of 6). In the main survey content, the respondents were asked to report the frequency at which they exhibited sleep patterns in the following six dimensions33:
-
Sleep regularity: ‘How often do you have a regular sleep time rhythm? (go to bed at the same time of night and wake up at the same time of the morning)’
-
Sleep quality: ‘How often do you wake up refreshed?’
-
Sleepiness: ‘How often do you stay awake throughout the day without nodding off or dozing off?’
-
Sleep timing: ‘How often do you go to bed after midnight?’
-
Sleep efficiency: ‘How often do you fall asleep within 30 min from the time you prepare to sleep (including falling back to sleep after short periods of being awake in the night)?’
-
Sleep duration: ‘How often do you get 6–8 h of sleep per day?’
A score of 4 (i.e. ‘often’ for self-reported healthy sleep in all dimensions) was used as a cut-off point for ‘good’ and ‘poor’ sleep. To identify HCWs whose sleep were most affected by the pandemic, we excluded those who were ‘poor sleepers’ (with a CSHS of less than 4) before the pandemic and conducted a secondary analysis. The CSHS is more concise than other sleep scores, and its validity has been demonstrated in other population-based studies34,35,36,37.
In addition, an abbreviated version of the Maslach Burnout Scale38 was used to assess burnout. We purchased the Maslach Burnout Inventory license before administering the instrument via the MindGarden (http://www.mindgarden.com) webpage. The 14-item PSS39 and 2-item patient health questionnaire40 were used to evaluate stress and depression, respectively. A PSS score of more than 28 indicates moderate-to-severe stress39. Other factors affecting sleep frequency (e.g., time spent in front of a mobile phone screen, drinking alcohol, or consuming caffeine or smoking before bedtime) were also investigated. Finally, the respondents were asked about occupational exposure to COVID-19 and infection. All questions were not compulsory.
Statistical analysis
Appropriate central tendency and dispersion measures or counts and percentages for categorical data were used to summarise the data. As this was an anonymous survey, replies were reviewed for plausibility, but data reliability could not be guaranteed. Mann–Whitney U or Kruskal–Wallis tests were used to compare continuous non-parametric data among categorical variables. Paired t-tests were used to compare parametric data from several time points for each participant. Categorical variables within groups were compared using chi-squared tests, whereas paired proportions were compared using McNemar chi-squared test. Parameters with p-values < 0.1 in the univariate analyses were included in the logistic regression. p-values < 0.05 were considered statistically significant. All statistical analyses were conducted using R 3.6.3 and Python 3.7.
Data availability
Due to the nature of this study, participants in this study did not agree to share their data publicly and therefore supporting data could not be provided. If anyone would like to obtain data from this study, please contact the corresponding author.
References
Benahmed, A. G., Gasmi, A., Anzar, W., Arshad, M. & Bjørklund, G. Improving safety in dental practices during the COVID-19 pandemic. Health Technol. (Berl.) 12, 205–214 (2022).
Taş, B. G., Özceylan, G., Öztürk, G. Z. & Toprak, D. Evaluation of job strain of family physicians in COVID-19 pandemic period—An example from Turkey. J. Community Health 46, 777–785 (2021).
Zhang, J., Song, S., Zhang, M. & Wang, R. Influencing factors for mental health of general practitioners in Hebei Province under the outbreak of COVID-19: A cross-sectional study. Int. J. Clin. Pract. 75, e14783 (2021).
Irshad, K., Ashraf, I., Azam, F. & Shaheen, A. Burnout prevalence and associated factors in medical students in integrated modular curriculum: A cross-sectional study. Pak. J. Med. Sci. 38, 801–806 (2022).
Benedict, C., Partinen, M., Bjorvatn, B. & Cedernaes, J. Sleep in female healthcare workers during COVID-19: A cross-sectional survey study in Sweden during the flattening of the first wave of the pandemic. Ann. Am. Thorac. Soc. 18, 1418–1420 (2021).
Wang, S. et al. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. (Lond.) 70, 364–369 (2020).
Rossi, R. et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open 3, e2010185 (2020).
Tasdemir Yigitoglu, G., Yilmaz, A. & Yilmaz, H. The effect of Covid-19 on sleep quality, anxiety and depression on healthcare staff at a tertiary hospital in Turkey. Arch. Psychiatr. Nurs. 35, 504–510 (2021).
Serrano-Ripoll, M. J., Zamanillo-Campos, R., Castro, A., Fiol-de Roque, M. A. & Ricci-Cabello, I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: A systematic review of the literature and meta-analysis. Actas Esp. Psiquiatr. 49, 155–179 (2021).
Prather, A. A., Pressman, S. D., Miller, G. E. & Cohen, S. Temporal links between self-reported sleep and antibody responses to the influenza vaccine. Int. J. Behav. Med. 28, 151–158 (2021).
Robinson, C. H. et al. The relationship between duration and quality of sleep and upper respiratory tract infections: A systematic review. Fam. Pract. 38, 802–810 (2021).
Chen, H. et al. Psychotherapy and follow-up in health care workers after the COVID-19 epidemic: A single center’s experience. Psychol. Res. Behav. Manag. 15, 2245–2258 (2022).
Zhang, Y., Pi, D. D., Liu, C. J., Li, J. & Xu, F. Psychological impact of the COVID-19 epidemic among healthcare workers in paediatric intensive care units in China. PLoS One 17, e0265377 (2022).
Han, J. et al. Effect of a group-based acceptance and commitment therapy programme on the mental health of clinical nurses during the COVID-19 sporadic outbreak period. J. Nurs. Manag. 30, 3005–3012 (2022).
Guo, F. et al. Psychological distress was still serious among anesthesiologists under the post COVID-19 era. Psychol. Res. Behav. Manag. 15, 777–784 (2022).
Wang, W. et al. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Front. Psychiatry 11, 733 (2020).
Xu, Z. et al. Primary care practitioners’ barriers to and experience of COVID-19 epidemic control in China: A qualitative study. J. Gen. Intern. Med. 35, 3278–3284 (2020).
Aragonès, E. et al. Psychological impact of the COVID-19 pandemic on primary care workers: A cross-sectional study. Br. J. Gen. Pract. 72, e501–e510 (2022).
Qi, J. et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 72, 1–4 (2020).
Shi, L. S., Xu, R. H., Xia, Y., Chen, D. X. & Wang, D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: The mediating effects of social support and resilience. Front. Psychol. 12, 800183 (2021).
Sullivan, E. E., Dwiel, K., Hunt, L. S., Conroy, K. & Gergen Barnett, K. Moving the needle on primary care burnout: Using a driver diagram to accelerate impact. Healthc. (Amst). 9, 100595 (2021).
Lin, Y. N. et al. Burden of sleep disturbance during COVID-19 pandemic: A systematic review. Nat. Sci. Sleep 13, 933–966 (2021).
Song, Y., Yang, F., Sznajder, K. & Yang, X. Sleep quality as a mediator in the relationship between perceived stress and job burnout among Chinese nurses: A structural equation modeling analysis. Front. Psychiatry 11, 566196 (2020).
Zhao, Y. et al. COVID19: A systematic approach to early identification and healthcare worker protection. Front. Public Health 8, 205 (2020).
Nagesh, S. & Chakraborty, S. Saving the frontline health workforce amidst the COVID-19 crisis: Challenges and recommendations. J. Glob. Health 10, 010345 (2020).
Elbay, R. Y., Kurtulmuş, A., Arpacıoğlu, S. & Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 290, 113130 (2020).
SenGupta, S. et al. Clocks, viruses, and immunity: Lessons for the COVID-19 pandemic. J. Biol. Rhythms 36, 23–34 (2021).
Kim, H. et al. COVID-19 illness in relation to sleep and burnout. BMJ Nutr. Prev. Health 4, 132–139 (2021).
Serafin, L. I., Fukowska, M., Zyskowska, D., Olechowska, J. & Czarkowska-Pączek, B. Impact of stress and coping strategies on insomnia among Polish novice nurses who are employed in their field while continuing their education: A cross-sectional study. BMJ Open 11, e049787 (2021).
Cunningham, C. T. et al. Exploring physician specialist response rates to web-based surveys. BMC Med. Res. Methodol. 15, 32 (2015).
Moitra, M. et al. Mental health consequences for healthcare workers during the COVID-19 pandemic: A scoping review to draw lessons for LMICs. Front. Psychiatry 12, 602614 (2021).
Wu, T. et al. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 281, 91–98 (2021).
Buysse, D. J. Sleep health: Can we define it? Does it matter?. Sleep 37, 9–17 (2014).
Gutierrez-Colina, A. M. et al. A preliminary investigation of sleep quality and patient-reported outcomes in pediatric solid organ transplant candidates. Pediatr. Transplant. 23, e13348 (2019).
Brandolim Becker, N., Martins, R. I. S., Jesus, S. N., Chiodelli, R. & Stephen Rieber, M. Sleep health assessment: A scale validation. Psychiatry Res. 259, 51–55 (2018).
Pavlova, M., Ference, J., Hancock, M. & Noel, M. Disentangling the sleep-pain relationship in pediatric chronic pain: The mediating role of internalizing mental health symptoms. Pain Res. Manag. 2017, 1586921 (2017).
Moreau, D., Kirk, I. J. & Waldie, K. E. High-intensity training enhances executive function in children in a randomized, placebo-controlled trial. eLife 6, e25062 (2017).
West, C. P., Dyrbye, L. N., Satele, D. V., Sloan, J. A. & Shanafelt, T. D. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J. Gen. Intern. Med. 27, 1445–1452 (2012).
Katsarou, A. et al. Validation of a Greek version of PSS-14; a global measure of perceived stress. Cent. Eur. J. Public Health 20, 104–109 (2012).
Qiu, D. et al. Job dissatisfaction mediated the associations between work stress and mental health problems. Front. Psychiatry 12, 711263 (2021).
Author information
Authors and Affiliations
Contributions
All authors agree to the submission of this manuscript. W.C. and X.L. drafted the manuscript; Q.L. designed the research; W.C., X.L., Y.Y., and J.Z. carried out the research procedures; Y.Y. and J.Y. analyzed the data; and J.Y. and Q.L. contributed to data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cao, W., Li, X., Yan, Y. et al. Changes in sleep patterns in primary care workers during the first wave of the COVID-19 pandemic in 2022 in Shanghai: a cross-sectional study. Sci Rep 14, 12373 (2024). https://doi.org/10.1038/s41598-024-61311-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61311-z
- Springer Nature Limited