Abstract
This study investigated long COVID of patients in the Montefiore Health System COVID-19 (CORE) Clinics in the Bronx with an emphasis on identifying health related social needs (HRSNs). We analyzed a cohort of 643 CORE patients (6/26/2020–2/24/2023) and 52,089 non-CORE COVID-19 patients. Outcomes included symptoms, physical, emotional, and cognitive function test scores obtained at least three months post-infection. Socioeconomic variables included median incomes, insurance status, and HRSNs. The CORE cohort was older age (53.38 ± 14.50 vs. 45.91 ± 23.79 years old, p < 0.001), more female (72.47% vs. 56.86%, p < 0.001), had higher prevalence of hypertension (45.88% vs. 23.28%, p < 0.001), diabetes (22.86% vs. 13.83%, p < 0.001), COPD (7.15% vs. 2.28%, p < 0.001), asthma (25.51% vs. 12.66%, p < 0.001), lower incomes (53.81% vs. 43.67%, 1st quintile, p < 0.001), and more unmet social needs (29.81% vs. 18.49%, p < 0.001) compared to non-CORE COVID-19 survivors. CORE patients reported a wide range of severe long-COVID symptoms. CORE patients with unmet HRSNs experienced more severe symptoms, worse ESAS-r scores (tiredness, wellbeing, shortness of breath, and pain), PHQ-9 scores (12.5 (6, 17.75) vs. 7 (2, 12), p < 0.001), and GAD-7 scores (8.5 (3, 15) vs. 4 (0, 9), p < 0.001) compared to CORE patients without. Patients with unmet HRSNs experienced worse long-COVID outcomes compared to those without.
Similar content being viewed by others
Introduction
Post-acute sequelae of SARS-CoV-2 infection (PASC), also referred to as long COVID, has emerged as a significant public health concern in part because of the sheer number of individuals infected by SARS-CoV-21,2,3,4. PASC includes, but are not limited to, anxiety, depression, post-traumatic stress disorder, and other neurological, psychiatric, and cognitive symptoms5,6,7,8.
COVID-19 has disproportionately affected marginalized communities, amplifying the inequalities they face in accessing healthcare, resources, and socioeconomic stability9,10. Factors such as limited access to quality healthcare, higher rates of underlying health conditions, overcrowded living conditions, and employment in essential but higher-risk jobs have all contributed to the heightened impact of COVID-19 on vulnerable populations11,12. A few studies have shown that patients with lower socioeconomic status or unmet health related social needs (HRSNs) are more likely to be infected by SARS-CoV-2 and have worse acute clinical outcomes13,14,15,16,17,18. These vulnerable populations are also at higher risk of developing long COVID but are less studied19. Common HRSNs include food and housing, utilities, out of pocket healthcare costs, child/adult care, and healthcare transportation. Examining the relationship between HRSNs and PASC could shed light on the likely challenges faced by this population and could help to address the nuanced needs of individuals experiencing prolonged health consequences post-COVID infection20.
The Bronx in New York City was hit hard by the first wave of COVID-19 and by multiple subsequent surges of infection from different variants21. Montefiore Health System is the largest health care provider in Bronx County, serving a diverse patient population, including many patients with low socioeconomic status. In June 2020, Montefiore Medical Center established two COVID-19 Recovery and Engagement (CORE) Clinics for COVID-19 survivors with protracted symptoms. A detailed evaluation protocol was implemented to assess physical, emotional, and function across the neurological and psychiatric domains for patients suspected to have long COVID.
In this paper, we reported long-COVID symptoms, physical, emotional, and cognitive function of CORE patients from June 26th, 2020 and February 24th, 2023. Outcomes were interpreted with emphasis on their relationship with socioeconomic data which included median incomes, insurance status, and HSRNs. The objective of this study was to identify the prevalence of HSRNs as a risk factor for long COVID symptoms incidence and severity in a diverse and underserved population of CORE patients.
Methods
Data sources
This study was approved by the Einstein IRB (IRB# 2021–13658) with a waiver of informed consent. The Montefiore Health System included a large number of hospitals and outpatient clinics in the Bronx and surrounding towns. This is a retrospective observational cohort study of COVID-19 adult patients with protracted symptoms who were referred to our COVID-19 Recovery and Engagement (CORE) clinics. Eligible patients were at least 18 years of age who had probable or confirmed COVID-19 infection and were experiencing new or continued symptoms greater than 4 weeks after initial infection. Patients who came to the CORE clinics included both patients who were hospitalized and not hospitalized for COVID-19. CORE patients could come from anywhere and could be referred to by any health provider. The CORE clinics were also advertised in the local communities. There were 643 patients who came to the CORE clinics for COVID-19 related medical issues between June 26th, 2020 and February 24th, 2023.
As an aside, brief comparisons of patient profiles were also made for all COVID-positive (COVID +) cohort which consisted of 52,089 Montefiore patients who returned alive three months after initial COVID + diagnosis date over the same period. The date of the first positive reverse transcription polymerase chain reaction (RT-PCR) was extracted as the date of COVID-19 diagnosis. For CORE patients without positive RT-PCR results in their chart, the date of COVID-19 infection is recorded by CORE physicians in the doctor’s note and collected via chart review.
Data abstraction
De-identified health data were obtained for research after standardization to the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) version 6. OMOP CDM represents healthcare data from diverse sources, which are stored in standard vocabulary concepts19, allowing for the systematic analysis of disparate observational databases, including data from the electronic medical record (EMR), administrative claims, and disease classifications systems (e.g., ICD-10, SNOWMED, LOINC, etc.). ATLAS, a web-based tool developed by the Observational Health Data Sciences and Informatics (OHDSI) community that enables navigation of patient-level, observational data in the CDM format, was used to search vocabulary concepts and facilitate cohort building. Data were subsequently exported and queried as SQLite database files using the DB Browser for SQLite (version 3.12.0). To ensure data accuracy, our team performed extensive cross validation of all major variables extracted by manual chart reviews on subsets of patients13,14,15,16,17,18.
Demographics and comorbidities
Age, sex, BMI, combined race ethnicity, median household income quintile, and insurance status were extracted from patient EMR. Age and BMI at the time of or closest to COVID-19 diagnosis were recorded. Income data was obtained by matching patient’s zip code to median household income as reported by the census, and then assigning quintiles based on the cohorts’ combined incomes. Preexisting comorbidities included hypertension, chronic obstructive pulmonary disease (COPD), asthma, diabetes mellitus, congestive heart failure (CHF), and chronic kidney disease (CKD) that were designated by ICD10 codes at admission or prior.
This retrospective study was approved by the Einstein-Montefiore Institutional Review Board (#2021–13658). This study has an exemption for informed consent and a HIPAA waiver and was performed in accordance with relevant guidelines and regulations.
COVID-19 disease severity
COVID-19 disease severity was categorized into non-hospitalized, hospitalized (general floor), and hospitalized (critically ill). All hospitalized patients admitted to the intensive care unit (ICU) or placed on invasive mechanical ventilation (IMV) were considered critically ill.
Vaccination status
The vaccination status of CORE patients at the time of COVID-19 infection was recorded by CORE physicians in the doctor’s note and collected via chart review. Vaccination status could not be collected for COVID + patients given the inconsistent coding in Epic and large sample size requiring chart review.
Health related social needs
The majority of CORE patients completed the Montefiore-Einstein Social Determinants of Health Screen, which is a standardized instrument developed by Health Leads Toolkit (https://healthleadsusa.org/) and adapted by Montefiore-Einstein’s Office of Community and Population Health in 2018. This screening tool is provided during routine clinical visits across the health system and is integrated into the EHR. The responses were not required (it was voluntary). The screener asks about the following social need categories: housing, food insecurity, utilities, health transportation, medications, child or elderly care, legal services, family stress and safety22. The number of responses to date is about 250,000.
Long COVID physical symptom questionnaires
All CORE patients were surveyed for the presence of various post-infection symptoms, labeled as “Symptoms Present at 1st Core Visit.” CORE patients additionally completed a revised Edmonton Symptom Assessment System (ESAS-r) where they scored various symptoms from 0 (no symptoms or best overall wellbeing) to 10 (the worst level of symptom imaginable or worst overall wellbeing). The median, first quartile (Q1), and third quartile (Q3) of each ESAS-r symptom severity was calculated.
Long COVID behavioral symptom questionnaire
CORE patients were assessed for depression and anxiety using the Patient Health Questionnaire (PHQ-9) Questionnaire and Generalized Anxiety Disorder (GAD-7) Questionnaire, respectively. Questionnaire results were reported as median (Q1, Q3), in addition to incidence of various respective provisional diagnosis categories.
Statistical analysis
Analysis was performed by comparing CORE patients with all other COVID-19 patients. Analysis was also performed between patients with and without unmet social needs. Analysis of group differences employed χ2 tests for categorical variables and unpaired t-tests for continuous variables via the statistical libraries in SPSS and RStudio, respectively. Mann–Whitney U tests were performed for median comparisons. When comparing differences of categorical variables across three groups, χ2 tests were used to identify group differences and ad hoc pairwise tests were used to identify the specific pairwise group difference. Statistics were not adjusted for multiple comparison and no variables were controlled for due to the exploratory nature of the study. P < 0.05 was considered statistically significant.
Results
Figure 1 displays a histogram of date of COVID-19 infection and 1st CORE visit. Relatively more CORE patients were infected earlier in the pandemic compared to later in the pandemic. More CORE patients visited early in the pandemic compared to later in the pandemic.
Table 1 shows the demographic, disease severity, and socioeconomic profiles of CORE patients. The average age was 53.38 ± 14.50, majority female (72.47%), Hispanic (46.50%), unvaccinated (83.67%), and with a median household income quintile less than $55,275.80 (53.81%).
As an aside, we compared CORE patient profiles only with all COVID + patient profiles (Supplemental Table 1). Compared to the all COVID + cohort, CORE patients were older (53.38 ± 14.50 versus (vs.) 45.91 ± 23.79 years old, p < 0.001), had higher BMI (31.80 ± 7.64 vs. 28.34 ± 7.70, p < 0.001), and more likely to be female (72.74% vs. 56.86%, p < 0.001). Except for White, not Hispanic (9.64% vs. 12.42%, p = 0.033) and Hispanic (46.50% vs. 39.84%, p = 0.001), there were no statistically significant differences in combined race and ethnicity (p > 0.05) between the two groups. With respect to comorbidities, CORE patients had higher proportions of hypertension (45.88% vs. 23.28%, p < 0.001), COPD (7.15% vs. 2.28%, p < 0.001), asthma (25.51% vs. 12.66%, p < 0.001), and diabetes mellitus (22.86% vs. 13.83%, p < 0.001), but no statistically significant difference in CHF or CKD (p > 0.05). CORE patients had slightly decreased hospitalization (general floor) rates (22.86% vs. 23.86%, p < 0.001), but no difference in critical illness (p > 0.05). CORE patients were also primarily unvaccinated at the time of COVID-19 infection (83.67%).
With respect to socioeconomic data, CORE patients had higher proportions of 1st (lowest) quintile median household income as compared to the COVID + cohort (53.81% vs. 43.67%, p < 0.001). Additionally, CORE patients were more likely to have private insurance (32.97% vs. 26.19%, p < 0.001) or care management organization (11.98% vs. 3.97%, p < 0.001), but also less likely to use Medicaid (31.73% vs. 41.01%, p < 0.001) and Medicare (14.93% vs. 19.51%, p = 0.004). Overall, there were significantly more CORE patients with unmet social needs (29.62% vs. 18.49%, p < 0.001).
Supplemental Fig. 1 presents the HRSN questionnaire results for CORE versus COVID + groups broken down by individual unmet need. CORE patients had statistically significant greater incidence of concerns about housing quality (11.96% vs. 5.57%, p < 0.001), housing situation (11.14% vs. 5.02%, p < 0.001), money for food (8.97% vs. 5.86%, p = 0.046), utilities shut threat (5.98% vs. 3.21%, p = 0.012), and legal help (5.43% vs. 2.77%, p = 0.008) as compared to the COVID + group.
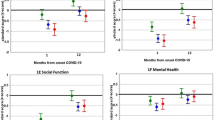
The results of the long COVID physical symptom and behavioral questionnaires for CORE patients are shown in Table 2. The most common symptoms were dyspnea (47.43%), fatigue (39.04%), decreased exercise tolerance (27.84%), and brain fog/cognitive issues (27.53%). According to the ESAS-r Questionnaire, the most severe symptoms were tiredness (median 6; IQR (3, 8)), worsened overall wellbeing (5 (1.25, 7)), and shortness of breath (4 (0, 7)). On average, PHQ-9 and GAD-7 questionnaires showed CORE patients experienced mild depression (8 (3, 14)) and no or little anxiety (4 (1, 10)).
CORE patients were broken down by disease severity into non-hospitalized (N = 446), general floor (N = 147), and critically ill (N = 50). Across disease severity groups, higher incidence of dyspnea, fatigue, decreased exercise tolerance, and cough incidence were associated with higher disease severity. Incidence of normal or minimal depression and anxiety both increased as disease severity worsened.
The demographic, disease severity, and socioeconomic profiles of CORE patients without and with unmet HRSNs are presented in Table 3. There were no statistically significant differences in age, female sex composition, BMI, combined race and ethnicity, or comorbidities (all p > 0.05). Disease severity and vaccination status was also not significantly different between groups (p > 0.05). Patients with unmet needs had lower incidence of 5th quintile median household income (0.91% vs. 5.79%, p = 0.035) and higher Medicaid use (43.64% vs. 26.64%, p = 0.001) compared to patients without unmet needs.
Table 4 compares the long COVID physical symptoms and behavioral questionnaires stratified by patients without and with social needs. Only brain fog/cognitive issues were higher in patients with unmet needs (42.73% vs. 32.05%, p = 0.049) compared to patients without 0 unmet needs. In the ESAS-r responses, patients with unmet needs did experience more severe symptoms compared to patients without unmet needs, with the top five severe ones being tiredness (7 (4.25, 8) vs. 5 (0,7), p = 0.002), worsened overall wellbeing (5 (4, 7) vs. 4 (1, 6), p < 0.001), shortness of breath (5 (1, 7) vs. 3 (0, 6), p = 0.025), pain (5 (2, 7) vs. 3 (0, 6), p < 0.001), and anxiety (5 (1, 8) vs. 2 (0, 5), p < 0.001). Patients with unmet needs additionally experienced worsened depression (12.5 (6, 17.75) vs. 7 (2, 12), p < 0.001) and anxiety (8.5 (3, 15) vs. 4 (0, 0), p < 0.001) as compared to patients without unmet needs according to the PHQ-9 and GAD-7, respectively. CORE patients with unmet needs had increased rates of clinically severe depression (15.60% vs. 5.93%, p = 0.003) and severe anxiety disorder (28.44% vs. 8.39%, p < 0.001).
Discussion
This study investigated the patient characteristics and prevalence of long COVID symptoms in our CORE clinics between June 26th, 2020 and February 24th, 2023 with emphasis on the potential influence of unmet HRSNs. The major findings are: (i) most CORE patients are infected during the early waves of COVID-19 and were largely unvaccinated, (ii) COVID-19 survivors report a wide range of severe long-COVID symptoms across the physical, emotional, and cognitive health domains, (iii) some COVID-related symptoms (i.e., dyspnea, fatigue, decreased exercise tolerance, and cough) show higher incidence among more severe COVID-19 patients but these symptoms were not limited to hospitalized or critically ill patients, and (iv) patients with unmet HRSNs have similar demographics (except lower percentage of high income bracket and higher percentage with Medicaid), but experience similar rates of physical and psychological long-COVID symptoms compared to patients without unmet HRSNs, but with greater severity of symptoms.
More CORE patients were infected during the early waves. These peak infection periods matched the reported SARS-CoV-2 infection spikes in New York metropolitan areas23. Vaccination and treatments were limited during the earlier waves of the pandemic and thus it is likely that these patients infected in earlier waves experienced more severe disease courses24,25,26. Our data indicated that most CORE patients were in fact unvaccinated at the time of infection. Patients infected in later waves likely had less severe disease course and long-term outcomes as vaccines and COVID-19 treatments became more available.
The high incidences of dyspnea, fatigue, brain fog, decreased exercise tolerance, and shortness of breath reported in this study are consistent with the literature27,28. Goertz et al.29 found that fatigue, dyspnea, headache, and chest tightness were the four most common persistent symptoms 3-months after infection. Huang et al.30 reported that fatigue or muscle weakness was by far the most common symptom hospitalized COVID-19 patients at 6-months followed up. Carfi et al.31 found fatigue, dyspnea, and joint pains to be the three most prevalent symptoms in COVID survivors about 2 months after their COVID-19 hospitalization. These symptomologies are not surprising given many COVID-19 patients were often discharged with major medical referrals32,33. The incidence of dyspnea, fatigue, decreased exercise tolerance, and cough increased as disease severity worsened, in agreement with other papers34,35,36.
Additionally, CORE patients broadly showed signs of mild anxiety and mild depression. Surprisingly, the severity of anxiety and depression was inversely correlated to COVID-19 disease severity. Other studies have similarly found that after COVID-19 infection, a significant number of patients self-reported anxiety and depression37,38. One study found that most COVID-19 survivors had mild depression, specifically using the PHQ-9 questionnaire, in agreement with our study. As anxiety and depression are known risk factors for developing PASC39, it is concerning that the majority of CORE patients screened positive for clinically significant anxiety and depression.
Some, but not all, CORE patients showed more long-COVID symptoms and abnormal physical, emotional, and cognitive scores. More severe COVID-19, as measured by hospitalization in the general floor or ICU/IMV interventions, showed higher incidence of long COVID symptoms compared to the non-hospitalized cohort. It is striking that many non-hospitalized patients had substantial symptoms and abnormal scores. Although non-hospitalized patients who visited our CORE clinics were more likely to exhibit symptoms given the nature of their visit, these data suggested that long COVID is not limited to severely ill COVID-19 patients. A recent prospective study demonstrates similar findings, in which patients with high respiratory symptomatic burden 3-months post-COVID were associated with high disease severity40. Previous studies have reported individuals with mild symptoms from SARS-CoV-2 infection (i.e., not requiring hospitalization) or asymptomatic infection may also be susceptible to general and neurological PASC41,42,43.
CORE patients with and without unmet HRSNs had similar baseline demographics, comorbidities, and disease severity in our cohort, except patients with unmet social needs had lower proportion of 5th quintile income and more were on Medicaid as expected. However, the incidence of severe depression and anxiety was nearly tripled in patients with unmet HRSNs as compared to patients without. Patients with unmet HRSNs also experienced more severe long COVID symptoms compared to those without.
It is likely that the persistent stress associated with these unmet needs is increasingly understood as a pivotal factor, amplifying the susceptibility to and severity of long-term consequences from COVID-19. It is well known that sustained, chronic stress has several deleterious effects on normal physiology. It sets off a chain reaction within the body, sparking inflammatory responses and prompting intricate alterations in gene expression, known as epigenetic modifications44. These modifications, in turn, have the potential to significantly impact health outcomes, potentially worsening the long-term effects of COVID-19.
Moreover, persistent structural barriers in accessing quality health care services, particularly preventative care, places vulnerable populations at a distinct disadvantage. The higher prevalence of pre-existing health conditions among marginalized groups, often due to systemic inequalities, acts as a significant contributor to the severity of long COVID outcomes. The cumulative effect of these intersecting factors serves to magnify the disproportionate toll that COVID-19 exacts on historically marginalized populations, highlighting the urgent need for targeted interventions addressing these underlying socioeconomic disparities.
This study has several limitations. Our findings were limited to COVID-19 survivors who came to our CORE clinics and who were more likely to have more severe COVID-19 symptoms, and thus our cohort was not representative of the general population. Findings also rely on the assumption that COVID-19 controls did not seek medical care outside of the Montefiore system for long-COVID symptoms, as this data would not be available. Multicenter and prospective studies are needed to validate these findings and achieve broader generalization. It was not possible to definitively distinguish abnormalities that were due to COVID-19, pre-existing or worsened by COVID-19 disease. SDOH data were only available for a subset of patients because these questionnaires were incorporated in 201845 with the administration and responses being encouraged but voluntary. Long-term outcomes may have been affected by vaccination status and reinfection. Long COVID-19 is time dependent post infection46,47,48,49. It is possible that symptom score related to long-COVID is dependent the duration of time post infection. A previous work has identified no change in clinical variables at 3–6 months follow-up50.
Conclusions
COVID-19 patients have a wide range of severe long COVID symptoms across the physical, emotional, and cognitive health domains, and these symptoms are not limited to patients who were hospitalized or critically ill. Patients with unmet social needs are more likely to experience exacerbated long COVID outcomes, furthering the widening health disparity. These findings call attention to the impacts of health disparity on socioeconomically vulnerable patients with long COVID. This pandemic has underscored the urgent need to address systemic issues and work towards equitable healthcare and support systems for all.
Data availability
The data used in this study are available upon request to the corresponding author.
References
Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 38, 101019. https://doi.org/10.1016/j.eclinm.2021.101019 (2021).
Rubin, R. As their numbers grow, COVID-19 “Long Haulers” stump experts. JAMA 324, 1381–1383. https://doi.org/10.1001/jama.2020.17709 (2020).
Zhao, Y. M. et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery. EClinicalMedicine 25, 100463. https://doi.org/10.1016/j.eclinm.2020.100463 (2020).
Iosifescu, A. L., Hoogenboom, W. S., Buczek, A. J., Fleysher, R. & Duong, T. Q. New-onset and persistent neurological and psychiatric sequelae of COVID-19 compared to influenza: A retrospective cohort study in a large New York City healthcare network. Int. J. Methods Psychiatr. Res. 31, e1914. https://doi.org/10.1002/mpr.1914 (2022).
Moghimi, N. et al. The neurological manifestations of post-acute sequelae of SARS-CoV-2 infection. Curr. Neurol. Neurosci. Rep. 21, 44. https://doi.org/10.1007/s11910-021-01130-1 (2021).
Collantes, M. E. V., Espiritu, A. I., Sy, M. C. C., Anlacan, V. M. M. & Jamora, R. D. G. Neurological manifestations in COVID-19 infection: A systematic review and meta-analysis. Can. J. Neurol. Sci. 48, 66–76. https://doi.org/10.1017/cjn.2020.146 (2021).
Graham, E. L. et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers”. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.51350 (2021).
Wang, F., Kream, R. M. & Stefano, G. B. Long-term respiratory and neurological sequelae of COVID-19. Med. Sci. Monit. 26, e928996. https://doi.org/10.12659/MSM.928996 (2020).
Bambra, C., Riordan, R., Ford, J. & Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Commun. Health 74, 964–968. https://doi.org/10.1136/jech-2020-214401 (2020).
Ambrose, A. J. H. Inequities during COVID-19. Pediatrics https://doi.org/10.1542/peds.2020-1501 (2020).
Abrams, E. M. & Szefler, S. J. COVID-19 and the impact of social determinants of health. Lancet Respir. Med. 8, 659–661. https://doi.org/10.1016/S2213-2600(20)30234-4 (2020).
Singu, S., Acharya, A., Challagundla, K. & Byrareddy, S. N. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front Public Health https://doi.org/10.3389/fpubh.2020.00406 (2020).
Green, H., Fernandez, R. & MacPhail, C. The social determinants of health and health outcomes among adults during the COVID-19 pandemic: A systematic review. Public Health Nurs. 38, 942–952. https://doi.org/10.1111/phn.12959 (2021).
Acosta, A. M. et al. Racial and ethnic disparities in rates of COVID-19-associated hospitalization, intensive care unit admission, and in-hospital death in the United States from march 2020 to february 2021. JAMA Netw. Open 4, e2130479. https://doi.org/10.1001/jamanetworkopen.2021.30479 (2021).
Correa-Agudelo, E. et al. Identification of vulnerable populations and areas at higher risk of COVID-19 related mortality in the U.S. medRxiv, doi:https://doi.org/10.1101/2020.07.11.20151563 (2020).
Magesh, S. et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: A systematic-review and meta-analysis. JAMA Netw. Open 4, e2134147. https://doi.org/10.1001/jamanetworkopen.2021.34147 (2021).
Kanwal, A. et al. The effect of race and socioeconomic status on hospitalized patients with COVID-19 infection. J. Commun. Hosp. Intern. Med. Perspect. 12, 14–19. https://doi.org/10.55729/2000-9666.1035 (2022).
Saltzman, L. Y., Lesen, A. E., Henry, V., Hansel, T. C. & Bordnick, P. S. COVID-19 mental health disparities. Health Secur. 19, S5-s13. https://doi.org/10.1089/hs.2021.0017 (2021).
Subramanian, A. et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 28, 1706–1714. https://doi.org/10.1038/s41591-022-01909-w (2022).
Brakefield, W. S., Olusanya, O. A., White, B. & Shaban-Nejad, A. Social determinants and indicators of COVID-19 among marginalized communities: A scientific review and call to action for pandemic response and recovery. Disaster Med. Public Health Prep. 17, e193. https://doi.org/10.1017/dmp.2022.104 (2022).
Hoogenboom, W. S. et al. Clinical characteristics of the first and second COVID-19 waves in the Bronx, New York: A retrospective cohort study. Lancet Reg. Health Am. 3, 100041. https://doi.org/10.1016/j.lana.2021.100041 (2021).
Fiori, K. P. et al. Scaling-up social needs screening in practice: a retrospective, cross-sectional analysis of data from electronic health records from Bronx county, New York, USA. BMJ Open 11, e053633. https://doi.org/10.1136/bmjopen-2021-053633 (2021).
COVID-19 Data: Trends and Totals, <https://www.nyc.gov/site/doh/covid/covid-19-data-totals.page> (2023).
Hoogenboom, W. S. et al. Clinical characteristics of the first and second COVID-19 waves in the Bronx, New York: A retrospective cohort study. Lancet Reg. Health Am. 3, 100041. https://doi.org/10.1016/j.lana.2021.100041 (2021).
Feikin, D. R. et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: results of a systematic review and meta-regression. Lancet 399(10328), 924–944. https://doi.org/10.1016/S0140-6736(22)00152-0 (2022).
Amani, B. & Amani, B. Efficacy and safety of nirmatrelvir/ritonavir (Paxlovid) for COVID-19: A rapid review and meta-analysis. J. Med. Virol. 95(2), e28441. https://doi.org/10.1002/jmv.28441 (2023).
Eligulashvili, A. et al. COVID-19 patients in the COVID-19 recovery and engagement (CORE) clinics in the Bronx. Diagnostics (Basel) https://doi.org/10.3390/diagnostics13010119 (2022).
Yong, S. J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. (Lond.) 53, 737–754. https://doi.org/10.1080/23744235.2021.1924397 (2021).
Goertz, Y. M. J. et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome?. ERJ Open Res. https://doi.org/10.1183/23120541.00542-2020 (2020).
Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 397, 220–232. https://doi.org/10.1016/S0140-6736(20)32656-8 (2021).
Carfi, A., Bernabei, R., Landi, F., Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA 324, 603–605. https://doi.org/10.1001/jama.2020.12603 (2020).
Musheyev, B. et al. Functional status of mechanically ventilated COVID-19 survivors at ICU and hospital discharge. J. Intensive Care 9, 31. https://doi.org/10.1186/s40560-021-00542-y (2021).
Musheyev, B. et al. Characterizing non-critically ill COVID-19 survivors with and without in-hospital rehabilitation. Sci. Rep. 11, 21039. https://doi.org/10.1038/s41598-021-00246-1 (2021).
Taboada, M. et al. Post-COVID-19 functional status six-months after hospitalization. J. Infect. 82, e31–e33. https://doi.org/10.1016/j.jinf.2020.12.022 (2021).
Raman, B. et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine 31, 100683. https://doi.org/10.1016/j.eclinm.2020.100683 (2021).
Halpin, S. J. et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 93, 1013–1022. https://doi.org/10.1002/jmv.26368 (2021).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 89, 594–600. https://doi.org/10.1016/j.bbi.2020.07.037 (2020).
Taquet, M., Luciano, S., Geddes, J. R. & Harrison, P. J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry 8, 1330–1140. https://doi.org/10.1016/S2215-0366(20)30462-4 (2021).
Takao, M. & Ohira, M. Neurological post-acute sequelae of SARS-CoV-2 infection. Psychiatry Clin. Neurosci. 77, 72–83. https://doi.org/10.1111/pcn.13481 (2023).
Freund, O. et al. Interactions and clinical implications of serological and respiratory variables 3 months after acute COVID-19. Clin. Exp. Med. 23(7), 3729–3736. https://doi.org/10.1007/s10238-023-01139-5 (2023).
Townsend, L. et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One 15, e0240784. https://doi.org/10.1371/journal.pone.0240784 (2020).
van den Borst, B. et al. Comprehensive health assessment 3 months after recovery from acute coronavirus disease 2019 (COVID-19). Clin. Infect. Dis. 73, e1089–e1098. https://doi.org/10.1093/cid/ciaa1750 (2021).
Boufidou, F. et al. SARS-CoV-2 reinfections and long COVID in the post-omicron phase of the pandemic. Int. J. Mol. Sci. https://doi.org/10.3390/ijms241612962 (2023).
Howell, C. R. et al. Associations between cardiometabolic disease severity, social determinants of health (SDoH), and poor COVID-19 outcomes. Obesity (Silver Spring) 30, 1483–1494. https://doi.org/10.1002/oby.23440 (2022).
Heller, C. G., Parsons, A. S., Chambers, E. C., Fiori, K. P. & Rehm, C. D. Social risks among primary care patients in a large urban health system. Am. J. Prev. Med. 58, 514–525. https://doi.org/10.1016/j.amepre.2019.11.011 (2020).
Boparai, M. S., Musheyev, B., Hou, W., Mehler, M. F. & Duong, T. Q. Brain MRI findings in severe COVID-19 patients: A meta-analysis. Front. Neurol. 14, 1258352. https://doi.org/10.3389/fneur.2023.1258352 (2023).
Zhang, V., Fisher, M., Hou, W., Zhang, L. & Duong, T. Q. Incidence of new-onset hypertension post-COVID-19: Comparison with influenza. Hypertension 80, 2135–2148. https://doi.org/10.1161/HYPERTENSIONAHA.123.21174 (2023).
Xu, A. Y., Wang, S. H. & Duong, T. Q. Patients with prediabetes are at greater risk of developing diabetes 5 months postacute SARS-CoV-2 infection: A retrospective cohort study. BMJ Open Diabetes Res. Care 11, e003257. https://doi.org/10.1136/bmjdrc-2022-003257 (2023).
Lu, J. Y. et al. Long-term outcomes of COVID-19 survivors with hospital AKI: Association with time to recovery from AKI. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfad020 (2023).
Freund, O. et al. Assessment of a close respiratory follow-up schedule at 3 and 6 months after acute COVID-19 and its related investigations. Respir. Med. 217, 107367. https://doi.org/10.1016/j.rmed.2023.107367 (2023).
Author information
Authors and Affiliations
Contributions
A.E.: conceptualization, data curation, formal analysis, investigation, methodology, validation, visualization, writing—original draft, writing—review & editing. M.D.: conceptualization, data curation, investigation, methodology, validation, writing—original draft, writing—review & editing. M.G., W.J.: data curation. K.P.F., S.C.: conceptualization, data curation, investigation, methodology, writing—original draft. T.Q.D.: conceptualization, data curation, investigation, methodology, project administration, supervision, writing—original draft, writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eligulashvili, A., Darrell, M., Gordon, M. et al. Patients with unmet social needs are at higher risks of developing severe long COVID-19 symptoms and neuropsychiatric sequela. Sci Rep 14, 7743 (2024). https://doi.org/10.1038/s41598-024-58430-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58430-y
- Springer Nature Limited