Abstract
Transient global amnesia (TGA) often involves precipitating events associated with changes in autonomic nervous system (ANS), and heart rate variability (HRV) reflects the ANS state. This study aimed to investigate HRV changes after TGA. A retrospective analysis of HRV included patients diagnosed with TGA between January 2015 and May 2020. The time and frequency domains of HRV were compared among three groups: early (< 1 week after TGA, n = 19), late (1–4 weeks after TGA, n = 38), and healthy control (HC, n = 19). The Pearson’s correlation between time and time-domain HRV was also examined. The standard deviation of NN intervals (SDNN) (early, 47.2; late, 35.5; HC, 41.5; p = 0.033) and root mean square of successive RR interval differences (RMSSD) (early, 38.5; late, 21.3; HC, 31.0; p = 0.006) differed significantly among the three groups. Post-hoc analysis showed statistically significant differences only in the early and late groups in both SDNN (p = 0.032) and RMSSD (p = 0.006) values. However, the frequency domain with total power, low-frequency and high-frequency powers, and low-frequency/high-frequency ratio did not differ. SDNN (Pearson correlation coefficient =− 0.396, p = 0.002) and RMSSD (Pearson correlation coefficient =− 0.406, p = 0.002) were negatively correlated with time after TGA. Changes in HRV occurred over time after the onset of TGA, with the pattern showing an increase in the first week and then a decrease within 4 weeks.
Similar content being viewed by others
Introduction
Transient global amnesia (TGA) is a clinical syndrome characterized by sudden and severe memory impairment without other neurological deficits, followed by full recovery within 24 hours1. Reversible selective memory disturbance is a key characteristic of TGA2,3. This unique and striking feature has long attracted the attention of researchers. Several pathogenic hypotheses have been proposed, including arterial ischemia, venous flow abnormality, seizure, migraine, and psychogenic disorders4,5. However, the pathogenesis of TGA has not been precisely elucidated.
TGA often follows precipitating events such as the Valsalva maneuver, emotional stress, a hot bath, a cold swim, physical exertion, sexual intercourse, and defecation6,7, most of which are closely related to changes in the autonomic nervous system (ANS), suggesting an association between TGA and ANS dysregulation. Heart rate variability (HRV) quantifies the variation in R-wave to R-wave (RR) intervals and its expression through several related variables8,9,10. HRV is considered a useful non-invasive tool for assessing ANS, particularly cardiac parasympathetic modulation11,12. HRV is easily measured, especially in the clinical setting where patients with TGA are first encountered and has been measured in other neurological conditions known to share pathomechanisms with TGA. While HRV has been studied in patients with potential etiologies of TGA, including cerebral ischemia, epilepsy, and migraine13,14,15,16, analytical studies of HRV in patients diagnosed with TGA are lacking.
Here, we aimed to identify changes in HRV in TGA patients and to determine how HRV changes over time in TGA patients compared to that in healthy controls (HCs). In addition, we wanted to identify the types of HRV that can be used to differentiate the disease clinically and explore whether they can help explain the pathogenesis of the disease.
Results
Clinical characteristics
The clinical characteristics of the early, late, and HC groups are shown in Table 1. No significant differences were found in the proportion of women (early, 63.2%; late, 73.7%; HC, 63.2%; p = 0.614) and mean age (early, 59.6 ± 8.1 years; late, 61.4 ± 7.3 years; HC, 54.4 ± 16.6 years; p = 0.067) among the three groups. The Mini-Mental State Examination (MMSE) scores of patients with TGA did not differ between the early and late groups (early, 24.9 ± 3.3; late, 25.0 ± 4.4; p = 0.960). Magnetic resonance imaging (MRI) abnormalities were identified in five patients each in the early (5/19, 26.3%) and late (5/38, 13.2%) groups (p = 0.275). All MRI abnormalities were dot-like diffusion-restricted lesions in the hippocampus. An electroencephalogram (EEG) showed left temporal sharp waves in one patient in the late group (1/38, 2.6%).
HRV-time domain
The HRV values for each group are shown in Table 2. The mean values of RR intervals, standard deviation of NN intervals (SDNN), and root mean square of successive RR interval differences (RMSSD) for each group were compared in the time-domain analysis. SDNN (early, 47.2 ± 19.2; late, 35.5 ± 10.9; HC, 41.5 ± 20.1; p = 0.033; partial eta squared (η2p) = 0.089) and RMSSD (early, 38.5 ± 29.3; late, 21.3 ± 11.0; HC, 31.0 ± 19.6; p = 0.006; η2p = 0.130), which reflect the total variability and parasympathetic activity, respectively, were significantly different among the three groups. The post hoc pairwise comparison showed higher SDNN (p = 0.032) and RMSSD (p = 0.006) values in the early group than in the late group. However, no significant difference was observed in the RR intervals among the three groups (early, 935.9 ± 184.2; late, 890.0 ± 114.7; HC, 899.0 ± 152.7; p = 0.522).
HRV-frequency domain
In the frequency-domain analysis, we compared the natural logarithms of the total power, low-frequency (LF) power, high-frequency (HF) power, and the original values of the low- to high-frequency power ratio (LF/HF). The natural logarithms of the total power (early, 7.1 ± 1.0; late, 6.6 ± 0.8; HC, 6.8 ± 1.0; p = 0.162), LF power (early, 5.4 ± 1.0; late, 4.9 ± 1.0; HC, 5.2 ± 1.2; p = 0.120), and HF power (early, 5.1 ± 1.5; late, 4.5 ± 1.1; HC, 5.0 ± 1.3; p = 0.122) demonstrated no significant differences among the three groups. Additionally, no significant difference was observed in the LF/HF (early, 1.8 ± 1.4; late, 2.0 ± 1.6; HC, 1.4 ± 0.8; p = 0.372).
Changes in HRV over time after TGA onset
We used the Pearson’s correlation coefficient (r) to examine the changes in SDNN and RMSSD values with time intervals after TGA (Fig. 1). SDNN (r = − 0.396, p = 0.002) and RMSSD (r = − 0.406, p = 0.002) had a weak negative correlation with the time interval after TGA. We also found that SDNN (β = − 0.644, p = 0.005) and RMSSD (β = − 0.951, p = 0.004) showed a significant negative correlation with time intervals after TGA using a linear regression adjusted for age and sex.
Discussion
We retrospectively assessed HRV in patients with TGA at two-time points and compared their HRV findings with those of HCs. The time-domain HRVs, SDNN and RMSSD, were lower when measured between 1 and 4 weeks after TGA than when measured within 1 week after TGA. SDNN and RMSSD decreased with the elapsed time after TGA. HRV measured within 1 week or between 1 and 4 weeks of TGA onset did not differ in the time or frequency domain compared to that of HC.
Three main hypotheses regarding the pathogenesis of TGA are cerebral ischemia, seizures, and migraine5. While no previous studies have directly explored the link between TGA and HRV, alterations in HRV associated with cerebral ischemia, seizures, and migraines have been documented. Prior research has reported reduced HRV in patients with cerebral infarction17,18, epilepsy15,19,20, and migraines21,22. In particular, HRV was not higher in patients within hours or days of symptom attack of cerebral ischemia, seizures, or migraine than in healthy controls. The higher HRV observed in our study within 1 week after TGA suggests that other pathomechanisms than those commonly proposed may underlie TGA. The higher HRV observed in the present study within 1 week after TGA leads us to expect a role for HRV as an adjunct to differential diagnosis in situations where it is clinically necessary to differentiate from stroke, epilepsy, and migraine, and further suggests that pathologic mechanisms other than those commonly suggested may underlie TGA. This is also consistent with the inability of any of these three hypothesized mechanisms to fully explain the pathogenesis of TGA.
In this study, we observed a temporary increase in HRV during the first week following a TGA episode, a pattern consistent with prior research revealing alterations in physiological indicators during the same timeframe. Among patients who underwent single-photon emission computed tomography within the initial week post-TGA, researchers detected a transitory reduction in perfusion, notably in the left hippocampus and left thalamus21. Additionally, an examination of EEG power spectra within the first week following a TGA episode revealed significantly diminished absolute beta 1 (12–17.9 Hz) and alpha power in TGA patients compared to those in HCs. This decrease was particularly pronounced in the left-sided locations and left temporal location23. These findings collectively suggest that the physiological changes occurring within the initial week following a TGA episode may have relevance to the condition. Up to 90% of patients experience pre-TGA onset precipitating events24,25. Women and men are more likely to experience emotional and physical precipitating events, respectively26. Events preceding TGA, such as emotional stress, bouts of exercise, and Valsalva maneuvers, are commonly accompanied by changes in the state of ANS. In previous studies, HRV decreased immediately after emotional stress in short experimental settings lasting less than 30 min before returning to baseline levels27,28,29. Additionally, HRV parameters demonstrate a curvilinear decline during exercise, a time-dependent recovery upon exercise cessation, and an eventual return to pre-exercise levels within minutes or up to 72 hours10,30,31,32,33. Notably, during post-exercise recovery, an HRV rebound phenomenon was observed, during which HRV overshoots above the pre-exercise levels in the hours or days after short and long exercise periods; however, the precise underlying mechanism is unclear31,34,35. In this study, HRV was elevated within 1 week after TGA and then decreased to a level not significantly different from that of controls. Although more data are needed, we speculate that the transient elevation may be a rebound phenomenon.
We observed decrease patterns in both the SDNN and RMSSD as time progressed following a TGA episode. These findings are significant as SDNN and RMSSD are key indicators of HRV, reflecting different aspects of ANS function. Specifically, SDNN represents overall HRV and is considered a marker of both sympathetic and parasympathetic activity, while RMSSD primarily reflects parasympathetic (vagal) activity, which is linked to heart rate deceleration36. The autonomic adjustment observed suggests a phase of recovery from the acute stress of TGA, where the initial heightened autonomic activity diminishes as the body returns to a stable state37. This reflects the ANS’s dynamic response after TGA, highlighting the usefulness of HRV measurements as indicators for recovery tracking and understanding TGA's autonomic effects.
This study has several limitations. First, continuous changes in HRV over time after TGA could not be identified, as HRV was not continuously measured. Second, HRV, which can be influenced by circadian rhythm, was measured in this study within the range of 9 AM to 5 PM. It is worth noting that the timing of measurements could introduce some variability as a potential limitation of the study. Third, we used a single-center design, and the study had a small sample size. Fourth, whether the transient elevation in HRV was primary or a consequence of TGA is unknown. In a clinical setting, however, it is nearly impossible to predict the moment TGA occurs and measure HRV just before the symptom onset of TGA.
This study also has several strengths. First, we determined the changes in HRV after TGA by reviewing electrocardiograms (ECGs) at two time points. To the best of our knowledge, this is the first study to describe post-TGA HRV changes over time. Second, we suggested the use of HRV for future research on TGA. Measuring HRV in TGA patients is readily accessible because ECG is commonly performed with EEG, which is frequently used for the differential diagnosis of TGA. Third, we made notable efforts to accurately diagnose TGA, which is defined by diagnostic criteria based primarily on patient- and witness-reported symptoms. Neurologists performed the clinical diagnoses of TGA in our study, and differential diagnoses were ruled out based on clinical, laboratory, radiological, and electrophysiological findings.
In conclusion, we found that TGA and changes in the state of ANS were related and that post-TGA HRV changed over time, showing an increase during the first week followed by a decrease within 4 weeks. Further studies with larger samples and continuous HRV monitoring may provide a deeper understanding of the role of temporary autonomic dysfunction in TGA, which may shed light on the pathogenesis of TGA.
Methods
Data and participants
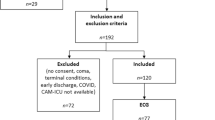
We created a study design and collected data for a retrospective observational study comparing HRV in patients with TGA and HCs. We retrospectively reviewed the data of 684 consecutive patients who visited the emergency department of Yongin Severance Hospital in Seoul, Republic of Korea, between January 2015 and May 2020 and were diagnosed with TGA. Neurology residents first examined all patients in the emergency department. A neurologist (KMK) then confirmed the diagnosis on the basis of medical records according to the Hodges and Warlow criteria1. Demographic and clinical characteristics, MMSE scores, brain MRI, and ECG with EEG data were collected. We excluded patients without MRI or ECG findings. Patients who underwent ECGs more than 4 weeks after the TGA episode were also excluded.
Of the 684 patients, 243 underwent MRI within 4 weeks, and only 57 underwent MRI and ECG over 20 min within 4 weeks of TGA onset. Of the 57 patients with TGA finally enrolled, those who underwent ECG within 1 week of TGA onset were assigned to the early group. Patients who underwent ECG between 1 and 4 weeks after the TGA episode were assigned to the late group. The selection of participants for this study is summarized in Fig. 2. ECG data were also collected from 19 HCs without medical, neurological, or psychiatric disorders who visited our institution for medical check-ups.
In the MRI analysis, abnormalities were defined as cases in which a neuroradiologist visually identified and reported any abnormality. For the EEG analysis, abnormalities were determined based on the identification of epileptiform discharges by an epileptologist.
This study was approved by the institutional review board of Yongin Severance Hospital, Yonsei University (No. 9-2020-0125). The requirement for written informed consent was waived owing to the retrospective nature of the study. Our research adhered to the ethical guidelines of the institutional and national research committees, aligning with the principles of the 1964 Declaration of Helsinki and its subsequent updates. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist.
HRV
HRV was recorded between 9 am and 5 pm under conditions of temperature and humidity appropriate for a hospital setting. HRV was analyzed using the ECG waveform obtained simultaneously with EEG. ECG was recorded using two electrodes placed at the parasternal area in the fourth intercostal space, similar to the V1 and V2 placements in general ECG recordings with 200 Hz sampling rate. All ECGs were recorded for at least 20 min, and 20-min concatenated segments were selected for analysis. The RR files were then exported to an HRV analysis program created in MATLAB38. Each ECG recording was manually inspected to avoid abnormal QRS wave morphology and movement artifacts and to ensure that the R-waves were correctly marked by the program to allow accurate detection of the RR intervals. The HRV analysis program applied a linear time-domain analysis to the entire 20-min segment to measure the mean and variance of the RR intervals. The following values were obtained: the mean of all RR intervals, SDNN, and RMSSD. Frequency‐domain parameters were computed using fast Fourier transform based on 5‐minute epochs that were averaged and included total power, LF power (0.04–0.15 Hz), HF power (0.15–0.40 Hz), and the LF/HF. All HRV analyses adhered to the analysis methods prescribed by the HRV Task Force in 199639.
Statistical analyses
The Statistical Package for Social Sciences (SPSS v24.0; IBM, Armonk, NY, USA) was used for all statistical analyses. Student’s t-tests or analyses of variance were used for continuous variables in demographic, clinical, and HRV variables when normality was confirmed using the Kolmogorov–Smirnov test. The post-hoc analysis employed the Bonferroni method for statistical comparisons of HRV variables among groups. Chi-square tests were used to compare categorical variables in demographic and clinical variables. Pearson's correlation analysis and multiple linear regression were conducted to examine the relationship between time after symptom onset and SDNN and RMSSD. We used partial eta squared (η2p) to quantify the effect size. Statistical significance was set at a two-tailed p-value of < 0.05.
Data availability
The data not provided in the article may be shared upon request to any qualified investigator for the purposes of replicating the procedures and results.
Change history
03 June 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-62399-z
References
Hodges, J. & Warlow, C. Syndromes of transient amnesia: Towards a classification. A study of 153 cases. J. Neurol. Neurosurg. Psychiatry 53, 834–843 (1990).
Bartsch, T. & Deuschl, G. Transient global amnesia: Functional anatomy and clinical implications. Lancet Neurol. 9, 205–214 (2010).
Bartsch, T. et al. Selective affection of hippocampal CA-1 neurons in patients with transient global amnesia without long-term sequelae. Brain 129, 2874–2884 (2006).
Jäger, T., Bäzner, H., Kliegel, M., Szabo, K. & Hennerici, M. G. The transience and nature of cognitive impairments in transient global amnesia: A meta-analysis. J. Clin. Exp. Neuropsychol. 31, 8–19 (2009).
Pantoni, L., Lamassa, M. & Inzitari, D. Transient global amnesia: A review emphasizing pathogenic aspects. Acta Neurol. Scand. 102, 275–283 (2000).
Alessandro, L. et al. Transient global amnesia: Clinical features and prognostic factors suggesting recurrence. Arquivos de Neuro-Psiquiatria 77, 3–9 (2019).
Spiegel, D. R. et al. Transient global amnesia: Current perspectives. Neuropsychiatr. Dis. Treat. 13, 2691–2703 (2017).
Berntson, G. G. et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 34, 623–648 (1997).
Vinik, A. I., Erbas, T. & Casellini, C. M. Diabetic cardiac autonomic neuropathy, inflammation and cardiovascular disease. J. Diabetes Investig. 4, 4–18 (2013).
Michael, S., Graham, K. S. & Davis, G. M. Cardiac autonomic responses during exercise and post-exercise recovery using heart rate variability and systolic time intervals—a review. Front. Physiol. 8, 301 (2017).
Buchman, T. G., Stein, P. K. & Goldstein, B. Heart rate variability in critical illness and critical care. Curr. Opin. Crit. Care 8, 311–315 (2002).
Schmidt, J. M. Heart rate variability for the early detection of delayed cerebral ischemia. J. Clin. Neurophysiol. 33, 268–274 (2016).
Xiong, L. et al. Autonomic dysfunction in different subtypes of post-acute ischemic stroke. J. Neurol. Sci. 337, 141–146 (2014).
Orlandi, G. et al. Transient autonomic nervous system dysfunction during hyperacute stroke. Acta Neurol. Scand. 102, 317–321 (2000).
Myers, K. A., Sivathamboo, S. & Perucca, P. Heart rate variability measurement in epilepsy: How can we move from research to clinical practice?. Epilepsia 59, 2169–2178 (2018).
Nilsen, K., Tronvik, E., Sand, T., Gravdahl, G. & Stovner, L. Increased baroreflex sensitivity and heart rate variability in migraine patients. Acta Neurol. Scand. 120, 418–423 (2009).
Chen, C.-F., Lai, C.-L., Lin, H.-F., Liou, L.-M. & Lin, R.-T. Reappraisal of heart rate variability in acute ischemic stroke. Kaohsiung J. Med. Sci. 27, 215–221 (2011).
Korpelainen, J. T., Sotaniemi, K. S. A., Mäkikallio, A., Huikuri, H. V. & Myllylä, V. V. Dynamic behavior of heart rate in ischemic stroke. Stroke 30, 1008–1013 (1999).
Jeppesen, J., Beniczky, S., Fuglsang-Frederiksen, A., Sidenius, P. & Jasemian, Y. Detection of epileptic-seizures by means of power spectrum analysis of heart rate variability: A pilot study. Technol. Health Care 18, 417–426 (2010).
Toth, V. et al. Periictal heart rate variability analysis suggests long-term postictal autonomic disturbance in epilepsy. Eur. J. Neurol. 17, 780–787 (2010).
Kim, B. S., Cho, S. S., Choi, J. Y. & Kim, Y. H. Transient global amnesia: A study with Tc-99m ECD SPECT shortly after symptom onset and after recovery. Diagn. Interv. Radiol. 22, 476 (2016).
Zhang, L., Qiu, S., Zhao, C., Wang, P. & Yu, S. Heart rate variability analysis in episodic migraine: A cross-sectional study. Front. Neurol. 12, 647092 (2021).
Primavera, A., Novello, P. & Stara, S. Transient global amnesia: A quantified electroencephalographic study. Acta Neurol. Scand. 87, 115–117 (1993).
Griebe, M. et al. Enhanced cortisol secretion in acute transient global amnesia. Psychoneuroendocrinology 99, 72–79 (2019).
Rsler, A., Mrass, G., Frese, A., Albert, I. & Schnorpfeil, F. Precipitating factors of transient global amnesia. J. Neurol. 1, 53–54 (1999).
Quinette, P. et al. What does transient global amnesia really mean? Review of the literature and thorough study of 142 cases. Brain 129, 1640–1658 (2006).
Tharion, E., Parthasarathy, S. & Neelakantan, N. Short-term heart rate variability measures in students during examinations. Natl. Med. J. India 22, 63–66 (2009).
Taelman, J., Vandeput, S., Vlemincx, E., Spaepen, A. & Van Huffel, S. Instantaneous changes in heart rate regulation due to mental load in simulated office work. Eur. J. Appl. Physiol. 111, 1497–1505 (2011).
Visnovcova, Z. et al. Complexity and time asymmetry of heart rate variability are altered in acute mental stress. Physiol. Meas. 35, 1319 (2014).
Stanley, J., Peake, J. M. & Buchheit, M. Cardiac parasympathetic reactivation following exercise: implications for training prescription. Sports Med. 43, 1259–1277 (2013).
Hautala, A. et al. Changes in cardiac autonomic regulation after prolonged maximal exercise. Clin. Physiol. 21, 238–245 (2001).
James, D., Barnes, A., Lopes, P. & Wood, D. Heart rate variability: response following a single bout of interval training. Int. J. Sports Med. 23, 247–251 (2002).
Mourot, L., Bouhaddi, M., Tordi, N., Rouillon, J.-D. & Regnard, J. Short-and long-term effects of a single bout of exercise on heart rate variability: Comparison between constant and interval training exercises. Eur. J. Appl. Physiol. 92, 508–517 (2004).
Arai, Y. et al. Modulation of cardiac autonomic activity during and immediately after exercise. Am. J. Physiol. Heart Circ. Physiol. 256, H132–H141 (1989).
Buchheit, M., Laursen, P. B., Al-Haddad, H. & Ahmaidi, S. Exercise-induced plasma volume expansion and post-exercise parasympathetic reactivation. Eur. J. Appl. Physiol. 105, 471–481 (2009).
Choi, I. Y. et al. Low heart rate variability from 10-s electrocardiograms is associated with development of non-alcoholic fatty liver disease. Sci. Rep. 12, 1062. https://doi.org/10.1038/s41598-022-05037-w (2022).
Erdur, H. et al. Myocardial injury in transient global amnesia: A case-control study. Eur. J. Neurol. 26, 986–991. https://doi.org/10.1111/ene.13920 (2019).
Pichot, V., Roche, F., Celle, S., Barthelemy, J.-C. & Chouchou, F. HRVanalysis: A free software for analyzing cardiac autonomic activity. Front. Physiol. 7, 557 (2016).
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93, 1043–1065 (1996).
Acknowledgements
None.
Funding
This study was supported by a research grant from Yongin Severance Hospital, Yonsei University College of Medicine, Korea. This study was supported by a faculty research grant of Yonsei University College of Medicine (6-2020-0068). The sponsors had no role in the study design; the collection, analysis, and interpretation of the data; the writing of the report; or the decision to submit this article for publication.
Author information
Authors and Affiliations
Contributions
S.C.: Data acquisition, analysis, and interpretation and drafting of the manuscript. S.H.L., H.J.L., M.K.C., W.K., and K.H.: Revision of the manuscript for important intellectual content. K.M.K.: Conception and design of the study; data acquisition, analysis, and interpretation and drafting and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained an error in the Funding section. The Grant Number of the Yonsei University College of Medicine was incorrect. Full information regarding the correction made can be found in the correction for this Article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, S., Lee, S.H., Lee, H.J. et al. Changes in heart rate variability over time from symptom onset of transient global amnesia. Sci Rep 14, 6944 (2024). https://doi.org/10.1038/s41598-024-57546-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57546-5
- Springer Nature Limited