Abstract
Both developed and developing countries carry a large burden of pediatric intussusception. Sentinel site surveillance-based studies have highlighted the difference in the regional incidence of intussusception. The objectives of this manuscript were to geospatially map the locations of hospital-confirmed childhood intussusception cases reported from sentinel hospitals, identify clustering and dispersion, and reveal the potential causes of the underlying pattern. Geospatial analysis revealed positive clustering patterns, i.e., a Moran’s I of 0.071 at a statistically significant (p value < 0.0010) Z score of 16.14 for the intussusception cases across India (cases mapped n = 2221), with 14 hotspots in two states (Kerala = 6 and Tamil Nadu = 8) at the 95% CI. Granular analysis indicated that 67% of the reported cases resided < 50 km from the sentinel hospitals, and the average travel distance to the sentinel hospital from the patient residence was calculated as 47 km (CI 95% min 1 km–max 378 km). Easy access and facility referral preferences were identified as the main causes of the existing clustering pattern of the disease. We recommend designing community-based surveillance studies to improve the understanding of the prevalence and regional epidemiological burden of the disease.
Similar content being viewed by others
Introduction
Both developed and developing countries carry a large burden of pediatric intussusception1. The sentinel surveillance-based studies conducted thus far have highlighted the difference in the regional prevalence of intussusception in children, for example, in India, i.e., 17.7 (95% CI 5.9, 41.4) in northern India to 254 (95% CI 5.9, 41.4) cases per 100,000 child years in southern India2,3. However, the true incidence, prevalence and epidemiology of intussusception are unclear3. Community-based studies illustrating the distribution and referral pattern of patients with this acute abdominal emergency are limited1,3. INCLEN established a nationwide multisite sentinel surveillance network (23 hospitals) in India for documenting the epidemiology of intussusception in children during the pre- and postrotavirus vaccine introduction periods4,5.
Geospatial methods provide promising insights for analyzing the distribution, distance and density of health events, care-seeking behavior and referral patterns6. Disease mapping is one of the most important public health tools because it provides a comprehensive understanding of the relationships between health conditions and places6,7,8,9. Geographical information system (GIS)-based disease mapping helps in understanding the locations of disease occurrence, disease transmission patterns, environmental and socioeconomic risk factors, healthcare utilization and the spatial relationships between them6,9. Furthermore, geospatial tools utilizing residences and hospital locations/coordinates could provide useful insights into clients’ decision-making behavior and hospital catchment areas6,9. Healthcare research and service delivery rely heavily on GIS-based mapping and clustering technologies to improve the knowledge base and interpretation, as well as visualization of the population and risk factor characteristics9,10,11. Furthermore, GIS has been proven to be a very useful tool for healthcare facility planning, as it provides analytical tools for assessing facility catchments and objectively analyzing the distance between clients and hospitals using various matrices, e.g., straight lines, travel distances and travel times12,13,14,15. The geostatistical functions that were successfully utilized in epidemiology and public health studies include nearest neighbor analysis, spatial autocorrelation analysis, network analysis, location-allocation, quadrant analysis, distance matrix, hotspots, density, spatial interpolation and ordinary least squares regression12,13,14,15,16,17,18,19,20. However, the utilization of geospatial tools is limited in low- and middle-income countries (LMICs) due to the lack of standardized open source data at the granular scale, poor data currency and partial national spatial data infrastructure21,22. Thus, there are fewer research studies using geospatial approaches in LMICs than in high-income countries (HICs)21,22,23. The objectives of this article are to (1) illustrate the geospatial distribution of hospital-confirmed intussusception cases in children, (2) examine the statistically significant clustering and dispersion of the cases, and (3) assess the potential reasons behind the existing distribution patterns of the cases.
Methods
The data utilized in this study were obtained from the INCLEN lead sentinel surveillance study2,24. The case data of intussusception children aged 2–23 months were collected from 23 nationally representative tertiary care hospitals (a mix of public and private) called sentinel surveillance sites across 22 states and union territories and were divided into four regions (North region, 5 sites, 3 public and 2 private; South region, 8 sites, 3 public and 5 private; East region, 7 sites, 6 public and 1 private; and West region, 3 sites, 2 public and 1 private) of India (S1 and S2; Supplementary file S1). The detailed methodology and selection of the sites have been published previously5. All of these sentinel hospitals served as referral centers for the same district, nearby districts, and even states. The INCLEN study documented intussusception in children aged 2–23 months through retrospective (from July 2010 to September 2017, total duration = 87 months) and prospective (April 2016–September 2017) surveillance conducted at these sentinel sites. The information on the address of the confirmed intussusception patients reported during the retrospective and prospective surveillance was collated for geospatial mapping at a granular scale.
Tools and techniques
Geospatial analysis was conducted using GIS software, i.e., the Environmental System Research Institute (ESRI) and ArcGIS Desktop 10. 8.2 ©, 2021, and open source geospatial foundation project, Q-GIS 3.1©, 2020. The coordinates of the residential addresses were extracted using Google Earth Pro©. Coordinates (latitude and longitude) were taken in degree-minutes-second (DMS) format. All the coordinates were documented in the Google Sheet© for easy transfer to the GIS software for visualization and geoanalytics. Attribute data were prepared while maintaining the study participant’s unique IDs, and all other personal identifiers were removed. For the cases where the full address was not available, the subdistrict locations were used for the extraction of proxy address coordinates.
Processes
The retrospective and prospective surveillance data were pooled for geospatial mapping and analysis. The study process flow is shown in Fig. 1. The findings generated through the descriptive analysis are expressed as proportions, means, standard deviations, or medians and interquartile ranges (IQRs), as appropriate. The specific geostatistical data analyses were conducted for the point-pattern analysis, geographical proximity, and care-seeking phenomena, as mentioned below.
-
The nearest neighbor index (NNI) was used to precisely measure the spatial relationship between the distribution of intussusception cases according to their residence13,25.
-
Moran’s I was calculated using the Global Moran's I tool to document the spatial autocorrelation based on the location and density of the cases. The z score and p value for statistical significance were calculated.
-
Hotspot analysis was performed using the Getis-Ord Gi* statistic after confirmation of the clustering in the data for each point feature (case location). For hotspot analysis, the data were processed using an integrated tool, and each point was given weights (inverse distance weights) based on the number of cases colliding within a 5-km diameter. The diameter was fixed by moving the circular window via the iterative distance method. The hotspot analysis helped in the identification of hot spots and cold spots using statistical significance.
-
Inverse distance weighting (IDW): The z scores were derived from the hotspot technique for visualization of the multivariate interpolation using the IDW function. The IDW assigned values to unknown points and prepared a continuous surface using a weighted average.
-
Geographical proximity of the treating facility and contiguity: The distance from the patient’s residence to the treating hospital was calculated using the hub analysis function in QGIS 3.1. Overlaying analysis was conducted using ArcGIS 10.8.2 software. Distribution pattern of patient residences according to hospital location studied using GIS tools, i.e., buffer, locational, contiguity analysis, etc.
-
A hub analysis and distance matrix were used to calculate the distance (Euclidean distance) of the treating hospitals from the residence. The cases were categorized into five distance bands: < 10 km, > 10–50 km, > 50–100 km, > 100–250 km, and > 251 km13,25.
Ethical issues
The study protocol was reviewed and approved by the ethics review committees of all the participating institutes. Confidentiality in the data handling was maintained. All the methods were performed in accordance with the ICMR National Ethical Guidelines for Biomedical and Health Research (2017).
Ethics approval and consent to participate
The study protocol was reviewed and approved by all the participating institutes. The list of ethics committees of the participating institutes included the INCLEN Independent Ethics Committee, The INCLEN Trust International, New Delhi, India (Ref No: IIEC 23; Dated June 30, 2015); the Institutional Ethics Committee, King George’s Medical University, Lucknow, Uttar Pradesh, India (Ref no: 7951/Ethics/R. Cell-15; Dated December 4, 2015); Institutional Ethics Committee, MP Shah Government Medical College, Jamnagar, Gujarat, India (ref no: 01/46/2016; Dated January 6, 2016); Institutional Ethics Committee, Sher-I-Kashmir Institute of Medical Sciences, Srinagar, Jammu & Kashmir, India (Ref no: 42/2015; Dated October 29, 2015); Institutional Ethics Committee, Gauhati Medical College, Guwahati, Assam, India (Ref no: MC/02/2015/274; Dated May 30, 2016); Institutional Human Ethics Committee, PSG Institute of Medical Sciences, Coimbatore, Tamil Nadu, India (Ref no 15/294; Dated November 16, 2015); Institutional Ethics Committee, King George Hospital, Andhra Medical College, Vishakhapatnam, Andhra Pradesh, India (Dated October 26, 2015); Institutional Ethics Committee, Fortis Escorts Hospital, Jaipur, Rajasthan, India (Ref no: FEHJ/IEC/15/0023; Dated September 14, 2015); Institutional Ethics Committee, Grant Medical College & JJ Hospital, Mumbai, Maharashtra, India (Ref no: IEC/Pharm/288/15; Dated November 19, 2015); Institutional Ethics Committee, Government Medical College & SAT Hospital, Thiruvananthapuram, Kerala, India (Ref no: 06/05/2015/MCT; Dated December 9, 2015); Medanta Institutional Ethics Committee, Medanta-The Medicity, Gurgaon, Haryana, India (MICR 559/2015; Dated January 21, 2016); Institutional Ethics Committee, SCB Medical College, Cuttack, Odisha, India; Institutional Ethics Committee, IMS & SUM Medical College & Hospital, Bhubaneswar, Odisha, India (Ref no 210/5/10/2015; Dated October 14, 2015); Institutional Ethics Committee; Choithram Hospital and Research Centre, Indore, Madhya Pradesh, India (Ref no: EC/Oct/15/20; Dated October 27, 2015); Institutional Ethics Committee, Agartala Government Medical College, Agartala, Tripura, India; Institutional Ethics Committee- Clinical Studies, Apollo Hospitals, Chennai, Tamil Nadu (Dated October 14, 2015); Institutional Ethics Committee, Maulana Azad Medical College, Delhi, India (Ref no: F.1/IEC/MAMC/50/4/2015/308; Dated November 20, 2015); Institutional Ethics Committee, Institute of Post Graduate Medical Education and Research, Kolkata, West Bengal, India (Ref no: Inst/IEC/2016/197; Dated March 1, 2016); Institutional Ethics Committee, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India (Ref no: 1256/Acad; Dated November 11, 2016); and Ethics Committee, Apollo Hospital, Hyderabad, Telengana, India ((Dated October 13, 2015). The interviews with stakeholders were performed after written informed consent was obtained. Written informed consent was obtained from the parents/legal guardians of the children enrolled in the study.
Results
Study participants and demographics
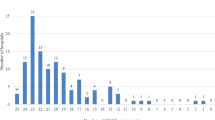
During the surveillance period, 2279 episodes of intussusception were reported among 2221 children across the 23 network hospitals (S1, S2; Supplementary file S1). A total of 58 children out of 2221 had more than 1 episode of hospitalization for intussusception. Thus, data for 2221 children (retrospective surveillance, n = 1566; prospective surveillance, n = 655) were analyzed. There were 1467 (66%) boys and 754 (34%) girls (male‒female ratio, 1.96). The majority (75%) of patients were less than 12 months old. A sharp increase (fivefold increase) in the annual number of intussusception cases at the sites was observed from 2010 to 2017 (S3, Supplementary file S1), with the highest (31%) increase occurring between 2014 and 2015.
Pattern and clustering of cases
Throughout the surveillance period, the highest number of intussusception cases was reported from the southern region (n = 1125, 51%; retrospective n = 833, prospective, n = 292), followed by the eastern (n = 607, 26.4%; retrospective, n = 410, prospective, n = 197), northern (n = 372, 17.1%; retrospective, n = 239, prospective, n = 133) and western (n = 117, 5.3%; retrospective, n = 84, prospective, n = 33) regions. The region wise case distribution pattern is shown in Fig. 2.
Distribution of intussusception cases. (a) Country-level distribution of patients. (b) Spatial pattern of intussusception cases and sentinel site hospital location in the northern region. (c) Spatial pattern of intussusception cases and sentinel site hospital location in the western region. (d) Spatial pattern of intussusception cases and sentinel site hospital location in the eastern region. (e) Spatial pattern of intussusception cases and sentinel site hospital location in the southern region. Software used: Arc GIS 10.8.2 https://desktop.arcgis.com/en/arcmap.
The average NNI was 0.171 (p value < 0.001) according to the pooled cases, suggesting a highly clustered pattern. The NNI varied from 0.311 to 0.171 across the four regions. The clustering pattern was further confirmed by a Moran’s I index of 0.071 at a statistically significant (p value < 0.0010) z score of 16.14. Moran’s I indicates the location of statistically significant hotspots in a few locations.
Hotspot analysis and IDW
The three regions where disease hotspots were found were the southern region, followed by the eastern and the northern regions. Hotspots were located in the Trivandrum (Kerala), Cuttack (Odisha), and Srinagar (Jammu and Kashmir) districts of India (see Fig. 3). Granular analysis revealed that, out of the 2221 locations (residence of children with intussusception) across the country, a high density of cases was reported from 14 locations (6 in Kerala and 8 in Tamil Nadu). The IDW surface generated using z scores computed via hotspot analysis indicated that the surface area followed a locus pattern and that the IDW faded with increasing distance from the hospital (Fig. 4). Additionally, the IDW values varied from 4.45 to –0.88 across the sites, which indicated greater variation and clustering.
Hotspot analysis of the residence location of children under two years old with intussusception in India. Software used: Arc GIS 10.8.2 https://desktop.arcgis.com/en/arcmap.
Interpolation of hotspots (z scores) and inverse distance weights (IDWs) for the residence locations of children under two years old with intussusception in India. Software used: Arc GIS 10.8.2 https://desktop.arcgis.com/en/arcmap.
Hub analysis and distance matrix
The average distance traveled by families to access a hospital for intussusception treatment was 47 km (95% CI 1–378). At the pooled level, 67% of the patients resided less than 50 km from the hospitals. No preferential behavior is observed in terms of traveling long distances for the treatment of male versus female children. Table 1 shows the distribution of the patients according to the different distance bands from the hospitals across all the 4 regions.
Distribution of cases and hospital proximity
The majority (n = 1555, 70%) of the reported cases were concentrated around six network hospitals. Thiruvananthapuram (Kerala, n = 843, 36.9%), Cuttack (Odisha, n = 271, 11.8%) and Srinagar (Jammu & Kashmir, n = 153, 6.7%) contributed the highest number of cases. The proximity analysis conducted in the GIS environment revealed that the majority of the cases were from nearby areas (same or adjacent districts). This was especially the case in the southern and western regions, where 59.4% and 67.8%, respectively, of the patients were concentrated at the same hospital or adjacent districts (Table 2).
Discussion
This is the first study describing the detailed spatial distribution of intussusception cases among children aged less than 2 years in India. The spatial aspects of the intussusception cases, including their geographical distribution, distance, density and direction, are presented in this manuscript. Previous studies have reported that the epidemiology of intussusception varies according to the country and region2,26. However, granular examination of the location of patients reported at sentinel surveillance network hospitals, with the help of geostatistics techniques, revealed that the regional pattern inferred from hospital-based studies may be misleading. Due to reporting bias, unfixed catchments, and unavailability of clinical registries, hospital caseloads do not represent the true epidemiological burden of the disease. It is important to note that the healthcare services offered by 23 hospitals under the surveillance site network were highly specialized, and admission to these hospitals was strictly referral-based5,24. Furthermore, a large proportion of patients with pediatric intussusception conditions do not reach tertiary care hospitals, resort to local healthcare facilities, reach tertiary healthcare facilities late, or die without timely intervention1. Other studies have also reported differential case fatalities, as observed in Africa (1 death in every 10 hospital admissions) and the rest of the world (fewer than 1 death in every 100–2000 hospital admissions)3,27. The availability of pediatric surgical facilities, specialists in surveillance network hospitals, referral systems and accessibility were the major factors influencing the differential caseloads reported from the surveillance hospitals. Understanding and recognizing the causes of disease localization are important in assessing the regional differences in the number of intussusception cases.
Like many other LMICs, India lacks a centralized health administrative database and comprehensive clinical registries28. Although the sentinel hospitals were tertiary care hospitals serving large catchment areas, there were other hospitals also serving the same catchment area. In the absence of fixed catchment areas, estimation of the risk ratio, floating accessibility14,15, demand and supply could not be performed. The catchment area of each hospital is influenced by the distance. The six hospitals from the three regions, i.e., southern (n-2), eastern (n-2) and northern (n-2) regions, had the highest number of cases. A total of 86% (1904/2221) of the episodes were reported from subdistricts within 100 km of referral hospitals. Approximately 60% of the patients in the southern region were from the same district, and 34% of the patients were from other districts where the hospitals were based. Conversely, in the North region, 45% of the patients were from distant districts (neither from the same district nor from adjacent districts). India is a large country with a 3.2 million km2 area. The probable reason for the greater average distance traveled in the North region is the relatively poor density of hospitals compared to that in the South region. However, further exploration is needed to determine the reasons for this interesting pattern of hospital access in the southern region, where disease reporting at sentinel hospitals was mostly from nearby areas, versus the northern region of India, where patients were from faraway areas.
The probability of cases being reported at hospitals for surgical purposes is a function of the distance between the patient location and healthcare providers29. The case reporting probability decreases (0.1–0.6) at a travel distance of 10 km and is effectively zero at distances > 30–40 km29. Our analysis clearly showed that the number of cases and hospital distance were inversely related, as29 two-thirds (67%) of the cases reported at the network hospitals were located less than 50 km apart, while one-third (33%) traveled more than 50 km. The median distance traveled for an intussusception patient was 47 km (95% CI 1–378 km) for hospitalization.
As per the 2011 census conducted by the national government, there are 640 districts and 5570 subdistricts in India. In this study, three major hotspots were identified, covering only 12 (n-640) districts of India. Techniques utilized for measuring the spatial pattern of diseases, i.e., nearest neighbor analysis (NNA), Moran's I, and disease hotspots, were also used in the literature10,18,19,20. Spatial analysis proved to be a valuable method for exploring the spatial patterns of intussusception cases.
Although demographic, clinical, diagnostic and treatment practice-related data were available in the hospital logs and registers, information on the patient distance and mode of transport road conditions was missing. Another constraint in conducting sophisticated network analysis is the unavailability of base maps depicting the road network with road type, surface, and quality information. Additionally, in LMICs, there is no well-established or functioning public transport system in many areas of developing countries13, and roads are adopted because of the convenience of traveling on foot or by vehicle. These data-related constraints are not found in the case of HICs14,15. The calculation of straight-line distances in a GIS environment provided a useful alternative to fill this data gap, and objective measures were made on the distance variable. The distance matrix used by us required only two-point coordinates, i.e., the origin (patient home) to the destination (health care facility) and a georeferenced baseman. A strong correlation was noted between straight-line distances and travel distances (r = 0.92, (p < 0.001))13. Euclidean distance was considered an acceptable proxy for the time spent traveling, especially in resource-poor settings13. For some locations, complete addresses were missing in the records; therefore, density clusters were generalized up to the subdistrict scale (1:5000 m). Patients who fell within a 5 km distance were snapped during the preprocessing stage. The 5 km radius was selected through the iterative process considering subdistricts as a primary unit of analysis.
Active surveillance or community-based surveillance provides a more complete picture for estimating the true burden of diseases29. Nevertheless, the strength of this study is that it provides important insights into the geospatial distribution of intussusception cases and the potential causes of the emerging pattern. To suggest any epidemiological pattern, more expanded regional and community-based studies are required to validate the results. Community-based studies conducted at demographic and health surveillance sites can provide added advantages by providing the exact population denominator for the calculation of spatial and temporal disease rates.
Limitations
This study has several limitations. Approximately 70% (2279) of the cases were captured through retrospective surveillance, and background information about these patients was retrieved from the hospital records. The data about barriers to seeking healthcare, such as socioeconomic status, access (travel mode), route, and time, were not available in hospital records. Furthermore, sentinel surveillance failed to provide a community-level estimation of total intussusception cases because there were more hospitals in the districts where patients might have gone for treatment, but cases could not be considered. The distance between the residence and the hospital was calculated using the straight-line method in a GIS environment. However, the exact travel-time distance could not be calculated using network analysis due to the lack of data on the travel mode and route taken by the patients. Granular data on road networks, including level, surface typology, and quality, were not available in open-source libraries. Additionally, the analysis was limited by the inability to define the catchment area for intussusception cases and to obtain accurate birth cohort data for the catchment population.
Conclusions
This study contributes new knowledge on the epidemiology of intussusception in children under two years of age and can reveal the regional pattern of intussusception, which cannot be determined by merely performing a quantitative analysis of cases from these sentinel sites. The use of sentinel surveillance data alone has health facility bias because the concentration of cases will increase near the preferred facility. Therefore, to assess the true burden and regional pattern of this disease, community-based surveillance studies are required at the identified hotspots and cold spot areas. Further research, including detailed information on local healthcare-seeking behavior, along with population measurements, is needed for accurate estimation of population-based incidence rates and epidemiology.
Data availability
All the data are available from the investigators and can be provided by the corresponding author upon reasonable request.
Abbreviations
- GIS:
-
Geographical information system
- km:
-
Kilometer
- NNI:
-
Nearest Neighbor Index
- LMIC:
-
Low and middle income country
- HIC:
-
High income country
References
Clark, A. D. et al. Update on the global epidemiology of intussusception: A systematic review of incidence rates, age distributions and case-fatality ratios among children aged < 5 years, before the introduction of rotavirus vaccination. 1316–1326. https://doi.org/10.1093/ije/dyz028 (2019).
Das, M. K. et al. Profile and epidemiology of intussusception in children under-two years of age: A prospective surveillance. Indian J. Pediatr. 88, 1187–1194 (2021).
Jiang, J. et al. Childhood intussusception: A literature review. PLoS ONE 8, 1–14 (2013).
Das, M. K. Experience of establishing and coordinating a nationwide network for bidirectional intussusception surveillance in India: lessons for multisite research studies. BMJ Open 11, e046827 (2021).
Das, M. K., Arora, N. K., Bonhoeffer, J., Zuber, P. L. F. & Maure, C. G. Intussusception in young children: Protocol for multisite hospital sentinel surveillance in India. Methods Protoc. 1, 1–9 (2018).
Boulos, M. N. K. Toward evidence-based, GIS-driven national spatial health information infrastructure and surveillance services in the United Kingdom. Int. J. Health Geogr. 3, 1 (2004).
Kwan, M. P. K. GIS methods in time-geographic research gis methods in time-geographic research: geocomputation and geovisualization of human activity patterns. Geogr. Ann. 86–267 (2004).
Mennecke, B. E. Geographic information systems in developing countries : Issues in data collection. Implementation and Management Geographic Information Systems in Developing Countries: Issues in Data. https://doi.org/10.4018/jgim.2001100103.This (2001).
Higgs, G. & Richards, W. The use of geographical information systems in examining variations in sociodemographic profiles of dental practice catchments: A case study of a Swansea practice. Prim Dent Care 9, (2002).
Chaikaew, N., Tripathi, N. K. & Souris, M. Exploring spatial patterns and hotspots of diarrhea in Chiang Mai Thailand. Int. J. Health Geogr. 8, 36 (2009).
Thornton, L. E. et al. Using Geographic Information Systems (GIS) to assess the role of the built environment in influencing obesity: A glossary. Int. J. Behav. Nutr. Phys. Act. 8, 71–71 (2011).
Schuurman, N., Randall, E. & Berube, M. A spatial decision support tool for estimating population catchments to aid rural and remote health service allocation planning. Health Inf. J. 17, 277–293 (2011).
Al-Taiar, A., Clark, A., Longenecker, J. C. & Whitty, C. J. Physical accessibility and utilization of health services in Yemen. Int. J. Health Geogr. 9, 38 (2010).
Luo, W. & Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 30, 865–884 (2003).
Ikram, S. Z., Hu, Y. & Wang, F. Disparities in spatial accessibility of pharmacies in Baton Rouge. Louisiana. Geogr. Rev. 105, 492–510 (2015).
Moore, D. A. & Carpenter, T. E. Spatial analytical methods and geographic information systems: use in health research and epidemiology. Epidemiol. Rev. 21, 143–161 (1999).
Huerta Munoz, U. & Källestål, C. Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int. J. Health Geogr. 11, 1–11 (2012).
Unwin, D. J. GIS, spatial analysis and spatial statistics. Prog. Hum. Geogr. 20, 540–551 (1996).
Tiwary, B. et al. Spatial evaluation of pregnancy loss among child-bearing women in India. GeoJournal 87, 3815–3826 (2022).
Singh, M. et al. Understanding the spatial predictors of malnutrition among 0–2 years children in india using path analysis. Front. Public Health 9, 667502 (2021).
Thomson, D. R. et al. Extending data for urban health decision-making: a menu of new and potential neighborhood-level health determinants datasets in LMICs. J. Urban Health 96, 514–536 (2019).
Acharya, P. S. & Pandey, S. National Spatial Data Infrastructure India (NSDI-India)—Present Status and the Future Strategies. in Geospatial Infrastructure, Applications and Technologies: India Case Studies (eds. Sarda, N. L., Acharya, P. S. & Sen, S.) 7–16 (Springer Singapore, Singapore, 2018). https://doi.org/10.1007/978-981-13-2330-0_2.
Naik, G., Basavaraj, K. P., Hegde, V. R., Paidi, V. & Subramanian, A. Using geospatial technology to strengthen data systems in developing countries: The case of agricultural statistics in India. Appl. Geogr. 43, 99–112 (2013).
Das, M. K. et al. Risk of intussusception after monovalent rotavirus vaccine (Rotavac) in Indian infants: A self-controlled case series analysis. Vaccine 39, 78–84 (2021).
Friedman, J. M. et al. Distance to hospital and utilization of surgical services in Haiti : Do children , delivering mothers , and patients with emergent surgical conditions experience greater geographical barriers to surgical care ? (2012).
Moodley, Y. Geospatial distribution of severe pediatric intussusception in KwaZulu-Natal province. South Africa. 36, 1–7 (2020).
Moodley, Y., Moodley, V. M., Mashele, S. S., Kiran, R. P. & Madiba, T. E. Geospatial distribution of severe pediatric intussusception in KwaZulu-Natal province, South Africa. Pan Afr. Med. J. 36, (2020).
Lecky, F. E. et al. Harnessing interdisciplinary collaboration to improve emergency care in low- and middle-income countries (LMICs): Results of research prioritization setting exercise. BMC Emerg. Med. 20, 68 (2020).
Nelli, L. et al. Distance sampling for epidemiology: An interactive tool for estimating underreporting of cases from clinic data. Int. J. Health Geogr. 19, 16 (2020).
Acknowledgements
We acknowledge the support from the Ministry of Health and Family Welfare, Government of India, for undertaking the study. We are thankful to the hospital administrations and the clinicians at the study site institutes, who supported and facilitated the undertaking of the study. We highly value the technical guidance and inputs provided by the members of the Technical Advisory Group: Satinder Aneja, Anju Seth and Archana Puri, Lady Hardinge Medical College, New Delhi; Ashok Patwari, Hamdard Institute of Medical Sciences & Research, New Delhi; Yogesh Kumar Sarin, Maulana Azad Medical College, New Delhi; Rakesh Aggarwal, Anshu Srivastava and Ujjal Poddar, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow; Malathi Satyasekharan, Kanchi Kamakoti Chailds Trust Hospital, Chennai; Raju Sharma and Nirupam Madan, All India Institute of Medical Sciences, New Delhi; Jyoti Joshi and Deepak Polpakara, Immunization Technical Support Unit; Ministry of Health & Family Welfare, New Delhi; Umesh D. Parashar; Centers of Disease Control and Prevention, Atlanta, USA; Naveen Thacker, Child Health Foundation, Gandhigram; and Rashmi Arora, Ansari, Nagar, New New Delhi. We acknowledge the contributions of the research staff at The INCLEN Trust International: Harshpreet Kaur, Janvi Chaubey, Mrimmaya Das, Shweta Sharma and Vaibhav Jain. We highly appreciate the efforts made by the research staffs at the study sites: Aarezo Bashir and Rafia; Sher-e-Kashmir Institute of Medical Sciences, Srinagar, Jammu & Kashmir; Prabha Shankar, Medanta-The Medicity Hospital, Gurgaon, Haryana; Anju Sharma; Maulana Azad Medical College, New Delhi; Anita Singh and Shubhranshu Srivastava, King George Medical University, Lucknow, Uttar Pradesh; Hemant Meena, Choithram Hospital, Indore, Madhya Pradesh; Pankaj Kumar and Shashi Kant; Indira Gandhi Institute of Medical Sciences, Patna, Bihar; Goutam Benia, IMS & SUM Medical College & Hospital, Bhubaneshwar, Odisha; Prasntajyoti Mohanty, SVP Post Graduate Institute of Pediatrics, Cuttack, Odisha; Angshuman Chatterjee, Institute of Postgraduate Medical Education and Research & SSKM Hospital, Kolkata, West Bengal; S. Yamuna, Andhra Medical College, Vishakhapatnam, Andhra Pradesh; Srinidhi Sudan, Apollo Hospitals, Hyderabad, Telengana; Rajesh Francis, Apollo Hospitals, Chennai, Tamil Nadu; T. Easter Chandru, PSG Institute of Medical Sciences, Coimbatore, Tamil Nadu; Deepthy R, Julie and Anju Shivkumar, Government Medical College & SAT Hospital, Thiruvananthapuram, Kerala; Archit Vaidya, Grant Medical College & JJ Hospital, Mumbai, Maharashtra; Nimesh Chouksey, MP Shah Government Medical College, Jamnagar, Gujarat; Nidhi Singh, Fortis Escorts Hospital, Jaipur, Rajasthan; Mrinmoy Gohain, Gauhati Medical College, Guwahati, Assam; Arpita Bhattachrjee, Saugat Ghosh and Tanusmita Debnath, Agartala Government Medical College, Agartala, Tripura.
Disclaimer
The content represents the views of the authors individually and does not necessarily represent the official positions of their organizations.
Funding
This project was supported by the Bill and Melinda Gates Foundation, USA, to The INCLEN Trust International (grant number OPP1116433). The funder or his or her representative had no role in the design of the study; the collection, analysis, or interpretation of the data; or the writing of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
MKD and NKA conceptualized the intussusception study. MKD coordinated the implementation and data collection. TIISNSG contributed to the acquisition of the data. SD and CRD contributed to the collation and analysis of the data. SD prepared analysis plan. SD and MKD interpreted the data. SD and MKD prepared and revised the manuscript. All the authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dixit, S., Das, M.K., Ramadugu, D.C. et al. Geospatial methodology for determining the regional prevalence of hospital-reported childhood intussusception in patients from India. Sci Rep 14, 6664 (2024). https://doi.org/10.1038/s41598-024-57187-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57187-8
- Springer Nature Limited