Abstract
The relationship between oral functions and dementia was examined in 7384 older adults (age ≥ 75 years) who visited a dental clinic in Gifu, Japan. Participants without dementia in a baseline survey in April 2018 were followed until March 2021. As oral functions, chewing function, tongue and lip function, and swallowing function were assessed by self-administered questionnaire, by oral diadochokinesis test, and by repetitive saliva swallowing test, respectively. The presence of systemic diseases was based on data obtained from the National Database of Health Insurance of Japan. At follow-up, 415 (6%) participants were diagnosed with dementia. Multivariate logistic regression analyses showed the presence of dementia at follow-up was associated with female (odds ratio [OR] 1.386; 95% confidence interval [CI] 1.117–1.719), age (OR 1.078; CI 1.056–1.101), regular dental checkups (absence; OR 1.452; CI 1.180–1.788), brushing frequency ≥ twice/day (absence; OR 1.510; CI 1.194–1.911), decayed teeth (presence; OR 1.328; CI 1.071–1.648), swallowing function (poor; OR 1.484; CI 1.135–1.939) at baseline. It was found that poor swallowing function was associated with the future onset of dementia.
Similar content being viewed by others
Introduction
In Japan, the population is aging more rapidly than in other countries1, and as of 2021, there were approximately 18.7 million older adults aged ≥ 75 years, accounting for nearly 15% of the total population2. The important issue in an aging society is the increasing prevalence of physical and mental disabilities with age3,4. Of the physical and mental disabilities with age, the proportion of older adults with dementia has been increasing in recent years, with a report in 2020 showing that 20% of older adults aged ≥ 75 years had dementia, which has become one cause of pressure on social security costs in Japan5. Dementia is a disease in which once normally developing intelligence is irreversibly decreased due to organic brain damage6,7. Dementia is often confused with age-related memory impairment8. However, it becomes more pronounced memory impairment, disorientation, and cognitive dysfunction as symptoms progress9,10. In addition, no fundamental treatment for dementia has yet been developed11. Therefore, it is very important to investigate factors related to dementia and explore immediate countermeasures.
Studies have reported the relationship between oral status and dementia. For example, it has been reported that tooth loss and occlusion affect brain function and trigger the onset of dementia12. It is also known that alterations of the oral microbiota causing chronic periodontal disease are associated with the risk of dementia13. In a longitudinal study, it was reported that poor periodontal health and tooth loss appear to increase the risk of both cognitive decline and dementia14. However, these reports demonstrated associations between specific oral diseases and dementia, and it is not clear from these diseases which oral functions are impaired and thus bring on dementia. Therefore, further studies investigating the longitudinal relationships between oral functions and dementia are needed.
In Japan, the National Database of Health Insurance of Japan (NDB) provides a database of the state of people with dementia. In addition, dental checkups including oral functions are conducted once a year for older adults aged ≥ 75 years in Gifu, Japan, and the results of oral functions are also compiled in a database. Therefore, by combining these data, it is possible to analyze the relationship between oral functions and dementia. Oral functions include chewing, swallowing, and tongue function, and the relationship between oral functions and dementia may differ according to the types of oral functions. Therefore, this was a longitudinal study over a period of two years in which the aim was to clarify the longitudinal relationships between three types of oral functions and dementia in Japanese older adults aged ≥ 75 years.
Methods
Participants
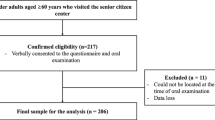
Data from community residents who received dental checkups in Gifu City, Kagamihara City, Kani City, and Ogaki City in Gifu, Japan, were analyzed. Between April 2018 and March 2019, a total of 8584 Japanese older adults aged ≥ 75 years participated in the baseline survey. First, participants with dementia at baseline (450 participants) were excluded. Furthermore, participants with missing data for oral functions, including participants with missing data for chewing function (8 participants), tongue and lip function (47 participants), and swallowing function (47 participants), were excluded from the analysis. Of these 8032 participants, 7384 were followed from April 2020 to March 2021 (follow-up rate, 92%). Therefore, the data of 7384 community residents (3078 men and 4306 women, mean age 80.0 years) were analyzed in the present study (Fig. 1).
Survey items in the National Health Insurance database system
The information about sex, age, and presence or absence of hypertension, diabetes mellitus, and dementia was obtained from the National Database of Health Insurance of Japan (NDB)15. Presence or absence with dementia was investigated both at baseline and follow-up, and Participants with dementia at follow-up selected as outcome.
Smoking habits and oral items
Data on the following smoking habits and oral items were obtained at baseline: presence or absence of regular dental checkups, presence or absence of brushing frequency ≥ twice/day, presence or absence of number of present teeth ≥ 20, presence or absence of decayed teeth, presence or absence of periodontal pockets ≥ 4 mm, chewing function, tongue and lip function, and swallowing function. The data for the oral items were provided by the Gifu Dental Association, Japan. For smoking habits, participants who smoked at least one cigarette per day were included (presence or absence)15,16. Regular dental checkups were considered to involve regular visits to the dental clinic (at least once every 6 months or less than once every 6 months)15,17. The number of decayed teeth was calculated as D (Decayed), missing teeth as M (Missing), and filled teeth as F (Filled), and the number of DMF teeth was used to evaluate dental caries history15,18. The coded values of the Community Periodontal Index (CPI) were used to evaluate periodontal pockets ≥ 4 mm, with codes 1 and 2 being evaluated as periodontal pockets ≥ 4 mm15,19. Chewing function was assessed by difficulty eating hard food. Participants were asked to choose from “It is more difficult to eat hard food than it was six months ago (presence or absence)” in the self-administered questionnaire15,20. Tongue and lip function was assessed using the oral diadochokinesis test for tongue and lip function, with poor tongue and lip function defined as less than 30 syllables in 5 s of any one of “Pa”, “Ta”, or “Ka”15,21. For swallowing function, those who swallowed less than 3 times in 30 s in the repetitive saliva swallowing test were evaluated as having poor swallowing function15,22.
Statistical analysis
The Kolmogorov–Smirnov test was used to check the normality of the data. Because all continuous variables were not normally distributed, data are expressed as medians (first and third quartiles). The chi-squared test was used to evaluate significant differences in characteristics of oral functions with and without dementia. Univariate and multivariate logistic regression analyses were performed with presence of dementia as the dependent variable. In the multivariate stepwise logistic regression analysis, variables with p > 0.10 were excluded from the model23. Additionally, variables that were significantly different in univariate logistic regression analysis were selected into a third category in addition to gender and age. A Hosmer–Lemeshow fit test was performed to confirm the goodness of fit of our model. A statistical analysis software (SPSS statistics version 27; IBM Japan, Tokyo, Japan) was used to analyze all data. A p values < 0.05 were considered significant15.
Research ethics
Our study is an experiment involving human participants and informed consent has been obtained in writing from all participants and/or their legal guardians, and the confirmation document is attached separately (Fig. 2). Our study was approved by the Ethics Committee of Asahi University (No. 33006) and was performed in accordance with the Declaration of Helsinki (as revised in Brazil 2013).
Results
Table 1 shows the characteristics of the participants at baseline and at follow-up. Overall, there were 3078 males (42%) and 4306 females (58%). The proportion of participants with hypertension (p < 0.001) was significantly higher at follow-up than at baseline. In addition, the proportion of participants with number of present teeth ≥ 20 (p < 0.001) was significantly lower at follow-up than at baseline. However, there were no significant differences in the other factors, except the proportions of those with hypertension and with number of present teeth ≥ 20, between at baseline and at follow-up.
Table 2 shows the characteristics of oral functions at baseline by with and without dementia at follow-up. In the present study, 415 participants (6%) were newly diagnosed with dementia at follow-up. Participants with dementia were characterized by a significantly higher proportion of poor tongue and lip function (p = 0.028) and poor swallowing function (p < 0.001) than those without dementia. On the other hand, there was no significant association between chewing function and dementia.
Table 3 shows crude odds ratio (OR) and 95% confidence interval (CI) for dementia at follow-up. The results showed that the risk of dementia after two years was significantly correlated with female (OR 1.368; 95% CI 1.112 to 1.684), age (OR 1.096; 95% CI 1.075 to 1.117), hypertension (presence; OR 1.304; 95% CI 1.062 to 1.601), regular dental checkups (absence; OR 1.620; 95% CI 1.322 to 1.984), brushing frequency ≥ twice/day (absence; OR 1.601; CI 1.277–2.006), number of present teeth ≥ 20 (absence; OR 1.337; CI 1.092–1.636), decayed teeth (presence; OR 1.490; CI 1.208–1.837), tongue and lip function (poor; OR 1.206; CI 1.025–1.549), and swallowing function (poor: OR 1.819; 95% CI 1.421 to 2.327) at baseline. On the other hand, there was no significant association between dementia after two years and chewing function at baseline.
Table 4 shows adjusted OR and 95% CI for dementia at follow-up. After adjusting for after adjusted for gender, age, hypertension, regular dental checkups, brushing frequency ≥ twice/day, number of present teeth ≥ 20, decayed teeth, tongue and lip function, and swallowing function, the risk of dementia at two years was significantly correlated with female (OR 1.386; 95% CI 1.117–1.719), age (OR 1.078; CI 1.056–1.101), regular dental checkups (absence; OR 1.452; CI 1.180–1.788), brushing frequency ≥ twice/day (absence; OR 1.510; CI 1.194–1.911), decayed teeth (absence; OR 1.328; CI 1.071–1.648), swallowing function (poor; OR 1.484; CI 1.135–1.939) at baseline. However, chewing function and tongue and lip function were not associated with the presence of dementia.
Discussion
To the best of our knowledge, this is the first longitudinal study to examine the associations between swallowing function and dementia in Japanese older adults using data from the NDB. The results showed that participants with dementia after two years of follow-up had a higher proportion of poor swallowing function at baseline than those without dementia. The results of logistic regression analysis showed that, after adjusting for gender, age, hypertension, regular dental checkups, brushing frequency ≥ twice/day, number of present teeth ≥ 20, decayed teeth, and tongue and lip function, the presence or absence of dementia after 2 years was associated with swallowing function at baseline. From these results, it was predicted that a decrease in swallowing function was associated with a higher risk of the onset of dementia in the future.
There are several possible mechanisms for the relationship between swallowing function and dementia. Swallowing actions activate brain function and improve learning and memory skills24,25. It was also reported that swallowing actions increase cerebral blood flow and the partial pressure of oxygen in the brain26. Decreased cerebral blood flow is a known risk factor for dementia27. Thus, participants with swallowing difficulties might have a greater risk for dementia because of reduced cerebral blood flow and even ischemia. In addition, people with poor swallowing function tend to consume less fruit and vegetables and more high-energy foods than those with good swallowing function28. High-calorie diets rich in carbohydrates and saturated fatty acids tend to increase the risk of dementia29. Therefore, these may be also among the mechanisms. However, further research is needed to clarify the mechanisms by which poor swallowing function is associated with dementia.
In the present study, chewing function was not associated with dementia. A previous report showed an association between chewing function using the evaluation of chewing function was based on muscle activity of the masticatory muscles and dementia30. The results in the previous and present studies may have been different due to their different measurement methods. In the future, we would like to consider judging chewing function by methods such as assessing the distribution of crushed particles in chewing samples (e.g., gummy jellies), the amount of elution of contents in chewing samples, or the activity of the masticatory muscles.
In addition, a cross-sectional study reported an association between poor tongue and lip function and dementia using the same research methodology as the present study31. This finding differs from the present study. This may be related to differences in research methods (cross-sectional vs. longitudinal studies). It may also be related to the bias in the proportion of participants with poor tongue and lip function at baseline. In the previous study, most participants possessed good tongue and lip function31, unlike the present study. Therefore, external validity should be considered in this study.
In the present study, lack of regular dental checkups and decayed teeth were associated with dementia. Past reports showed that recommendations for regular dental checkups reduced the risk of dementia onset32. Furthermore, it was reported that mutans bacteria that cause tooth decay adhere to the walls of blood vessels in the brain and reduce cognitive function33. These previous studies support the results of the present study. These studies reported that maintaining a good oral environment and controlling oral bacteria decrease the risk of dementia onset. In the present study, brushing frequency ≥ twice/day was associated with dementia. It is widely known that proper brushing habits are important for preventing decayed teeth and maintaining a good oral environment34,35. Therefore, participants in the present study who brushed ≥ twice/day may have engaged in proper brushing habits, had a good oral environment, and may not have had decayed teeth, and thus had a lower risk of dementia onset. Therefore, brushing habits may indirectly contribute to delaying the onset of dementia via maintaining a good oral environment.
There was no association between number of present teeth and dementia in our study. Past studies were reported that missing tooth is associated with development of Alzheimer's dementia36. This may be related to number of participants with missing tooth. In our study, proportion of participants with number of present teeth ≥ 20 was 66%, which is very higher than average in older adults aged ≥ 75 years in Japan (51.6%)37. Therefore, it is possible that there was no association between number of present teeth and dementia because number of participants with missing tooth was too small.
A major strength of the present study is its sample size of more than 7000 Japanese older adults. In addition, it was a longitudinal study, which is useful for establishing a causal relationship between dementia and poor swallowing function and for inferring factors that contribute to pressure on social security costs in Japan. Furthermore, it was possible to gather study population data from multiple locations in Gifu, Japan (Gifu City, Kagamihara City, Kani City, and Ogaki City).
In the present study, the Hosmer–Lemeshow fit test was used in a multivariate logistic regression analysis model. The Hosmer–Lemeshow fit test is used to examine the fit of a multivariate logistic regression analysis model and tests whether the observed event rate in a subgroup model fits the expected event rate. The Hosmer–Lemeshow test is considered to show a good fit with p values > 0.0538. In the present study, the p value was 0.288, suggesting a good fit.
However, there are several limitations to the present study. First, since participants of the present study visited to dental checkups, they may have been a highly health-conscious population. In our study, 8.6% of all participants were certified as needing supports and 6.9% were certified as needing cares based on Long-Term Care Insurance Law in Japan at baseline. This was a low value compared to proportion with certified as needed supports (8.8%) and needed cares (23.1%) in older adults aged ≥ 75 years in Japan2. Second, the presence or absence of diseases not in the database is unknown, since the NDB was used. Finally, our study is a longitudinal study, but may be the potential reversal of cause and effect. For example, certain types of dementia, like Parkinson’s-associated dementia and vascular dementia, are known to affect swallowing function, even in the preclinical stage of cognitive dysfunction.
In conclusion, the present study showed that Japanese older adults with poor swallowing function have a higher risk for future dementia.
Data availability
The data that support the findings of this study are available from “Gifu National Health Insurance Federation” and “Wide-Area Federation of Medical Care for Late-Stage Older People” but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of “Gifu National Health Insurance Federation” and “Wide-Area Federation of Medical Care for Late-Stage Older People”.
References
Arai, H. et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr. Gerontol. Int. 15, 673–687 (2015).
Cabinet Office. White paper on aging society 2022. (Cited 4 July 2023). Available from: https://www8.cao.go.jp/kourei/whitepaper/w-2022/zenbun/04pdf_index.html
Umit, T. et al. Age, gender and disability predict future disability in older people: The Rotterdam study. BMC Geriatr. 11, 1–7 (2011).
Gill, T. M., Han, L., Gahbauer, E. A., Leo-Summers, L. & Allore, H. G. Prognostic effect of changes in physical function over prior year on subsequent mortality and long-term nursing home admission. J. Am. Geriatr. Soc. 66, 1587–1591 (2018).
Ministry of Health Labour and Welfare. Patient survey in 2020. (Cited 4 July 2023). Available from: https://www.mhlw.go.jp/toukei/saikin/hw/kanja/20/index.html
Seth, A. G., Diler, A. & Kirk, R. D. Dementia. Am. J. Med. 131, 1161–1169 (2018).
Dag, A. Epidemiology and pathophysiology of dementia-related psychosis. J. Clin. Psychiatry 81, 27625 (2018).
Vladimir, H. Dementia: New vistas and opportunities. Neurol Sci. 40, 763–767 (2019).
Cheng, S. T. Dementia caregiver burden: A research update and critical analysis. Curr. Psychiatry Rep. 19, 64 (2017).
Ismail, Z. et al. Affective and emotional dysregulation as predementia risk markers: Exploring the mild behavioral impairment symptoms of depression, anxiety, irritability, and euphoria. Int. Psychogeriatr. 30, 185–196 (2018).
Tisher, A. & Salardini, A. A comprehensive update on treatment of dementia. Semin. Neurol. 39, 167–178 (2019).
Nakamura, T., Zou, K., Shibuya, Y. & Michikawa, M. Oral dysfunctions and cognitive impairment/dementia. J. Neurosci. Res. 99, 518–528 (2021).
Sureda, A. et al. Oral microbiota and Alzeimer’s disease: Do all roads lead to rome?. Pharmacol. Res. 151, 104582 (2020).
Asher, S., Stephen, R., Mäntylä, P., Suominen, L. A. & Solomon, A. Periodontal health, cognitive decline, and dementia: A systematic review and meta-analysis of longitudinal studies. J. Am. Geriatr. Soc. 70, 2695–2709 (2022).
Iwai, K. et al. Relationship between oral function and support/care-need certification in Japanese older people aged ≥ 75 years: A three-year cohort study. Int. J. Environ. Res. Public Health 19, 16959 (2022).
Sultan, Q. et al. Electronic cigarette among health science students in Saudi Arabia. Ann. Thorac. Med. 14, 56–62 (2019).
Patrick, A. F. et al. Recall intervals for oral health in primary care patients. Cochrane Datab. Syst. Rev. 14, 10 (2020).
Jo, F. Caries epidemiology and its challenges. Monogr. Oral Sci. 27, 11–23 (2018).
World Health Organization. Oral Health Surveys, Basic Methods 5th edn. (World Health Organization Publishers, 2013).
Ministry of Health Dental Health Division. Manual for dental health examination for late-stage senior citizens. (Cited 11 July 2023). Available from: https://www.mhlw.go.jp/content/000410121
Satake, A. et al. Effects of oral environment on frailty: Particular relevance of tongue pressure. Clin. Interv. Aging 12, 1643–1648 (2019).
Tamura, F., Mizukami, M., Ayano, R. & Mukai, Y. Analysis of feeding function and jaw stability in bedridden elderly. Dysphagia. 17, 235–241 (2002).
Iwai, K. et al. Association between self-reported chewing status and glycemic control in Japanese adults. Int. J. Environ. Res. Public Health 18, 9548 (2021).
Yamada, Y. Neural control mechanism for swallowing. NiigataDent.J. 29, 1–9 (1999).
Sessle, J. B. Fifty years of development of neuroscientific insights into orofacial pain and its control. J. Oral Rehabil. 50, 1–17 (2023).
Gowda, NS. & Jesus, DO. Brainstem infarction. StatPearls (2022).
Beishon, L. C. et al. The role of the autonomic nervous system in cerebral blood flow regulation in dementia: A review. Auton. Neurosci. 240, 102985 (2022).
Iwasaki, M. et al. Longitudinal association of dentition status with dietary intake in Japanese adults aged 75 to 80 years. J. Oral Rehabil. 43, 737–744 (2016).
Bednarz, K. & Siuda, J. Alzeimer’s disease and type 2 diabetes mellitus: Similarities in pathomechanisms lead to therapeutic opportunities. Neurol. Neurochir. Pol. 55, 418–428 (2021).
Yoshizawa, H. et al. Reciprocal cortical activation patterns during incisal and molar biting correlated with bite force levels: An fMRI study. Sci. Rep. 9, 8419 (2019).
Watanabe, Y. et al. Oral function as an indexing parameter for mild cognitive impairment in older adults, Geriatrics & gerontology international. Geriatr. Gerontol. Int. 18, 790–795 (2018).
Yamamoto, T. et al. Association between self-reported dental health status and onset of dementia: A 4-year prospective cohort study of older Japanese adults from the Aichi gerontological evaluation study (AGES) project. Psychosom. Med. 74, 241–248 (2012).
Watanabe, I. et al. Oral cnm-positive streptococcus mutans expressing collagen binding activity is a risk factor for cerebral microbleeds and cognitive impairment. Sci. Rep. 6, 38561 (2016).
Yousaf, M. et al. Individual, family, and socioeconomic contributors to dental caries in children from low- and middle-income countries. Int. J. Environ. Res. Public Health 19, 7114 (2022).
Tudoroniu, C., Popa, M., Iacob, M. S., Pop, L. A. & Nasui, A. B. Correlation of caries prevalence, oral health behavior and sweets nutritional habits among 10 to 19-year-old Cluj-Napoca Romanian adolescents. Int. J. Environ. Res. Public Health 17, 6923 (2020).
Tsuneishi, M., Yamamoto, T., Yamaguchi, T., Kodama, T. & Sato, T. Association between number of teeth and Alzheimer’s disease using the national database of health insurance claims and specific health checkups of Japan. PLoS One 16, e0251056 (2021).
Ministry of Health Labour and Welfare. Survey on dental diseases in 2022. (Cited 26 January 2024). Available from: https://www.mhlw.go.jp/content/10804000/001112405
Hosmer, D. W. & Lemeshow, S. Applied Logistic Regression 2nd edn. (Wiley, 2000).
Acknowledgements
This study was self-funded by the authors and their institution. The authors are grateful to the Gifu National Health Insurance Federation and the Wide-Area Federation of Medical Care for Late-Stage Older People for providing us with the data.
Author information
Authors and Affiliations
Contributions
The present study was carried out with the collaboration of all authors. K.I., T.A., and T.T. conceived the study. T.A., T.Y., Y.S., T.N., I.S., Y.I., Y.M., S.N., and Y.A. collected the data. K.I. and T.T. analyzed the data, interpreted the results, and wrote the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iwai, K., Azuma, T., Yonenaga, T. et al. Longitudinal association of oral functions and dementia in Japanese older adults. Sci Rep 14, 5858 (2024). https://doi.org/10.1038/s41598-024-56628-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-56628-8
- Springer Nature Limited
This article is cited by
-
Short-term data suggests cognitive benefits in the elderly with single-implant overdentures
Evidence-Based Dentistry (2024)