Abstract
The emergence and dissemination of carbapenem-resistant species of Acinetobacter and Pseudomonas have become a serious health concern. Routine antimicrobial disk susceptibility tests in clinical laboratories cannot distinguish between isolates that are highly carbapenem-resistant and those that are moderately carbapenem-resistant. The present study describes antimicrobial susceptibility tests using disks containing high doses (1000 μg) of meropenem. The diameters of inhibition zones were significantly negatively correlated with the MICs of Pseudomonas and Acinetobacter species for meropenem (R2: 0.93 and 0.91, respectively) and imipenem (R2: 0.75 and 0.84, respectively). Double disk synergy tests using clavulanic acid or sodium mercaptoacetate can detect ESBL or MBL producers. Susceptibility tests using disks containing high doses of meropenem can easily detect highly carbapenem-resistant isolates in a quantitative manner. These disks may be useful in bacteriological laboratories because of their technical ease, stability, and relatively low cost.
Similar content being viewed by others
Introduction
The emergence and spread of carbapenem-resistant species of Pseudomonas and Acinetobacter have become a serious health concern worldwide1. Infections with these microorganisms are associated with high mortality rates and limited treatment options2. Several mechanisms, including efflux pumps, porin channels and production of carbapenemases, contribute to carbapenem resistance in Acinetobacter and Pseudomonas species, with carbapenemases being especially responsible for high carbapenem resistance3,4. These bacteria frequently produce carbapenemases, including metallo-β-lactamases (MBLs), such as DIM-, IMP-, NDM- and VIM-type MBLs; as well as variants of OXA-type and extended-spectrum β-lactamases (ESBLs), such as GES-5, OXA-23, OXA-48 and OXA-723,4. In bacteriological laboratories, however, routine antimicrobial susceptibility testing, including both disk diffusion and microdilution methods, are unable to quantify the levels of carbapenem resistance, because neither method has been adapted to analyze highly carbapenem-resistant isolates. Most carbapenemase-producing isolates of Pseudomonas and Acinetobacter species are highly resistant to carbapenems4, and several agents to infections caused by carbapenem-resistant isolates has been developed such as ceftazidime-avibactam, ceftolozane-tazobactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, plazomicin, eravacycline, and cefiderocol5. Therefore, it is clinically important to distinguish highly from moderately carbapenem-resistant isolates in clinical laboratories, which would also provide useful information about infection control practice in hospitals.
The mean peak plasma concentrations of carbapenems were actually 112 μg/ml (range: 83–140 μg/ml) after a 5-min intravenous bolus injection and 49 μg/ml (range 39–58 μg/ml) after a 30 min intravenous infusion, according to the product monograph6. Furthermore, different formula could be developed in infections with them, such as antimicrobial agents combined with carbapenemase-inhibitors and/or efflux pomp inhibitors5. Routine antimicrobial susceptibility testing of clinical isolates, including disk diffusion methods and twofold microdilution methods, cannot distinguish highly from moderately carbapenem-resistant isolates, because these methods have not been adapted to evaluation of highly carbapenem-resistant isolates7,8. The present study describes the development of antimicrobial susceptibility tests using disks containing high doses (1000 μg) of meropenem. This method was easily able to detect highly carbapenem-resistant Pseudomonas and Acinetobacter species, and it could be applicable especially in bacterial laboratories in developing countries where genetic diagnosis testing is not introduced.
Methods
Bacterial strains
All clinical isolates tested were obtained in the studies described in Tables 1 and 2, and their whole genome sequences had been determined using MiSeq (Illumina, San Diego, CA, USA) in the previous studies9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. This study evaluated 125 clinical isolates of Pseudomonas species, comprising 111 isolates of Pseudomonas aeruginosa, 10 of P. asiatica and four of P. monteilii; and 112 clinical isolates of Acinetobacter species, comprising 105 isolates of Acinetobacter baumannii, three of A. nosocomialis, and one each of A. bereziniae, A. indicus, A. pittii and A. radioresistens. Of all the isolates tested, 84 Pseudomonas isolates and 85 Acinetobacter isolates were resistant to meropenem. All meropenem-resistant isolates of Pseudomonas species harbored genes encoding various types of β-lactamase and were expected to produce them, including various metallo-β-lactamases, including DIM-1-type (n = 1), both DIM-1- and NDM-1-type (n = 1), IMP-1-type (n = 5), IMP-1- and DIM-1-type (n = 1), IMP-6-type (n = 1), IMP-7-type (n = 1), IMP-43-type (n = 1), IMP-44-type (n = 1), NDM-1-type (n = 9), VIM-1-type (n = 8), VIM-2-type (n = 10), VIM-24-type (n = 6), and VIM-60-type (n = 3); and various GES-types of serine β-lactamases, including GES-1-type (n = 2), GES-5-type (n = 18), GES-6-type (n = 1), GES-15-type (n = 5), GES-24-type (n = 1), GES-26-type (n = 13), GES-30-type (n = 1) and KPC-2-type (n = 2) (All these β-lactamase-producing isolates were described in references cited in Table1.). Eighty meropenem-resistant isolates of Acinetobacter species harbored genes encoding various types of carbapenemase and were expected to produce them, including IMP-14 metallo-β-lactamase (n = 1); NDM-1-type metallo-β-lactamase (n = 4); NDM-1-type metallo-β-lactamase and OXA-type and PER-type serine β-lactamases (n = 4); NDM-1-type metallo-β-lactamase and OXA-type serine β-lactamase (n = 4); NDM-1-type metallo-β-lactamase and OXA-type, VEB-type and ADC (OXA-51-like) serine β-lactamases (n = 2); NDM-1-type metallo-β-lactamase and TEM-type and ADC serine β-lactamases (n = 1); and several types of serine β-lactamase, including OXA-, TEM-, PER-, VEB- and ADC-type serine β-lactamases (n = 71) (These isolates were described in references in Table 2.). Acinetobacter baumannii harbors an intrinsic blaOXA-51-like gene encoding a charbapenemase, and an intrinsic blaADC encoding cephalosporinase, ADC (AmpC) β-lactamas, on chromosome; and ISAba1 flanked by the blaOXA-51-like and blaADC are responsible for the production of OXA-51-like carbapenemase and the production of ADC cephalosporinase β-lactamase, respectively2. Two isolates of A. baumannii NCGM174 and NCGM211 listed in Table 2 were resistant to carbapenem and expected to produce ADC, because they harbored blaADC flanked by ISAba1, but not other genes associated with known β-lactamases. P. aeruginosa ATCC27853 and PAO1 (ATCC15692) were obtained from the American Type Culture Collection (Manassas, VA, USA).
Antimicrobial disk susceptibility tests
Antimicrobial susceptibility tests were performed using disks containing standard (10 μg), moderate (100 μg) and high (1000 μg) doses of meropenem. Each isolate was suspended in sterile saline and adjusted to a turbidity of 0.5 McFarland units. Isolates were inoculated onto Mueller–Hinton (MH) agar plates with sterile cotton swabs. A disk containing meropenem was placed onto the center of each plate, and the plates were incubated at 35 °C for 18 h to test Pseudomonas species or 24 h to test Acinetobacter species. The diameter (mm) of each inhibition zone was measured.
Double disk synergy tests
Double disk synergy tests were performed using disks containing 1000 μg meropenem, together with disks containing the ESBL inhibitor clavulanic acid (40, 80 or 120 μg)27, or disks containing the MBL inhibitor sodium mercaptoacetate (3000, 6000 or 12,000 μg)28. Bacterial isolates were inoculated onto MH agar plates, and two disks, one containing meropenem and the other containing clavulanic acid or sodium mercaptoacetate, were separately placed on these plates at center-to-center distances of 5, 10 or 20 mm. The plates were incubated at 35 °C for 18 or 24 h, as described above, and the shape of each meropenem inhibition zone was determined.
Microdilution method
The MICs of imipenem, meropenem, ciprofloxacin and amikacin were also determined by a microdilution method, as described by Clinical Standards Laboratory Institute guidelines7. Carbapenemase production was detected with the CIMTrisII carbapenem inactivation method (Kohjin Bio, Saitama, Japan)24.
Ethical approval and consent to participate
This study was approved by the Biosafety Committee, Juntendo University [Approval Number BSL2/29-1].
Results
Antimicrobial disk susceptibility tests
Testing of antimicrobial susceptibility using standard disks containing 10 μg meropenem showed that carbapenem-susceptible P. aeruginosa PAO1 formed an inhibition zone of diameter 24 mm (Fig. 1A), whereas carbapenem-resistant P. aeruginosa IMCJ2.S1 did not form any inhibition zone (Fig. 1B). When tested with disks containing a moderate dose of meropenem (100 μg), PAO1 showed an inhibition zone of diameter 34 mm, whereas IMCJ2.S1 did not show any inhibition zone (date not shown). Using disks containing a high dose of meropenem (1000 μg), PAO1 and IMCJ2.S1 formed inhibition zones of diameter 50 mm (Fig. 1C) and 15 mm (Fig. 1D), respectively.
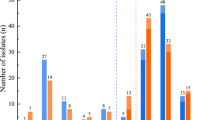
Testing of Pseudomonas species showed that the diameters of inhibition zones were significantly negatively correlated with MICs for both meropenem (R2: 0.93) and imipenem (R2: 0.75) but did not correlate with MICs for amikacin (R2: 0.31) or ciprofloxacin (R2: 0.63) (Fig. 2). The diameters of inhibition zones of Acinetobacter species were also significantly negatively correlated with MICs for meropenem (R2: 0.91) and imipenem (R2: 0.84) but did not correlate with MICs for amikacin (R2: 0.45) or ciprofloxacin (R2: 0.50) (Fig. 3).
Double disk synergy tests
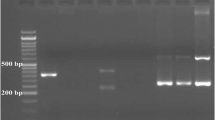
Double disk synergy tests were performed using a P. aeruginosa isolate that produced GES-5. Placement of a disk containing 10 μg clavulanic acid, together with a disk containing 1000 μg meropenem, on an MH agar plate at a distance of 5 or 10 mm showed that clavulanic acid did not alter the shape of the meropenem inhibition zone (Fig. 4). The shape of the meropenem inhibition zone was also unaffected by placement of a disk containing 40 μg clavulanic acid at distances of 5 and 10 mm (Fig. 5A,B). At a distance of 20 mm, the meropenem inhibition zone was slightly enhanced at the front of the disk containing 40 μg clavulanic acid, altering the shape of the meropenem inhibition zone (Fig. 5C). Placement of a disk containing 80 μg clavulanic acid 20 mm from the disk containing 1000 μg meropenem enhanced the meropenem inhibition zone at the front of the clavulanic acid-containing disk (Fig. 6A). This enhancement of the inhibition zone was also observed when a disk containing 120 μg clavulanic acid was placed 20 mm from the disk containing 1000 μg meropenem, although the clavulanic acid disk alone formed an inhibition zone (Fig. 6B). These findings showed that double disk synergy tests of a P. aeruginosa isolate producing GES-24 with clavulanic acid doses of 80 and 120 μg similarly enhanced the inhibition zone formed by 1000 μg meropenem (Fig. 7).
Double disk synergy tests were also performed using an isolate of NDM-1 producing P. aeruginosa. Separate placement of disks containing 1000 μg meropenem and 3000 μg sodium mercaptoacetate on MH agar plates at distances of 5, 10 and 20 mm showed that, at distances of 5 and 10 mm, the meropenem inhibition zone was slightly enhanced at the front of the disks containing sodium mercaptoacetate (Fig. 8A,B), with greater enhancement observed when the disks were at a distance of 20 mm (Fig. 8C). This enhancement of the inhibition zone was also observed following placement of a disk containing 6000 μg sodium mercaptoacetate (Fig. 9A). Moreover, a disk containing 12,000 μg sodium mercaptoacetate alone formed an inhibition zone (Fig. 9B), as did a disk containing 10 μl of 0.5 M EDTA, an inhibitor of metallo-β-lactamase such as NDM-1 (data not shown).
Discussion
The present study found that antimicrobial susceptibility tests using disks containing a high dose of meropenem were able to quantitatively determine the carbapenem resistance of Acinetobacter and Pseudomonas species (Figs. 2, 3). Of the 125 clinical isolates of Pseudomonas species tested, 70 were highly resistant to meropenem, defined as having MICs ≥ 64 μg/ml for meropenem (Table 1), with 69 of these 70 highly carbapenem-resistant isolates of Pseudomonas having inhibition zones of diameter < 32 mm (Table 3). Moreover, all 42 highly carbapenem-resistant isolates of Acinetobacter species had inhibition zones of diameter < 27 mm (Table 3).
These findings suggest that, in double disk synergy tests, a disk containing 1000 μg meropenem and a disk containing 80 μg clavulanic acid should be placed 20 mm apart on an MH agar plate to detect bacteria that produce class A carbapenems, whereas a disk containing 1000 μg meropenem and a disk containing 6000 μg sodium mercaptoacetate should be placed 20 mm apart on an MH agar plate to detect bacteria that produce class B metallo-β-lactamases. Although double disk synergy tests were optimized to detect ESBL and MBL producers, these tests failed to detect OXA-23 and KPC-2 producers. Similar results were observed with double disk synergy tests using standard disks that could not detect producers of OXA-type and KPC-type carbapenemases. Carbapenem inactivation methods, such as CIMTrisII24 are useful in the detection of Pseudomonas spp. and Acinetobacter spp. isolates that produce all types of carbapenemases, including OXA-type and KPC-type enzymes. These disks may be useful in bacteriological laboratories because of their technical ease, stability, and relatively low cost. Antimicrobial susceptibility tests using disks containing a high dose of meropenem will be useful in bacteriological laboratories because of their technical ease, stability, and relatively low cost. Although screening agar containing carbapenems has been shown useful in detecting carbapenem-resistant isolates of Enterobacteriaceae29,30,31, screening agar has not been routinely used in bacteriological laboratories because carbapenems in agar are chemically instable, making laboratory storage difficult.
Conclusion
Susceptibility tests using disks containing a high dose of meropenem (1000 μg) can easily detect highly carbapenem-resistant isolates of Acinetobacter and Pseudomonas species in a quantitative manner. Double disk synergy tests using the disk containing meropenem with a disk containing a high dose of clavulanic acid (80 μg) or sodium mercaptoacetate (6000 μg) can detect ESBL and MBL producers, respectively, although these tests failed to detect OXA-23 and KPC-2 producers.
Data availability
The datasets analyzed during the current study are available from the corresponding author on request.
Abbreviations
- ESBL:
-
Extended-spectrum β-lactamase
- MBL:
-
Metallo-β-lactamase
- MH:
-
Mueller-Hinton
- MIC:
-
Minimal inhibitory concentration
References
Potron, A., Poirel, L. & Nordmann, P. Emerging broad-spectrum resistance in Pseudomonas aeruginosa and Acinetobacter baumannii: Mechanisms and epidemiology. Int. J. Antimicrob. Agents. 45, 568–585. https://doi.org/10.1016/j.ijantimicag.2015.03.001 (2015).
Gniadek, T. J., Carroll, K. C. & Simner, P. J. Carbapenem-resistant non-glucose-fermenting Gram-negative bacilli: The missing piece to the puzzle. J. Clin. Microbiol. 54, 1700–1710. https://doi.org/10.1128/jcm.03264-15 (2016).
Darby, E. M. et al. Molecular mechanisms of antibiotic resistance revisited. Nat. Rev. Microbiol. 21, 280–295. https://doi.org/10.1038/s41579-022-00820-y (2023).
Queenan, A. M. & Bush, K. Carbapenemases: The versatile β-lactamases. Clin. Microbiol. Rev. 20, 440–458. https://doi.org/10.1128/cmr.00001-07 (2007).
Doi, Y. Treatment options for carbapenem-resistant gram-negative bacterial infections. Clin. Infect. Dis. 69, S565–S575. https://doi.org/10.1093/cid/ciz830 (2019).
Pfizer Laboratories. Product monograph: MEROPENEM IV (meropenem for injection) Pfizer Inc. NY. https://www.pfizer.com/products/product-detail/merrem_i_v (2023)
Wayne, P. A. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 32th ed, informational supplement. CLSI M100-S30. http://em100.edaptivedocs.net/dashboard.aspx (2022).
The European Committee on Antimicrobial Susceptibility Testing. Clinical breakpoints - breakpoints and guidance. The European Committee on Antimicrobial Susceptibility Testing. https://www.eucast.org/clinical_breakpoints/ (2022)
Tohya, M. et al. Emergence of clinical isolates of Pseudomonas asiatica and Pseudomonas monteilii from Japan harbouring an acquired gene encoding a carbapenemase VIM-2. J. Med. Microbiol. 70, 001258. https://doi.org/10.1099/jmm.0.001258 (2021).
Tohya, M. et al. Emergence of carbapenem-resistant Pseudomonas asiatica producing NDM-1 and VIM-2 metallo-β-lactamases in Myanmar. Antimicrob. Agents Chemother. 63, e00475-e519. https://doi.org/10.1128/aac.00475-19 (2019).
Tada, T. et al. Molecular characterization of multidrug-resistant Pseudomonas aeruginosa isolates in hospitals in Myanmar. Antimicrob. Agents Chemother. 63, e02397-e2418. https://doi.org/10.1128/aac.02397-18 (2019).
Hisihinuma, T. et al. Spread of GES-5 carbapenemase-producing Pseudomonas aeruginosa clinical isolates in Japan due to clonal expansion of ST235. PLoS ONE 13, e0207134. https://doi.org/10.1371/journal.pone.0207134 (2018).
Tada, T. et al. Pseudomonas aeruginosa clinical isolates in Nepal coproducing metallo-β-lactamases and 16S rRNA methyltransferases. Antimicrob. Agents Chemother. 61, e00694. https://doi.org/10.1128/aac.00694-17 (2017).
Tada, T., Miyoshi-Akiyama, T., Shimada, K., Shimojima, M. & Kirikae, T. IMP-43 and IMP-44 metallo-β-lactamases with increased carbapenemase activities in multidrug-resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 57, 4427–4432. https://doi.org/10.1128/aac.00716-13 (2013).
Uechi, K. et al. A modified carbapenem inactivation method, CIMTris, for carbapenemase production in Acinetobacter and Pseudomonas species. J. Clin. Microbiol. 55, 3405–3410. https://doi.org/10.1128/jcm.00893-17 (2017).
Miyoshi-Akiyama, T., Kuwahara, T., Tada, T., Kitao, T. & Kirikae, T. Complete genome sequence of highly multidrug-resistant Pseudomonas aeruginosa NCGM2.S1, a representative strain of a cluster endemic to Japan. J. Bacteriol. 193, 7010. https://doi.org/10.1128/jb.06312-11 (2011).
Hishinuma, T., Tada, T., Uchida, H., Shimojima, M. & Kirikae, T. A novel VIM-type metallo-β-lactamase variant, VIM-60, with increased hydrolyzing activity against fourth-generation cephalosporins in Pseudomonas aeruginosa clinical isolates in Japan. Antimicrob. Agents. Chemother. 63, e00124-e219. https://doi.org/10.1128/aac.00124-19 (2019).
Hishinuma, T. et al. Emergence and spread of VIM-type metallo-β-lactamase-producing Pseudomonas aeruginosa clinical isolates in Japan. J. Glob. Antimicrob. Resist. 23, 265–268. https://doi.org/10.1016/j.jgar.2020.09.010 (2020).
Takahashi, T. et al. Molecular characterisation of carbapenem-resistant Pseudomonas aeruginosa clinical isolates in Nepal. J. Glob. Antimicrob. Resist. 26, 279–284. https://doi.org/10.1016/j.jgar.2021.07.003 (2021).
Hamada, Y. et al. Three cases of IMP-type metallo-β-lactamase-producing Enterobacter cloacae bloodstream infection in Japan. J. Infect. Chemother. 19, 956–958. https://doi.org/10.1007/s10156-012-0520-6 (2013).
Tada, T. et al. PER-8, a novel extended-spectrum β-lactamase PER variant, from an Acinetobacter baumannii clinical isolate in Nepal. Antimicrob. Agents Chemother. 61, e02300-e2316. https://doi.org/10.1128/aac.02300-16 (2017).
Shrestha, S. et al. Molecular epidemiology of multidrug-resistant Acinetobacter baumannii isolates in a university hospital in Nepal reveals the emergence of a novel epidemic clonal lineage. Int. J. Antimicrob. Agents. 46, 526–531. https://doi.org/10.1016/j.ijantimicag.2015.07.012 (2015).
Tada, T., Miyoshi-Akiyama, T., Shimada, K., Shimojima, K. & Kirikae, T. Dissemination of 16S rRNA methylase ArmA-producing Acinetobacter baumannii and emergence of OXA-72 carbapenemase coproducers in Japan. Antimicrob. Agents Chemother. 58, 2916–2920. https://doi.org/10.1128/aac.01212-13 (2014).
Uechi, K. et al. An improved carbapenem inactivation method, CIMTrisII, for carbapenemase production by Gram negative pathogens. J. Med. Microbiol. 68, 124–131. https://doi.org/10.1099/jmm.0.000888 (2019).
Tada, T. et al. Dissemination of clonal complex 2 Acinetobacter baumannii strains co-producing carbapenemases and 16S rRNA methylase ArmA in Vietnam. BMC Infect. Dis. 15, 433. https://doi.org/10.1186/s12879-015-1171-x (2015).
Tada, T. et al. Molecular epidemiology of multidrug-resistant Acinetobacter baumannii isolates from hospitals in Myanmar. J. Glob. Antimicrob. Resist. 22, 122–125. https://doi.org/10.1016/j.jgar.2020.02.011 (2022).
Tzelepi, E. et al. Detection of extended-spectrum β-lactamases in clinical isolates of Enterobacter cloacae and Enterobacter aerogenes. J. Clin. Microbiol. 38, 542–546. https://doi.org/10.1128/jcm.38.2.542-546.2000 (2000).
Wachino, J. et al. Evaluation of a double-disk synergy test with a common metallo-β-lactamase inhibitor, mercaptoacetate, for detecting NDM-1-producing Enterobacteriaceae and Acinetobacter baumannii. Jpn. J. Infect. Dis. 67, 66–68. https://doi.org/10.7883/yoken.67.66 (2014).
Flores, E. A. et al. Detection of carbapenem resistant enterobacteriaceae from fomite surfaces. Am. J. Infect. Control. 49, 128–130. https://doi.org/10.1016/j.ajic.2020.05.023 (2021).
Kuwahara, K. et al. Evaluation of a new selective agar medium for detection of carbapenem-resistant Enterobacteriaceae. Diagn. Microbiol. Infect. Dis. 95, 114882. https://doi.org/10.1016/j.diagmicrobio.2019.114882 (2019).
Adler, A. et al. Laboratory and clinical evaluation of screening agar plates for detection of carbapenem-resistant Enterobacteriaceae from surveillance rectal swabs. J. Clin. Microbiol. 49, 2239–2242. https://doi.org/10.1128/jcm.02566-10 (2011).
Acknowledgements
The authors thank Mr. Koji Sato for technical assistants.
Funding
The research was supported by grants from Research Program on Emerging and Re-emerging Infectious Diseases from Japan Agency for Medical Research and Development (AMED) (Grant Number 22fk0108604h0702), Science and Technology Research Partnership for Sustainable Development (SATREPS) from AMED and Japan International Cooperation Agency (JICA) (JP20jm0110023h0001), JSPS KAKENHI (Grant Numbers 21K07031, 22K16379, 22K15460 and 20K16252) and a grant from the Institute for Fermentation (Grant Number Y-2021-1-002). SW received the endowed chair from Asahi Group Holdings, Ltd. SJ works for Kohjin Bio Co., Ltd.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: S.E. and T.K. Performed the experiments: S.E. Analyzed the data: S.E. and T.K. Wrote the manuscript: S.E. and T.K. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Endo, S., Tada, T., Oshiro, S. et al. Evaluation of antimicrobial susceptibility tests for Acinetobacter and Pseudomonas species using disks containing a high dose of meropenem. Sci Rep 14, 2749 (2024). https://doi.org/10.1038/s41598-024-52538-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52538-x
- Springer Nature Limited