Abstract
Several reports stated that erythema multiforme (EM) was associated with COVID-19 with detrimental outcomes in patients. However, since most of these are case reports, it is challenging to quantitively assess their associations. Therefore, our study aims to determine the prevalence of EM in the context of COVID-19. The study was designed as a retrospective cross-sectional hospital-based study of registered patients at the University of Florida Health Hospital. The ICD-10 codes for EM, COVID-19 infection, and COVID-19 vaccines were searched in the database. The odds ratio was calculated to assess the risk of EM after COVID-19 infection or vaccination. Our study included 43,547 patients with a history of COVID-19 infection, of whom 92 developed EM. Patients with COVID-19 infection were 6.68 times more likely to have EM than those without COVID-19 (P < 0.0001). Similarly, the risk of developing EM after COVID-19 vaccination was 2.7, significantly higher than the general population (P < 0.0001). The prevalence of EM following COVID-19 infection or vaccination significantly differs from the general population, highlighting the importance of monitoring patients for EM after COVID-19 infection and/or vaccination. It is imperative to disseminate awareness to clinicians and patients regarding the impact of COVID-19 on EM.
Similar content being viewed by others
Introduction
Erythema multiforme (EM) is an acute immune mediated mucocutaneous disease affecting the skin and mucous membranes. It presents a wide range of clinical manifestations varying from mild clinical features of the minor form of EM, which may only affect the skin and/or oral mucosa, to severe clinical features of the major form (Steven-Johnson syndrome) or toxic epidermal necrolysis that may involve other organs including the eyes and genital organs. EM is mostly detected in young adult patients as different forms of skin eruptions with or without oral ulcerations1.
Various etiological factors of EM were reported, with infection being the major cause. In 90% of patients, EM was detected following viral and fungal infections, while the most common were Herpes simplex virus (HSV) (> 80% of cases), followed by Epstein–Barr virus (EBV) and Mycoplasma pneumoniae. Furthermore, Drugs were reported as a triggering factor for EM including antibiotics, non-steroidal anti-inflammatory drugs, and anticonvulsants. EM may be detected as an adverse drug reaction after vaccination, which was reported following COVID-19 vaccines2,3.
The prognosis of EM differs between patients due to the different clinical forms of EM, ranging from 2–3 weeks for the minor form to 4–6 weeks for the major form mentioned earlier. Treatment of EM includes topical and systemic steroids, antihistamines, and analgesics. If the condition is caused by an underlying infection or medication, those underlying causes will need to be identified and treated as well3,4,5.
COVID-19 is a global pandemic that emerged in late 2019. The respiratory illness caused by the novel coronavirus (SARS-CoV-2) has been associated with various other symptoms, including oral and dermatologic diseases6,7,8,9. Although EM can be triggered by numerous factors, including viral infections, its association with COVID-19 has become a topic of interest in recent years10. The effect of COVID-19 on the health of the oral cavity can be primarily affected by the patient's immune system and medication prescribed, as well as the pathogenesis of the virus11,12. The oral cavity was reported as a perfect environment for the invasion of the SARS-CoV-2 virus13. This virus has an affinity to the angiotensin-converting enzyme 2 receptors located on the oral mucous membranes, salivary glands, and the respiratory tract. To our knowledge, this the first large hospital population-based study, investigating the prevalence and odds ratio of EM after COVID-19 infection or vaccination.
Materials and methods
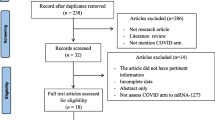
Acquisition of the data
A retrospective cross-sectional study was performed with a focus on the patients registered at the University of Florida Health and Shands Hospital from January 2020 to December 2022. Using the Integrated Data Repository (IDR) i2b2 platform, we extracted the data on COVID-19 (ICD 10-U07.1), EM (ICD 10-L51), and EM after COVID-19 vaccination according to the tenth edition of the International Classification of Diseases (ICD-10). The diagnosis of COVID-19 was confirmed by PCR, while the diagnosis of EM was mainly based on clinical and histopathological features.
We measured the onset of EM within 6 weeks after the diagnosis of COVID-19 infection or receiving COVID-19 vaccination. Cases with a history of exposure to certain triggers of EM were excluded from the current study including HSV (types 1 and 2), EBV, cytomegalovirus, mycoplasma pneumoniae and other triggering infections. Vaccines reported to trigger EM were excluded from the current study including the vaccines of herpes zoster, influenza hepatitis B vaccine, and Measles, Mumps, Rubella Vaccine. The study was limited to the de-identified data, thus not requiring IRB approval for human research.
Statistical analysis
The patients were divided into six groups; total hospital population, patients with COVID-19 infection, patients with EM disease, patients who received any of the following types of COVID-19 vaccine (AstraZeneca, Janssen (J&J), Novavax, Moderna, and Pfizer), patients with COVID-19 infection and developed EM after the COVID-19 infection, and vaccination. Rates between groups were compared by the prevalence ratios and the odds ratio (OR) was measured. The 95% confidence interval (CI) and P-value for each OR will be tabulated. p < 0.05 is significant.
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations (Declaration of Helsinki). The ethical approval and informed consent were waived by Institutional Review Board of university of Florida (UF). Research conducted only using that de-identified data set has been determined by the UF-IRB to not meet the definition of human research, and thus does not require IRB approval.
Results
We identified 43,547 patients with confirmed COVID-19 infection, while 188,233 received COVID-19 vaccines. 92 cases had EM after COVID-19 infection, compared to 158 patients who developed EM after COVID-19 vaccination. The prevalence of EM occurrence in the COVID-19 group was 0.2%, whereas the prevalence of EM in the general population was 0.03% (CI 5.407–8.699) with P < 0.0001. People with COVID-19 infection were 6.68 times more likely to have EM than those without COVID-19. We found statistically significant differences in the prevalence of EM after COVID-19 across age groups and races (P < 0.0001) (Tables 1 and 2).
Our study detected different types of EM, including 49 patients with EM minor, 115 with Steven Johnson syndrome, 56 with toxic epidermal necrolysis, and 42 with a history of Stevens Johnson syndrome/toxic epidermal necrolysis overlap syndrome.
People who received a COVID-19 vaccination were 2.7 times more likely to develop EM. The prevalence of EM after COVID-19 vaccination was 0.08% compared to 0.03% in the general population (CI 2.234–3.317) with P < 0.0001. We found statistically significant differences in the prevalence of EM after COVID-19 vaccination across races (P < 0.0001) (Tables 1 and 3).
Discussion
In the present study, the prevalence of EM was significantly increased in the COVID-19 group. COVID-19 patients were 6.68 times to have EM than people who didn’t experience COVID-19. It is important to note that this study does not establish a causal relationship between COVID-19 and EM due to its cross-sectional design10. However, it is possible that COVID-19 may act as a trigger for EM, as previous studies have reported an association between the two14. For example, one study found that 28% of COVID-19 patients with acute palmoplantar skin lesions had EM-like lesions.
The majority of EM cases after COVID-19 in our study were detected in patients younger than 34 years old (63%) while 80% of them were children with age range between 1 and 17 years old. These findings align with a previous study, mentioned earlier, reporting that 28% of patients with COVID-19-related palmoplantar skin lesions having EM-like lesions fell into the age ranges between being 1 and 29 years old14. Another report by Bapst et al.15 reported the case of a 13-year-old child who developed EM as the initial sign of multisystem inflammatory syndrome after COVID-19 infection. Palaia et al.16 also described EM as an early symptom of COVID-19 in a 30-year-old woman without any other multi-organ symptoms despite being immunocompetent.
Our hospital established a comprehensive approach to diagnose EM through clinical evaluation of the characteristic features of EM including the target lesion with concentric rings and skin rashes. However, if it was difficult to clinically diagnose the case, skin biopsy was obtained to confirm the diagnosis based on histological features, including the presence of keratinocyte apoptosis. However, we acknowledge the potential challenges in differentiating EM from conditions like HSV oral lesions and mycoplasma-induced mucositis due to the similarity in presentation. To address this, a rigorous diagnostic process was used including the clinical assessment, histopathological examination and laboratory testing including PCR for HSV, mycoplasma, and others to confirm or exclude these specific etiologies.
The pathophysiological mechanism of EM after COVID-19 infection may be due to targeting the SARS-CoV-2 antigens in the skin by the lymphocytes inducing a hypersensitivity reaction with apoptosis of the epithelial cells similar to what was reported for EM associated with other infections17. Besides the viral cytopathic effect, it was reported that SARS-CoV-2can induce Type II and Type IV hypersensitivity reactions. The cytokine storm which refers to the release of cytokines from host cells was linked to COVID-19 infection. All these factors may explain the possible relationship between EM and COVID-1918,19.
The occurrence of EM following COVID-19 vaccination may indicate an adverse drug reaction. However, the causal relationship between the vaccine and EM has not yet been established. Nevertheless, it is not uncommon for medications to trigger this disease1,17. We observed a prevalence of EM after vaccination of 0.08% in our study, which was significantly higher than the general population (P < 0.0001). Although age does not seem to affect the occurrence of EM after vaccination, we found significant differences between different races. Interestingly, females reported a higher percentage of EM after COVID-19 infection as well as COVID-19 vaccination.
There have been reports of several cases of EM following COVID-19 vaccinations. A study reported three cases of EM occurring within two to four days after the first dose of the Pfizer-BioNTech COVID-19 vaccine20. The authors of the study suggested a possible association between the vaccine and the development of EM. Similarly, in another report, four patients developed oral and dermatologic lesions of EM after receiving the Pfizer- BNT162b2 vaccine, despite having no history of erythema-like or herpetic manifestations21. In addition, Kong et al. detected EM-like lesion after the second dose of mRNA-1273 (Moderna) COVID-19 vaccine22. Although there have been reports of EM after COVID-19 vaccination, the incidence appears to be very low, and the exact cause of this phenomenon is still being investigated20. Interestingly, Lavery et al. reported a recurrence of EM after BNT162b2 vaccination in a female patient who had already been affected by the disease in 201823. The patient had bilateral cutaneous erythematous plaques on the hands and feet without oral involvement.
COVID vaccination offers crucial relative risks and benefits. It significantly reduces the risk of severe COVID-19 illness, hospitalization, and death while presenting minimal risks compared to the disease itself. Vaccination remains a pivotal tool in curbing the pandemic's impact and safeguarding public health. We noticed that our study found a higher incidence of vaccine-induced EM compared to the available literature on case reports and small cohorts. However, we believe this is an important aspect of our findings, as it highlights a potential discrepancy between real-world data and previously reported cases. This raises the need for further investigation into the underlying mechanisms and risk factors, which can contribute to a more comprehensive understanding of vaccine side effects24,25.
We acknowledge that our patient cohort primarily consists of individuals who developed COVID-19 while hospitalized. This selection may not fully represent the broader community population where COVID-19 prevalence might differ. Our aim was to investigate and analyze the outcomes of COVID-19 cases within a hospital setting.
While the COVID-19 Vaccination campaign is progressing, the knowledge about the probable side effects is growing and their adverse events are new scopes in medicine. The exact mechanism by which the COVID-19 vaccine triggers EM is not yet fully understood. However, it is believed to be related to the immune response generated by the vaccine, which can result in the development of an immune-mediated skin reaction. Similar to other vaccines, the expression of an antigen on keratinocyte may cause T-cell activation. Vaccination stimulates the immune system and causes T cell polarization26,27. Furthermore, Sahin et al. reported that the BNT162b2 vaccine induced a coordinated humoral and cellular adaptive immunity28. Others suggest that the vaccine may trigger the reactivation of a previous infection or an underlying autoimmune disorder21,28.
The limitation of the study includes that the i2b2 IDR provides the total number of patients who meet the selected search criteria. In other words, the search outcome consists of the total number of patients with a certain disease rather than any individual patient data. In addition, certain drugs received by COVID-19 positive patients may trigger EM however, the i2b2 IDR provides the total number of patients who meet the selected criteria (the total number of positivity or negative cases for particular clinical/ laboratory parameters searched) rather than providing the medication received by each patient. Therefore, there is no way to know the drugs received by each patient during COVID-19 infection before the appearance of EM. Another limitation of our study is that the cross-sectional design can’t provide the true causality of the diseases. We acknowledge that there might be potential biases in data collection and reporting. So, further research is required to confirm our findings and explore the potential mechanisms behind the observed differences in EM incidence after COVID-19 vaccination.
In conclusion, EM is a skin condition that can be triggered by various factors such as infections, medications, and vaccines. There have been reports of EM occurring in patients after COVID-19 infection or vaccination, indicating that the virus may serve as a trigger for this condition or host immune reactions to the vaccination may lead to EM. respectively. Further research is necessary to establish the association between COVID-19 and EM and develop more effective treatment protocols. It is crucial for clinicians to be aware of the link between the two conditions, which can facilitate the diagnosis and management of both conditions. Early recognition of oral and dermatologic diseases linked to SARSCoV-2 infection by informed clinicians will allow the early detection of COVID-19 infection and/or timely intervention to prevent a serious sequela of both conditions.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Grünwald, P., Mockenhaupt, M., Panzer, R. & Emmert, S. Erythema multiforme, Stevens-Johnson syndrome/toxic epidermal necrolysis—Diagnosis and treatment. J. Dtsch. Dermatol. Ges. 18(6), 547–553. https://doi.org/10.1111/ddg.14118 (2020).
Rizo-Potau, D., Marti-Marti, I. & Fustà-Novell, X. Erythema multiforme. Med. Clin. 156(10), 533. https://doi.org/10.1016/j.medcli.2020.04.063 (2021).
Samim, F., Auluck, A., Zed, C. & Williams, P. M. Erythema multiforme: A review of epidemiology, pathogenesis, clinical features, and treatment. Dent. Clin. North Am. 57(4), 583–596. https://doi.org/10.1016/j.cden.2013.07.001 (2013).
Sola, C. A. & Beute, T. C. Erythema multiforme. J. Spec. Oper. Med. Fall 14(3), 90–92. https://doi.org/10.55460/bl7l-501p (2014).
Trayes, K. P., Love, G. & Studdiford, J. S. Erythema multiforme: Recognition and management. Am. Fam. Phys. 100(2), 82–88 (2019).
Erbaş, G. S. et al. COVID-19-related oral mucosa lesions among confirmed SARS-CoV-2 patients: A systematic review. Int. J. Dermatol. 61(1), 20–32. https://doi.org/10.1111/ijd.15889 (2022).
Martín Carreras-Presas, C., Amaro Sánchez, J., López-Sánchez, A. F., Jané-Salas, E. & Somacarrera Pérez, M. L. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. 27(Suppl 3), 710–712. https://doi.org/10.1111/odi.13382 (2021).
Daneshgaran, G., Dubin, D. P. & Gould, D. J. Cutaneous manifestations of COVID-19: An evidence-based review. Am. J. Clin. Dermatol. 21(5), 627–639. https://doi.org/10.1007/s40257-020-00558-4 (2020).
Saleh, W., Ata, F. & Elashry, M. M. Is COVID-19 infection triggering oral herpes zoster? A case report. SAGE Open Med. Case Rep. https://doi.org/10.1177/2050313X211065793 (2021).
Bennardo, L. et al. Erythema multiforme and COVID-19: What do we know?. Medicina https://doi.org/10.3390/medicina57080828 (2021).
Fidan, V., Koyuncu, H. & Akin, O. Oral lesions in Covid 19 positive patients. Am. J. Otolaryngol. 42(3), 102905. https://doi.org/10.1016/j.amjoto.2021.102905 (2021).
Saleh, W., Eman, S. H., Halim, G. A. & Ata, F. Oral lichen planus after COVID-19, a case report. Ann. Med. Surg. 72, 103051 (2021).
Xu, H. et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 12(1), 8. https://doi.org/10.1038/s41368-020-0074-x (2020).
Fernandez-Nieto, D. et al. Characterization of acute acral skin lesions in nonhospitalized patients: A case series of 132 patients during the COVID-19 outbreak. J. Am. Acad. Dermatol. 83(1), e61–e63. https://doi.org/10.1016/j.jaad.2020.04.093 (2020).
Bapst, T., Romano, F., Müller, M. & Rohr, M. Special dermatological presentation of paediatric multisystem inflammatory syndrome related to COVID-19: Erythema multiforme. BMJ Case Rep. https://doi.org/10.1136/bcr-2020-236986 (2020).
Palaia, G. et al. Erythema multiforme as early manifestation of COVID-19: A case report. Pathogens. 6, 654 (2022).
Sokumbi, O. & Wetter, D. A. Clinical features, diagnosis, and treatment of erythema multiforme: A review for the practicing dermatologist. Int. J. Dermatol. 51(8), 889–902. https://doi.org/10.1111/j.1365-4632.2011.05348.x (2012).
Icenogle, T. COVID-19: Infection or autoimmunity. Front. Immunol. 11, 2055. https://doi.org/10.3389/fimmu.2020.02055 (2020).
Dotan, A. The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmun. Rev. 20(4), 102792. https://doi.org/10.1016/j.autrev.2021.102792 (2021).
McMahon, D. E. et al. Cutaneous reactions reported after Moderna and Pfizer COVID-19 vaccination: A registry-based study of 414 cases. J. Am. Acad. Dermatol. 85(1), 46–55. https://doi.org/10.1016/j.jaad.2021.03.092 (2021).
Petruzzi, M., Galleggiante, S., Messina, S. & Della Vella, F. Oral erythema multiforme after Pfizer-BioNTech COVID-19 vaccination: A report of four cases. BMC Oral Health. 22(1), 90. https://doi.org/10.1186/s12903-022-02124-2 (2022).
Kong, J. et al. Bullous drug eruption after second dose of mRNA-1273 (Moderna) COVID-19 vaccine: Case report. J. Infect. Public Health. 14(10), 1392–1394. https://doi.org/10.1016/j.jiph.2021.06.021 (2021).
Lavery, M. J., Nawimana, S., Parslew, R. & Stewart, L. A flare of pre-existing erythema multiforme following BNT162b2 (Pfizer-BioNTech) COVID-19 vaccine. Clin. Exp. Dermatol. 7, 1325–1327 (2021).
Verdecia, M. et al. COVID-19 vaccine platforms: Delivering on a promise?. Hum. Vaccin. Immunother. 17(9), 2873–2893. https://doi.org/10.1080/21645515.2021.1911204 (2021).
Fathizadeh, H. et al. SARS-CoV-2 (Covid-19) vaccines structure, mechanisms and effectiveness: A review. Int. J. Biol. Macromol. 188, 740–750. https://doi.org/10.1016/j.ijbiomac.2021.08.076 (2021).
Loche, F., Schwarze, H. P., Thedenat, B., Carriere, M. & Bazex, J. Erythema multiforme associated with hepatitis B immunization. Clin. Exp. Dermatol. 25(2), 167–168. https://doi.org/10.1046/j.1365-2230.2000.00601.x (2000).
Egan, K. P., Wu, S., Wigdahl, B. & Jennings, S. R. Immunological control of herpes simplex virus infections. J. Neurovirol. 19(4), 328–345. https://doi.org/10.1007/s13365-013-0189-3 (2013).
Sahin, U. et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature. 595(7868), 572–577. https://doi.org/10.1038/s41586-021-03653-6 (2021).
Acknowledgements
We acknowledge the University of Florida Integrated Data Repository (IDR) and the UF Health Office of the Chief Data Officer for providing the analytic data set for this project.
Funding
The study was supported by the NIH/NIAMS grant (AR079693), which was awarded to S.C.
Author information
Authors and Affiliations
Contributions
W.S. and H.A.: conceptualization; methodology; resources; writing-original draft; review and editing. S.C.: methodology; resources; supervision, review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saleh, W., Alharbi, H. & Cha, S. Increased prevalence of erythema multiforme in patients with COVID-19 infection or vaccination. Sci Rep 14, 2801 (2024). https://doi.org/10.1038/s41598-024-52099-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52099-z
- Springer Nature Limited