Abstract
Exposure to air pollution is associated with many different health effects, especially cardiovascular and respiratory diseases. Additionally, highly significant links between exposure to air pollution and fertility, particularly male fertility was observed, however the studies regarding exposure to selected air pollutants and female fertility assessed by ovarian reserve are rare. Hence, the main aim of the study was to analyze relationship between exposure to ambient air pollution and ovarian reserve parameters among Polish women. The study population consisted of 511 women, who attended to infertility clinic because of diagnostic purposes. Participants filled in the questionnaire about social-demographic, lifestyle and health factors. Infertility specialists assessed ovarian parameters such as: antral follicle count (AFC) and concentration of hormones: Anti-Müllerian hormone (AMH), follicle stimulating hormone (FSH) and estradiol (E2). The air pollutants level (sulfur dioxide, nitrogen dioxide, carbon monoxide, ozone, particulate matters) were obtained via National Environmental Protection Inspectorate database. Significant negative association between PM2,5 and AMH (p = 0.032), as well as AFC (p = 0.044) was observed. Moreover, SO2 concentrations decrease AFC (p = 0.038). The results also suggest that PM10, PM2.5, SO2 exposure on antral follicle count may be more pronounced among women with a female factor infertility diagnosis. Additionally, exposure to PM2.5 and NOx on AFC and AMH was stronger among older women (> 35 years of age). To conclude, the present study found that air pollution could lead to decrease in follicle antral count and Anti-Müllerian hormone level, especially exposure to PM2,5 and SO2 thus the evidence suggest negative impact to ovarian reserve.
Similar content being viewed by others
Introduction
Currently ambient air pollution caused a serious environmental problem in many countries. The sources can be anthropogenic or natural. The pollutants of anthropogenic origin include: automotive industry, metallurgic industry and energy industry, whereas the natural sources include: volcanic eruptions, fires, biochemical processes, flash of lightening etc.1. Most of the studies regarding air pollution exposure are focused on monitoring of the air parameters such as: sulfur dioxide (SO2), nitrogen dioxide (NO2), carbon monoxide (CO), ozone (O3), particulate matters (PM2,5 and PM10). A components of particulate matters (PM) can be organic (e.g. dioxins, benzene, polycyclic aromatic hydrocarbons) or inorganic (e.g. heavy metals, chlorides, carbon) origins2. According to the new report by European Environment Agency (Air quality in Europe 2022 report) in 2020 96% of the urban population in European Union was exposed to PM levels exceeded guidelines by the World Health Organization3. In Poland air pollution caused a huge problem, according to the World Bank Group 36 of the 50 most polluted cities in the European Union are located in Poland. The particulate matters (PM2,5) are mostly responsible for air pollution in these cities4.
Air pollution exposure can be associated with many different health effects, especially: respiratory or cardiovascular system diseases5,6,7. Increasing number of studies and reviews suggest a negative impact of air pollution on human reproduction including male and female fertility. A lower X:Y sperm chromosome ratio among men and abnormal morphology (51,78%) was observed after air pollution exposure7. Additionally, air pollution exposure negatively affects: DNA fragmentation8,9, sperm aneuploidy10,11, sperm concentration and sperm motility8,12,13,14,15,16,17,18. In comparison to male populations, female exposure to ambient air pollution and reproductive outcomes are not frequently studied, especially female fertility is rarely assessed. In the review performed by Conforti et al.19, the significant linkage between air pollution and female reproductive outcomes such as: higher miscarriages rate20,21, risk of stillbirth22 was observed. Additionally, Zeng et al.23 reported that, chronic exposure to air pollution can lead to reduced odds of IVF pregnancy outcomes (biochemical and clinical pregnancy). The studies assessing the female fertility are scare. The first study which evaluate the environmental exposure to air pollution (PM2,5) and one of the ovarian reserve parameters, antral follicle count (AFC) was performed by Gaskins et al.24. The study shows that exposure to particulate matters (PM2,5) can lead to decrease ovarian reserve. Other studies examined the exposure to particulate matter (PM10 and PM2,5) found the negative association with Anti-Müllerian hormone25 and decrease in AMH ratio, defined as an observed-to-expected AMH based on age26. In the study performed by Feng et al. long–term (between January 2013 and December 2019) exposure to SO2 was associated with lower antral follicle count27. In animals the studies also confirm that air pollution exposure may decrease fertility. The studies on mice suggest that, exposure to fraction PM2,5 can reduce the level of Anti-Müllerian hormone (AMH)28. Other researchers reported that, exposure to PM2,5 can affects antral follicle count, pregnancy loss and birth weight29.
In comparison to previous research this study is the first which describe all parameters of ovarian reserve (AFC, FSH, E2, and AMH) and different air pollutants (SO2, NOx, CO, O3, PM2,5 and PM10) exposure. Thus this study aims to evaluate the relationship between air pollution exposure and ovarian reserve.
Materials and methods
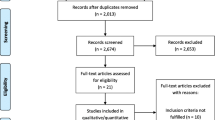
Study population
The study group include 511 women in reproductive age (25–39 years of age) recruited from fertility clinic. Only menstruating women with ovulatory cycles without co-existing chronic diseases (e.g., fragile X syndrome, adrenocortical insufficiency, abnormal karyotype) were included. Women with: three spontaneous miscarriages, more than three in vitro fertilization procedures, chemotherapy or radiotherapy of pelvis, premature ovarian failure, previous surgical treatment of the ovaries, polycystic ovary syndrome, cyst in the ovaries with endometrium, hyperprolactinemia, hypogonadotropic and hypogonadism were excluded. 700 woman fulfill the inclusion criteria and were suitable for the research, however only 511 (73%) gave the approval to participate in the research.
All the participants filled the questionnaire about socio-demographic characteristics, lifestyle factors (e.g. smoking, alcohol drinking, physical activity), health conditions (e.g. co-existing diseases), and occupational exposures.
This study was approved by the Nofer Institute of Occupational Medicine Bioethical Committee Board (ethics approval number: Resolution 23/2016). All experiments were performed in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects.
Analysis of ovarian reserve parameters
In the study ovarian reserve parameters were assessed such by antral follicular count (AFC), and reproductive hormones level (AMH, FSH, and estradiol).
The count of the antral follicle was assessed by ultrasonography (USG) according to Broekmans et al. criteria30. To assessment considered antral follicle with dimension measurement extent from 2 to 10 mm. All procedure was performed by trained gynecologist. The antral follicle count was treated for the analysis as the sum of antral follicle in both ovaries.
The blood samples were collected in early follicular phase cycle of spontaneous menstruation (2–4 day of cycle). The concentrations of the following hormones were assessed in serum: AMH (Anti-Müllerian hormone), FSH (follicle stimulating hormone) and estradiol (E2). The blood samples were centrifuged and a serum collected to polypropylene test tubes and stored in − 80 °C to time of analysis.
An enzyme linked immunosorbent method was used to analyzed the level of AMH using Gen-II ELISA kits (Beckman Coulter, Inc., USA) based on manufacturer instruction. The chemiluminescence method was used to measure levels of FSH and estradiol from ITROS ECi Immunodiagnostic System with MicroWell technology using commercially available VITROS Reagent Packs and the VITROS Calibrators which was used based on manufacturer instruction (Ortho-Clinical Diagnostics Johnson & Johnson, UK).
Air pollution data and exposure assessment
The air pollutants concentrations were obtain the National Environmental Protection Inspectorate (https://powietrze.gios.gov.pl/pjp/current). Daily levels (24-h average) of particulate matter < 10 μm in aerodynamic diameter (PM2.5), particulate matter > 10 μm in aerodynamic diameter (PM10), and sulfur dioxide (SO2) (reported as μg/m3) were collected. Additionally, the carbon monoxide CO (reported as μg/m3) and ozone (reported as μg/m3) measured in maximum 8-h average and nitrogen dioxide NOx (reported as μg/m3) -maximum 1-h average. Also meteorological factors such as temperature, atmospheric pressure, humidity, wind direction were collected.
For each pollutant, the average value for the 6 months which address the period of developmental stage from primary follicle to antral follicle, nearest monitoring sites was assigned to the women according to their ZIP code of residence.
Statistical methods
Descriptive statistics were calculated for subjects grouped by demographic characteristics, along with the layout of examined air pollutants, and AMH, E2 and FSH levels and AFC. Multiple least squares linear regression models were used to quantify the relationship of air pollution exposure (explanatory variables) with AFC and the concentrations of AMH, E2 and FSH as dependent variables. Multivariate regression models was used to explore an association between air pollutants levels, reproductive hormone concentrations and AFC. Two models were constructed. The first model was adjusted for following variables: BMI (kg/m2), age (years), smoking (no/yes), initial infertility diagnosis (male factor; female factor; unexplained) and the second model for age, BMI, smoking, infertility diagnosis, duration of infertility (1–3 years; 3–5 years; > 5 years); alcohol consumption (none or < 1 drink/week; 1–3 drinks /week; everyday). The covariates in the model were included on biological and statistical consideration. The air pollutants in the model were treated as the categorical variable (first to 25th percentile value, second-greater than the 25th percentile value to the median, third greater than the median to 75th percentile value, while the fourth group consisted of values greater than the 75th percentile or continuous variable. Effect modification of the association between exposure to air pollution and ovarian reserve parameters by age, BMI, current smoking, infertility diagnosis, duration of infertility, all well-known predictors of ovarian reserve, by adding a cross-product term to the final multivariate model was tested. R statistical software was used for the analysis (version 4.2.2).
Ethics approval and consent to participate
The Bioethical Committee in Lodz, Poland, approved the study (Resolution no 23/2016). All participants obtained and signed written informed consents prior to enrollment.
Results
Participants’ characteristics
Characteristics of the study population were described in Table 1. The majority of participants had higher (75.34%, n = 385) or secondary (21.14%, n = 108) education, the mean age was 33.30 ± 3.69 years and mean BMI (body mass index) 23.18 ± 3.80 kg/m2. The women were mostly nonsmokers (92.17%, n = 471), and 55% (281) of study subjects announced that they do not drink alcohol or drink less than 1 drink per week whereas 224 (44%) declare drinking 1–3 drinks per week. The initial diagnosis of infertility during recruitment was: male factor (37.8%, n = 193), idiopathic infertility (31.1%, n = 159), endometriosis (13.7%, n = 70), ovarian factor (4.7%, n = 24) and tubal factor (10.2%, n = 52). The duration of couple’s infertility declared by study participant were: over 5 years (35.23%, n = 180), 3–5 years (29.55%, n = 151), 2–3 years (27.59%, n = 141) and 1–2 years (7.63%, n = 39).
Ovarian reserve parameters
Table 2 presents ovarian reserve parameters among study population. For AFC arithmetic mean (± SD) was 12.73 ± 8.94. Reproductive hormones levels were: 1.17 ± 1.46 (ng/ml) for Anti-Müllerian Hormone, 6.38 ± 2.18 (IU/l) for follicle stimulating hormone and 93.74 ± 16.63 (pg/ml) for estradiol. According to the guidelines the AFC, FSH was in normal range (range for AFC: more than 4 antral follicles in ovary and range for FSH: lower than 15 IU/l). Additionally, estradiol for follicular phase of cycle was in normal range (range for E2: 12,5–166 pg/ml), the same as AMH (range for AMH: lower than 1 ng/ml).
Ambient air pollution levels
The levels of ambient air pollution are presented in the Table 3. A geometric means were: 44.80 ± 18.21 µg/m3 (range: 12.31–88.12 µg/m3) for ozone, 38.98 ± 31.14 µg/m3 (range: 8.21–117.56 µg/m3) for PM10, 31.22 ± 21.12 µg/m3 (range: 9.21–90.12 µg/m3) for PM2,5, 41.56 ± 9.82 µg/m3 (range: 11.32–170.66 µg/m3) for SO2, 35.70 ± 24.60 µg/m3 (range: 1.45–174.89 µg/m3) for NOx and 0.48 ± 0.32 µg/m3 (range: 0.11–1.98 µg/m3) for CO. According to Regulation of the Minister of the Environment of August 24, 2012 on the levels of certain substances in the air, almost all levels of air pollution31 in the study were fulfilled (Ozone range: 120 µg/m3, PM10 range: 50 µg/m3, SO2 range: 125 µg/m3, NOx range: 30 µg/m3, CO range: 10,000 µg/m3). Only level of PM2,5 was run over (range: 20 µg/m3).
Parameters of ovarian reserve and exposure to air pollution
The Table 4 presented relationship between air pollution levels and parameters of ovarian reserve. The statistical model was adjusted for: age, BMI, smoking and infertility diagnosis. A significant associations between parameters of ovarian reserve and air pollution was observed in 4th quartile of exposure to PM2,5 for antral follicle count (AFC) (p = 0.044) and Anti-Müllerian Hormone (AMH) (p = 0.032) compared to the first quartile, when the exposure was treated as the categorical variable. Additionally, statistically significant relationship was found between SO2 concentration and antral follicle count (AFC) (p = 0.038). No association was found between estradiol (E2) and follicle stimulating hormone (FSH) and any examined air pollutants (PM2.5, PM10, SO2, CO, NOx, ozone) in quartiles of exposure. When the air pollution exposure was treated in the model as a continuous variable no association were found between any air pollutants and any examined ovarian reserve parameters (Table 4). When the model was adjusted additionally for duration of infertility and alcohol consumption only exposure to PM2,5 in 4th quartile was related to decrease in antral follicle count number (p = 0.045) and AMH concentration (p = 0.048) (Table 4). Other air pollutants (SO2, PM10, ozone, NOx, CO) were not significantly associated with ovarian reserve parameters.
The estimated effect of PM10, PM2.5, SO2 exposure on antral follicle count was stronger among women whose primary infertility diagnosis was attributable to a female cause compared to women with an unexplained or male factor diagnosis (p-for-interaction 0.04, 0.02, 0.04 respectively) (Table 5). Additionally the effect of exposure to PM2.5 and NOx was more pronounced among women > 35 years of age compared to women < 35 years old (p-for-interaction 0.01, 0.03 respectively). PM2.5 affect also AMH concentration among older women (p-for-interaction 0.03) (Table 5).
Discussion
According to our best knowledge this is one of first study which assessed ambient air pollution exposure and ovarian reserve in European population. Additionally, contrary to previous studies the ovarian reserve was examined in complex way based on different ovarian reserve parameters (AFC, AMH, FSH, and E2). Also different air pollutants levels were evaluated (ozone, PM10, PM2.5, SO2, NOx, CO). Negative association between exposure to PM2.5 and AMH levels and AFC were found. Additionally, exposure to SO2 in the 4th quartile of exposure compared to the first one decrease the AFC. The results also suggest that PM10, PM2.5, SO2 exposure on antral follicle count may be more pronounced among women with a female factor infertility diagnosis. Additionally, exposure to PM2.5 and NOx on AFC and AMH was stronger among older women (> 35 years of age).
Four epidemiological studies were performed to assess the air pollution exposure and ovarian reserve24,25,26,27. The first study was performed by Gaskins et al.24, the author observed significant negative relationship between exposure to PM2,5 and antral follicle count. The association of PM2.5 with antral follicle count was stronger among women with female factor infertility and abnormal menstrual cycles. The observed results are similar to our study regarding to PM2.5 exposure and more pronounced effect among female with female factor of infertility. Abareshi et al.25 observed inverse relationship between exposure to air pollution (PM1, PM2,5) and levels of Anti-Müllerian hormone (AMH). In the study, the author examined only particulate matters exposure (PM1, PM2,5 and PM10) in population of 67 women25. Another study performed in Korea found that exposure to PM10 and PM2,5 decrease ovarian reserve assessed only by AMH concentrations26 which is in line with our results. In the study by Feng et al.27 only the antral follicular count (AFC) and air pollution exposure were evaluated. In the study SO2 exposure was associated with lower antral follicle count27. Similar relationship was observed in our study however the duration of exposure was different than in our study. The study covered of long-term exposure to ambient air (from 2013 to 2019), whereas in our study for each pollutant, the average value for the 6 months which address the period of developmental stage from primary follicle to antral follicle was assessed. The study by Feng et al.27 evaluated only AFC, as the main parameter of ovarian reserve.
The study performed in animals demonstrated that exposure to PM may reduce the antral follicle count in mice29. Another study in mice found diminishing ovarian reserve32 after exposure to diesel exhaust. Furthermore, Zhou et al.33 observed ovarian dysfunction associated with chronic PM2,5 exposure (4 months). The causal relationship that links air pollution to ovarian reserve has yet to be elucidated. Prior reports have suggested that folliculogenesis can be impaired by the increased oxidative stress and cellular apoptosis induced by ambient air containing a range of pollutants34. ROS can damage the oocytes and can lead to negative impact on female reproduction35. In results oxidative stress (OS) can lead telomere dysfunction (DNA damage or aberrant telomere recombination) and caused miscarriages and infertility36. Basically, there are three ways how the environmental pollutants can impact ovarian function: by causing endocrine disrupting effect, by induction of oxidative stress and by causing epigenetic modification37. Thus according to study performed by Styszko et al.38, PM10 and PM2,5 fractions of aerosols shows high oxidative potential (OP) and also included metals in composition such as: K, Ca, Ti, V, Mn, Fe, Pb, Cu, Cr, Zn, Hg, Ni, some of these metals can as endocrine disrupting chemicals so via the impact on the hormone level the ovarian reserve can be diminished39. Hence, endocrine disruptors can alter hormone receptor binding and action, such as: mainly on the aryl hydrocarbon receptor (AHR), estrogen receptors (ERs) or androgen receptor (AR), which can lead directly on disturb ovarian functions40. The studies in mice suggest that aryl hydrocarbon receptor (AHR) can play a function in the formation primordial follicles and also regulation of antral follicle count41. Other study reported that the AHR can regulate follicle growth through change estradiol biosynthesis pathway factors. The study performed by Revelli et al., suggest that estrogens and progesterone lead in the intraovarian regulation of follicle growth42. According to study Walters et al., the androgen receptor can lead to follicular growth and follicle and ovulation development43.
In present study the ovarian reserve was assessed by specialist in gynaecological endocrinology and reproduction, which result in the reliable assessment of antral follicle count. Moreover this is the first study which assess all parameters of ovarian reserve such as: Anti-Müllerian Hormone (AMH), follicle-stimulating hormone (FSH) and antral follicle count (AFC). AFC has been well-established biomarker for reflecting ovarian reserve from the aspect of visualization44. Also AMH is a reliable predictor for reflecting ovarian reserve due to its invariability with cyclical menstrual cycles45 and is associated with follicular size46.
The levels of air pollution which were found in present study (Ozone mean: 44,8 µg/m3, PM10 mean: 38,98 µg/m3, PM2,5 mean: 31,22 µg/m3, SO2 mean: 41,56 µg/m3, NOx mean: 35,70 µg/m3, CO mean: 0,48 µg/m3) are comparable with Abareshi et al., the median IQR of PM2,5 (42,2 µg/m3) and PM10 (47,4 µg/m3) concentrations25. Kim et al. assessed PM10, PM2,5, SO2, CO and ozone, but only two pollutants were in similar range PM10 (46,7 µg/m3) and ozone (37,5 µg/m3), the level of PM2,5 (25,8 µg/m3) and SO2 (4,4 µg/m3) were lower, and one higher CO (62,1 µg/m3)26. In the study carried out by Gaskins et al. the level of PM2,5 was lower than in present study (9 µg/m3)24. In the China study only SO2 were similar (53 µg/m3) compared to our study. In case of PM10, PM2,5, CO and ozone the levels were higher (108 µg/m3, 61 µg/m3, 120 µg/m3, 120 µg/m3)27.
The study has several strengths such as: performing the study in one fertility center, biological samples were collected and analyzed using the same procedure. The qualified medical specialist (infertility specialist) was assessed ovarian reserve according to the same standardized protocol. All procedures were carried out at the 2–4 days of the cycle (beginning of follicular phase). Moreover all participants answered the same questionnaire about sociodemographic, lifestyle and medical risk factors thus, we allowed for controlling potential confounding factors in statistical model.
The study has also some limitations. First, the study was performed in fertility clinic, which may not lead to generalized the results directly to general population. Second,, air pollution was assessed based on the information about ZIP code of residence for each women and was linked to the nearest air monitoring station. This method may not constitute the actual levels of exposure because we are not staying all the time in our places of residents. More proper measurement would minimize such a potential measurement bias. Nevertheless this is the popular method used in epidemiological studies with big sample size, where the individual monitoring may be not comfortable for participants and expensive24,25,26,27,47,48,49.
Conclusions
In summary, we observed that the exposure to PM2,5 decrease antral follicle count and AMH concentration, whereas the SO2 exposure was also negatively related only to antral follicle count. The results rise of importance to reduce the potential risk of ambient air pollution exposure and suggest the need for more strict regulations and controls forced by appropriate law. Additionally, further studies involving general population and underlying the mechanism of adverse impact on ovarian reserve are needed.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable.
Change history
12 February 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-53558-3
References
Popescu, F. & Ionel, I. Anthropogenic air pollution sources. In Air Quality (ed. Kumar, A.) 1–22 (Sciyo, 2010).
Manisalidis, I., Stavripoulon, E., Stavropoulos, A. & Bezirtzoglou, E. Environmental and health impacts of air pollution: A review. Front. Public Health 8, 2296–2565. https://doi.org/10.3389/fpubh.2020.00014 (2020).
Report no. 05/2022.. Air quality in Europe 2022, doi: https://doi.org/10.2800/488115 Available from: https://www.eea.europa.eu/publications/air-quality-in-europe-2022 1977–8449 (2023)
Guerreiro, C., Ortiz, A., de Leeuw, F., Viana, M. Air quality 2018 - EEA report 12 2018. doi: https://doi.org/10.2800/777411. (2018)
Brunekreef, B. & Holgate, S. T. Air pollution and health. Lancet 360, 9341. https://doi.org/10.1016/S0140-6736(02)11274-8 (2002).
Cohen, A. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 10082. https://doi.org/10.1016/S0140-6736(17)30505-6 (2017).
Radwan, M. et al. Air pollution and human sperm sex ratio. Am. J. Mens Health. 12, 1557–9883. https://doi.org/10.1177/1557988317752608 (2018).
Selevan, S. et al. Semen quality and reproductive health of young Czech men exposed to seasonal air pollution. EHP 108, 9. https://doi.org/10.1289/ehp.00108887 (2000).
Rubes, J., Selevan, S. G., Sram, R. J., Evenson, D. P., Perreault, S. D. GSTM1 genotype influences the susceptibility of men to sperm DNA damage associated with exposure to air pollution, Mutat Res-Fund Mol Mech Mutagen. 625, 1–2. https://doi.org/10.1016/j.mrfmmm.2007.05.012 (2007)
Robbins, W. A., Rubes, J., Selevan, S. G. & Perreault, S. D. Air pollution and sperm aneuploidy in healthy young men. Int J Hyg Environ Health. 1, 125–131 (1999).
Jurewicz, J. et al. The relationship between exposure to air pollution and sperm disomy. Environ. Mol. Mutagen. 56, 50–59. https://doi.org/10.1002/em.21883 (2015).
Sokol, R. Z. et al. Exposure to environmental ozone alters semen quality. EHP 114, 3. https://doi.org/10.1289/ehp.8232 (2006).
Hansen, C. et al. The effect of ambient air pollution on sperm quality. EHP 118, 2. https://doi.org/10.1289/ehp.0901022 (2010).
Hammoud, A. et al. Decreased sperm motility is associated with air pollution in Salt Lake City. Fert. Steril. 93, 6. https://doi.org/10.1016/j.fertnstert.2008.12.089 (2010).
Zhou, N. et al. Air pollution and decreased semen quality: A comparative study of Chongqing urban and rural areas. Environ. Pollut. 187, 145–152. https://doi.org/10.1016/j.envpol.2013.12.030 (2014).
Wu, L. et al. Association between ambient particulate matter exposure and semen quality in Wuhan, China. Environ. Int. 98, 219–228. https://doi.org/10.1016/j.envint.2016.11.013 (2017).
Santi, D. et al. Sperm quality and environment: A retrospective, cohort study in a Northern province of Italy. Environ. Res. 150, 144–153. https://doi.org/10.1016/j.envres.2016.05.053 (2016).
Radwan, M. et al. Exposure to ambient air pollution-does it affect semen quality and the level of reproductive hormones?. Ann. Hum. Biol. 43, 1. https://doi.org/10.3109/03014460.2015.1013986 (2016).
Conforti, A. et al. Air pollution and female fertility: A systematic review of literature. Reprod. Biol. Endocrinol. 16, 117. https://doi.org/10.1186/s12958-018-0433-z (2018).
Perin, P., Maluf, M., Czeresnia, C. E., Januário, D. A. N. F. & Saldiva, P. H. N. Impact of short-term preconceptional exposure to particulate air pollution on treatment outcome in couples undergoing in vitro fertilization and embryo transfer (IVF/ET). J. Assist. Reprod. Genet. 27, 371–382. https://doi.org/10.1007/s10815-010-9419-2 (2010).
Green, R. et al. Residential exposure to traffic and spontaneous abortion. EHP 117, 12. https://doi.org/10.1289/ehp.0900943 (2009).
Faiz, A. S. et al. Ambient air pollution and the risk of stillbirth. Am. J. Epidemiol. 176, 4. https://doi.org/10.1093/aje/kws029 (2012).
Zeng, X., Jin, S., Chen, X. & Qiu, Y. Association between ambient air pollution and pregnancy outcomes in patients undergoing in vitro fertilization in Chengdu, China: A retrospective study. Environ. Res. 184, 109304. https://doi.org/10.1016/j.envres.2020.109304 (2020).
Gaskins, A. et al. Exposure to fine particulate matter and ovarian reserve among women from a fertility clinic. Epidemiology 30, 4. https://doi.org/10.1097/EDE.0000000000001029 (2019).
Abareshi, F. et al. Association of exposure to air pollution and green space with ovarian reserve hormones levels. Environ. Res. 184, 109342. https://doi.org/10.1016/j.envres.2020.109342 (2020).
Kim, H. et al. Outdoor air pollution and diminished ovarian reserve among infertile Korean women. Environ. Health Prev. Med. 26, 20. https://doi.org/10.1186/s12199-021-00942-4 (2021).
Feng, X. et al. Association of exposure to ambient air pollution with ovarian reserve among women in Shanxi province of north China. Environ. Pollut. 278, 116868. https://doi.org/10.1016/j.envpol.2021.116868 (2021).
Gai, H. F. et al. Ovarian damages produced by aerosolized fine particulate matter (PM2.5) pollution in mice: Possible protective medications and mechanisms. Chin. Med. J. 130, 12. https://doi.org/10.4103/0366-6999.207472 (2017).
Veras, M. et al. Chronic exposure to fine particulate matter emitted by traffic affects reproductive and fetal outcomes in mice. Environ. Res. 109, 5. https://doi.org/10.1016/j.envres.2009.03.006 (2009).
Broekmans, F. et al. The antral follicle count: Practical recommendations for better standardization. Fertil. Steril. 94(3), 1044–1051. https://doi.org/10.1016/j.fertnstert.2009.04.040 (2010).
[Regulation of the Minister of the Environment of August 24, 2012 on the levels of certain substances in the air. J. Laws 2021, item 845]. Polish
Ogliari, K. et al. Intrauterine exposure to diesel exhaust diminishes adult ovarian reserve. Fertil. Steril. 99, 6. https://doi.org/10.1016/j.fertnstert.2013.01.103 (2013).
Zhou, S. et al. Ovarian dysfunction induced by chronic whole-body PM2.5 exposure. Small 16, 2000845. https://doi.org/10.1002/smll.202000845 (2020).
Dechanet, C. et al. Effects of cigarette smoking on reproduction. Hum. Reprod. Update 17, 1. https://doi.org/10.1093/humupd/dmq033 (2010).
Agarwal, A., Gupta, S. & Sharma, R. K. Role of oxidative stress in female reproduction. Reprod. Biol. Endocrinol. 3, 28. https://doi.org/10.1186/1477-7827-3-28 (2005).
Keefe, D. & Lin, L. Telomeres and reproductive aging. Reprod. Fertil. Dev. 21, 10–14. https://doi.org/10.1071/RD08229 (2008).
Vabre, P. et al. Environmental pollutants, a possible etiology for premature ovarian insufficiency: A narrative review of animal and human data. Environ. Health 16, 37. https://doi.org/10.1186/s12940-017-0242-4 (2017).
Styszko, K. et al. Oxidative potential of PM10 and PM2.5 collected at high air pollution site related to chemical composition: Krakow case study. Air Qual. Atmos. Health 10, 1123–1137. https://doi.org/10.1007/s11869-017-0499-3 (2017).
Iavicoli, I., Fontana, L. & Bergamaschi, A. The effects of metals as endocrine disruptors. J. Toxicol. Environ. Health B 12, 3. https://doi.org/10.1080/10937400902902062 (2009).
Craig, Z. R., Wang, W. & Flaws, J. A. Endocrine-disrupting chemicals in ovarian function: Effects on steroidogenesis, metabolism and nuclear receptor signaling. Reproduction 142, 5. https://doi.org/10.1530/REP-11-0136 (2011).
Benedict, J. C., Lin, T. M., Loeffler, I. K., Peterson, R. E. & Flaws, J. A. Physiological role of the aryl hydrocarbon receptor in mouse ovary development. Toxicol. Sci. 56(2), 382–388. https://doi.org/10.1093/toxsci/56.2.382 (2000).
Revelli, A., Paahioni, D., Cassoni, P., Bussolati, G. & Massobrio, M. In situ hybridization study of messenger RNA for estrogen receptor and immunohistochemical detection of estrogen and progesterone receptors in the human ovary. Gynecol. Endocrinol. 10, 177–186. https://doi.org/10.3109/09513599609027986 (1996).
Waters, K. M., Safe, S. & Gaido, K. W. Differential gene expression in response to methoxychlor and estradiol through ERα, ERβ, and AR in reproductive tissues of female mice. Toxicol. Sci. 63, 1. https://doi.org/10.1093/toxsci/63.1.47 (2001).
Penzias, A. et al. Testing and interpreting measures of ovarian reserve: A committee opinion. Fertil. Steril. 6, 1151–1157. https://doi.org/10.1016/j.fertnstert.2020.09.134 (2020).
Kaya, C., Pabuccu, R. & Satiroglu, H. Serum antimüllerian hormone concentrations on day 3 of the in vitro fertilization stimulation cycle are predictive of the fertilization, implantation, and pregnancy in polycystic ovary syndrome patients undergoing assisted reproduction. Fertil. Steril. 94, 6. https://doi.org/10.1016/j.fertnstert.2009.12.002 (2010).
Andersen, C. Y. et al. Concentrations of AMH and inhibin-B in relation to follicular diameter in normal human small antral follicles. Hum. Reprod. 25, 5. https://doi.org/10.1093/humrep/deq019 (2010).
Yang, S. et al. Ambient air pollution the risk of stillbirth: A prospective birth cohort study in Wuhan, China. Inl. J. Hyg. Environ. Health 221, 3. https://doi.org/10.1016/j.ijheh.2018.01.014 (2018).
Smith, R. et al. Impacts of air pollution and noise on risk of preterm birth and stillbirth in London. Environ. Int. 134, 105290. https://doi.org/10.1016/j.envint.2019.105290 (2020).
Gaskins, A. J. et al. Time-varying exposure to air pollution and outcomes of in vitro fertilization among couples from a fertility clinic. EHP 127, 7. https://doi.org/10.1289/EHP4601 (2019).
Funding
This work was supported by “Exposure to widespread, environmental endocrine disrupting chemicals and ovarian reserve” supported by National Science Centre in Poland from grant no. UMO-2017/27/B/NZ7/01921.
Author information
Authors and Affiliations
Contributions
K.W. and J.J. were involved in data interpretation and drafting of the manuscript. Joanna Jurewicz was involved in study concept and design. M.R. and P.R. were responsible for ovarian reserve parameters assessment. A.K., D.S., K.P., were involved data interpretation. All authors provided substantial intellectual contributions and approved the final version of manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, the Anti-Müllerian hormone ‘(AMH)’ was misspelt as ‘(AHM)’. Full information regarding the correction made can be found in the Correction for this Article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wieczorek, K., Szczęsna, D., Radwan, M. et al. Exposure to air pollution and ovarian reserve parameters. Sci Rep 14, 461 (2024). https://doi.org/10.1038/s41598-023-50753-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50753-6
- Springer Nature Limited