Abstract
In the perioperative management of patients with glioblastoma (GBM), physicians face the question of whether and when to administer prophylactic or therapeutic anticoagulation (AC). In this study, we investigate the effects of the timing of postoperative heparinization on thromboembolic events (TE) and postoperative hemorrhage (bleeding, PH) as well as the interactions between the two in the context of an underlying intracerebral malignancy. For this retrospective data analysis, 222 patients who underwent surgery for grade IV glioblastoma, IDH-wildtype (2016 CNS WHO) between 01/01/2014 and 31/12/2019 were included. We followed up for 12 months. We assessed various biographical and clinical data for risk factors and focused on the connection between timepoint of AC and adverse events. Subgroup analyses were performed for pulmonary artery embolism (PE), deep vein thrombosis, and postoperative intracranial hemorrhage (PH) that either required surgical intervention or was controlled radiologically only. Statistical analysis was performed using Mann–Whitney U-Test, Chi-square test, Fisher’s exact test and univariate binomial logistic regression. p values below 0.05 were considered statistically significant. There was no significant association between prophylactic AC within 24 h and more frequent major bleeding (p = 0.350). AC in patients who developed major bleeding was regularly postponed by the physician/surgeon upon detection of the re-bleeding; therefore, patients with PH were anticoagulated significantly later (p = 0.034). The timing of anticoagulant administration did not differ significantly between patients who experienced a thromboembolic event and those who did not (p = 0.634). There was considerable overlap between the groups. Three of the six patients (50%) with PE had to be lysed or therapeutically anticoagulated and thereafter developed major bleeding (p < 0.001). Patients who experienced TE were more likely to die during hospitalization than those with major bleeding (p = 0.022 vs. p = 1.00). Prophylactic AC within 24 h after surgery does not result in more frequent bleeding. Our data suggests that postoperative intracranial hemorrhage is not caused by prophylactic AC but rather is a surgical complication or the result of antithrombotic therapy. However, thromboembolic events worsen patient outcomes far more than postoperative bleeding. The fact that bleeding may occur as a complication of life-saving lysis therapy in the setting of a thromboembolic event should be included in this cost–benefit consideration.
Similar content being viewed by others
Neurosurgical patients are at high risk for both thromboembolic events and postoperative intracranial hemorrhage1,2,3,4. This applies especially for patients’ undergoing glioma surgery. As a practitioner, one is caught between a rock and a hard place when it comes to the onset of prophylactic anticoagulation, for both adverse events impair patients’ outcomes significantly5,6,7. Risk factors for both bleeding and thromboembolic events have been largely examined. To prevent thromboembolism, prophylactic anticoagulation with low molecular weight heparin and its derivatives is standard in perioperative care6,7,8. There are various studies on whether or not to apply chemoprophylaxis or mechanical devices such as intermittent pneumatic compression boots in patients with intracranial pathologies9,10. Yet, there is scarce data on when to apply said prophylaxis11,12.
The rare cases in which pulmonary artery embolism occurs are associated with high mortality13. Causal therapy by means of therapeutic anticoagulation or lysis therapy is crucial here, but is used only very hesitantly due to the risk of bleeding. Due to its relatively scarce occurrence, there is no evident data on the application of full-dose anticoagulation in these cases.
The main objective of this study is to investigate the impact of the timing of prophylactic anticoagulation on serious adverse events, thereby contributing to a better understanding of the need for and risk of postoperative anticoagulation. In addition, the interaction between these two adverse events will be further elucidated. Subsequently, suggestions for conclusive prospective research should be developed in order to define precise guidelines.
Methods
The study was approved by the ethics committee of the Medical Faculty, University of Leipzig (No. 053/19-ek). The need for informed consent was waived by the ethics committee of the University of Leipzig. Apart from the patient selection, methodology has been described before8,11,12. I confirm that all methods were performed in accordance with the relevant guidelines and regulations.
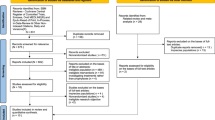
Patient selection
All patients who underwent surgery for grade IV glioblastoma, IDH-wildtype (according to the 2016 World Health Organization Classification of Tumors of the Central Nervous System) from 01/01/2014 to 31/12/2019 were identified using the digital patient database of the University Hospital of Leipzig. We started data analysis on 01/03/2019. All patient data were fully anonymized. Being an anonymous retrospective review with no personal data, informed consent was not required. Inclusion criteria were age above 18 years and conclusive documentation on the initiation of anticoagulation. 222 patients were included.
Diagnosis of intracranial bleeding and thromboembolism.
Magnetic resonance imaging (MRI) or alternatively 5 mm and 1.25 mm computed tomography (CT) scans were regularly performed within 24 h after surgery if contraindications to MRI were present. Patients displaying new neurological deficits or insufficient awakening after surgery were CT-scanned immediately.
Postoperative hemorrhage was defined as radiologically diagnosed intracranial residual blood. Re-Bleeding was defined independently by an experienced neuroradiologist and distinguished between residual blood and re-bleeding. This definition was reviewed again during data assessment for this study. We identified both major and minor bleedings to increase sensitivity for PH. Major bleeding was defined as bleeding that either required surgery or would have required surgery in a setting other than palliative. Minor bleeding was defined as bleeding that did not require surgery and was controlled radiologically only. Unless stated otherwise, the statistical evaluation focuses on major bleedings.
Thromboembolic events were defined as pulmonary artery embolism or deep vein thrombosis detected by either CT scan or duplex sonography. Diagnostic methods were only initiated if symptoms occurred.
In one case, pulmonary artery embolism was diagnosed on the basis of clinical and echocardiographic features (sudden onset of severe dyspnea, most severe right heart strain on echocardiography and the need for cardiopulmonary resuscitation). The patient died before any conclusive imaging was performed.
We also examined cases in which intracranial ischemia occurred. In all cases, the infarctions could be attributed to the access pathways or complications during resection. Therefore, they were not considered to be thromboembolic events.
Anticoagulation regimen
All cases admitted to our neurooncological center were discussed in a weekly, interdisciplinary tumor board, where the therapy regimen regarding surgical treatment or conservative procedure was decided based on international guidelines [EANO]. Patients were anticoagulated in accordance with national guidelines14,15, known independent risk factors, and pre-existing diseases, as well as body weight. The timing and dose as well as the choice of substance were decided according to the hospital’s guidelines and in interdisciplinary bedside discourse with intensive care and neurosurgical practitioners. The fact that anticoagulation did not follow a definite protocol resulted in the variety of timings and therapy regimens examined in this study. However, the common course of treatment and diagnosis can be described as follows:
Patients are not anticoagulated until CT or MR imaging of the head is obtained, which is routinely done on the first postoperative day (or within 24 h after surgery). CT scans are performed immediately following the onset of new neurological deficits. We begin prophylactic AC treatment in patients undergoing intracranial surgery on the first day after surgery, as long as postoperative CT or MR imaging do not show any signs of residual bleeding. Patients with postoperative or perioperative hemorrhage are mainly anticoagulated after two to five days following a repeat CT scan without any sign of a growing hemorrhage. In patients with a preoperative regimen of direct oral anticoagulants (DOAC) or vitamin K antagonists (VKA), therapy was interrupted for up to three weeks depending on indications during the period concerned. In these cases, heparin bridging was regularly performed and paused the day prior to surgery. Since 2014, a standard operating procedure has stated that hospitalized tumor patients should be considered for anticoagulation as long as there are no contraindications, in which case either mechanical prophylaxis or no prophylaxis at all should be applied. We have adapted this regimen and administer prophylactic anticoagulation with low-molecular-weight or unfractionated heparin to all eligible inpatients until the day before surgery.
Assessed data
Baseline data
Gender; smoking; diabetes; hypertension; atrial fibrillation; previous resection; paresis of lower limbs before surgery (defined according to JANDA ≤ 4); therapeutic anticoagulation in patient medication; platelet aggregation inhibitor in patient medication; American Society of Anesthesiologists (ASA)—score before surgery; age; body-mass-index (BMI).
Perioperative data
Necessity for blood products intraoperatively (fresh frozen plasma, platelet concentrates, or red cell concentrates); intraoperative positioning (abdominal vs back-positioning); extent of resection (biopsy vs. subtotal/grosstotal resection); usage of steroids at intensive care unit (ICU); administration of prophylactic anticoagulation before surgery; duration of surgery (measured in minutes); highest systolic blood pressure intraoperatively (measured in mmHg); lowest body temperature intraoperatively (measured in degree Celsius); intensive care unit (ICU) time after surgery (measured in hours).
Anticoagulation regimen
Timing of preoperative heparinization (measured in hours); timing of postoperative heparinization (measured in hours).
Outcome.
Postoperative intracranial hemmorrhage
Major bleeding: radiologically defined, requiring surgical revision; Minor bleeding: radiologically defined, not requiring surgical revision.
Thromboembolic events
Pulmonary artery embolism, deep vein thrombosis.
Death and functional status
Need for cardiopulmonary resuscitation (CPR); in-hospital mortality; mortality after 30 days, three, six and twelve months; Modified Rankin Scale (MRS) at discharge and after three months.
Statistical analysis
To describe the cohort, continuous parameters are presented as median, mean and with standard deviation; nominal parameters are displayed as percentage.
The population was dichotomously branched by the occurrence or nonoccurrence of adverse events (intracranial hemorrhage and thromboembolic event).
Continuous and ordinal parameters were evaluated with Mann–Whitney U-Test. Dichotomous parameters were analyzed using Fisher’s exact test. p values lower than 0.05 were considered statistically significant. Odd’s Ratios and their 95% confidence interval were calculated with univariate binomial logistic regression.
All analyses were computed using IBM SPSS Statistics software version 24 (IBM, Armonk, New York State, USA).
Results
Baseline data
There was no statistically significant difference in baseline and epidemiological data between both groups (Table 1).
Perioperative data
We found no significant difference in the distribution of maximum intraoperative systolic blood pressure and the incidence of major bleeding. Duration of surgery was significantly longer (U = 542.500, Z = -2.176, p = 0.028; OR = 1.009, 95% CI [1.003/1.014]) and intraoperative body temperature decreased in the hemorrhage group (U = 439.000, Z = − 2.732, p = 0.005; OR = 0.181, 95% CI [0.046 /0.711]).
Anticoagulation regimen
Patients who experienced major bleeding were anticoagulated significantly later (U = 561.500, Z = − 2.109, p = 0.034; OR = 1.052, 95% CI [1.018/1.086]).
Outcome
The occurrence of TE was correlated to PHrs (p = 0.002; OR = 20.800, 95% CI [4.013/107.813]) as was the intraoperative administration of blood products (p = 0.004; OR = 60.571; 95% CI [4.894/749.639]). While major bleeding was not more likely to lead to in-hospital death (p = 1.000; OR = 0.958; 95% CI [0.932/0.985]) and did not worsen functionality at discharge (p = 0.208; OR = 1.002; 95% CI [0.512/1.964]) or three months thereafter (p = 0.273, OR = 1.219; 95% CI [0.735/2.021]), it did result in longer ICU treatment (U = 143.500, Z = − 3.985, p < 0.001; OR = 1.009; 95% CI [1.004/1.014]) (Table 1).
Individual time course
Three patients developed major bleeding after life-saving lysis therapy or therapeutic AC due to pulmonary artery embolism and thereby circulatory deterioration. Only one patient (11,8%) suffered major bleeding after administration of prophylactic AC. This case is nonetheless exceptional, as intracranial hemorrhage occurred 18 days after first LMWH application. All other cases had not been given any kind of anticoagulation when hemorrhage occurred (Table 2).
Baseline data
Apart from BMI, which was higher in the thromboembolism group than in the comparison group (U = 403.000, Z = − 2.540, p = 0.009; OR = 1.182; 95% CI [1.022/1.366]), there was no other significant difference in epidemiologic and baseline data between both groups (Table 3).
Perioperative data
We found no significant difference in distribution of the operation time in the overall analysis (U = 610.500, Z = − 1.344, p = 0.183; OR = 1.006; 95% CI [1.000/1.012]). However, a significantly longer operative time was shown in the subgroup analysis of pulmonary artery emboli (U = 322.500; Z = − 2.078, p = 0.036; OR = 1.009; 95% CI [1.002/1.015]).
Anticoagulation regimen.
The timing of anticoagulation started postoperatively between the thromboembolism group and the comparison group did not differ significantly (U = 769.500, Z = − 0.486, p = 0.634; OR = 0.996, 95% CI [0.950/1.045]).
Outcome
In-hospital mortality in the TE group was increased (p = 0.022; OR = 13.933; 95% CI [2.236/86.829]) as was the need for cardiopulmonary resuscitation (p = < 0.001; OR = 63.600; 95% CI [8.634/468.491]). Functional capacity, which was measured by the modified Rankin scale, was lower in the TE group upon discharge from hospital (p = 0.047; OR = 1.929, 95% CI [1.126/3.299]) (Table 3).
Individual time course
Four of the eight patients (50%) who developed TE were anticoagulated prior to it. None of the above events occurred within the first week after surgery. The remaining four events, all of which were pulmonary artery emboli, occurred within three days after surgery and were not previously anticoagulated (Table 4).
When grouped into AC initiation prior to or later than 48 h, we found no significant development of either TE (p = 0.149) or PH (p = 0.365) (Table 5). There was no significant difference in outcome when comparing time point of AC and mRS overall.
Discussion
Limitations
The study is limited by the rare occurrence of adverse events in general. A total of 17 adverse events occurred in 222 patients, some of which showed overlap. Under given circumstances, we found little significant evidence. Furthermore, the validity of the result decreases as the observation period progresses due to the high number of dropouts. This is certainly due in part to the severity of the underlying disease, which has a high mortality rate and often results in a palliative approach far from university hospital care. Another limiting factor are the large interindividual differences of preoperative functional status and previous diseases which continue to exist despite the narrowly defined patient clientele. Moreover, in the retrospective analysis, no conclusion can be drawn about the causality of the relationships.
Early application of prophylactic anticoagulation has no impact on bleeding rates
We found no increase in occurrence of postoperative hemorrhage due to early application of prophylactic anticoagulation, which aligns with preliminary results11,12,16,17,18. Nonetheless, we found significant increase in major bleeding after administration of therapeutic AC or lysis therapy in vital indication (Table 2). The fact that prolonged duration of surgery and the need for intraoperative administration of blood products are related to an increased rate of bleeding events may seem trivial at first glance, as both may be consequences of intraoperative complications. However, these two factors may also be sensitizing for postoperative bleeding complications that occur later and thus play a warning role. Furthermore, this study supports the importance of perioperative temperature management, as hypothermia can lead to coagulopathy and thus increased bleeding19.
Prophylactic anticoagulation as a mean to prevent thromboembolic events
We found no evidence for a positive impact of early prophylactic AC on TE rates. Unfortunately, or luckily, early postoperative adverse events in glioma patients are so rare, that bigger patients’ collectives are needed to detect statistical differences here. Furthermore, we have not compared groups receiving AC with patients not receiving any thromboembolic prophylaxis, as existing data clearly indicates the necessity of AC in perioperative setting20,21,22,23
Adverse events and their impact on the overall outcome
The occurrence of TE as life-threatening events largely compromised patients’ immediate outcome (Table 3), whereas the occurrence of postoperative intracranial hemorrhage had no statistical impact on overall outcome (Table 1). As described before, we assume the occurrence of pulmonary embolism the more dreadful adverse event, compared to postoperative hemorrhage11,12. This has to be taken into account when defining AC regimen in elective glioma surgery.
Conclusion
We conclude that early postoperative use (i.e. within 24 h after surgery) of prophylactic anticoagulation is safe in patients undergoing glioma surgery. We found no evidence underlining that pausing prophylactic AC is indicated. Regarding therapeutic anticoagulation or lysis therapy in life-threatening events under CPR conditions, hemorrhage seems to be a very regular complication. This especially applies to the early occurrence of PE (within 48 h after surgery). Regarding future research areas, inhibition of factor XI, which is currently in clinical development, represents a promising approach to prophylaxis of thromboembolic events while ensuring hemostasis24,25. In addition, there are interesting developments in catheter-based therapy of pulmonary artery embolism, which may become particularly relevant for neurosurgery26.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Change history
06 May 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-60939-1
References
Cote, D. J. & Smith, T. R. Venous thromboembolism in brain tumor patients. J. Clin. Neurosci. 25, 13–18. https://doi.org/10.1016/j.jocn.2015.05.053 (2016).
Benjamin, E. J. et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation 135, e146–e603. https://doi.org/10.1161/CIR.0000000000000485 (2017).
Khaldi, A., Helo, N., Schneck, M. J. & Origitano, T. C. Venous thromboembolism: Deep venous thrombosis and pulmonary embolism in a neurosurgical population. J. Neurosurg. 114, 40–46. https://doi.org/10.3171/2010.8.JNS10332 (2011).
Cote, D. J., Dubois, H. M., Karhade, A. V. & Smith, T. R. Venous thromboembolism in patients undergoing craniotomy for brain tumors: A U.S. nationwide analysis. in Seminars Thrombosis Hemostasis 42, 870–6. https://doi.org/10.1055/s-0036-1592306 (2016).
Epstein, N. E. A review of the risks and benefits of differing prophylaxis regimens for the treatment of deep venous thrombosis and pulmonary embolism in neurosurgery. Surg. Neurol. 64, 295–301. https://doi.org/10.1016/j.surneu.2005.04.039 (2005).
Ganau, M. et al. Risk of deep vein thrombosis in neurosurgery: State of the art on prophylaxis protocols and best clinical practices. J. Clin. Neurosci. 45, 60–66. https://doi.org/10.1016/j.jocn.2017.08.008 (2017).
Moussa, W. M. M. & Mohamed, M. A. A. Prophylactic use of anticoagulation and hemodilution for the prevention of venous thromboembolic events following meningioma surgery. Clin. Neurol. Neurosurg. 144, 1–6. https://doi.org/10.1016/j.clineuro.2016.02.040 (2016).
Wilhelmy, F. et al. Tinzaparin vs. nadroparin safety and efficacy in neurosurgery. Neurol. Int. 13, 202–206. https://doi.org/10.3390/neurolint13020021 (2021).
CLOTS (Clots in Legs Or sTockings after Stroke) Trials Collaboration. Effect of intermittent pneumatic compression on disability, living circumstances, quality of life, and hospital costs after stroke: Secondary analyses from CLOTS 3, a randomised trial. Lancet Neurol. 13, 1186–1192. https://doi.org/10.1016/S1474-4422(14)70258-3 (2014).
Prell, J. et al. Reduced risk of venous thromboembolism with the use of intermittent pneumatic compression after craniotomy: A randomized controlled prospective study. J. Neurosurg. https://doi.org/10.3171/2017.9.JNS17533 (2018).
Hantsche, A. et al. Early prophylactic anticoagulation after subarachnoid hemorrhage decreases systemic ischemia and improves outcome. Clin. Neurol. Neurosurg. 207, 106809. https://doi.org/10.1016/j.clineuro.2021.106809 (2021).
Wilhelmy, F. et al. Perioperative anticoagulation in patients with intracranial meningioma: No increased risk of intracranial hemorrhage. PLoS One 15, e0238387. https://doi.org/10.1371/journal.pone.0238387 (2020).
Wang, X. et al. The risk of postoperative hemorrhage and efficacy of heparin for preventing deep vein thrombosis and pulmonary embolism in adult patients undergoing neurosurgery: A systematic review and meta-analysis. J. Investig. Med. 65, 1136–1146. https://doi.org/10.1136/jim-2016-000235 (2017).
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften. S3-Leitlinie: Prophylaxe der venösen Thrombembolie. https://www.awmf.org/leitlinien/detail/ll/003-001.html (2015).
Riess, H., Pabinger-Fasching, I., Alt-Epping, B., Demarmels Biasiutti, F., Langer, F. & Wörmann, B. Venöse thrombembolien (VTE) bei tumorpatienten. Available from: https://www.onkopedia.com/de/onkopedia/guidelines/venoese-thrombembolien-vte-bei-tumorpatienten/@@guideline/html/index.html (2019).
Gerlach, R. et al. Risk of postoperative hemorrhage after intracranial surgery after early nadroparin administration: Results of a prospective study. Neurosurgery 53, 1028–1034. https://doi.org/10.1227/01.neu.0000088565.15719.22 (2003).
Kleindienst, A. et al. Early antithrombotic prophylaxis with low molecular weight heparin in neurosurgery. Acta Neurochir. (Wien) 145, 1085–1090. https://doi.org/10.1007/s00701-003-0142-y (2003).
Raabe, A., Gerlach, R., Zimmermann, M. & Seifert, V. The risk of haemorrhage associated with early postoperative heparin administration after intracranial surgery. Acta Neurochir. (Wien) 143, 1–7. https://doi.org/10.1007/s007010170131 (2001).
Rajagopalan, S., Mascha, E., Na, J. & Sessler, D. I. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology 108, 71–77. https://doi.org/10.1097/01.anes.0000296719.73450.52 (2008).
Senders, J. T. et al. Venous thromboembolism and intracranial hemorrhage after craniotomy for primary malignant brain tumors: A national surgical quality improvement program analysis. J. Neurooncol. 136, 135–145. https://doi.org/10.1007/s11060-017-2631-5 (2018).
Senders, J. T. et al. Length of thromboprophylaxis in patients operated on for a high-grade glioma: A retrospective study. World Neurosurg 115, e723–e730. https://doi.org/10.1016/j.wneu.2018.04.151 (2018).
Smith, T. R. et al. Development of venous thromboembolism (VTE) in patients undergoing surgery for brain tumors: Results from a single center over a 10 year period. J. Clin. Neurosci. 22, 519–525. https://doi.org/10.1016/j.jocn.2014.10.003 (2015).
Cote, D. J., Dawood, H. Y. & Smith, T. R. Venous thromboembolism in patients with high-grade glioma. in Seminars Thrombosis Hemostasis 42, 877–83. https://doi.org/10.1055/s-0036-1592334 (2016)
Hsu, C., Hutt, E., Bloomfield, D. M., Gailani, D. & Weitz, J. I. Factor XI inhibition to uncouple thrombosis from hemostasis: JACC review topic of the week. J. Am. Coll. Cardiol. 78, 625–631. https://doi.org/10.1016/j.jacc.2021.06.010 (2021).
Fredenburgh, J. C. & Weitz, J. I. Factor XI as a target for new anticoagulants. Hamostaseologie 41, 104–110. https://doi.org/10.1055/a-1384-3715 (2021).
Javed, Q. A. & Sista, A. K. Endovascular therapy for acute severe pulmonary embolism. Int. J. Cardiovasc. Imaging 35, 1443–1452. https://doi.org/10.1007/s10554-019-01567-z (2019).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
F.W. and M.G. assessed data, analysed it and wrote the main manuscript. U.P. and J.K. edited and reviewed the manuscript. G.P. reviewed all radiological data. C.F. reviewed all histological data. R.O. submitted data on clinical course and outcome. J.M. and D.L. supervised the investigation. All Authors read and reviewed the manuscript and agreed to publication in its current form.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained errors. An older version of the Table 1 and 3 was erroneously uploaded with an incorrect bigger subgroup of patients. The correct group size is 222 patients. As the result of this error, column ‘Total’ was removed from the tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wilhelmy, F., Gaier, M., Planitzer, U. et al. Venous thromboembolism and intracranial hemorrhage in patients undergoing glioblastoma surgery. Sci Rep 13, 21679 (2023). https://doi.org/10.1038/s41598-023-48542-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48542-2
- Springer Nature Limited