Abstract
Pupil dilation response (PDR) has been proposed as a physiological marker of conscious access to a stimulus or its attributes, such as novelty. In a previous study on healthy volunteers, we adapted the auditory “local global” paradigm and showed that violations of global regularity elicited a PDR. Notably without instructions, this global effect was present only in participants who could consciously report violations of global regularities. In the present study, we used a similar approach in 24 non-communicating patients affected with a Disorder of Consciousness (DoC) and compared PDR to ERPs regarding diagnostic and prognostic performance. At the group level, global effect could not be detected in DoC patients. At the individual level, the only patient with a PDR global effect was in a MCS and recovered consciousness at 6 months. Contrasting the most regular trials to the most irregular ones improved PDR’s diagnostic and prognostic power in DoC patients. Pupillometry is a promising tool but requires several methodological improvements to enhance the signal-to-noise ratio and make it more robust for probing consciousness and cognition in DoC patients.
Similar content being viewed by others
Introduction
Probing residual cognition in patients with disorders of consciousness (DoC) is of tremendous importance to provide an accurate neurologic prognosis and to choose appropriate therapeutics1. These states include in particular the vegetative state (VS), also termed unresponsive wakefulness syndrome (UWS), and the minimally conscious state (MCS). To diagnose DoC with the best precision, a cumulative set of evidence converges to the necessity to complete a rich, rigorous and repeated behavioural examination with additional measures of brain activity2,3,4,5,6. In this perspective, developments of various indirect physiological measures of brain activity appear as potentially relevant tools7,8,9. One of these promising tracks of clinical research is pupillometry. Indeed, pupillometry is more easily accessible at the bedside, does not require complex data processing such as EEG-based measures, and could provide an objective physiological measure of residual cortically mediated behaviours10. At the acute phase, pupillary light reactivity is a well-described prognostic factor after severe brain damages11,12,13,14. More recently, pupil dilation response (PDR) has been used in intensive care unit (ICU) to monitor nociception15, communicate16 and demonstrate command-following16,17.
Previous studies conducted on healthy subjects suggested that PDR may be used as a somatic signature of cognitive effort18 and conscious access19,20,21,22,23. Conscious access refers to a cognitive stage of stimulus processing defined by the ability of the individual to self-report (verbally or not) stimulus presence or some of its attributes6,24,25. Pupil diameter increases before perceptual reports of ambiguous stimuli20,21, or along with the recognition stage when presented with ambiguous transforming stimuli22,26. PDR is also modulated by subjective image interpretation of brightness, motion or distance19,23,27,28. Moreover, PDR has been reliably identified as a physiological marker of standard vs deviant auditory stimulus discrimination in oddball paradigms with various manipulations of the stimulus probability, property, and intensity29,30.
In a previous study on healthy volunteers, we adapted to pupillometric recordings the auditory “local global” paradigm we previously conceived and designed for ERPs. In the “local global” paradigm31, two types of auditory regularities are crossed: an intra-trial regularity (local effect) and an inter-trial regularity (global effect). High-density scalp EEG, intracranial recordings and fMRI revealed that violation of the local regularity (local effect) was associated with a mismatch negativity (MMN) response originating from auditory cortices, whereas violation of global regularity (global effect) was associated with a P3b response originating from a widespread cortical network including prefrontal and parietal cortices, anterior cingulate cortex and hippocampal structures31,32. Crucially, in the passive attentive version of the local–global paradigm, a global effect (P3b) was present only in individuals who were spontaneously aware of the existence of a global regularity, and the global effect vanished when conscious resources were allocated to a concurrent rapid serial visual presentation task31.
In DoC patients, a global effect was observed only in conscious individuals (emergence from MCS) or in individuals who subsequently rapidly regained consciousness, suggesting that they were actually covertly conscious during the local–global task31,33,34,35. This notion of covert consciousness in behavioral unresponsive patients is often referred to the generic name of Cognitive-Motor-Dissociation (CMD) and may actually concern a significant fraction of acute DoC patients36,37.
It is essential to remind the predicted asymmetry prevailing between global effect and conscious state. We showed that individuals with a global effect consciously accessed to stimulus global regularity status (i.e., global deviant or global standard), and were therefore in a conscious state. This prediction was tested and confirmed in a large set of studies using various brain activity measures (EEG, MEG, iEEG, fMRI, PDR) combined with subjective reports31,32,38. So, as a clear consequence, if global effect is a specific measure of consciousness, its sensitivity is very limited given that it is not enough to be in a conscious state. Individuals also have to pay attention to the task, hear stimuli, be motivated, stay awake etc. In a recent study conducted on 236 DoC patients, 28% of patients had an ERP global effect33 (presence of global effect predicted behaviorally overt consciousness recovery in survivors with high specificity (Sp = 84%) and high positive predictive value (PPV = 80%) but with low sensitivity (Se = 35%) and low negative predictive value (NPV = 42%). Indeed, in the absence of any global effect, a patient may still be conscious but unable to understand the instructions, actively maintain attention, deploy working memory processes or may just be distracted.
We adapted the ”local–global” task to the slow dynamics of PDR and used it in two substantial sets of healthy volunteers with both an acoustic and a phonemic version of this task39. In a set of experiments, we could transpose ERPs results to PDR the following way : (i) we showed the existence of a generic PDR to any kind of auditory stimulus (local standard/deviant; global standard/deviant); (ii) this generic PDR was not affected by the local effect (i.e. similar PDR for local standard and local deviant trials); (iii) the global effect was associated to a significant PDR (i.e. larger PDR for global deviant than for global standard trials); (iv) this PDR global effect was associated to conscious access to violations of global regularity. This global effect was present in active versions of the task (i.e., subjects were explicitly instructed about global deviance and counted global deviant trials). In passive attentive versions of the task, global effect was present only in individuals who spontaneously and consciously discovered the existence of a global rule. All these results suggested that a global effect PDR should be a relevant sign of conscious processing.
In the present study, we aimed to test this key prediction,—as well as more generally the relevance of auditory PDR in DoC patients -, to improve both diagnosis and prognosis performance.
Materials and methods
Patients
From 27/08/2013 to 02/06/2015, 42 patients referred to the Neurology Intensive Care Unit of the Pitié-Salpêtrière University hospital (APHP, Sorbonne University, Paris, France) for an evaluation of consciousness were screened for participation in the study. All behavioural procedures performed in the present study were performed in accordance with the ethical standards of the Helsinki declaration (1964) and its later amendments and were approved by the local ethical committee (Comité de protection des personnes Ile de France I, #2013-A00106-39). An informed consent was obtained from all the participants’ legal guardians for both study participation and publication of identifying images in an online open-access publication.
Behavioral examination
Clinical examination was performed by an experienced neurologist and included the Coma Recovery Scale Revised (CRS-R)40 and the assessment of brainstem reflexes. Of particular interest here, the integrity of the pupillary light reflex of each eye was checked. Comatose patients with an arousal Coma Recovery Scale subscale inferior to 1 were excluded, as well as conscious patients (EMCS scoring). An auditory startle was defined as present if eyelid flutter or blink occurs immediately following an auditory stimulus on at least two trials, as previously described41. Crucially, a CRS-r score was performed immediately before pupillometric recordings.
Clinical outcome at 6 months and 1 year after the initial clinical evaluation was assessed using the Glasgow Outcome Scale-Extended (GOSE) and items of the CRS-R through a phone interview with a close relative or with patients’ physicians or were extracted from medical records.
Auditory paradigm and procedure
We used a version of the classical auditory ”local global” paradigm31 that was previously adapted to the slower temporal dynamic of pupil variations and validated in healthy volunteers39. This auditory paradigm crosses two types of auditory regularities (Fig. 1): an intra-trial regularity (local effect) and an inter-trial regularity (global effect). Repeated series of five sounds were presented via the laptop speakers. Each sound lasted 50 ms (SOA 150 ms) and could be either a low-pitched tone (A) or a high-pitched tone (B).
Auditory paradigm and pupillometry setup Reproduced with permission from39 (a) On each trial 5 sounds were presented. (b) Each of the four experimental blocks started with four identical series of sounds defining the global regularity, before delivering global standard (80%) or global deviant (20%) trials, that were also either local standard or local deviant trials. (c) Eyebrain mobile device including two independent infrared cameras centred on each pupil captures pupil images of each eye at a sampling rate of 120 Hz.
Four different series were used, the first two consisted of the same five sounds to conserve the local regularity (either AAAAA or BBBBB, called local standard (LS) stimulus); and the other two with the final sound swapped to break the local regularity (either AAAAB or BBBBA, called local deviant (LD) stimulus). The global regularity was defined by the repetition of one of the series in about 80% of the trials (global standard (GS) or frequent stimulus). This global regularity was broken in about 20% of the trials by the presentation of an alternative series with a different local regularity (global deviant (GD) or infrequent stimulus). Finally, we used four block types by experiment designed by the frequent sequence (global standard): type AAAAA (AAAAA frequent is LSGS / AAAAB infrequent is LDGD), type BBBBB (BBBBB frequent is LSGS /BBBBA infrequent is LDGD), type AAAAB (AAAAB frequent is LDGS / AAAAA infrequent is LSGD), type BBBBA (BBBBA frequent is LDGS / BBBBB infrequent is LSGD). Each block started with five identical series of the frequent type to define the global regularity. The number of infrequent stimuli per block was randomized between 4 and 7 and each one was followed by a frequent stimulus to remind the global regularity. The time interval between the two series was 3000 ms (instead of 1350–1650 ms in evoked potentials) in order to adapt to the slower dynamics of pupil dilation/constriction. Each block included 30 trials and lasted 90 s (in total the experience lasted 6 min).
Pupillometry: data acquisition and analysis
Pupillometric data were recorded binocularly at a 120 Hz sampling rate with the Mobile eyetracked (e(ye)BRAIN, www.eye-brain.com, France) that received CE marking approval for medical purposes. The acquisition was performed at the bedside, in intensive care units where the luminance and environment noise level were not controlled. Auditory stimuli were delivered by the MeyeParadigm software and raw data were stored and extracted by MeyeAnalysis software (www.eye-brain.com, France).
Raw pupil data were first pre-processed with the ET-remove-artifacts toolbox (https://github.com/EmotionCognitionLab/ET-remove-artifacts). Dilation speed outliers and eye blinks were detected and removed, and a linear interpolation was used to fill in gaps in the data. Then, these pre-processed pupil data were imported into the Brainstorm toolbox (available for download online under the GNU general public license (http://neuroimage.usc.edu/brainstorm)42). Data were filtered with a 10 Hz low pass filter, and epochs for each trial were extracted from 200 to 3000 ms after the beginning of the first sound. A trial was rejected when more than 25% of the data was interpolated. A patient dataset was excluded if it included more than 50% of rejected trials. All patients with a trial rejection rate superior to 25% (but inferior to 50%) were labeled as “poor quality” datasets. When the clinical examination revealed an asymmetric pupillary reflex, data from the most reactive eye were analysed. Otherwise, both eyes were analysed and we kept the best quality dataset (i.e., left or right eye dataset) for further analyses.
Event-related potentials
In complement to pupillometry, ERP were acquired during the auditory “local–global” paradigm in a different session at the bedside. ERPs were recorded at 250 Hz with a 256-electrodes geodesic sensor net (EGI R, Oregon, USA) referenced to the vertex. Trials were band-pass filtered (0.5–45 Hz), then segmented in epochs ranging from − 200 to + 1.344 ms from the first sound onset. Electrodes with voltages exceeding 100 µV in more than 50% of the epochs were removed. Moreover, voltage variance was computed across all correct electrodes. Electrodes with a voltage variance Z-score higher than four were removed. This process was repeated four times. Bad electrodes were interpolated using a spline method. Epochs were labeled as bad and discarded when voltage exceeded 100 µV in more than 10% of electrodes. Moreover, voltage variance was computed across all correct epochs, and epochs with a Z-score larger than four were removed. This process was also repeated four times. The remaining stimulus-locked epochs were averaged and digitally transformed to an average reference. An 800 ms baseline correction (before the onset of the fifth sound of the trial) was applied. EEG recordings had to satisfy the following two criteria to be considered of good quality: they should include a minimum of 75% valid channels and 30% of valid epochs, otherwise they were considered to be of “poor quality”. Preprocessing was implemented using MNE Python environment. Similarly to pupillometric recordings, a CRS-R was scored immediately before EEG acquisition.
Statistics
Population characteristics
Population characteristics (age, sex, time since brain injury, etiology, medication affecting pupil size) between VS/UWS and MCS were compared using a Mann–Whitney-U for continuous data, and the Fisher exact test for categorical variables as appropriate.
Generic PDR to sounds
We analysed the variation of the pupil diameter in a time window of interest starting with the beginning of the baseline window and ending with the trial (− 500–3000 ms). For each participant, LSGS trials were compared to the mean baseline (− 500–0 ms before first sound onset) with a sample-by-sample Student t-test corrected for multiple comparisons with the false discovery rate (FDR) in time (p ≤ 0.05).
Regularity violations of PDR effects
Responses to the violation of auditory regularity were studied at 3 levels: (i) the local effect was defined as the PDR difference between local deviant (LDGD and LDGS) and local standard trials (LSGS and LSGD), (ii) the global effect was defined as the PDR difference between global deviant (GDLS and GDLD) and global standard trials (GSLD and GSLS), (iii) the “maximal violation effect” (MVE) was defined by the PDR difference between trials that were both global and local deviant (LDGD) and trials that were both local and global standard (LSGS).
In each trial, the average pupil diameter computed from the baseline window was subtracted from all data points. For each participant, we computed the mean PDR for each condition. For the group analysis, we then performed paired t-tests at each time point (≤ p 0.05 after correction in time for multiple comparisons with the FDR). To compute single-participant statistics, single-trial data were compared using a sample-by-sample Student t-test.
ERPs
For individual subject statistics, unpaired Welch’s tests were performed for each time sample. An effect was considered significant if it satisfied the following triple-threshold criterion p < 0.05 on a minimum of five consecutive samples (20 ms), on a minimum of 10 contiguous electrodes,during the expected time window of the corresponding ERP effect. For the local effect, an ERP was expected from 100 ms after the first sound onset to the end of epochs, whereas the time window ranged from 200 ms to end of epoch for the global effect31.
Results
Patients’ characteristics
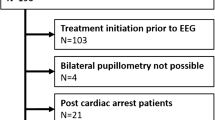
Among the 42 DoC patients enrolled for the study, 7 were excluded because they were in a comatose state, and one because he was conscious but with limited interaction capabilities due to a severe Guillain-Barré syndrome that involved cranial nerves with no pupillary response to noise and a weak pupillary light reflex (EMCS scoring with recovery of functional communication). Ten additional patients were rejected because of bad pupillometric data quality (i.e., rejection of more than 75% of the trials, because of too many artefacts). The final sample consisted of 24 patients (12 females; median age 43 years (IQR: 28–56)). Ten patients were in the VS/UWS group (median CRS-R 5, range 3–7) and 14 in the MCS group (median CRS-R range 7–18). Neurological examination confirmed the presence of pupillary light reflex in both eyes of each of these patients. Demographic and clinical findings (reported in Table 1) did not differ between the two groups.
Data quality
Median number of rejected trials was 17% (IQR: 7–25%, see Supplementary material Table S1) and did not differ between MCS and VS patients (Mann–Whitney-U p = 0.2). Six patients (2 in a VS/UWS and 4 in a MCS) for which trials rejection rate was > 25% and < 75% were labeled as “poor quality pupillometry datasets”. ERP data were acquired with a median time of 1 day before the pupillometry (4 ERP datasets were acquired either the same day as pupillometry (N = 4), or before pupillometry (N = 13, min = 4 days) or after (N = 4, max = 5 days). ERPs were not available in one patient and did not meet data quality criterion (see M&M) because of too many artefacts due to agitation in one other patient, and 9 additional patients (3 VS and 6 MCS) were labeled as “poor quality EEG datasets “(i.e., automatic voltage rejection in more than 10% of electrodes in more than 70% of epochs).
A non-specific generic auditory PDR was present in most patients
We first tested a non-specific generic PDR to auditory stimuli by computing the mean PDR in LSGS condition and testing PDR amplitude against baseline (t-test statistics significant at FDR corrected p-value ≤ 0.05; see M&M). At the group-level this generic and non-specific auditory PDR was present both in patients in a MCS and in patients in a VS/UWS (see Fig. 2). Baseline corrected auditory PDR did not differ significantly between MCS and VS/UWS patients (t-test statistics FDR corrected), although mean PDR was visually larger for the VS/UWS group than for the MCS group. We then ran the same analysis at the individual level: a generic auditory PDR was found significant in all patients (see “Sound” PDR column in Table 2), except for one VS/UWS patient and one MCS patient (note however that those patients had auditory ERP responses, see below).
A non-specific pupil dilation response to sounds was observed both in the MCS and in the VS/UWS patients and did not differ between the two groups. Grand averages of pupil diameter (in pixels) are plotted over time (in seconds) in MCS (n = 14) and VS/UWS patients (n = 10). Grey dotted lines index first sound onset and fifth sound offset respectively. Temporal windows in which the pupil dilatation is significant from baseline are marked in with horizontal blue (MCS) and orange (VS/UWS) lines.
Pupil dilation response (PDR) to violations of auditory regularities
At the group-level, we did not find significant local or global PDR effects, both in the whole population of patients and within each MCS and VS/UWS groups (t-test statistics significant at FDR corrected p-value, all p-values > 0.05, Fig. 3). Note that in VS/UWS patients although mean PDR was visually larger for the standard trials than for the deviant trials, this difference did not reach significance. In order to maximize the sensitivity of PDR, we finally contrasted the two maximally different conditions: LDGD vs LSGS trials. At the group level a significantly larger pupil dilation was observed after LDGD trials than after LSGS trials in MCS patients (FDR corrected p < 0.05; see Fig. 3 bottom panels). In contrast this effect was absent in VS/UWS patients. Besides, the PDR LDGD-LSGS difference was larger in MCS patients compared to VS/UWS patients during the 0.7–1.7 s time window interval (FDR corrected p < 0.05).
Local, global and maximal violation PDR effects for MCS and VS/UWS groups of DoC patients. Grand averages of pupil diameter (in pixels) are plotted over time (in seconds) in MCS (n = 14) and VS/UWS patients (n = 10) in an oddball paradigm. While the event-related pupil response was undistinguishable between LSGS (green curves) and LDGD (red curves) trials in the VS/UWS group, a significant (black horizontal segments) pupil dilation was observed in response to deviant trials in the MCS group. To distinguish conscious processing of inter-trials global regularity from non-conscious processing of intra-trials local regularity we contrast local standard trials to local deviant trials and global standard trials to global deviant trials and found no global or local effect in both groups. Grey dotted lines index first sound onset and fifth sound offset respectively.
At the individual level, we followed the same approach. All but 2 patients showed a generic auditory PDR effect. As a quality check, these two patients did not show any significant local, global or LDGD/LSGS effects. No patient had a significant local effect, one patient showed a trend of a local effect (0.05 < p < 0.1; MCS patient #13) and did not regain consciousness. Only one patient showed a PDR global effect (MCS patient #24, Fig. 4, see Table 2), and another patient also in a MCS showed a trend of a global effect (0.05 < p < 0.1; MCS patient #18). Both patients regained consciousness at 6 months.
In MCS patient n°24 while the event-related pupil response was undistinguishable between local standard (green curves) and local deviant (red curves) trials, a global effect was observed: a significant sustained (black horizontal segment) pupil dilation was observed in response to global deviant trials. Grey dotted lines index first sound onset and fifth sound offset respectively. This patient regained consciousness 6 months later.
Finally, the [LSGS vs LDGD] contrast revealed a significant effect in 4 MCS patients and in 1 VS/UWS patient (see Table 2). Two additional MCS patients showed a trend for this effect (0.05 < p < 0.1). Note however that presence of [LSGS vs LDGD] effect (significant or with a trend) did not differ between MCS and VS/UWS patients in our small sample of patients (Fisher exact p = 0.17; sensibility to discriminate MCS from VS/UWS 43% (18–71); specificity 90% (56–100); PPV 86% (46–98); NPV 53% (41–65)).
Outcome data was available for 23/24 patients. Generic PDR effect to sounds was much too ubiquitous to be associated with any significant predictive value (p = 1). PDR Local (N = 1) and global (N = 2) effects were too rare to be correlated with any outcome in this limited sample of patients. Notably, the [LSGS vs LDGD] PDR effect showed a higher performance: 4/7 patients with a significant effect or a trend of an effect (p = 0.1) regained consciousness, versus 3/16 for patients who lacked this effect (Fisher exact p = 0.1; sensibility to predict recovery of consciousness: 57% (18–91), specificity 81% (54–96), PPV 57% (29–82), NPV 81% (64–91)).
Event-related potentials
ERP results were available for 8/10 patients in a VS/UWS, and for all (14/14) patients in a MCS. Early cortical responses to sounds were observed in all patients (see “Sound” ERP column in Table 2), whereas a behavioural auditory startle was absent in 2/8 VS/UWS patients, and in 2/14 MCS patients (Table 2).
At the group level, a significant local effect and a significant LSGS vs LDGD effect were observed in the whole population of patients, as well as in MCS and in the VS/UWS groups (t-test statistics significant at FDR corrected p-value all p-values < 0.05). In contrast, a global effect was not observed, neither in the whole population of patients nor in MCS and VS/UWS groups (t-test statistics significant at FDR corrected p-value all p-values > 0.05).
At the individual level, a local effect was found significant in 10/14 MCS patients and in 5/8 VS/UWS patients (Fisher exact p = 0.4; sensibility 71% (42–92), specificity 38% (9–76); PPV: 67% (52–79); NPV: 43% (18–72)). Among these patients, 5 regained consciousness (Fisher exact p = 0.7, sensibility to predict recovery of consciousness 71% (29–96); specificity 36% (13–65); PPV 36 (23–51) %; NPV 71% (39–91)).
A global effect was found in 5 patients who were all in a MCS (Fisher exact p = 0.1; sensibility to discriminate MCS from VS/UWS 36% with 95% CI (13–65), specificity 100% (63–100), PPV 100%, NPV 43% (38–57)). Among the 5 patients with a global effect, 3 recovered consciousness at 6 months.
An ERP [LSGS vs LDGD] effect was found in 5/8 VS/UWS patients and in 11/14 MCS patients (Fisher exact p = 0.6; sensibility 79% (49–95), specificity 38% (9–76); PPV: 69% (55–80); NPV: 50% (21–79)). Among these patients, 5 regained consciousness (sensibility to predict recovery of consciousness (Fisher exact p = 0.6 ; 86% (42–79); specificity 36% (13–65); PPV 40 (29–52) %; NPV 83% (42–97)).
The two patients with a significant or a trend of a PDR global effect also had an EEG global effect. Among the patients with a significant or a trend [LSGS vs LDGD] PDR effect 5/6 patients also have an ERP [LSGS vs LDGD] effect. The presence of an ERP and a PDR global effect were not statically correlated (Fischer exact p = 0.4). The presence of an ERP and a PDR [LSGS vs LDGD] effects were not statically correlated either (Fischer exact p = 0.6).
Discussion
In this study, we explored PDR in a population of DoC patients exposed to the local global auditory paradigm. At the group level, we found a generic PDR to sounds that was similar for MCS and VS/UWS groups, and we did not observe any significant local effect. These two results are in line with our previous report using the very same paradigm in healthy volunteers39. The preservation of generic auditory PDR response in VS/UWS patients is consistent with the previously reported early phasic pupillary dilation response corresponding to the automatic low-level processing of stimuli18. Note however that contrarily to our previous finding in conscious healthy volunteers39 we could not find a PDR global effect in groups of patients (neither across all patients nor in MCS or in VS/UWS groups). This negative result may stem from at least two factors that are not mutually exclusive. First, the global effect requires working memory resources and attentional engagement31, and is therefore very demanding cognitively. Our recent survey33 indeed confirmed that most patients showing a preserved ERP global effect were probably conscious (i.e., including patients with cognitive-motor dissociation36 during recording. Second, part of this negative result may also stem from signal-to-noise ratio issue, and in particular from poor data quality (i.e., resulting in numerous rejected trials), and the slow dynamics of PDR that forced us to record a lower number of trials, as compared with ERPs. Future methodological developments may improve this power issue, such as using deconvolution techniques using a fast event-related PDR paradigm as in fMRI43. This signal-to-noise ratio issue is made even more important when considering the difficult conditions of recording the ICU (i.e. including a lot of irrelevant auditory and light stimulation), in patients under various pharmacological treatments that may affect pupil dilation, and who frequently show eye blinks, head movements and other sources of artefacts. Finally, the head-mounted device used in the present study may have induced more artefacts than other eye-tracker devices.
Confronted to these limitations, we then defined a “maximal violation effect” by contrasting LSGS to LDGD trials in order to maximize differences in cognitive processing between, on the one hand, trials that respected both intra and inter-trial regularities, and on the other hand trials that violated both intra and inter-trial regularities. We could then detect a significant [LSGS vs LDGD] PDR effect for the group of MCS patients. Of particular interest, this effect was absent in the group of VS/UWS patients. Given that pupil dilation has been associated with conscious effortful processing, this finding suggests a richer cortical processing in MCS than in VS/UWS patients, as recently conceptualized under the acronym of cortically mediated state (CMS): MCS as defined by CRS-R criterion does not necessarily imply a residual consciousness but necessarily implies the existence of a CMS6.
We then applied the same approach at the individual level from generic auditory PDR to local, global and MVE effects. A generic auditory PDR was present in almost all patients except two VS/UWS patients and was therefore not a good predictor of diagnosis (i.e., MCS vs VS/UWS), or of consciousness recovery outcome. The only patient showing a significant PDR global effect was in MCS and recovered consciousness at 6 months.
Of special interest, presence of a significant individual [LSGS vs LDGD] PDR in 4 MCS patients and in 1 VS/UWS patient showed a trend of a predictive effect on consciousness recovery outcome. Concerning the VS/UWS patient with a significant LSGS vs LDGD] PDR effect, he died a few weeks after the evaluation and no evoked potentials were available. Besides we cannot determine whether his PDR effect reflected a defect in the specificity of the test, or demonstrated a richer state than clinically assumed. Many studies converge to show up to 15–20% of patients appear to be in a VS/UWS whereas their brain activity is suggestive of a MCS or even of a conscious state2,44,45.
ERPs were more sensitive than PDR to probe a global effect: a significant ERP MVE effect was found in 5 patients (4 MCS and 1 VS/UWS). Three of these patients recovered consciousness at 6 months. This last result tends to confirm the importance of artefacts and power issue (number of trials) that may have limited our ability to probe cognition with PDR in the current study.
Taken together, our results tend to suggest that bedside pupillometry and eye-tracking should still be considered as new approaches to explore consciousness and to predict recovery of consciousness in DoC patients. However, the current limitations we met at the individual level point to the necessity to solve several methodological issues. DoC patients blink rates are highly variable from one patient to another46,47 and are poorly controllable during the acquisition by the experiment in the absence of functional communication. When too abundant, and when other eye artefacts may impair PDR data (e.g., partial lid closures and sustained blepharospasms), PDR data may be unexploitable48,49. The current artefact correction techniques such as interpolation algorithms are not sufficient to overcome these limiting experimental conditions. Besides, patients must remain awake and non-agitated during the entire 6 min- paradigm to exploit pupillometric data and to be able to interpret them with high sensitivity to the current best conscious state. Here, among the 42 patients of the initial set, only 24 datasets (57%) were analyzable. Another difficulty stems from medications: in this study 41% of patients took medications such as opioids or scopolamine that probably influenced their pupillary function. Also, we cannot exclude that the pupillary response was artefacted by cognitive expectancy of the fifth sound. Indeed using the same paradigm, we previously measured an EEG contingent negative variation response (CNV) that corresponds to a slow anterior midline negative drift beginning from the onset of the first sound to the onset of the fifth sound34,50,51. In DoC patients the CNV was not more present in MCS or conscious state recordings than in VS recordings34. Another limitation inherent to pupillometry is the wide range of mental processes that can trigger pupillary dilations in the ICU environment such as pain, arousal fluctuations, displeasure and sudden environmental noise52.
To conclude, despite numerous technical challenges that remain to be overcome, these results open the way to a new window to probe residual cognition in DoC patients and by extension in non-communicating patients, at bedside, with cheap, non-invasive, relatively low-cost and non-constraining technology. Limitations pointed out by the present study should help to target the major directions of technological and methodological improvements, including an increase in the number of trials.
Data availability
The experimental datasets generated and analysed during the current study are available from the corresponding author upon reasonable request.
References
Edlow, B. L., Claassen, J., Schiff, N. D. & Greer, D. M. Recovery from disorders of consciousness: Mechanisms, prognosis and emerging therapies. Nat. Rev. Neurol. 17, 135–156 (2021).
Kondziella, D., Friberg, C. K., Frokjaer, V. G., Fabricius, M. & Møller, K. Preserved consciousness in vegetative and minimal conscious states: Systematic review and meta-analysis. J. Neurol. Neurosurg. Psych. 87, 485–492 (2016).
Giacino, J. T. et al. Comprehensive systematic review update summary: Disorders of consciousness. Neurology 91, 461–470 (2018).
Comanducci, A. et al. Clinical and advanced neurophysiology in the prognostic and diagnostic evaluation of disorders of consciousness: Review of an IFCN-endorsed expert group. Clin. Neurophysiol. https://doi.org/10.1016/j.clinph.2020.07.015 (2020).
Hermann, B. et al. Importance, limits and caveats of the use of “disorders of consciousness” to theorize consciousness. Neurosci. Conscious 2021, niab048 (2022).
Naccache, L. Minimally conscious state or cortically mediated state?. Brain 141, 949–960 (2018).
Raimondo, F. et al. Brain-heart interactions reveal consciousness in noncommunicating patients. Ann. Neurol. 82, 578–591 (2017).
Candia-Rivera, D. et al. Neural responses to heartbeats detect residual signs of consciousness during resting state in postcomatose patients. J. Neurosci. 41, 5251–5262 (2021).
Perez, P. et al. Conscious processing of narrative stimuli synchronizes heart rate between individuals. Cell Rep. https://doi.org/10.1101/2020.05.26.116079 (2020).
Lugo, Z. R. et al. Beyond the gaze: Communicating in chronic locked-in syndrome. Brain Inj. 29, 1056–1061 (2015).
Lieberman, J. D. et al. Use of admission Glasgow Coma Score, pupil size, and pupil reactivity to determine outcome for trauma patients. J. Trauma 55, 437–442 (2003) (discussion 442–443).
Peluso, L., Oddo, M., Sandroni, C., Citerio, G. & Taccone, F. S. Early neurological pupil index to predict outcome after cardiac arrest. Intensive Care Med. 48, 496–497 (2022).
Romagnosi, F. et al. Neurological pupil index for the early prediction of outcome in severe acute brain injury patients. Brain Sci. 12, 609 (2022).
Rossetti, A. O., Rabinstein, A. A. & Oddo, M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 15, 597–609 (2016).
Paulus, J. et al. Pupillary reflex measurement predicts insufficient analgesia before endotracheal suctioning in critically ill patients. Crit. Care 17, R161 (2013).
Stoll, J. et al. Pupil responses allow communication in locked-in syndrome patients. Curr. Biol. 23, R647-648 (2013).
Vassilieva, A., Olsen, M. H., Peinkhofer, C., Knudsen, G. M. & Kondziella, D. Automated pupillometry to detect command following in neurological patients: A proof-of-concept study. PeerJ 7, e6929 (2019).
Kahneman, D. & Beatty, J. Pupil diameter and load on memory. Science 154, 1583–1585 (1966).
Binda, P., Pereverzeva, M. & Murray, S. O. Pupil constrictions to photographs of the sun. J. Vis. 13, 8–8 (2013).
Einhäuser, W., Stout, J., Koch, C. & Carter, O. Pupil dilation reflects perceptual selection and predicts subsequent stability in perceptual rivalry. Proc. Natl. Acad. Sci. U. S. A. 105, 1704–1709 (2008).
Kietzmann, T. C., Geuter, S. & König, P. Overt visual attention as a causal factor of perceptual awareness. PLoS ONE 6, e22614 (2011).
Salvi, C., Simoncini, C., Grafman, J. & Beeman, M. Oculometric signature of switch into awareness? Pupil size predicts sudden insight whereas microsaccades predict problem-solving via analysis. Neuroimage 217, 116933 (2020).
Sperandio, I., Bond, N. & Binda, P. Pupil size as a gateway into conscious interpretation of brightness. Front Neurol. 9, 1070 (2018).
Dehaene, S. et al. Cerebral mechanisms of word masking and unconscious repetition priming. Nat. Neurosci. 4, 752–758 (2001).
Naccache, L. Why and how access consciousness can account for phenomenal consciousness. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373, 20170357 (2018).
Suzuki, Y., Minami, T. & Nakauchi, S. Association between pupil dilation and implicit processing prior to object recognition via insight. Sci. Rep. 8, 6874 (2018).
Castellotti, S., Conti, M., Feitosa-Santana, C. & Del Viva, M. M. Pupillary response to representations of light in paintings. J. Vis. 20, 14 (2020).
Sulutvedt, U., Mannix, T. K. & Laeng, B. Gaze and the eye pupil adjust to imagined size and distance. Cognit. Sci. 42, 3159–3176 (2018).
Friedman, D., Hakerem, G., Sutton, S. & Fleiss, J. L. Effect of stimulus uncertainty on the pupillary dilation response and the vertex evoked potential. Electroencephalogr. Clin. Neurophysiol. 34, 475–484 (1973).
Marois, A., Labonté, K., Parent, M. & Vachon, F. Eyes have ears: Indexing the orienting response to sound using pupillometry. Int. J. Psychophysiol. 123, 152–162 (2018).
Bekinschtein, T. A. et al. Neural signature of the conscious processing of auditory regularities. Proc. Natl. Acad. Sci. U. S. A. 106, 1672–1677 (2009).
El Karoui, I. et al. Event-related potential, time-frequency, and functional connectivity facets of local and global auditory novelty processing: An intracranial study in humans. Cereb Cortex 25, 4203–4212 (2015).
Perez, P. et al. Auditory event-related ‘global effect’ predicts recovery of overt consciousness. Front Neurol. 11, 588233 (2020).
Faugeras, F. et al. Event related potentials elicited by violations of auditory regularities in patients with impaired consciousness. Neuropsychologia 50, 403–418 (2012).
Faugeras, F. et al. Probing consciousness with event-related potentials in the vegetative state. Neurology 77, 264–268 (2011).
Schiff, N. D. Cognitive motor dissociation following severe brain injuries. JAMA Neurol. 72, 1413–1415 (2015).
Claassen, J. et al. Detection of brain activation in unresponsive patients with acute brain injury. N. Engl. J. Med. 380, 2497–2505 (2019).
Wacongne, C. et al. Evidence for a hierarchy of predictions and prediction errors in human cortex. Proc. Natl. Acad. Sci. 108, 20754–20759 (2011).
Quirins, M. et al. Conscious processing of auditory regularities induces a pupil dilation. Sci. Rep. 8, 14819 (2018).
Giacino, J. T., Kalmar, K. & Whyte, J. The JFK Coma Recovery Scale-Revised: Measurement characteristics and diagnostic utility11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated. Arch. Phys. Med. Rehabil. 85, 2020–2029 (2004).
Hermann, B. et al. Habituation of auditory startle reflex is a new sign of minimally conscious state. Brain 143, 2154–2172 (2020).
Tadel, F., Baillet, S., Mosher, J. C., Pantazis, D. & Leahy, R. M. Brainstorm: A user-friendly application for MEG/EEG analysis. Comput. Intell. Neurosci. https://doi.org/10.1155/2011/879716 (2011).
Burock, M. A., Buckner, R. L., Woldorff, M. G., Rosen, B. R. & Dale, A. M. Randomized event-related experimental designs allow for extremely rapid presentation rates using functional MRI. NeuroReport 9, 3735–3739 (1998).
Sitt, J. D. et al. Large scale screening of neural signatures of consciousness in patients in a vegetative or minimally conscious state. Brain 137, 2258–2270 (2014).
Thibaut, A. et al. Preservation of brain activity in unresponsive patients identifies MCS star. Ann. Neurol. 90, 89–100 (2021).
Bonfiglio, L. et al. Spontaneous blinking behaviour in persistent vegetative and minimally conscious states: Relationships with evolution and outcome. Brain Res. Bull. 68, 163–170 (2005).
Magliacano, A. et al. Spontaneous eye blinking as a diagnostic marker in prolonged disorders of consciousness. Sci. Rep. 11, 22393 (2021).
Johansson, J., Franzon, K., Godbolt, A. K. & Möller, M. C. Methodological aspects of using a wearable eye-tracker to support diagnostic clinical evaluation of prolonged disorders of consciousness. J. Rehabil. Med. 53, jrm00213 (2021).
Yoo, K., Ahn, J. & Lee, S.-H. The confounding effects of eye blinking on pupillometry, and their remedy. PLoS ONE 16, e0261463 (2021).
Chennu, S. et al. Expectation and attention in hierarchical auditory prediction. J. Neurosci. 33, 11194–11205 (2013).
Rozier, C. et al. Conscious and unconscious expectancy effects: A behavioral, scalp and intracranial electroencephalography study. Clin. Neurophysiol. 131, 385–400 (2020).
Eckstein, M. K., Guerra-Carrillo, B., Miller Singley, A. T. & Bunge, S. A. Beyond eye gaze: What else can eyetracking reveal about cognition and cognitive development?. Dev. Cognit. Neurosci. 25, 69–91 (2016).
Acknowledgements
A.S. was funded by “Bourse poste d’Accueil” Grant from “Inserm” and by the foundation “Gueule Cassée” and the Foundation “Matmut Paul Bennetot”; L.N was funded by an “FRM Equipe 2015” and by UNIM Grant.
Author information
Authors and Affiliations
Contributions
A.S., C.E. and L.N. planned and ran the analyses, wrote and revised the manuscript, A.S. finalized tables and figures; M.Q., C.M., M.V., performed the experiments; L.N., P.P, M.Q., N.W.; B.R.; S.D., A.B., E.M. and J.S., C.E.; designed the experiments and organized the research project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sangare, A., Quirins, M., Marois, C. et al. Pupil dilation response elicited by violations of auditory regularities is a promising but challenging approach to probe consciousness at the bedside. Sci Rep 13, 20331 (2023). https://doi.org/10.1038/s41598-023-47806-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47806-1
- Springer Nature Limited
This article is cited by
-
Covert Consciousness in Acute Brain Injury Revealed by Automated Pupillometry and Cognitive Paradigms
Neurocritical Care (2024)