Abstract
Heart failure is a challenging public health problem associated with poor health-related quality of life (HRQoL). Data on the quality of life of people with heart failure are limited in Ethiopia. This study aimed to assess the HRQoL and its influencing factors in people with heart failure in Ethiopia. A hospital-based, cross-sectional study design was conducted in the cardiac outpatient clinics of two tertiary-level hospitals in Addis Ababa, Ethiopia. Data were collected from people with heart failure who met the inclusion criteria using an interviewer-administered questionnaire. The HRQoL was measured using the Minnesota Living with Heart Failure Questionnaire (MLHFQ). A multiple linear regression model was fitted to identify factors that influenced HRQoL. All statistical analyses were conducted using STATA version 17 software. A total of 383 people with heart failure participated in the study. The mean age of the participants was 55 years. The MLHFQ score was 48.03±19.73, and 54% of participants had poor HRQoL. Multiple linear regression analysis revealed that age (β= 0.12, 95% CI 0.11, 0.28), diabetes mellitus comorbidity (β= 4.47, 95% CI 1.41, 7.54), social support score (β= − 1.48, 95% CI − 1.93, − 1.03), and depression score (β = 1.74, 95% CI 1.52, 1.96) were significant factors influencing overall HRQoL (p < 0.05). This study found that people in Ethiopia with heart failure had poor HRQoL, influenced by several factors. The findings can help health professionals identify appropriate interventions to improve the HRQoL of people with heart failure.
Similar content being viewed by others
Introduction
Heart failure (HF) is a chronic medical condition associated with high morbidity and mortality rates1. It is diagnosed in one to two of every 100 adults in the general population, but the actual prevalence is probably around 4%2. Its risk factors include age, coronary artery disease, rheumatic heart disease, hypertension, and diabetes mellitus. Heart failure is the most common type of cardiovascular disease (CVD) in Africa and has a great social and economic impact mainly affecting young individuals. Rheumatic heart disease is one of the most prevalent risk factors for HF, occurring in 14 % of people with HF in sub-Saharan Africa3,4,5. According to the international congestive heart failure study report, the highest annual mortality in people with HF was observed in Africa6. In Ethiopia, the in-hospital mortality due to HF is high7.
Health-related quality of life (HRQoL) is an individual’s perception of their physical, social, emotional, psychological, and mental functioning8,9. Measuring HRQoL is often used to assess the effectiveness of HF treatment and the course of the disease10. Living with HF is challenging as it has a poor prognosis and increased socioeconomic burden due to increased healthcare costs, debilitating symptoms such as dyspnoea, oedema, fatigue, and sleep disturbance, and frequent hospitalisations which collectively, significantly impact HRQoL. Poor HRQoL increases the risk of hospitalisation and death11,12.
Many factors influence the HRQoL of people with HF. The revised Wilson and Clearly model is a practical conceptual framework that incorporates the relationship between different health concepts to guide quality of life research13. According to this model, HRQoL is affected by individual characteristics, biological function, environmental characteristics, symptoms, functional status, and general health perceptions. Previous studies have identified multiple predictors of poor HRQoL including gender (female), age (young), marital status (single), income and educational levels (low), presence of depression, high New York Heart Association (NYHA) functional class, tobacco exposure, low ventricular ejection, history of hospitalisation, comorbidity, polypharmacy, poor medication adherence and duration of heart failure14,15,16,17,18,19,20. Identifying meaningful factors influencing HRQoL is critical to develop effective interventions to improve prognosis in this cohort21.
Improving symptoms and physical functioning are the major aims of heart failure management. Effective means of measuring how much the disease affects this population provides insights into targeted management interventions21,22. Both pharmacologic and non-pharmacologic interventions can enhance overall health and reduce poor health outcomes, and are recommended as an integral part of disease management strategies23,24. A systematic review and meta-analysis of randomized controlled trial showed significant overall HRQoL improvement after conducting psychosocial interventions for people with HF25. In Ethiopia, the government developed a comprehensive guideline for clinical management and care for major non-communicable diseases (NCDs) including HF. This is a major initiative aiming to reduce the increasing burden of NCDs in Ethiopia26.
Heart Failure is a major problem with high prevalence; however, few studies have investigated the impact of HF on HRQoL, especially in Africa. The available data indicates that poor quality of life in people with HF is a challenging problem in Ethiopia27. Consequently, this study sought to assess HRQoL and its influencing factors in people with HF based on the revised Wilson and Cleary model of HRQoL. Measuring HRQoL provides information about an individual’s overall health status and the impact of health interventions28. The findings from this study will inform healthcare policymakers on effective ways to improve care for this population in Ethiopia.
Methods
Study area and period
The study was conducted at the cardiac outpatient clinics of two tertiary level public hospitals in Addis Ababa, the capital of Ethiopia. St. Paul's Hospital Millennium Medical College and St. Peter Specialised Hospital are government-owned hospitals in Addis Ababa. They are Ethiopia’s largest tertiary-level specialist and teaching hospitals, providing referral services for people from all around the country. Currently, the two hospitals collaborate to provide care for patients with cardiac conditions. Each hospital had a weekly average of 30 people with HF coming to visit outpatient clinics for their routine follow-up care.
The survey was conducted between 21 Nov 2022 to 22 Jan 2023.
Study design
A hospital-based survey using a cross-sectional study design was conducted.
Theoretical framework
This study was guided by the revised version of Wilson and Cleary model of HRQoL13. This model provides a clear understanding of variables influencing HRQoL and clarify the relationships among them to guide quality of life research29. According to this model, HRQoL as the outcome variable is influenced by the characteristics of the individual, biological function, symptoms, functional status, characteristics of the environment, and general health perception (Fig. 1). It is the most widely used and the recommended model for HRQoL research30,31. This model, in the context of Ethiopia, provides a significant framework for assessing HRQoL that is adapted to the unique healthcare challenges of the country such as limited resources, poor healthcare access and diverse socioeconomic conditions that influence health outcomes32. By applying this model within this context, we identified factors affecting HRQoL of people with HF in Ethiopia.
Revised Wilson and Cleary model of HRQoL13.
Eligibility criteria and ethics
The following inclusion criteria were considered: 1) adults aged over 18 years of age, 2) diagnosed with heart failure (clinically using Framingham criteria or Echocardiography), 3) receiving follow-up care at the outpatient cardiac clinic for at least three months. The study was approved by the University of Technology Sydney (UTS) Human Research Ethics Committees (UTS HREC REF NO. ETH21-6739). Local ethical approval was obtained from the institutional review board (IRB) of each hospital where data collection took place. All methods were performed in accordance with the relevant guidelines and regulations.
Sample size and sampling procedure
The sample size was determined using a single proportion formula for finite population, N= (Zα/2)2*P (1 − P)2/D2)33, with the assumption of a 95% confidence interval, marginal error (d) of 5.0 % and 51.8% prevalence (P) of low HRQoL among people with HF in Northwest Ethiopia34. N= {(1.96)2*0.518 (1-0.518)}/0.052=383 people with HF.
Consecutive sampling technique was used, and all eligible people with HF with an appointment at the outpatient cardiac clinics were invited to participate in the study. Participants who met the inclusion criteria and agreed to provide informed consent were included in this study until the required sample size was achieved.
Variables
Dependent variable
-
Health-related quality of life
Independent variables
-
Characteristics of the individual
-
Age, sex, educational status, marital status, health insurance
-
-
Biologic function
-
Family history of heart failure, comorbidities
-
-
Symptoms
-
Depression
-
-
Functional status
-
The severity of heart failure: New York Heart Association (NYHA) class
-
-
Characteristics of the environment
-
Social support, residence, employment status, duration of illness, history of hospitalisations, number of medications taken each day.
-
-
Overall health perception
Operational definitions and definitions of terms
Adult: 18 years and over.
Heart failure: inability of the heart to effectively pump blood as evidenced by either signs and symptoms based on Framingham criteria or reduced ejection fraction (<40%)35,36.
Health-related quality of life: individuals’ perceptions and reactions to the impact of a disease or its treatment on their daily lives. It encompasses many dimensions of life, including physical, functional, emotional, and mental health37. Health-related quality of life of people with HF was measured by the Minnesota Living with Heart Failure Questionnaire (MLHFQ). This tool has 21 items or questions that asks participants how their disease has affected their life in the last month. Each question is coded using a six-point Likert-type scale that ranges from 0 (no effect) to 5 (very much effect). These scales are then added together to create a composite score that indicates the participant's overall HRQoL. The scores range from 0 to 105 with the higher composite scores represents the poorer quality of life. It gives a total score as well as scores on two dimensions: physical (from 2 to 7, 12, and 13, range, 0–40) and emotional (from 17 to 21, range, 0–25). The remaining eight questions (1, 8, 9, 10, 11, 14, 15, and 16) are only considered to calculate the total composite score38,39,40. It is a gold standard and widely used disease-specific quality of life measurement instrument that has been validated for use in many countries20,41,42,43,44,45.
Depression: feelings of unhappiness and lack of interest in daily activities with symptoms for at least two weeks based on DSM-5 diagnostic criteria46. Depression was measured using the patient health questionnaire (PHQ-9). This is a 9-item tool based on DSM-IV criteria that can be scored from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27, with higher scores indicating a higher likelihood of depression. Each item requires participants to rate the frequency of a depressive symptom experienced in the two weeks prior to assessment. PHQ-9 is a reliable and valid instrument for detecting major depressive disorder among Ethiopian adults with chronic conditions in outpatient settings47,48.
The level of social support was measured using the Oslo Social Support Scale (OSSS-3). This scale consists of three items that asks about numbers of close confidants, sense of concern from other people, and relationships with neighbours, with a focus on the availability of practical help. The scores range from 3-14, with high values representing strong levels and low values representing weak levels of social support49. It has good construct and predictive validity and good internal consistency with a Cronbach alpha of 0.9150.
General health perception: a representation of all health concepts together which determined overall satisfaction with life using one global question that asks the respondent to rate their overall health on a Likert scale as "excellent", "very good", "fair" or "poor"13.
The severity of heart failure: New York Heart Association criteria (NYHA) is used to classify the severity of heart failure as Class I: no limitation during ordinary activity, Class II: slight limitation during ordinary activity, Class III: marked limitation of normal activities without symptoms at rest, Class IV: unable to undertake physical activity without symptoms and symptoms may be resent at rest51.
Data collection procedure and instruments
The questionnaire was adapted from different literature and validated tools, and the process involved translation, cultural adaptation, and validation, which involved professional and language experts and pre-testing. These adaptations were made to ensure that the questionnaire was suitable for the cultural and linguistic context of Ethiopia. The questionnaire consisted of four parts: The first part related to sociodemographic and clinical related characteristics; the second part dealt with social support, the third part measured depression and the final section evaluated HRQoL. People with HF who met the eligibility criteria were contacted by trained research assistants (RAs) during their routine follow-up visit to the outpatient cardiac clinic of each hospital. RAs collected the data in person using an interviewer-administered questionnaire.
The sociodemographic and clinical characteristics were assessed using a 19-item questionnaire. This questionnaire collected information about age, sex, marital status, employment status, residence, educational level, health insurance, family history of HF, hospitalisation history, comorbidities, duration of illness, NYHA class, number medication taken each day and general health perception. The Oslo Social Support Scale (OSSS-3) was used to measure the level of social support and depression was measured using the patient health questionnaire (PHQ-9). Finally, the Minnesota Living with Heart Failure Questionnaire (MLHFQ) was used to measure the health-related quality of life of participants.
To ensure the quality of data, training on data collection procedure was provided to the research assistants. The collected data were checked for completeness and clarity daily. Two supervisors supervised the data collection process.
Data management and analysis
Collected data were cleaned and entered into Epi-Data version 3.1 and exported to STATA Version 17 for analysis52. Descriptive analyses were performed to describe the socio-demographic and clinical characteristics of the participants, the OSSS-3, the PHQ-9, and the MLHFQ scores. A linear regression model was fitted to assess the association between independent variables and dependent variable. First, simple linear regression was performed to test the association between each independent variable with the dependent variable. All independent variables with a p-value of less than 0.25 on the simple linear regression analysis were eligible for further analysis in the multiple linear regression model. The assumptions of linear regression such as normality, linearity, independence, and homoscedasticity were checked. The results are presented in text, tables and graphs based on the types of data.
Ethics approval and consent to participate
The study was approved by the University of Technology Sydney (UTS) Human Research Ethics Committees (UTS HREC REF NO. ETH21-6739), and local Ethical approval latter to conduct the study was obtained from the institutional review board (IRB) of each hospital where the data collection took place. The purpose, risk and benefit of the study were explained to the participants before conducting data collection. Written informed consent was obtained from participants who agreed to participate, and they were assured of the anonymity and confidentiality of their personal information. The data were collected in a quite area at the hospital.
Results
Sociodemographic and clinical characteristics
Three hundred and eighty-three (383) people with heart failure participated in this study with a response rate of 100%. Of these, 199 (51.96%) were female and 184 (48.04%) were male. The mean age of the participants was 55.1 (± 15.38) years. From all participants, 97 (25.33%) came from rural areas, and 196 (51.17%) were married. A total of 114 (29.77%) participants did not have any formal education. The Ethiopian Community Health Insurance (CHI) was held by 276 (72.06%) participants and 132 (34.46%) had a history of recent hospitalisation. Concerning comorbidities, 169 (44.13%) and 80 (20.89%) participants had hypertension and diabetes mellitus, respectively. The participants’ length of time since HF diagnosis ranged from 3 months to 22 years, with a mean of 4.80 years. Their mean social support and depression scores were 8.98 ±2.94 and 11.02 ±6.14, respectively. In the study, 100 (26.11%) participants had poor general health perception. Other sociodemographic and clinical characteristics are presented in Table 1.
Health-related quality of life of people with heart failure
In this study, HRQoL of people with HF was assessed with MLHFQ. The mean of total MLHFQ score was 48.03±19.73, indicating a poor HRQoL among the study participants. Higher scores on the MLHFQ represent poorer quality of life. The subscale scores of MLHFQ were found to be 21.03±8.46 for physical scale and 10.12±6.26 for emotional scale (Table 2).
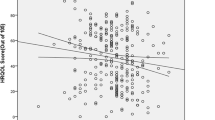
The MLHFQ score was used to determine the level of HRQoL as people who score less than 24 labelled as having (good) HRQOL, 24–45 (moderate), and greater than 45 as (poor) HRQOL53,54. The analysis revealed that 204 (53.26%) participants had a poor HRQoL (Fig. 2).
Factors influencing the HRQoL of people with heart failure
Simple linear regression analysis demonstrated that variables such as age, sex, marital status, employment status, educational level, hospitalisation history, hypertension, diabetes mellitus, Acquired Immune Deficiency Syndrome (AIDS), New York Heart association (NYMA) class, social support scores, depression scores, and general health perception were factors associated with MLHFQ score at p<0.25 and were eligible for multiple linear regression. The multiple linear regression model revealed that only age, employment status, DM comorbidity, social support scores, NYHA class, depression scores, and general health perception were significantly associated with overall HRQoL of people with heart failure at p≤0.05. These variables explain 70% of variation of the overall MLHFQ scores.
Each extra year of age of participants predicts an increase in MLHFQ score by 0.12 (β = 0.12, CI (0.11, 0.28), p = 0.001). People who were unemployed scored an average 2.73-point higher MLHFQ score than employed people (β= 2.73, CI (0.22, 5.24), p = 0.033). A 1-unit increase in Oslo social support score corresponded to a 1.48-unit decrease in MLHFQ score (β = − 1.48, CI = (− 1.93, − 1.03), p=0.001). This means that strong social support is positively associated with HRQoL. People with diabetes scored an average 4.47-point higher MLHFQ score than those without diabetes (β = 4.47, CI (1.41, 7.54), p = 0.004). A 1 unit increase in the PHQ-9 score was associated with an increase in MLHFQ score by 1.744 (β= 1.74, CI (1.52, 1.96), p=0.001). Compared to participants with NYHA class I, those with class III (β=4.621, CI (1.50, 7.74), p=0.004) and IV (β=7.955, CI (3.66, 12.25), p=0.001) had a significantly higher HRQoL score, indicating poorer HRQoL as physical limitation or severity increases. The detailed result of multiple linear regression analysis is presented in Table 3.
Discussion
Health related quality of life (HRQoL) is a critically important clinical outcome for people with HF55. This study investigated the HRQoL of people with heart failure and examined its influencing factors using the revised Wilson-Cleary HRQoL model. In this study, 53.26% (95%CI: 48.12, 58.35) of participants had poor HRQoL. This finding is consistent with the result of previous studies conducted in low-middle income countries34,56,57. The mean of total MLHFQ scores in the current study was 48.03 (95%CI: 46.04, 50.01), which indicates that people with HF have poor physical, emotional, and overall HRQoL. This finding is consistent with the previous similar studies that have shown the negative impact of HF on the physical, emotional and the general aspects of HRQoL34,38,57. The mean total MLHFQ score of the current study was higher than similar studies conducted in Brazil58,59,60, China61, Myanmar1, South Korea16,62 and Thailand17. The higher MLHFQ score in our population could be due to the cohort age as most participants were aged 40-69 years and had higher rate of depression than reported in studies from countries. Conversely, the mean of total MLHFQ score in this study was lower than studies conducted in Colombia63, Serbia14,64, Georgia65, and South Korea66. This difference might be due to variation in methodological approaches, sample size, socioeconomic characteristics, and study settings.
The current study identified various sociodemographic and clinical factors influencing the HRQoL of people with HF. Factors such as higher age, unemployment, poor social support, comorbid depression, diabetic comorbidity, higher NYHA class, and poor health perception were significantly associated with low HRQoL in people with HF, after controlling for known confounders such as gender, hospitalisation history, marital status, educational level, hypertension, and HIV/AIDS.
Sociodemographic factors such as age and employment had a strong influence on HRQoL, but gender had a weak influence. Increasing age was significantly associated with an increased MLHFQ score. This was supported by similar studies that reported a decrease in the HRQoL as people aged16,67. This finding can be attributed to the fact that older individuals experience more physical limitations and psychological problems68. A significant negative association between age and HRQoL was observed in other studies; the lower the age, the worse the quality of life58,60. According to the results of previous studies16,57,69, gender was a significant predictor of poor HRQoL, with women reporting significantly lower quality of life than men. Ahmeti et al. reported that females had poorer quality of life than males with HF38. However, there was no association between gender and HRQoL in the current study, which is consistent with Erceg et al. (2013) findings70. Regarding employment, people who were unemployed had a lower HRQoL than employed people. This finding is supported by previous studies16,70,71. This may be attributed to unemployed individuals often having a lower economic status and experience financial hardship due to medication and other health costs, which negatively impact management of HF and reduce their HRQoL69.
Another factor which influenced HRQoL in people with HF was social support. A strong social support network was associated with a better HRQoL. A similar study by Barutcu , et al. (2013) showed that higher levels of social support was significantly associated with better HRQoL in people with HF72. In addition, Soleimani et al. found that people with higher levels of social support had significantly improved HRQoL73. Other studies showed that social support improve HRQoL indirectly by enhancing self-care66,74. This could be because strong social support plays a critical role in helping individuals with emotional support that can help them to cope with the emotional burden of their condition and protect them from harmful outcomes, consequently improving HRQoL66,75.
In the current study, comorbid depression and diabetes mellitus predicted lower HRQoL with a significant association between depression and HRQoL. This finding is consistent with previous studies that reported a strong association between depression and HRQoL14,65,70,76,77,78,79,80. Comorbid depression negatively influences an individual's psychosocial wellbeing and affect selfcare practices and treatment adherence81,82. Similarly, a significant influence of comorbid diabetes mellitus on the overall HRQoL was observed. The same finding has been reported in previous studies83,84,85. People with diabetes who have poor glycaemic control and associated complications are more likely to experience various health problems that significantly lower HRQoL86. In addition, non-cardiovascular comorbidities accelerates disease progression and increases risk of rehospitalisation which can lead to additional socioeconomic burden, ultimately reducing HRQoL80.
In the present study, people with NYHA class III and IV were associated with poor HRQoL. This finding has been reported in many previous studies70,87,88. The possible justification for impaired HRQoL being correlated with higher NYHA class could be because the ability to carry out daily activities decreases as the severity of the disease increase, which negatively affects quality of life54.
Limitations and suggestions for future research
The findings of this study have implications for clinical practice. Determining the quality of life of people with HF provides information about the impact of HF on overall perceived well-being. A better understanding of factors influencing HRQoL may help health care professionals to identify effective interventions to improve individuals’ HRQoL. This study has several limitations that should be considered when interpreting its results. First, its cross-sectional nature limits its ability to establish cause-and-effect relationships. Therefore, longitudinal studies in this domain are recommended to investigate causal relationships. Second, the use of a self-report questionnaire to collect data in this study could lead to information bias, and participants could be influenced by recall bias or the Hawthorn effect89. Finally, the influence of critical factors from the Wilson and Cleary model, such as selfcare practice, medication adherence and HF knowledge, were not evaluated in this study. Future research should evaluate these variables to gain a deeper understanding of their influence.
Conclusion
This study reported the impact of HF on the HRQoL in an Ethiopian cohort. The results revealed that more than half of all people living with HF in Ethiopia had a poor HRQoL, as demonstrated by the mean score of total MLHFQ and its subscales. Factors such as age, employment status, depression, social support, diabetic comorbidity, NYHA class, and health perception were significant in influencing the HRQoL of people with HF. Future interventional studies are recommended with the aim of improving the HRQoL of these population.
Data availability
All the data analysed in this study are available from the corresponding author upon a reasonable request.
Abbreviations
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- HF:
-
Heart failure
- HRQoL:
-
Health-related quality of life
- MLHFQ:
-
Minnesota living with heart failure questionnaire
- NYHA:
-
New York heart association
- NCDs:
-
Non-communicable diseases
- OSSS-3:
-
Oslo social support scale
- PHQ-9:
-
Patient health questionnaire
- SE:
-
Standard error
References
Thida, M., Asdornwised, U., Thosingha, O., Dumavibhat, C. & Chansatitporn, N. Symptom experience, symptom management strategies, and health related quality of life among people with heart failure. Pacific Rim Int. J. Nurs. Res. 25(3), 359–74 (2021).
Groenewegen, A., Rutten, F. H., Mosterd, A. & Hoes, A. W. Epidemiology of heart failure. Eur. J. Heart Fail. 22(8), 1342–56 (2020).
Arrigo, M. et al. Acute heart failure. Nat. Rev. Dis. Primers 6(1), 1–15 (2020).
Meijers, W. C. & de Boer, R. A. Common risk factors for heart failure and cancer. Cardiovasc. Res. 115(5), 844–53 (2019).
Nyaga, U. F. et al. Data on the epidemiology of heart failure in Sub-Saharan Africa. Data Brief 17, 1218–39 (2018).
Dokainish, H. et al. Global mortality variations in patients with heart failure: Results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Global Health 5(7), e665–e72 (2017).
Tirfe, M., Nedi, T., Mekonnen, D. & Berha, A. B. Treatment outcome and its predictors among patients of acute heart failure at a tertiary care hospital in Ethiopia: A prospective observational study. BMC Cardiovasc. Disord. 20(1), 1–10 (2020).
Anderson, N. & Ozakinci, G. Effectiveness of psychological interventions to improve quality of life in people with long-term conditions: Rapid systematic review of randomised controlled trials. BMC Psychol. 6(1), 11 (2018).
Kang, K., Gholizadeh, L., Inglis, S. C. & Han, H. R. Interventions that improve health-related quality of life in patients with myocardial infarction. Qual. Life Res. 25(11), 2725–37 (2016).
Westlake, C. et al. Correlates of health-related quality of life in patients with heart failure. Heart Lung 31(2), 85–93 (2002).
Hobbs, F. et al. Impact of heart failure and left ventricular systolic dysfunction on quality of life. A cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur. Heart J. 23(23), 1867–76 (2002).
AbuRuz, M. E. Anxiety and depression predicted quality of life among patients with heart failure. J. Multidiscip. Healthc. 11, 367 (2018).
Ferrans, C. E., Zerwic, J. J., Wilbur, J. E. & Larson, J. L. Conceptual model of health-related quality of life. J. Nurs. Scholarsh. 37(4), 336–42 (2005).
Erceg, P. et al. Health-related quality of life in elderly patients hospitalized with chronic heart failure. Clin. Interv. Aging 8, 1539–46 (2013).
Boombhi, J. et al. Quality of life in patients with chronic heath failure followed at the tertiary hospitals of Sub-Saharan Africa. Cardiovasc. Res. 3(4), 80–5 (2019).
Chu, S. H. et al. Factors affecting quality of life in Korean patients with chronic heart failure. Japan J. Nurs. Sci. 11(1), 54–64 (2014).
Silavanich, V., Nathisuwan, S., Phrommintikul, A. & Permsuwan, U. Relationship of medication adherence and quality of life among heart failure patients. Heart Lung 48(2), 105–10 (2019).
Shojaei F. Quality of life in patients with heart failure. Hayat. 2008;14(2).
Demir, M. & Unsar, S. Assessment of quality of life and activities of daily living in Turkish patients with heart failure. Int. J. Nurs. Pract. 17(6), 607–14 (2011).
Hwang, S. L., Liao, W. C. & Huang, T. Y. Predictors of quality of life in patients with heart failure. Jpn. J. Nurs. Sci. 11(4), 290–8 (2014).
AbuRuz, M. E., Alaloul, F., Saifan, A., Masa’Deh, R. & Abusalem, S. Quality of life for Saudi patients with heart failure: a cross-sectional correlational study. Global J. Health Sci. 8(3), 49 (2016).
Butler, J. et al. Empagliflozin and health-related quality of life outcomes in patients with heart failure with reduced ejection fraction: The EMPEROR-Reduced trial. Eur. Heart J. 42(13), 1203–12 (2021).
Lin, X., Gao, B.-B. & Huang, J. Prevalence of depressive symptoms in patients with Heart Failure in China: A meta-analysis of comparative studies and epidemiological surveys. J. Affect. Disord. 274, 774–83 (2020).
Mo, Y., Wang, H., Huang, G. & Chu, M. Effectiveness of nurse-led program on mental health status and quality of life in patients with chronic heart failure. Medicine (Baltimore) 99(33), e21746 (2020).
Samartzis, L., Dimopoulos, S., Tziongourou, M. & Nanas, S. Effect of psychosocial interventions on quality of life in patients with chronic heart failure: A meta-analysis of randomized controlled trials. J. Cardiac Fail. 19(2), 125–34 (2013).
Dagnaw WW, Yadeta D, feleke y, Kebede T. Ethiopian National Guideline on Clinical and Programmatic Management of Major Non Communicable Diseases. 2016.
Yazew KG, Beshah DT, Salih MH, Zeleke TA. Factors associated with depression among heart failure patients at cardiac follow-up clinics in northwest Ethiopia, 2017: A cross-Sectional Study. Psychiatry J. 2019; 2019.
Tito, K., Gebremariam, G. T., Beyene, K., Sander, B. & Gebretekle, G. B. Health-related quality of life and treatment satisfaction of patients with cardiovascular disease in Ethiopia. Front. Public Health https://doi.org/10.3389/fpubh.2022.972378 (2022).
Son, Y.-J., Baek, K.-H., Lee, S. J. & Seo, E. J. Health-related quality of life and associated factors in patients with atrial fibrillation: An integrative literature review. Int. J. Environ. Res. Public Health 16(17), 3042 (2019).
Bakas, T. et al. Systematic review of health-related quality of life models. Health Qual. Life Outcomes 10(1), 1–12 (2012).
Ojelabi, A. O., Graham, Y., Haighton, C. & Ling, J. A systematic review of the application of Wilson and Cleary health-related quality of life model in chronic diseases. Health Qual. Life Outcomes 15(1), 1–15 (2017).
Ayalneh, A. A., Fetene, D. M. & Lee, T. J. Inequalities in health care utilization for common childhood illnesses in Ethiopia: Evidence from the 2011 Ethiopian Demographic and Health Survey. Int. J. Equity Health 16, 1–9 (2017).
Suresh, K. & Chandrashekara, S. Sample size estimation and power analysis for clinical research studies. J. Hum. Reprod. Sci. 5(1), 7 (2012).
Seid, M. A. Health-related quality of life and extent of self-care practice among heart failure patients in Ethiopia. Health Qual. Life Outcomes 18(1), 1–7 (2020).
Löfström, U. et al. Prognostic impact of Framingham heart failure criteria in heart failure with preserved ejection fraction. ESC Heart Fail. 6(4), 830–9 (2019).
Hage, C. et al. Do patients with acute heart failure and preserved ejection fraction have heart failure at follow-up: Implications of the Framingham criteria. J. Cardiac Fail. 26(8), 673–84 (2020).
Lin, X.-J., Lin, I. M. & Fan, S.-Y. Methodological issues in measuring health-related quality of life. Tzu Chi Med. J. 25(1), 8–12 (2013).
Ahmeti A, Ibrahimi P, Bytyci I, Haliti E, Olloni R, Elezi S, et al., editors. Use of the “Minnesota living with heart failure questionnaire” quality of life questionnaire in Kosovo’s heart failure patients. Int. Cardiovasc. Forum J. 2016.
Rector TS. FDA medical device development tool (MDDT) qualification package for the Minnesota living with heart failure questionnaire (MLHFQ), 2017. 2017.
Audi, G. et al. Factors affecting health related quality of life in hospitalized patients with heart failure. Cardiol. Res. Pract. 2017, 1–12 (2017).
Garin, O. et al. Validación de la versión española del Minnesota Living with Heart Failure Questionnaire. Revista espanola de cardiologia 61(3), 251–9 (2008).
Middel, B. et al. Psychometric properties of the Minnesota living with heart failure questionnaire (MLHF-Q). Clin. Rehabil. 15(5), 489–500 (2001).
Moon, J. R. et al. Reliability and validity of the Korean version of the Minnesota Living with Heart Failure Questionnaire. Heart Lung 41(1), 57–66 (2012).
Saccomann, I. C., Cintra, F. A. & Gallani, M. C. B. Psychometric properties of the Minnesota Living with Heart Failure—Brazilian version—In the elderly. Qual. Life Res. 16(6), 997–1005 (2007).
Ho, C.-C., Clochesy, J. M., Madigan, E. & Liu, C.-C. Psychometric evaluation of the Chinese version of the Minnesota Living with Heart Failure Questionnaire. Nurs. Res. 56(6), 441–8 (2007).
Truschel J. Depression definition and DSM-5 diagnostic criteria. 2020.
Gelaye, B. et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 210(2), 653–61 (2013).
Degefa, M., Dubale, B., Bayouh, F., Ayele, B. & Zewde, Y. Validation of the PHQ-9 depression scale in Ethiopian cancer patients attending the oncology clinic at Tikur Anbessa specialized hospital. BMC Psychiatry 20(1), 446 (2020).
Kocalevent, R.-D. et al. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 6(1), 1–8 (2018).
Shumye, S., Belayneh, Z. & Mengistu, N. Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: A cross sectional study. Health Qual. Life Outcomes 17(1), 1–9 (2019).
Miller-Davis, C., Marden, S. & Leidy, N. K. The New York Heart Association Classes and functional status: What are we really measuring?. Heart Lung 35(4), 217–24 (2006).
StataCorp L. College Station, TX, USA, 2017. Â; 2020.
Kaptoge, S. et al. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Global Health 7(10), e1332–e45 (2019).
Poorshadan, S. et al. Quality of life and its predictors in hospitalized patients with heart failure at hospitals affiliated to Kermanshah-Iran University of medical Sciences. J. Cardiovasc. Dis. Res. 10(1), 16–9 (2019).
Kosiborod, M. N. et al. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: Results from the DAPA-HF trial. Circulation 141(2), 90–9 (2020).
An, Y., Zhang, Y., Wang, L., Chen, C. & Fan, X. The relationship between uncertainty in illness and quality of life in patients with heart failure: Multiple mediating effects of perceived stress and coping strategies. J. Cardiovasc. Nurs. 37(3), 257–65 (2022).
Molla, S., Yitayal, M. & Amare, G. Health-related quality of life and associated factors among adult patients with heart failure in Wolaita Zone Governmental Hospitals, Southern Ethiopia. Risk Manag. Healthc. Policy 14, 263 (2021).
Paz, L. F. A. et al. Quality of life related to health for heart failure patients. Revista brasileira de enfermagem. 72, 140–6 (2019).
de Sousa, M. M. et al. Physical and psychosocial effects of heart failure in perceived quality of life. Cogitare Enferm. 22(2), e49783 (2017).
Sousa, M. M. et al. Association of social and clinical conditions to the quality of life of patients with heart failure. Revista gaucha de enfermagem https://doi.org/10.1590/1983-1447.2017.02.65885 (2017).
Zhang, J., Gilmour, S., Liu, Y. & Ota, E. Effect of health literacy on quality of life among patients with chronic heart failure in China. Qual. Life Res. 29(2), 453–61 (2020).
Lee, H. et al. Knowledge, adherence to lifestyle recommendations, and quality of life among Koreans with heart failure. J. Cardiovasc. Pharmacol. Ther. 25(4), 324–31 (2020).
Afsharipour, Z., Khademiyeh, M., Arab, M. & Soltani-Nezhad, N. Evaluating the quality of life in hospitalized patients with heart failure at hospitals affiliated to Kerman University of Medical Sciences, Iran, during 2012. Nurs. Pract. Today 3(2), 51–6 (2016).
Jovanić, M., Zdravković, M., Stanisavljević, D. & Jović, Vraneš A. Exploring the importance of health literacy for the quality of life in patients with heart failure. Int. J. Environ. Res. Public Health 15(8), 1761 (2018).
DeWolfe, A. et al. Depression and quality of life among heart failure patients in Georgia, Eastern Europe. Congest. Heart Fail. 18(2), 107–11 (2012).
Jeong, Y., Yu, H. & Hwang, B. Self-care behaviors mediate the impacts of social support and disease knowledge on health-related quality of life in patients with heart failure. Clin. Nurs. Res. https://doi.org/10.1177/10547738221092864 (2022).
Yaghoubi, A. et al. Quality of life in cardiovascular patients in Iran and factors affecting it: A systematic review. J. Cardiovasc. Thorac. Res. 4(4), 95 (2012).
Audi, G. et al. Factors affecting health related quality of life in hospitalized patients with heart failure. Cardiol. Res. Pract. 2017, 4690458 (2017).
Costa, L. L., Islam, M. S., Anowar, M. N. & Latif, M. A. Quality of life of chronic heart failure patients. Open J. Nurs. 10(9), 831–57 (2020).
Erceg, P. et al. Health-related quality of life in elderly patients hospitalized with chronic heart failure. Clin. Interv. Aging 8, 1539 (2013).
Pour, E. P., Fayazee, S. & Latifi, M. Examining quality of life and its related factors in patients with chronic heart failure admitted to hospitals in Ahvaz in 2015. Jundishapur J. Chronic Dis. Care https://doi.org/10.17795/jjcdc-33519 (2016).
Barutcu, C. D. & Mert, H. The relationship between social support and quality of life in patients with heart failure. JPMA J. Pak. Med. Assoc. 63(4), 463–7 (2013).
Soleimani, M. A., Zarabadi-Pour, S., Motalebi, S. A. & Allen, K.-A. Predictors of quality of life in patients with heart disease. J. Relig. Health 59(4), 2135–48 (2020).
Koirala, B., Himmelfarb, C. R. D., Budhathoki, C. & Davidson, P. M. Heart failure self-care, factors influencing self-care and the relationship with health-related quality of life: A cross-sectional observational study. Heliyon 6(2), e03412 (2020).
Chung, M. L., Moser, D. K., Lennie, T. A. & Frazier, S. K. Perceived social support predicted quality of life in patients with heart failure, but the effect is mediated by depressive symptoms. Qual. Life Res. 22, 1555–63 (2013).
Tsabedze, N. et al. The prevalence of depression, stress and anxiety symptoms in patients with chronic heart failure. Int. J. Ment. Health Syst. https://doi.org/10.1186/s13033-021-00467-x (2021).
Son, Y.-J. et al. Factors associated with health-related quality of life in elderly Korean patients with heart failure. J. Cardiovasc. Nurs. 27(6), 528–38 (2012).
Alemoush, R. A., Al-Dweik, G. & AbuRuz, M. E. The effect of persistent anxiety and depressive symptoms on quality of life among patients with heart failure. Appl. Nurs. Res. 62, 151503 (2021).
Aburuz, M. E. Anxiety and depression predicted quality of life among patients with heart failure. J. Multidiscip. Healthc. 11, 367–73 (2018).
Comín-Colet, J., Martín Lorenzo, T., González-Domínguez, A., Oliva, J. & Jiménez Merino, S. Impact of non-cardiovascular comorbidities on the quality of life of patients with chronic heart failure: A scoping review. Health Qual. Life Outcomes 18, 1–13 (2020).
Kato, N. et al. Quality of life as an independent predictor for cardiac events and death in patients with heart failure. Circul. J. 75(7), 1661–9 (2011).
Loo, D. W. Y., Jiang, Y., Koh, K. W. L., Lim, F. P. & Wang, W. Self-efficacy and depression predicting the health-related quality of life of outpatients with chronic heart failure in Singapore. Appl. Nurs. Res. 32, 148–55 (2016).
Alaloul, F., AbuRuz, M. E., Moser, D. K., Hall, L. A. & Al-Sadi, A. Factors associated with quality of life in Arab patients with heart failure. Scandinavian J. Caring Sci. 31(1), 104–11 (2017).
Fotos, N. V. et al. Health-related quality of life of patients with severe heart failure. A cross-sectional multicentre study. Scandinavian J. Caring Sci. 27(3), 686–94 (2013).
Fritschi, C. & Redeker, N. S. Contributions of comorbid diabetes to sleep characteristics, daytime symptoms, and physical function among patients with stable heart failure. J. Cardiovasc. Nurs. 30(5), 411 (2015).
Olivera, M. J., Fory, J. A. & Buitrago, G. Comparison of health-related quality of life in outpatients with Chagas and matched non-Chagas chronic heart failure in Colombia: A cross-sectional analysis. Am. J. Trop. Med. Hyg. 104(3), 951 (2021).
Polikandrioti, M. et al. Assessment of quality of life and anxiety in heart failure outpatients. Arch. Med. Sci.-Atheroscl. Dis. 4(1), 38–46 (2019).
Eskandari, S., Heravi-Karimooi, M., Foroughan, M., Ebadi, A. & Kharameh, Z. T. Quality of life in heart failure patients using the Minnesota Living with Heart Failure Questionnaire (MLHF). Payesh (Health Monitor) 15(5), 559–66 (2016).
Perera A. What is the Hawthorne effect. Simply Psychology. 2021.
Acknowledgements
We would like to thank all staff members of St. Paul Hospital Millennium Medical College and St. Peter Specialised Hospital who cooperated during the ethical approval of the study. We would also like to express our gratitude to the data collectors and the respected respondents who took part in this study.
Funding
This study was funded by University of Technology Sydney (UTS). It is part of a PhD thesis by HM. HM is a higher degree research candidate at UTS, funded by the International Research Training Program (IRTP). The IRTP is a commonwealth scholarship funded by the Australian government and the Department of Education and Training.
Author information
Authors and Affiliations
Contributions
All authors (H.M., P.S. and A.W.) were involved in the conception, study design, methods, data collection, analysis, and interpretation. All authors have read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mulugeta, H., Sinclair, P.M. & Wilson, A. Health-related quality of life and its influencing factors among people with heart failure in Ethiopia: using the revised Wilson and Cleary model. Sci Rep 13, 20241 (2023). https://doi.org/10.1038/s41598-023-47567-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47567-x
- Springer Nature Limited