Abstract
Limited information regarding the anatomical and visual prognosis of macular telangiectasia (MacTel) type 2 in the Asian population is currently available. Herein, we conducted a retrospective longitudinal analysis of Japanese patients diagnosed with MacTel type 2. Disease progression was evaluated using the Simple MacTel Classification developed by Chew EY et al. in 2023, and its association with visual changes was analyzed. Sixteen eyes of eight Japanese patients were included in the study, with an average follow-up period of 8.2 ± 3.9 years (range, 2.2–14.0). At the initial visit, 7 (44%) and 5 (31%) eyes were classified as Grade 2 (central ellipsoid zone break) and Grade 3 (noncentral pigment), respectively. The proportion of eyes that progressed by 1 or 2-steps in grade after 1, 3, 5, 8, and 12 years was 0%, 14%, 43%, 70%, and 100%, or 0%, 7%, 7%, 30%, and 75%, respectively. The visual acuity significantly deteriorated during the follow-up period, particularly in the two eyes with full-thickness macular holes (FTMH). Three out of 7 patients exhibited low serum serine concentrations, although no apparent correlation with anatomical or visual outcomes was observed. Overall, this cohort demonstrated chronic disease progression, both anatomically and functionally, in eyes with MacTel type 2, with FTMH potentially associated with greater visual loss.
Similar content being viewed by others
Introduction
Macular Telangiectasia Type 2 (MacTel) is a rare progressive degenerative disorder that predominantly affects individuals aged 40–60 years and involves the bilateral macular retina1,2. The estimated prevalence of MacTel ranges from 0.0045 to 0.1%3,4 The typical retinal pathology of MacTel begins in the parafoveal temporal region and extends superiorly and nasally, often presenting with grayish retinal opacities, crystalline-like retinal deposits, and right-angle venules. As the disease progresses, neovascularization, lamellar hole, and full-thickness macular hole (FTMH) can occur2,5. Characteristic anatomic findings include dilated parafoveal retinal capillaries with fluorescein leakage on fluorescein angiography, as well as useful imaging tools such as fundus autofluorescence (FAF) and blue light reflectance imaging (BRI) for assessing retinal involvement in MacTel. Optical coherence tomography (OCT) often reveals intraretinal cavities, sub-internal limiting membrane (ILM) spaces, downward displacement of inner retinal layers, and the loss of the inner/outer segment junction6.
Recent insights have revealed that degenerative changes in Müller cells underlie the pathology of MacTel7. Additionally, studies have implicated the accumulation of neurotoxic metabolite, deoxysphingolipids, in the retina, which is associated with low levels of serine and glycine in the retina8.
Previous reports on the long-term course of MacTel have indicated that choroidal neovascularization (CNV), although rare, can lead to significant visual impairment. Even cases without CNV have been associated with milder visual decline2,9,10. More recently, pigmentation and ellipsoid zone (EZ) loss have been recognized as important factors in visual impairment and have been incorporated into a simplified classification system11.
It is important to note that previous reports have primarily focused on cohorts of Caucasian individuals, with limited information available regarding Asian populations. Only a few studies, such as a cross-sectional study12 or a short-term observation within 2 years13, have explored MacTel in Asian populations.
In this report, we present a longitudinal analysis of visual acuity and retinal morphology progression in Japanese patients with MacTel, with an average follow-up duration of 8 years. The objectives of this study are to investigate whether MacTel cases in our cohort exhibit progression according to the simplified classification system and to explore potential racial differences in the characteristics of progression.
Results
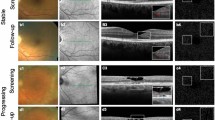
The study included sixteen eyes of eight Japanese patients, consisting of three men and five women. Table 1 presents the demographic and systemic characteristics. The mean age at the initial examination was 62.5 ± 7.2 years (range, 53–70). Out of the patients, two (25%) had diabetes, one (13%) had hypertension, and three (38%) had dyslipidemia. The mean follow-up time was 8.2 ± 3.9 years (range, 2.2–14.0). Table 2 summarizes the visual and anatomical findings. Supplementary Figure S1 displays fundus photographs and OCT B-scans with infrared fundus images using Spectralis OCT for both eyes in cases 1–8.
Disease progression
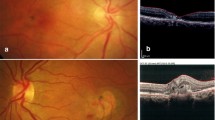
According to the Simple Classification system, the initial examination revealed 4, 7, 5, or 0 eyes classified into grade 0, 2, 3, or 4, respectively. Likewise, at the last examination, 3, 4, 5, or 4 eyes were classified into the same grades. Figure 1 illustrates a representative case of MacTel type 2 in the current cohort. None of the eyes exhibited exudative MNV (grade 6) during the follow-up period, although nonexudative MNV was observed in 2 eyes of one patient. FTMH was observed in two eyes, with one eye developing FTMH 3 years after the initial visit. Subsequently, pars plana vitrectomy was performed, resulting in the closure of the hole. No patients underwent treatments such as laser therapy or administration of antiangiogenic agents during the follow-up period. The longitudinal changes in the grade on the Simple Classification system are depicted in Fig. 2. At year 1, the grades of each eye were similar to the baseline. However, at year 3 or longer, a number of eyes exhibited progression from grade 0–3 to grade 2–4. The proportion of eyes showing progression of 1 or more steps or 2 or more steps in grade after 1, 3, 5, 8, and 12 years was 0%, 14%, 43%, 70%, and 100%, or 0%, 7%, 7%, 30%, and 75%, respectively (Fig. 3). Notably, no eyes exhibited grade 5 (central pigment) or 6 (exudative MNV) at the initial visit or at any subsequent visits. Furthermore, among the 8 patients, 5 (63%) displayed grade 2 (central EZ break) or more lesions bilaterally, while the remaining 3 (37%) patients exhibited asymmetrical manifestation, with one eye classified as grade 0 and the other eye classified as grade 2 or more.
Representative case of Matel type 2 in the current cohort. Seventy-year-old woman (Case 1) presented with visual impairment. Best-corrected decimal visual acuity in the left eye was (0.8). Fundoscopy revealed grayish change in the temporal macula (a), showing hyperfluorescence in the fluoresceine angiography (b). Ellipsoid zone loss involving the center with inner and outer intraretinal cavity were detected OCT, corresponding to Grade 2 (c). After 14 years, noncentral hyperpigmentation was seen (d). In OCT, hyperreflectivity at the outer retina was observed (e). Decimal visual acuity mildly decreased to (0.6).
The grade in Simple Classification System11 of each eye (n = 16) at the baseline, 1, 3, 5, 8, or 12 years.
Visual outcome
Regarding the visual outcome, the mean logarithm of minimum angle of resolution (logMAR) was 0.09 ± 0.20 at the initial visit and 0.23 ± 0.32 at the last visit, indicating a significant deterioration (p = 0.006, Table 2). Figure 4 illustrates the longitudinal changes in logMAR for each eye. The proportion of eyes showing a visual decline of 0.1 logMAR or more or 0.2 logMAR or more after 1, 3, and 5 years was 13%, 29%, and 43%, or 0%, 14%, and 29%, respectively (Fig. 5). At the last visit, one patient had both eyes with 0.4 logMAR (equivalent of 20/50) or worse, and none had 0.1 logMAR (equivalent of 20/200) or worse in both eyes. Visual prognosis tended to be distinct between eyes with and without FTMH. The eyes with FTMH showed a moderate or severe decrease of 0.3 logMAR or greater (indicated by the yellow and green lines in Fig. 4). In those without FTMH, visual decline was not clearly observed in the short-term but a mild decrease (within 0.3 logMAR) was seen in the long-term follow-up. There was a positive association between grade progression and the proportion of eyes with a visual change of 0.1 logMAR or greater or 0.2 logMAR or greater (p = 0.020 or 0.031, respectively).
Blood test
Blood test results were available for 7 patients (Table 1). Abnormally high serum triglyceride levels or low serum serine levels were observed in 2 or 3 patients, respectively. Three out of the 7 patients showed low serum serine concentration, without any apparent correlation with anatomical or visual outcomes.
Discussion
In this current study, we investigated the longitudinal anatomical progression and visual outcomes in patients with MacTel type 2 over an average follow-up period of 8 years. Using the Simple Classification system, we observed disease progression in multiple eyes during this time. At the last visit, there was a significant decline in mean visual acuity, and the proportion of eyes experiencing visual loss increased with the length of the follow-up period.
In the current analysis, Simple MacTel Classification system11 was used to assess disease progression because it provides information on the rate of progression within 1–5 years for each grade, as well as the association between grade progression and visual loss. Previous research11 indicated that 1-step or 2-steps progression over 5 years occurred in approximately 30–40% or 5–25%, respectively, of eyes classified as grade 0, 2, or 3, where the eyes in the current study were classified at the initial examination. It was compatible with the findings of our study, showing 1 or more or 2 or more progression in 5 years was 43% or 7%, respectively. These results suggest that disease progression in this population can be similar according to Simple Classification system. Additionally, our study revealed the progression over 8 or 12 years increased with time, suggesting the disease progression may not slow down even after a decade.
Furthermore, the present study showed that 37% of patients exhibited asymmetrical manifestation. Although MacTel 2 is usually bilateral, some patients showed asymmetricity14,15. Clemons et al. reported in the large-scale cohort study that many of the image characteristics and visual acuity had small to moderate agreement between eyes16.
As for visual acuity, a large-scale observational study among MacTel Project revealed that, after 5 years, there was a 27% probability of losing 10 or more letters, and a 15% probability of losing 15 or more letters17. Conversely, a previous case series involving 16 eyes of 8 Japanese patients13 indicated a more favorable visual outcome, with either improvement or maintenance during the follow-up period, although the mean follow-up time was less than 2 years. In our current study, which had a mean follow-up time of 8 years, it was observed that visual acuity significantly declined at the last examination, and 29% of eyes exhibited a decline of 0.2 logMAR or more after 5 years. These findings align with the previous report17. The current study also revealed that as the disease grade progressed, a greater proportion of eyes experienced visual loss, consistent with previous findings by Chew et al.11. These results suggest a similar outcome to the MacTel Project cohort16, which primarily comprised of Caucasian participants, with regards to visual changes over a longitudinal observation for 5 years or more. However, additional research involving a larger population of Asian individuals is necessary to validate this hypothesis. It is worth noting that the visual prognosis appeared to differ between eyes with and without FTMH. Eyes with FTMH exhibited moderate or severe visual decline (0.3 logMAR or greater), consistent with findings from a cross-sectional multicenter study18, which reported the possibility of severe vision loss in eyes with FTMH. Conversely, eyes without FTMH did not demonstrate significant visual decline, but did exhibit mild deterioration (within 0.3 logMAR) during the long-term follow-up, consistent with a previous report10.
In this study, we observed a decrease in serum serine levels in three patients with no apparent clinical differences, including the rate of progression, between eyes with decreased serine levels and those with normal levels. To the best of our knowledge, there have been no reports investigating the association between serum serine levels and longitudinal clinical course. Previous studies have suggested an association between abnormalities in serine-glycine metabolism and the onset of MacTel type 2, with the underlying abnormal synthesis of deoxysphingolipids being essential19. Deoxysphingolipids are known to exhibit neurotoxicity and have been shown to negatively correlate with serine levels in the serum of MacTel type 2 patients8. Therefore, monitoring the levels of deoxysphingolipids that may be more directly involved in the pathophysiology of MacTel type 2 is considered helpful.
The study has several limitations. It was a retrospective nonrandomized design, and the numbers of cases were relatively small. There might be some biases with a limited number of subjects in the current analysis and further analysis with a much greater number of patients by, for example, a multicenter study is required to confirm the findings from the current analysis. The follow-up time of each patient was variable, and retinal function was assessed only with visual acuity, not a microperimetric test. Therefore, a more extensive longitudinal study with a larger sample size will be necessary to validate the present findings.
In conclusion, we performed a longitudinal study to observe clinical characteristics of East Asian patients with MacTel type 2 over an average follow-up duration of 8 years. Our findings revealed significant progression in visual acuity and disease grade, which correlated with the length of the follow-up period. Notably, cases that developed FTMH demonstrated a substantial decline in visual acuity, while cases without FTMH experienced a noticeable but mild deterioration. Moreover, our analysis did not show any apparent association between serum serine levels and clinical progression.
Methods
Design
This retrospective study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the institutional review board (IRB) of the University of Tokyo (No. 2217). The requirement for written informed consent was waived by the IRB. However, participants who did not authorize the use of their medical records for research were excluded from the study.
Participants
We included patients who initially visited the Specialized Outpatient Clinic for Macular Diseases at the University of Tokyo Hospital between May 2005 and May 2021 and were diagnosed with MacTel type 2. They underwent a standard examination that included measurement of best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, color fundus photography (CFP) using TRC 50DX retinal camera (Topcon, Tokyo, Japan), and spectral domain optical coherence tomography (SD-OCT) using 3D-OCT 1000 (Topcon, Tokyo, Japan) or Spectralis OCT (Heidelberg Engineering, Heidelberg, Germany). Fundus autofluorescence imaging and blue light reflectance were acquired with Heidelberg Retina Angiograph 2 (Heidelberg Engineering, Heidelberg, Germany). BCVA was measured using the Landolt C chart, and values were converted from decimal acuity to logarithm of minimal angle of resolution (logMAR). All patients underwent fluorescein angiography (FA). OCT angiography (RTVue XR Avanti, Optovue Inc., Fremont, CA, USA) was performed to examine the development of macular neovascularization (MNV). Diagnosis of MacTel type 2 was based on characteristic findings on fundoscopy, OCT, and/or FA2,5. Multimodal imaging was also used to rule out other diseases, such as diabetic retinopathy, radiation retinopathy, retinal vein occlusion, tamoxifen retinopathy, or macular dystrophy, in order to exclude them from the analysis. The presence of diabetes, hypertension, or dyslipidemia was determined based on the patients' medication. Serum concentrations of triglyceride, total cholesterol, LDL cholesterol, serine, glycine, alanine, and beta-alanine were reviewed from the medical chart.
Evaluation of anatomical findings
To evaluate the anatomical findings obtained through multimodal imaging, we utilized the Simple MacTel Classification system developed by Chew EY and coworkers in 2023 as part of the MacTel Project11. In the system, three anatomical findings were featured as key for classification: OCT hyper-reflectivity, pigment, and EZ break. The severity of the grade is determined based on the decline in BCVA. The system consists of six grades; grade 0 (no lesions), grade 1 (noncentral EZ break), grade 2 (central EZ break), grade 3 (noncentral pigment), grade 4 (OCT hyper-reflectivity), grade 5 (central pigment), and grade 6 (neovascularization with exudative changes). Annual relative risk of progression over 5 years for visual acuity and for progression along the scale were also reported11. Additionally, we assessed the development of Full-thickness macular hole (FTMH) and MNV using SD-OCT and OCTA.
Statistical analysis
We analyzed various demographic factors including age, sex, systemic comorbidities, and laboratory data. The logMAR and the grades on the Simple Classification System were longitudinally investigated. The logMAR changes between the initial and final examinations were analyzed using a mixed model. We also analyzed the association between grade progression and the proportion of eyes with visual changes of 0.1 logMAR or greater, or 0.2 logMAR or greater, from the initial to the last visit using Cochran-Armitage trend analysis. JMP Pro version 16 (SAS Institute Inc.) was used for the statistical analysis. Statistical significance was set at p < 0.05.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Gass, J. D. & Oyakawa, R. T. Idiopathic juxtafoveolar retinal telangiectasis. Arch. Ophthalmol. 100, 769–780 (1982).
Gass, J. D. M. & Blodi, B. A. Idiopathic juxtafoveolar retinal telangiectasis: Update of classification and follow-up study. Ophthalmology 100, 1536–1546 (1993).
Klein, R. et al. The prevalence of macular telangiectasia type 2 in the Beaver Dam eye study. Am. J. Ophthalmol. 150, 55-62.e2 (2010).
Aung, K. Z., Wickremasinghe, S. S., Makeyeva, G., Robman, L. & Guymer, R. H. The prevalence estimates of macular telangiectasia type 2: The Melbourne Collaborative Cohort Study. Retina 30, 473–478 (2010).
Charbel Issa, P. et al. Macular telangiectasia type 2. Prog. Retin. Eye Res. 34, 49–77 (2013).
Pauleikhoff, D., Pauleikhoff, L. & Chew, E. Y. Imaging endpoints for clinical trials in MacTel type 2. Eye 36, 284–293 (2022).
Newman, E. & Reichenbach, A. The Müller cell: A functional element of the retina. Trends Neurosci. 19, 307–312 (1996).
Gantner, M. L. et al. Serine and lipid metabolism in macular disease and peripheral neuropathy. N. Engl. J. Med. 381, 1422–1433 (2019).
Watzke, R. C. et al. Long-term juxtafoveal retinal telangiectasia. Retina 25, 727–735 (2005).
Marsonia, K., Kiran Chandra, K., Ali, M. H., Chhablani, J. & Narayanan, R. Long term follow-up of visual acuity and incidence of subretinal neovascularization in Mactel Type 2 in 82 Eyes. Semin. Ophthalmol. 37, 136–141 (2022).
Chew, E. Y. et al. Macular telangiectasia type 2: A classification system using multimodal imaging MacTel project report number 10. Ophthalmol. Sci. 3, 100261 (2023).
Kim, Y. H. et al. Optical coherence tomographic features of macular telangiectasia type 2: Korean Macular telangiectasia type 2 study—Report no. 1. Sci. Rep. 10, 16594 (2020).
Shinkai, A. et al. Morphological features of macular telangiectasia type 2 in Japanese patients. Graefes Arch. Clin. Exp. Ophthalmol. 259, 1179–1189 (2021).
Charbel Issa, P., Heeren, T. F. C., Kupitz, E. H., Holz, F. G. & Berendschot, T. T. J. M. Very early disease manifestations of macular telangiectasia type 2. Retina 36, 524–534 (2016).
Bruè, C., Tseng, J. J., Barbazetto, I., Lima, L. H. & Yannuzzi, L. A. Peculiar manifestation of macular telangiectasia type 2. Retin. Cases Brief Rep. 5, 309 (2011).
Clemons, T. E. et al. Baseline characteristics of participants in the natural history study of macular telangiectasia (MacTel) MacTel project report no. 2. Ophthalmic Epidemiol. 17, 66–73 (2010).
Peto, T. et al. Correlation of clinical and structural progression with visual acuity loss in macular telangiectasia type 2: MacTel project report no. 6–The MacTel research group. Retina 38, S8–S13 (2018).
Heeren, T. F. C. et al. Macular telangiectasia type 2: Visual acuity, disease end stage, and the MacTel area: MacTel project report number 8. Ophthalmology 127, 1539–1548 (2020).
Eade, K. et al. Serine biosynthesis defect due to haploinsufficiency of PHGDH causes retinal disease. Nat. Metab. 3, 366–377 (2021).
Acknowledgements
We would like to thank Asako Ogawa-Murano, Kayoko Komatsu, Shoko Abe, Natsuki Maetani for technical assistance.
Author information
Authors and Affiliations
Contributions
R.O. and K.T. contributed to the conception or designed the study and the acquisition of the data. R.O. and K.T. wrote the main manuscript. S.A., T.A., K.K., K.A., R.F., and T.I. contributed the analysis and the interpretation of the data. All authors read and approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Totsuka, K., Aoki, S., Arai, T. et al. Longitudinal anatomical and visual outcome of macular telangiectasia type 2 in Asian patients. Sci Rep 13, 18954 (2023). https://doi.org/10.1038/s41598-023-46394-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46394-4
- Springer Nature Limited