Abstract
Fungal infections are a challenging to treat cutaneous condition. Approximately 20–25% of humans are affected by superficial fungal infections that invade and multiply within keratinized tissues. To compare the efficacy of either terbinafine or itraconazole orally versus the combination of the two drugs in the treatment of recalcitrant dermatophytosis. The current study included 45 patients with recalcitrant dermatophytosis who were distributed into 3 groups (each of 15 patients); Group A received terbinafine 250 mg twice a day for 4 weeks. Group B received itraconazole 200 mg twice a day for 4 weeks. Group C received terbinafine 250 mg once daily and itraconazole 200 mg once daily for 4 weeks. The patients were followed up for 12 weeks after initiation of treatment by clinical and microbiological assessment to determine the cure rate. At the end of twelve weeks, 12 (80%) patients in group A; 13 (86.7%) patients in group B and 15 (100%) patients in group C were completely cured. Despite of cure rates being higher in the combined group C; yet results were not statistically significant (p = 0.207). Clinical cure rates were non significantly higher in itraconazole + terbinafine combined group (p = 0.207). Combination of terbinafine and itraconazole had a higher clinical and mycological cure rate when compared to the use of either drug alone as monotherapy. Further randomized, multicenter, large cohort studies are warranted to validate the use of combination antifungal treatments.
Similar content being viewed by others
Introduction
Fungal infections are a challenging to treat common cutaneous condition. Approximately 20–25% of humans are affected by superficial fungal infections which can invade and multiply within keratinized tissues1.
Systemic therapy for dermatophytosis is indicated for extensive, recurrent and non responsive cases. Moreover; skin infections involving multiple sites and non responsive to topical treatment require using systemic antifungals. Wide variety of systemic antifungals is available for the treatment of tinea which consists of terbinafine, griseofulvin, itraconazole and fluconazole. Out of these, the commonly prescribed drugs are itraconazole and terbinafine as the other two require a longer duration2.
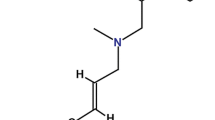
Owing to its mycological properties, terbinafine acting by inhibiting the enzyme squalene epoxidase was considered a first line treatment of choice when used in daily doses of 250 mg for two weeks and achieved cure rates of up to 90%. In recent years; terbinafine resistance emerged from overuse of the drug and resulted in increased clinical failures and relapses3.
On the other hand, itracanozole used at daily doses of 100 mg or 200 mgs for two weeks or one week has shown good results in treating dermatophytosis by inhibiting ergosterol synthesis4.
In recent years, there had been an increased resistance to systemic antifungals. And there had been a quest for finding an effective treatment with minimal relapse rates. A combination therapy of systemic antifungal drugs with different mechanism of action can enhance the cure rate and helps prevent drug resistance based on the concept of synergistic and additive effects of two or more drugs5.
Taking into consideration the lack of studies in literature on combination treatments, we aimed to compare the efficacy of either terbinafine or itraconazole orally versus the combination of the two drugs in the treatment of recalcitrant dermatophytosis.
Patients and methods
This was a prospective randomized observational study that was carried out at the outpatient clinic of dermatology and venerology department's outpatient clinic et al.-Azhar University Hospital in New Damietta, Egypt. The study was conducted over nine months duration, from January 2023 till August 2023.
Sample size
Sample size calculation was based on cure rate between different treatment lines of recalcitrant dermatophytosis using single or combined treatment retrieved from previous research by Singh et al., 2020 Using G*power version 3.0.10 to calculate sample size based on difference of 55.8%, 2-tailed test, α error = 0.05 and power of 80.0%; a sample size of 12 patients was determined sufficient for each group.
The enrolled patients were randomly categorized into three groups, A, B and C, each with 15 patients. Group a (ɳ = 15) received terbinafine 250 mg twice a day for 4 weeks. Group b (ɳ = 15) received itraconazole 200 mg twice a day for 4 weeks while group c (ɳ = 15) received terbinafine 250 mg once daily and itraconazole 200 mg once daily for 4 weeks. Randomization was done via a computer-generated random number sequence using the MS Excel software and one of the author assigned participants to the interventions.
Subjects were included if they fulfilled recalcitrance of dermatophyte infection based on the following criteria; complaining of cutaneous dermatophytosis for more than 6 months to 1 year with or without recurrence in spite of being adequately treated; those with two or more episodes of dermatophyte infections in the previous 12 months; recurrence of lesions within few weeks (< 6 weeks) after completion of the treatment and adults with relapsing dermatophytes after an infection-free interval of (6–8 weeks) following clinical cure.
The cases with the following criteria were excluded; immuno-compromised patients, patients with known active liver, cardiac, renal, or neurological diseases, patients with uncontrolled diabetes mellitus, a history of hypersensitivity to terbinafine or itraconazole, pregnant or lactating females, patients who had received oral antifungal medication or topical antifungal treatment during the previous 4 weeks and any patient with secondary bacterial infections on top of the dermatophytic lesion.
The study gained approval from the local ethical committee of the faculty of medicine, Al-Azhar University (DFM-IRB00012367-22-12-001). All patients felt free to withdraw from the study at any time point, based on their request. Patient confidentiality was preserved, and the collected data were used only for scientific purposes.
The cases were subjected to the following: history taking (including demographic data, analysis of the current condition and associated medical or surgical data) and clinical examination to determine the lesions extension, associated symptoms and to exclude any systemic diseases.
Clinical and mycological assessments
Various clinical signs and symptoms (scaling, pruritis, erythema) were rated according to a four-point scale from 0 to 3 (0 = absent, 1 = mild, 2 = moderate and 3 = severe). Patients were checked for residual changes or recurrence two weeks; four weeks (after treatment ended), eight weeks, and twelve weeks after treatment had begun.
Sample collection
The diagnosis was made by a clinical examination and then confirmed by a microbiological analysis. Direct microscopy with a 10% potassium hydroxide (KOH) mount was used for analyzing skin scrapings. Each smear was examined in detail at 400 × magnification at enrollment and at the end of the fourth week. A full blood picture was taken in addition to liver and renal function tests.
Follow up
A clinical evaluation was performed during each visit. Patients were monitored for at least 12 weeks post treatment to look for signs of recurrent dermatophytosis. The therapy's effectiveness was assessed every four weeks. When there were no visible symptoms (such as scaling, erythema, and pruritus) and a negative KOH, patients were deemed cured.
At each visit, photographic pictures were collected and compared to prior images to determine clinical response; Treatment failure was defined as a lack of significant (> 50%) clinical improvement after 4 weeks of treatment or the emergence of new lesions/extension of old lesions at any time throughout treatment. Treatment efficacy was defined by complete cure that includes both clinical cure (clinically completely normal skin) and mycological cure (negative KOH microscopy).
Statistical analysis of data
The data collected were coded, processed and analyzed with SPSS version 27 for Windows® (Statistical Package for Social Sciences) (IBM, SPSS Inc, Chicago, IL, USA). Qualitative data as number (frequency) and percent was presented. The Chi-Square test (or Monte-Carlo test) made the comparison between groups.
The Kolmogorov–Smirnov test tested quantitative data for normality. Parametric data were expressed as median ± SD while the non-parametric data were expressed as median (Range). To compare three groups with normally distributed quantitative variables, one-way analysis of the variance (One-way ANOVA) test was used and Kruskal–Wallis test was used if the data were abnormally distributed. Stuart Maxwell testwas used to compare between two dependent groups with qualitative variable (of more than two levels). For all tests, P values < 0.05 are considered significant.
Ethics approval
This study protocol was reviewed and approved by ethics committee on human research by Al Azhar Damietta faculty of medicine (DFM-IRB 00012367-22-12-001). All methods were performed in accordance with relevant guidelines and regulations.
Consent to participate
Written informed consents were received from participants upon explanation of the study.
Results
60 cases were assessed for eligibility; 45 of which were eligible for the study and 15 were excluded for not fulfilling inclusion criteria. The enrolled patients were randomly categorized into three groups, A, B and C, each with fifteen patients. The patient characteristics were comparable in all the groups. The mean age of the studied groups (A, B and C) was 41.53 ± 15.73, 31.87 ± 13.34 and 39.0 ± 14.19 respectively. Statistically, 82.2% of the overall participants were females. No significant difference was detected regarding gender, occupation, co morbid conditions or family history of dermatophytosis among all groups (P = 0.516) (Table 1).
The most common clinical variant was tinea corporis and cruris. Among group a; 66.7% were diagnosed as tinea cruris and 60% as tinea corporis. For group B; 73.3% tinea cruris and 40% tinea corporis while in group C; 93.3% were tinea cruris and 26.7% tinea corporis. No significant difference among case distribution was noticed in all groups (p = 0.188; p = 0.177) (Table 2).
At the end of twelve weeks, 12 (80%) patients in group A; 13 (86.7%) patients in group B and 15 (100%) patients in group C were completely cured. Despite of cure rates being higher in the combined group C; yet results were not statistically significant (p = 0.207). Clinical cure rates were non significantly higher in itraconazole + terbinafine combined group (p = 0.207). GIT upset was the most frequent adverse event reported by almost all patients in all groups. Other side effects were minimal and non significant among all groups (Table 3).
Recurrence rates assessed at 4, 8 and 12 weeks respectively showed no significance among all groups (p = 0.760, p = 1, p = 0.102 respectively). Following treatment, scaling, pruritis and erythema scores were significantly improved as compared to the baseline values in all groups (p < 0.03, p < 0.001, p < 0.001 respectively), slightly higher non significant improvement was noted in group C. This result indirectly implies that the clinical features of patients at the end of treatment improved in all groups due to the treatment given (Table 4; Figs. 1, 2).
Clinical image of a twenty five years old male complaining of (a) recalcitrant tinea corporis of the back before treatment, (b) two weeks after treatment and (c) four weeks after treatment (d) Positive microscopic examination using koh showing (large amount of branching fungal hyphae) and (e) Negative microscopic examination using KOH (absent fungal hyphae) four weeks after treatment.
Clinical image of a forty years old female complaining of (a) recalcitrant tinea corporis of the abdomen before treatment, (b) two weeks after treatment and (c) four weeks after treatment (d) Positive microscopic examination using koh showing (large amount of branching fungal hyphae) and (e) Negative microscopic examination using KOH (absent fungal hyphae) four weeks after treatment.
Discussion
In this study, combination of terbinafine with itraconazole produced non significantly higher clinical cure rates (p = 0.207) as compared to itraconazole and terbinafine monotherapy. Despite of cure rates being higher in the combined group C; yet results were not statistically significant (p = 0.207).
In the current study, the mean age of the studied groups was 41.53 ± 15.73, 31.87 ± 13.34 and 39.0 ± 14.19 for groups A, B & C, respectively. The majority of the patients were females (82.2%). This is was in accordance with the study by Ramesh et al.6 who reported a female prevalence of (64.9%). In other studies, by Singh et al.7 and Sharma et al.8 male predominance was reported to be (74.1% and 70%; respectively). The difference in gender differences could be to the nature of the study population, cultural differences or sample size variance; yet female prevalence could be related to the cosmetic concern, impact or stigma of fungal conditions on female population.
In the past, terbinafine, in the dosage of 250 mg/day, has shown consistent efficacy against dermatophytosis, achieving more than 90% cure rates at a dose of 250 mg/day when admonstered9. Recently resistance to terbinafine treatment in the previously mentioned doses has led some physicians to increase doses or provide combination therapies10.
In this study, itraconazole and terbinafine achieved comparable cure rates when used alone and achieved less non significant cure rates to the itraconazole + terbinafine combination. This was comparable to Shah et al. who reported significant comparable cure rates of itraconazole and terbinafine when used alone11. Singh et al. reported itraconazole to be more effective when compared to terbinafine7.
Majid et al. achieved only 43% cure rate after two weeks of daily 250 mg terbinafine oral treatment in dermatophytosis12. Other studies showed the mycological cure rate of terbinafine as 74% and 71% respectively13,14. In another study, three-week therapy of terbinafine 250 mg/day showed a 35% cure rate, compared to 50% cure rate using itraconazole 200 mg/day8.
The practice of combination therapy has not been widely studied and published despite of being much practiced in many medical settings. The current study showed a comparatively better complete clinical cure rate with terbinafine and itraconazole (100%). This value was much higher compared to the study by Ramesh et al.6 that reported 48.3% complete cure and more comparable to the studies conducted by Singh et al. and Sharma P et al., that reported 79.2% and 90% clinical and mycological cure rate after three weeks and four weeks of combination therapy respectively7,8.
Other studies assessed combination therapies for recurrent fungal infections15,16. One study demonstrated that terbinafine with sertaconazole achieved a better but non significant efficacy than itraconazole and sertaconazole combination. Successful complete response without recurrence was obtained following combination of oral (20 mg/day) and itraconazole (200 mg/day) along with daily application of topical sertaconazole15. Another recent study reported a significant clinical cure in 70% of the (itraconazole + isotretinoin combination) treated recurrent tinea patients when compared to only cure in 56.7% of itraconazole only treated patients16.
The most common side effects with terbinafine are gastric upset, headache, altered taste, altered liver function tests and rash; rarely, it can cause blood dyscrasias and hepatitis. Itraconazole can cause gastric upset, headache, taste alteration, and jaundice, and rarely, it can cause hypokalemia, torsades de pointes, and heart failure. In the current study, gastric upset was the most commonly reported adverse event, while hypersensitivity, loin pain and liver enzymes were unremarkably and non significantly reported among 3 patients in all groups.
The study is limited by its small sample size, female predominance. Mycological culture was not done and follow up durations were short. Moreover; the use of fixed doses represented a limitation. Another limitation was not investigating minimum inhibitory concentration of the combination of the two drugs.
Conclusion
In conclusion combination of the drugs terbinafine and itraconazole had a higher clinical and mycological cure rate when compared to the use of either drug alone as monotherapy. It is possible that the lack of a statistically significant difference is attributable to the small sample size of the cases that were included. Further randomized, multicenter, large cohort studies using in vitro characterization and investigating the minimal inhibitor concentrations of combined antifungal treatment are warranted to validate the use of combination antifungal treatments and establish optimal safe dosage in the management of recalcitrant dermatophytosis.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
All authors confirm all data and materials as well as software applications or custom code support their published claims and comply with field materials.
Abbreviations
- KOH:
-
Potassium hydroxide
References
Bouchara, J. P., Mignon, B. & Chaturvedi, V. Editorial: Dermatophytes and dermatophytoses: A reappraisal for the twenty-first century. Mycopathologia 166(5), 235–237 (2008).
Sahoo, A. K. & Mahajan, R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol. Online J. 7(2), 77–86 (2016).
Wahbah, H. R., Atallah, R. B., Eldahshan, R. M. & Elsaie, M. L. A prospective clinical and trichoscopic study of tinea capitis in children during treatment. Dermatol. Ther. 35(7), e15582 (2022).
Elsaie, M. L. Update on tinea capitis diagnosis and treatment. Cutis 110(5), 238–240 (2022).
Russo, G., Toutous Trellu, L., Fontao, L. & Ninet, B. Towards an early clinical and biological resistance detection in dermatophytosis: About 2 cases of Trichophyton indotineae. J. Fungi 9(7), 733 (2023).
Ramesh, A., Devasena, S. & Mathew, D. Efficacy and safety of oral terbinafine with itraconazole or griseofulvin combination therapy in the management of dermatophytosis: A randomised clinical trial. J. Clin. Diagn. Res. 16(1), 5–8 (2022).
Singh, S. K., Subba, N. & Tilak, R. Efficacy of terbinafine and itraconazole in different doses and in combination in the treatment of tinea infection: A randomized controlled parallel group open labeled trial with clinico mycological correlation. Indian J. Dermatol. 65, 284–289 (2020).
Sharma, P., Bhalla, M., Thami, G. P. & Chander, J. Evaluation of efficacy and safety of oral terbinafine and itraconazole combination therapy in the management of dermatophytosis. J. Dermatol. Treat. 31(7), 749–753 (2020).
George, M. et al. Comparative evaluation of efficacy of terbinafine and itraconazole in treatment of tinea cruris. Int. J. Basic Clin. Pharmacol. 8(7), 1460–1466 (2019).
Osborne, C. S., Leitner, I., Favre, B. & Ryder, N. S. Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine. Antimicrob. Agents Chemother. 49, 2840–2844 (2005).
Shah, B. et al. Comparative evaluation of efficacy and safety of terbinafine and itraconazole in the management of tinea corporis et cruris. IP Indian J. Clin. Exp. Dermatol. 6(3), 231–236 (2020).
Majid, I., Sheikh, G., Kanth, F. & Hakak, R. Relapse after Oral Terbinafine Therapy in Dermatophytosis: A Clinical and Mycological Study. Indian J. Dermatol. 61(5), 529–33 (2016).
Shakya, N. B., Jha, S. M., Dangol, A., Shakya, S. & Shah, A. Efficacy of itraconazole versus terbinafine for the treatment of tineacruris. Med. J. Shree Birendra Hosp. 11(1), 24–26 (2013).
Bhatia, A., Kanish, B., Badyal, D. K., Kate, P. & Choudhary, S. Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin: A prospective, randomized comparative study. Indian J Pharmacol. 51(2), 116–11 (2019).
Ardeshna, K. P., Rohatgi, S. & Jerajani, H. R. Successful treatment of recurrent dermatophytosis with isotretinoin and itraconazole. Indian J. Dermatol. Venereol. Leprol. 82(5), 579–582 (2016).
Khattab, F., Elkholy, B. M., Taha, M., Abd-Elbaset, A. & Fawzy, M. Voriconazole is superior to combined itraconazole/isotretinoin therapy and itraconazole monotherapy in recalcitrant dermatophytosis. Mycoses 65(12), 1194–1201 (2022).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed equally in the production of this work. Z.H, H.M, R.E and M.E designed and performed the research. Z.H, H.M, R.E and M.E performed the work; Z.H, H.M, R.E and M.E analyzed and wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hassaan, Z.R.A.A., Mohamed, H.A.K., Eldahshan, R.M. et al. Comparison between the efficacy of terbinafine and itraconazole orally vs. the combination of the two drugs in treating recalcitrant dermatophytosis. Sci Rep 13, 19037 (2023). https://doi.org/10.1038/s41598-023-46361-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-46361-z
- Springer Nature Limited
This article is cited by
-
Expert Panel Review of Skin and Hair Dermatophytoses in an Era of Antifungal Resistance
American Journal of Clinical Dermatology (2024)