Abstract
Intensive antiplatelet therapy did not reduce recurrent stroke/transient ischaemic attack (TIA) events as compared with guideline treatment in the Triple Antiplatelets for Reducing Dependency after Ischaemic Stroke (TARDIS) trial, but did increase the frequency and severity of bleeding. In this pre-specified analysis, we investigated predictors of bleeding and the association of bleeding with outcome. TARDIS was an international prospective randomised open-label blinded-endpoint trial in participants with ischaemic stroke or TIA within 48 h of onset. Participants were randomised to 30 days of intensive antiplatelet therapy (aspirin, clopidogrel, dipyridamole) or guideline-based therapy (either clopidogrel alone or combined aspirin and dipyridamole). Bleeding was defined using the International Society on Thrombosis and Haemostasis five-level ordered categorical scale: fatal, major, moderate, minor, none. Of 3,096 participants, bleeding severity was: fatal 0.4%, major 1.5%, moderate 1.2%, minor 11.4%, none 85.5%. Major/fatal bleeding was increased with intensive as compared with guideline therapy: 39 vs. 17 participants, adjusted hazard ratio 2.21, 95% CI 1.24–3.93, p = 0.007. Bleeding events diverged between treatment groups in the 8–35 day period but not in the 0–7 or 36–90 day epochs. In multivariate analysis more, and more severe, bleeding events were seen with increasing age, female sex, pre-morbid dependency, increased time to randomisation, prior major bleed, prior antiplatelet therapy and in those randomised to triple vs guideline antiplatelet therapy. More severe bleeding was associated with worse clinical outcomes across multiple physical, emotional and quality of life domains.
Trial registration ISRCTN47823388.
Similar content being viewed by others
Introduction
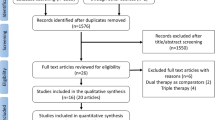
The large Triple Antiplatelets for Reducing Dependency after Ischaemic Stroke (TARDIS) trial compared intensive versus guideline based antiplatelet therapy in patients with acute non-cardioembolic ischaemic stroke or transient ischaemic attack (TIA)1. Although intensive antiplatelet therapy (comprising combined aspirin, clopidogrel and dipyridamole) did not reduce stroke recurrence as compared with guideline therapy (combined aspirin and dipyridamole, or clopidogrel alone), a significant increase in bleeding, and fatal and major bleeding, was present with intensive antiplatelets. Overall, the trial was neutral and there was no net balance in favour of hazard or benefit1.
Long-term antiplatelet therapy is recommended by guidelines for patients with a history of ischaemic stroke or TIA. However, antiplatelet therapy is complicated by bleeding which may be minor (e.g. ecchymoses), severe causing intracranial haemorrhage or requiring blood transfusion, or fatal. The risk of bleeding is increased in certain race-ethnicity groups, and rises with age, and the number and type of antiplatelet agents that are taken2. Understanding the severity and causes of bleeding after acute cerebral ischaemia, including the impact of antiplatelet drugs, may help develop a more patient-centred approach to secondary prevention.
In this pre-planned secondary analysis of the TARDIS trial focussing on bleeding, we aim to assess: bleeding seen with intensive vs. guideline antiplatelet therapy; rates of bleeding; predictors of bleeding using the REACH, S2TOP-BLEED and intracranial-B2LEED3S3 scores3,4,5; and the relationship of bleeding with clinical outcomes after acute cerebral ischaemia.
Results
Baseline participant characteristics by bleeding events
Of the 3096 TARDIS participants, 3072 (99.2%) had data pertaining to presence or absence of bleeding events. Of these, 444 (14.5%) had a bleeding event during the trial period. Bleeding severity was distributed as: fatal 0.4%, major 1.5%, moderate 1.2%, minor 11.4% and none 85.5% (Table 1). In unadjusted univariate analyses, when compared to those with no bleeding event, those with a bleeding event were more likely to be female, have a higher baseline mRS, a longer time from onset to randomisation, a previous major bleed, a lower body weight, and be randomised to triple antiplatelet therapy (Table 2). Trends were observed across the severity of bleeding events for all the significant baseline characteristics in the above unadjusted univariate analyses, i.e. severe bleeding was especially related to these characteristics. Acute neuroimaging markers did not differ between those with and without bleeding events: mass effect was common affecting 44% and 45.9% of participants respectively; and median ASPECTS was 87,9 (Table 3). Background neuroimaging markers also did not differ between those with and without bleeding events: cerebral atrophy in 93.4% and 91% respectively; leukoaraiosis in 43.1% and 41.9% respectively; and old stroke in 60%. The median ‘Brain frailty’ score was 21,3, but did not differ between those with and without bleeding events. Of the bleeding scores, the S2TOP-BLEED scores were higher in those with any bleed compared to those with no bleeding events, but not across severity of bleeding events (Table 2).
Adjusted univariate associations between baseline variables and ordinal bleeding revealed that increasing age, female sex, increasing pre-morbid mRS, longer time from onset to randomisation, prior major bleed, and lower body weight were all associated with more severe bleeding events (Table 4). In adjusted multivariate models, all these baseline variables except body weight maintained statistical significance. Randomisation to triple antiplatelet therapy was associated with more severe bleeding in both univariate and multivariate analyses. Prior antiplatelet therapy was associated with more severe bleeding in multivariate but not univariate models. There were no significant associations between acute and background imaging markers and ordinal bleeding events. The S2TOP-BLEED score at baseline was associated with more severe bleeding in both univariate and multivariate analyses, whilst the S2TOP-BLEED score on treatment was associated with more severe bleeding in univariate but narrowly missed statistical significance in the multivariate model. There were no significant associations noted for other bleeding scores (Table 4).
Bleeding by on-treatment parameters
There was a significant difference across the severity of bleeding events in regard to adherence to all of the first week of randomised treatment and for the S2TOP-BLEED score on treatment (Table 1). Across randomised treatment groups, bleeding events and their severity were significantly more common in those randomised to triple antiplatelet therapy compared to guideline therapy groups (Table 3, Fig. 1A). When the time course of bleeding was split into 0–7, 8–35 and 36–90 day epochs, the bleeding events diverged between the treatment groups in the 8–35 day period (p = 0.009) but not in the earlier or later periods. The time courses for intracranial and gastrointestinal bleeding did not differ by treatment group (Fig. 1B,C). In contrast, predominantly minor ‘other site’ bleeding events split early by treatment group and continued to diverge during the treatment period, then plateaued (Fig. 1).
Time course of bleeding by antiplatelet regimen for epochs 0–7, 8–35 and 36–90 days. (A) Major bleeding; ACD: aspirin + clopidogrel + dipyridamole; AD: aspirin + dipyridamole; C: clopidogrel. (B) Intracranial bleeding; ACD: aspirin + clopidogrel + dipyridamole; AD: aspirin + dipyridamole; C: clopidogrel. (C) Gastrointestinal bleeding; ACD: aspirin + clopidogrel + dipyridamole; AD: aspirin + dipyridamole; C: clopidogrel. (D) Other site bleeding; ACD: aspirin + clopidogrel + di/958pyridamole; AD: aspirin + dipyridamole; C: clopidogrel.
Fatal or major bleeds were relatively infrequent occurring in 39 (2.5%) participants randomised to triple antiplatelet therapy, 12 (1.4%) randomised to clopidogrel, and 5 (0.7%) randomised to aspirin and dipyridamole. Major or fatal bleeding was increased with intensive vs. guideline antiplatelets: 39 vs. 17 participants, adjusted hazard ratio 2.21, 95% CI 1.24–3.93, p = 0.007. Performing subgroup analyses in this bleeding category was not feasible due to the small number of events. Increased numbers of intracranial and extracranial bleeds were seen in those randomised to triple antiplatelet therapy, but no significant associations were noted for composite outcomes ‘stroke or major haemorrhage’ or ‘major adverse cardiovascular event or major haemorrhage’ categories (Table 3).
Ordinal bleeding and clinical outcomes
More severe bleeding was associated with death or deterioration in hospital (Table 5). At day 90, more severe bleeding was associated with increased death and dependency (mRS), increased disability (Barthel Index), worse depression score (Zung) and worse quality of life scores (HSUV and EQ-VAS). When the treatment effect on ordinal bleeding was assessed in pre-specified subgroups, there was a statistically significant interaction with type of randomised guideline therapy; randomisation to aspirin + dipyridamole was associated with less and less severe bleeding than randomisation to clopidogrel (p for interaction = 0.0021). Similarly, those participants who underwent thrombolysis prior to enrolment randomised to triple antiplatelet therapy had more and more severe bleeding than those who did not receive thrombolysis (p for interaction = 0.036). Within all other pre-specified subgroups, there were no significant interactions with the treatment effect on ordinal bleeding (Fig. 2).
Forest plot of ordinal bleeding by randomised treatment (Intensive vs. guideline) ABCD2: age, blood pressure, clinical symptoms, diabetes, duration; BP: blood pressure; IS: ischaemic stroke; LACS: lacunar syndrome; NIHSS: National Institutes of Health Stroke Scale PACS: partial anterior circulation syndrome; POCS: posterior circulation syndrome; TACS: total anterior circulation syndrome; TIA: transient ischaemic attack.
On-treatment bleeding scores
The REACH score poorly predicted bleeding both by site and severity (Table 6, Fig. 3). The intracranial-B2LEED3S3 score poorly predicted intracranial bleeding in this population (C-statistic 0.51, 95% CI 0.39–0.64). In contrast, the S2TOP-BLEED score moderately predicted bleeding by severity and site. Specifically the S2TOP-BLEED score was designed to predict major, including fatal, bleeding and achieved this with a moderate C-statistic of 0.62 (95% CI 0.55–0.69) in those with fatal or major bleeding and 0.63 (95% CI 0.54–0.71) in those with a major bleed (Table 6, Fig. 3).
Calibration plots for bleeding-free survival for the three predictive scores on treatment. (A) REACH: Reduction of Atherothrombosis for Continued Health. (B) S2TOP-BLEED: sex, smoking, blood pressure, lower body mass index, elderly, ethnicity, and diabetes. (C) Intracranial B2LEED3S3: Intracranial-B2LEED3S3: body mass index, blood pressure, lacune, elderly, ethnicity, coronary artery or cerebrovascular disease history, dual antithrombotic agent or oral anticoagulant, sex.
Discussion
In this large trial assessing triple versus guideline antiplatelet therapy in acute non-cardioembolic ischaemic stroke or TIA, fatal or major bleeding occurred more frequently in those randomised to triple vs guideline antiplatelet therapy. The divergence in major bleeding between the treatment groups occurred in the 8–35 day period but not in the earlier 0–7 and later 36–90 day periods. In multivariate analysis more, and more severe, bleeding events were seen with increasing age, female sex, increasing pre-morbid dependency, longer time from onset to randomisation, prior major bleed, prior antiplatelet therapy and in those randomised to triple vs guideline antiplatelet therapy. More severe bleeding was associated with worse clinical outcomes across multiple physical, emotional and quality of life domains. Those patients who underwent thrombolysis prior to enrolment had more, and more severe, bleeding in the presence of triple than guideline antiplatelet therapy. Of the bleeding scores assessed, the S2TOP-BLEED score moderately predicted major or fatal bleeding, whilst REACH and intracranial-B2LEED3S3 scores performed poorly.
The Platelet-Oriented Inhibition in New TIA and minor ischemic stroke (POINT)6 and the Clopidogrel in High-risk patients with Acute Nondisabling Cerebrovascular Events (CHANCE)7 trials both assessed aspirin plus clopidogrel vs aspirin alone in mild ischaemic stroke and TIA within 12 and 24 h of symptom onset, respectively. There were fewer bleeding events in both these trials compared with TARDIS. Major bleeding in POINT was seen in 0.9% of the intensive group (aspirin and clopidogrel) and 0.6% in the placebo (aspirin) group6, whilst CHANCE reported moderate or severe bleeding in 0.3% of patients in both treatment arms of the trial7. A recent systematic review and meta-analysis including four trials of dual antiplatelet therapy vs aspirin (CHANCE, POINT, THALES (The acute stroke or transient ischaemic attack treated with Ticagrelor and aspirin for prevention of stroke and death) and FASTER (Fast assessment of stroke and transient ischaemic attack to prevent early recurrence) found that dual antiplatelet therapy was associated with an increased risk of moderate or severe bleeding: relative risk 2.17, 95% CI 1.16 to 4.08)8. The authors stratified bleeding risk by treatment regimen or duration and noted the association was mainly seen with ticagrelor and treatment over 21 days.8 In contrast to TARDIS, dual antiplatelet therapy was not associated with an increased risk of minor bleeding events8. In addition to the number of antiplatelet agents being assessed, TARDIS differed from these studies by recruiting patients within 48 h of onset with no upper stroke severity limit and included 341 (11%) patients who had undergone thrombolysis. These differences, and the intensity of antiplatelet therapy, likely explain the higher bleeding rates seen in TARDIS, although it is interesting to note that stroke severity (NIHSS) was not associated with bleeding. The median [interquartile range] baseline NIHSS was 2.0 [1.0, 4.0] in TARDIS, compared with 2.0 [1.0, 3.0] in CHANCE7, 2.0 [1.0, 2.0] in POINT6, and 1.0 in FASTER9. THALES included patients with NIHSS ≤ 5: 60% NIHSS 0–3, 30% NIHSS 4–510. In a secondary analysis of THALES comparing those with NIHSS 0–3 to NIHSS 4–5, there was no difference in the treatment effect with Ticagrelor-Aspirin vs Aspirin alone, and no difference in severe bleeding11. Future research may wish to consider whether dual antiplatelet therapy in more severe stroke populations reduces recurrent ischaemic events without causing excessive bleeding.
Multivariate associations between baseline variables and ordinal bleeding revealed that increasing age, female sex, increasing pre-morbid dependency, a previous major bleed, previous antiplatelet therapy, and a longer time from onset to randomisation were associated with more severe bleeding events. In contrast, a secondary analysis of POINT reported that the only baseline variable significantly associated with the risk of major haemorrhage was increasing age12. In TARDIS, 70% of participants were recruited 24-48 h after onset, which is a high risk period for blood–brain barrier breakdown due to ischaemia, and coupled with triple antiplatelet therapy likely increased the risk of bleeding. Despite having pre-morbid mRS > 2 as an exclusion criteria, increasing pre-morbid mRS was associated with more severe bleeding events. Imaging markers of ‘brain frailty’, both individually and when amalgamated as a score, were not associated with increased bleeding although cerebral atrophy narrowly missed statistical significance. In a secondary analysis of the third international stroke trial (IST-3), cerebral atrophy (but not other background changes) was associated with an increased risk of symptomatic intracranial haemorrhage (sICH)13, whilst a secondary analysis of the enhanced control of hypertension and thrombolysis stroke study (ENCHANTED) found no association between atrophy and sICH14. In TARDIS, background imaging markers were surprisingly prevalent in a population who were independent according to the mRS at baseline. Clinical frailty was not measured in TARDIS but the burden of ‘brain frailty’ may suggest that this cohort was frailer than perhaps the mRS is able to delineate, which may have influenced the association with bleeding events.
In the present study, the only bleeding score to moderately predict bleeding for which it was designed was the S2TOP-BLEED score for major, including fatal, bleeding. This finding is similar to an external validation study from the Oxford Vascular Study group where the S2TOP-BLEED score was better at predicting bleeding for which it was designed, than the REACH and intracranial-B2LEED3S3 scores in 2072 patients on an antiplatelet agent following a TIA or ischaemic stroke15. Future trials may wish to stratify patients by bleeding risk in order to reduce the potential risk of bleeding in this patient group.
TARDIS used an ordinal bleeding scale16 incorporating minor bleeding events, which were more common in the intensive than guideline group, occurring from treatment onset throughout the treatment period. In contrast, major bleeding events occurred later in the treatment period. Meta-analyses of dual antiplatelet therapy trials have demonstrated that a short period (21 days) of intensive antiplatelet therapy seems to be optimum; reducing the risk of major bleeding events, whilst maximising any treatment benefit8,17. Whether an even shorter period of intensive triple antiplatelet therapy for 7 days is safe and effective is unclear.
This secondary analysis of TARDIS has several strengths including wide inclusion criteria and therefore generalisability, use of locally-sourced antiplatelet agents from a variety of manufacturers increasing validity, and an ordinal bleeding safety outcome incorporating minor bleeding. However, there are several limitations. First, the wide inclusion criteria included no upper stroke severity limit and allowed inclusion of patients up to 48 h after symptom onset. Although this allowed generalisability, increasing time to randomisation was associated with increased bleeding. Second, patients could be recruited 24–48 h after thrombolysis; hence, TARDIS shows, for the first time in a large trial, that acute intensive antiplatelet therapy should not be administered to patients 24–48 h after thrombolysis. Third, trial treatments were open label and therefore participants knew what they were taking and may have been more likely to report bleeding events, especially minor bleeds. Last, 30 days of triple treatment may have been too long given the associated bleeding risk and that bleeding events diverged between treatment groups in the 8–35 day period, but not before or after. Hence, the effect on bleeding occurred whilst on treatment and not after. The lack of divergence in the 0–7 day period implies that the duration of intensive antiplatelet therapy likely contributes to the risk of bleeding as demonstrated in the aforementioned meta-analysis8.
Further research, including meta-analysis of trials, should seek to establish the optimum timing of initiation, duration and types of antiplatelet therapy in acute minor ischaemic stroke and TIA. Triple antiplatelet therapy should be avoided in acute ischaemic stroke and TIA and particularly 24–48 h following thrombolysis pending further data. Stratifying patients using bleeding scores may help to minimise bleeding risk and rationalise antiplatelet treatment in future studies.
In summary, triple antiplatelet therapy in acute non-cardioembolic ischaemic stroke and TIA patients was associated with more fatal or major bleeds and more, and more severe, bleeding. For major bleeding events, the treatment groups separated after one week supporting the rationale for a short period of intensive treatment in dual antiplatelet trials of minor ischaemic stroke and TIA patients to maximise benefit whilst minimising bleeding risk. Increasing age, female sex, increasing pre-morbid dependency, longer time from onset to randomisation, previous major bleed and prior antiplatelet therapy were all associated with more, and more severe, bleeding. Clinicians should take these factors into consideration when counselling patients with acute cerebral ischaemia on the bleeding risk with intensive antiplatelet therapy.
Methods
Study design
TARDIS was an international multicentre prospective randomised open-label blinded-endpoint (PROBE) trial conducted in four countries (Denmark, Georgia, New Zealand, UK) at 106 sites. Information on the design, statistical analysis plan and baseline characteristics of the participants have already been published18,19,20.
Adult patients aged ≥ 50 years were suitable for inclusion if they were at risk of a recurrent ischaemic stroke and had either a non-cardioembolic ischaemic stroke with limb weakness, isolated dysphasia or isolated neuroimaging-positive hemianopia, or a non-cardioembolic TIA with at least 10 min of limb weakness or isolated dysphasia. Participants were randomised within 48 h of the onset of symptoms; if they had received intravenous thrombolysis they could be randomised after 24 h following receiving this treatment and brain imaging had excluded any cerebral bleeding. There was no stroke severity cut-off for inclusion into the trial. Exclusion criteria included: isolated sensory symptoms, facial weakness, vertigo or dizziness; intracranial haemorrhage; non-ischaemic cause for symptoms; definite need for, or contraindication to, aspirin, clopidogrel or dipyridamole; need for anticoagulation; and pre-randomisation dependency. Patients provided written informed consent, or if the patient lacked capacity written informed consent was obtained from a relative, carer or friend. A full listing of the study inclusion and exclusion criteria is available1.
Interventions
Randomisation was provided by entering data online into a secure web-based database system. Treatment assignment was stratified by country and index event (stroke, TIA), with minimisation on key prognostic baseline factors1 Participants randomised to the intervention group received aspirin (300 mg loading followed by 50-150 mg daily, typically 75 mg), clopidogrel (300 mg loading followed by 75 mg daily) and dipyridamole (200 mg twice daily modified release). Those randomised to guideline antiplatelet therapy received either clopidogrel alone or combined aspirin and dipyridamole, using the same doses above1 Randomised treatment was given for 30 days after which participants were treated according to local guidelines.
Assessments
Age, sex, ethnicity and prior antiplatelet therapy (none, aspirin, clopidogrel, dipyridamole, other) were recorded at baseline. The severity of index stroke was assessed with the National Institutes of Health Stroke Scale (NIHSS, scores range from 0 to 42 with higher scores indicating a more severe neurological deficit21) and risk of recurrence after index TIA assessed using the ABCD2 scale (scores range from 0 to 7 with higher scores indicating a higher risk of recurrence22). Clinical syndrome was assessed using the Oxfordshire Community Stroke Project classification23.
Participants were seen at days 7 (on treatment) and 35 (end of treatment) to determine whether any outcome or bleeding events had taken place and to assess treatment compliance. Final follow-up was performed centrally by blinded assessors at 90 days by telephone from the coordinating centre in each country. If the participant could not be contacted, a paper version of the form was sent by post. Data pertaining to recurrent cerebrovascular events were captured at days 7 and 35 (investigator-reported), in any serious adverse events, at day 90 telephone follow-up and in a general practitioner questionnaire after day 90. Expert adjudicators blinded to treatment assignment validated and categorised the primary outcome, haemorrhage and investigator-reported serious adverse events. Any participants who violated the protocol were still followed up in full and included in intention-to-treat analyses.
Neuroimaging
Brain imaging was essential for all ischaemic stroke patients prior to enrolment in TARDIS in order to exclude haemorrhage or an alternative imaging diagnosis. Imaging was not essential for patients with TIA. Computerised topography (CT) or magnetic resonance imaging (MRI) scans performed according to local practice and any additional clinical scans were collected and adjudicated centrally by a trained panel of expert neuroradiologists blinded to symptoms and randomised treatment, using approaches developed from the third international stroke trial (IST-3) and the efficacy of nitric oxide in stroke (ENOS) trial13,24.
Acute stroke lesions were graded by location, size, severity, swelling and mass effect. The Alberta Stroke Program Early CT Score (ASPECTS) was used to grade the degree of ischaemia affecting the middle cerebral artery territory.
Baseline pre-event imaging markers including cerebral atrophy, periventricular white matter lucencies and old vascular lesion(s) were assessed individually, and amalgamated as a ‘brain frailty’ score25.
-
Cerebral atrophy: assessed in cortical and central regions as 0 = absent, 1 = moderate, 2 = severe.
-
Periventricular white matter lucencies: assessed in anterior and posterior regions as 0 = absent, 1 = lucency restricted to region adjoining ventricles, 2 = lucency covering lateral ventricle to cortex.
-
Old vascular lesions: assessed by location.
-
‘Brain frailty’ score: 1 point for periventricular white matter lucencies (score of 1 or 2 anterior and/or posterior); 1 point for cerebral atrophy (scores of 1 or 2 cortical and/or central); and 1 point for old vascular lesion(s) (maximum 3 of 3).
Bleeding and other outcome measures
The severity of bleeding was assessed on a five level ordered categorical scale16,26: fatal, major, moderate, minor, none. The definitions of fatal, major and moderate haemorrhage were according to the International Society on Thrombosis and Haemostasis and are based on severity, bleeding site, haemoglobin drop and transfusion requirement27.
Further safety outcomes included all-cause and cause-specific case fatality, early neurological deterioration (defined as an increase from baseline to day 7 of at least 4 points on the NIHSS and/or a reduction in consciousness in the NIHSS consciousness domain), and serious adverse events.
The primary efficacy outcome was measured at 90 days and comprised stroke/TIA recurrence and its severity; severity was assessed using a six-level ordinal scale19,26: fatal stroke, non-fatal severe stroke (modified Rankin Scale, mRS 4, 5), moderate stroke (mRS 2, 3), mild stroke (mRS 0, 1), TIA, and neither stroke nor TIA18,19. Day 90 secondary outcomes28 included activities of daily living (Barthel Index29); cognition (telephone Mini-Mental State Examination, t-MMSE30; Telephone Interview for Cognition Scale-modified, TICS-M31; verbal fluency32); health-related quality of life (European Quality of Life-5 dimensions-3 level, EQ-5D-3L33, from which health status utility values, HSUV, were calculated; and EQ-visual analogue scale, EQ-VAS); and mood (short Zung Depression Score 34). At the time of hospital discharge, the length of hospital stay and discharge destination were recorded.
Bleeding risk prediction scores
Bleeding risk prediction scores were calculated from information provided at baseline as outlined in Supplementary Table 1. The REACH (Reduction of Atherothrombosis for Continued Health) score was designed to predict serious bleeding (including moderate, major and fatal)3. The S2TOP-BLEED score predicts major (including fatal) bleeding and incorporates sex, smoking, blood pressure, lower body mass index, elderly, ethnicity and diabetes in the algorithm4. The B2LEED3S3 score predicts intracranial bleeding and incorporates sex, body mass index, blood pressure, lacune, elderly, ethnicity, coronary artery or cerebrovascular disease history and dual antithrombotic agent or oral anticoagulant in the algorithm5.
Study oversight
All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by the East Midlands UK research ethics committee (reference: 08/H1102/112). The study was registered (ISRCTN47823388, EudraCT: 2007-006749-42) and adopted in the UK by the National Institute of Health Research (NIHR) Stroke Research Network. National competent authority (or equivalent) approvals were also obtained for this study. The study was sponsored by the University of Nottingham, UK.
Statistical analyses
Data are number (%), median [interquartile range] or mean (standard deviation).The effect of treatment on the primary safety outcome was analysed as a shift in bleeding and its severity (fatal, major, moderate, minor and none) using ordinal logistic regression. Additional sensitivity analyses included assessing bleeding individually by level of severity and as all bleeding. Comparisons between bleeding severity levels and treatments were assessed using ANOVA, the Chi-Square/Fisher's Exact test, the Kruskal-Wallis test, Kendall's rank correlation and Jonckheere-Terpstra test. Further analyses were performed using binary logistic regression (reported as adjusted odds ratio, aOR), ordinal logistic regression (adjusted common odds ratio, aOR) or multiple linear regression (adjusted mean difference, aMD); 95% confidence intervals are given with each, and covariates comprised: index event (TIA vs stroke), country, guideline randomisation choice, age, sex, pre-morbid function, systolic blood pressure, stroke syndrome (cortical vs. lacunar23), number of antiplatelets before index event, use of gastroprotection, use of low dose heparin, time to randomisation, NIHSS, ABCD2 score, number of TIAs in the last week and treatment with alteplase. A check that the assumption of common proportional odds was not violated was performed before ordinal logistic regression using the likelihood ratio test.
To assess the treatment effect on ordinal bleeding in pre-specified subgroups, an interaction term was added to an adjusted ordinal logistic regression model. Clinical outcomes included a value for death, as is standard for the mRS, Barthel Index and EQ-5D; values comprised: mRS 6, Barthel Index -5, t-MMSE -1, TICS-M -1, Verbal fluency -1, EQ-5D3L-HSUV 0, EQ-VAS -1, Zung 102.5. Age was analysed using a pre-specified cut-point (≤ 75 vs > 75 years) as well as a continuous variable using multiple linear regression.
We compared performance of the REACH, S2TOP-BLEED and intracranial B2LEED3S3 bleeding risk scores3,4,5 by means of the C statistic for integrated discrimination improvement, and calibration plot analysis35,36,37. The nominal level of significance for all analyses was p < 0.05. No adjustment was made for multiplicity of testing for secondary analyses. All analyses were by the intention to treat principle for all comparisons. Statistical analyses were performed by LJW using SAS software (version 9.4).
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request. Data have been shared with the virtual international stroke trials archive (VISTA): https://www.virtualtrialsarchives.org/vista/.
References
Bath, P. M. et al. Antiplatelet therapy with aspirin, clopidogrel, and dipyridamole versus clopidogrel alone or aspirin and dipyridamole in patients with acute cerebral ischaemia (TARDIS): A randomised, open-label, phase 3 superiority trial. Lancet 391(10123), 850–859 (2018).
Wong, K. S. et al. Early dual versus mono antiplatelet therapy for acute non-cardioembolic ischemic stroke or transient ischemic attack: An updated systematic review and meta-analysis. Circulation 128(15), 1656–1666 (2013).
Ducrocq, G. et al. Risk score to predict serious bleeding in stable outpatients with or at risk of atherothrombosis. Eur. Heart J. 31(10), 1257–1265 (2010).
Hilkens, N. A. et al. Predicting major bleeding in patients with noncardioembolic stroke on antiplatelets: S. Neurology 89(9), 936–943 (2017).
Amarenco, P. et al. The intracranial-B2LEED3S score and the risk of intracranial hemorrhage in ischemic stroke patients under antiplatelet treatment. Cerebrovasc. Dis. (Basel, Switzerland) 43(3–4), 145–151 (2017).
Johnston, S. C. et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N. Engl. J. Med. 369, 11 (2018).
Wang, Y. et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N. Engl. J. Med. 369(1), 11–19 (2013).
Li, Z.-X. et al. P2Y12 inhibitors plus aspirin versus aspirin alone in patients with minor stroke or high-risk transient ischemic attack. Stroke https://doi.org/10.1161/STROKEAHA.120.033040 (2021).
Kennedy, J. et al. Fast assessment of stroke and transient ischaemic attack to prevent early recurrence (FASTER): A randomised controlled pilot trial. Lancet Neurol. 6(11), 961 (2007).
Johnston, S. C. et al. Ticagrelor and aspirin or aspirin alone in acute ischemic stroke or TIA. N. Engl. J. Med. 383(3), 207–217 (2020).
Wang, Y. et al. Efficacy and safety of ticagrelor and aspirin in patients with moderate ischemic stroke: An exploratory analysis of the THALES randomized clinical trial. JAMA Neurol. 78(9), 1091–1098 (2021).
Tillman, H. et al. Risk for major hemorrhages in patients receiving clopidogrel and aspirin compared with aspirin alone after transient ischemic attack or minor ischemic stroke: A secondary analysis of the POINT randomized clinical trial. JAMA Neurol. 76(7), 774–782 (2019).
IST-3 collaborative group. Association between brain imaging signs, early and late outcomes, and response to intravenous alteplase after acute ischaemic stroke in the third International Stroke Trial (IST-3): Secondary analysis of a randomised controlled trial. Lancet Neurol. 4(5), 485–96 (2015).
Delcourt, C. et al. Brain imaging abnormalities and outcome after acute ischaemic stroke: The ENCHANTED trial. J. Neurol. Neurosurg. Psychiatry 91(12), 1290–1296 (2020).
Hilkens, N. A., Li, L., Rothwell, P. M., Algra, A. & Greving, J. P. External validation of risk scores for major bleeding in a population-based cohort of transient ischemic attack and ischemic stroke patients. Stroke 49(3), 601–606 (2018).
Woodhouse, L. J. et al. Statistical reanalysis of vascular event outcomes in primary and secondary vascular prevention trials. BMC Med. Res. Methodol. 21(1), 218 (2021).
Pan, Y. et al. Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack: A pooled analysis of clopidogrel in high-risk patients with acute non-disabling cerebrovascular events (CHANCE) and platelet-oriented inhibition in new TIA and minor ischemic stroke (POINT) trials. JAMA Neurol. 76(12), 1466–1473 (2019).
The TARDIS Trial Investigators. Safety and efficacy of intensive vs. guideline antiplatelet therapy in high-risk patients with recent ischemic stroke or transient ischemic attack: Rationale and design of the Triple Antiplatelets for Reducing Dependency after Ischaemic Stroke (TARDIS) trial (ISRCTN47823388). Int. J. Stroke 10, 1159–1165 (2015).
Bath, P. et al. Statistical analysis plan for the “Triple Antiplatelets for Reducing Dependency after Ischaemic Stroke” (TARDIS) trial. Int. J. Stroke 10(3), 449–451 (2015).
Bath, P. M. et al. Baseline characteristics of the 3096 patients recruited into the ‘Triple Antiplatelets for Reducing Dependency after Ischemic Stroke’trial. Int. J. Stroke 12(5), 524–538 (2017).
Adams, H. P. et al. Baseline NIH stroke scale score strongly predicts outcome after stroke. A report of the trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 53, 126–131 (1999).
Johnston, S. C. et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet 369(9558), 283–292 (2007).
Bamford, J., Sandercock, P., Dennis, M., Burn, J. & Warlow, C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337(8756), 1521–1526 (1991).
The ENOS Trial Investigators. Efficacy of nitric oxide, with or without continuing antihypertensive treatment, for management of high blood pressure in acute stroke (ENOS): A partial-factorial randomised controlled trial. The Lancet 385(9968), 617–628 (2015).
Appleton, J. P. et al. Imaging markers of small vessel disease and brain frailty, and outcomes in acute stroke. Neurology 94, e439–e452 (2020).
Bath, P. M. W., Geeganage, C. M., Gray, L. J., Collier, T. & Pocock, S. Use of ordinal outcomes in vascular prevention trials: Comparison with binary outcomes in published stroke trials. Stroke 39(10), 2817–2823 (2008).
Schulman, S. & Kearon, C. Int Society Thrombosis H. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 3(4), 692 (2005).
Schellinger, P. D. et al. Assessment of addtional endpoints relevant to the benefit of patients after stroke - what, when, where, in whom. Int. J. Stroke 7(3), 227–230 (2012).
Sulter, G., Steen, C. & de Keyser, J. Use of the Barthel Undex and modified Rankin Scale in acute stroke trials. Stroke 30, 1538–1541 (1999).
Bolland, K., Sooriyarachchi, M. R. & Whitehead, J. Sample size review in a head injury trial with ordered categorical responses. Stat. Med. 17, 2835–2847 (1998).
Desmond, D. W., Tatemichi, T. K. & Hanzawa, L. The telephone interview for cognitive status (TICS): Reliability and validity in a stroke sample. Int. J. Geriatr. Psychiatry 9, 803–807 (1994).
Tombaugh, T., Kozak, J. & Rees, L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch Clin Neuropsychol. 14(2), 167–177 (1999).
Brooks, R. EuroQol: The current state of play. Health Policy 37(1), 53–72. https://doi.org/10.1016/0168-8510(96)00822-6 (1996).
Zung, W. W. K. A self-rating depression scale. Arch. Gen. Psychiatry. 12, 63–70 (1965).
Pencina, M. J., D’Agostino, R. B. & Vasan, R. S. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat. Med. 27(2), 157–72 (2008).
Pencina, M. J., D’Agostino, R. B. & Steyerberg, E. W. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 30(1), 11–21 (2011).
Pencina, M. & D’Agostino, R. Evaluating discrimination of risk prediction models: The C statistic. JAMA 314(10), 1063–1064 (2015).
Schulman, S. & Kearon, C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thrombosis Haemostasis. 3, 592–694 (2005).
Roccaforte, M. D., Burke, W. J., Bayer, B. L. & Wengel, S. P. Validation of a telephone version of the mini-mental state examination. J. Am. Geriatr. Soc. 40(7), 697–702 (1992).
Acknowledgements
We thank the participants, investigators and research staff at the participating sites and the members of the Independent Data Monitoring Committee, for their involvement in and support for, the study. TARDIS acknowledges the support of the National Institute for Health Research (NIHR) Stroke Research Network/Clinical Research Network (Stroke); the large recruitment in the UK would not have been possible without this network support. The TARDIS start-up phase was funded by the British Heart Foundation (grant PG/08/083/25779, 1 April 2009 – 30 September 2012). The NIHR HTA programme funded the main phase of this project (10/104/24, 1 October 2012 – 30 September 2017, http://www.nets.nihr.ac.uk/projects/hta/1010424). This paper presents independent research funded by the NIHR. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health & Social Care. Indirect funding was provided by The Stroke Association through its funding of the former Division of Stroke, University of Nottingham. There was no commercial support for the trial and antiplatelet drugs were sourced locally at each site. The trial was sponsored by the University of Nottingham.
Funding
(Funded by National Institutes of Health Research Health Technology Assessment Programme and British Heart Foundation; ISRCTN47823388).
Author information
Authors and Affiliations
Contributions
L.J.W. performed statistical analyses. J.P.A. interpreted the data and wrote the manuscript. All other authors provided critical appraisal of the manuscript. P.M.B. is corresponding author and guarantor of the study.
Corresponding author
Ethics declarations
Competing interests
LJW and JPA were funded in part by NIHR TARDIS (10/104/24). JPA was supported, in part, by a NIHR Health and Care Research Scholarship, and is supported by a Nottingham University Hospitals NHS Trust Research & Innovation Award. TGR is a NIHR Senior Investigator. PMB is Stroke Association Professor of Stroke Medicine and an emeritus NIHR Senior Investigator; he has consulted for DiaMedica, Moleac, Phagenesis and Roche. Remaining authors (HC, RAD, TJE, MJ, KK, AAM, AR, NS) report no declarations.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Woodhouse, L.J., Appleton, J.P., Christensen, H. et al. Bleeding with intensive versus guideline antiplatelet therapy in acute cerebral ischaemia. Sci Rep 13, 11717 (2023). https://doi.org/10.1038/s41598-023-38474-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38474-2
- Springer Nature Limited