Abstract
Cerebrospinal meningitis (CSM) is a public health burden in Ghana that causes up to 10% mortality in confirmed cases annually. About 20% of those who survive the infection suffer permanent sequelae. The study sought to understand the predictive signs and symptoms of bacterial meningitis implicated in its outcomes. Retrospective data from the Public Health Division, Ghana Health Service on bacterial meningitis from 2015 to 2019 was used for this study. A pre-tested data extraction form was used to collect patients’ information from case-based forms kept at the Disease Control Unit from 2015 to 2019. Data were transcribed from the case-based forms into a pre-designed Microsoft Excel template. The data was cleaned and imported into SPSS version 26 for analysis. Between 2015 and 2019, a total of 2446 suspected bacterial meningitis cases were included in the study. Out of these, 842 (34.4%) were confirmed. Among the confirmed cases, males constituted majority with 55.3% of the cases. Children below 14 years of age were most affected (51.4%). The pathogens commonly responsible for bacterial meningitis were Neisseria meningitidis (43.7%) and Streptococcus pneumoniae (53.0%) with their respective strains Nm W135 (36.7%), Nm X (5.1%), Spn St. 1 (26.2%), and Spn St. 12F/12A/12B/44/4 (5.3%) accounting for more than 70.0% of the confirmed cases. The presence of neck stiffness (AOR = 1.244; C.I 1.026–1.508), convulsion (AOR = 1.338; C.I 1.083–1.652), altered consciousness (AOR = 1.516; C.I 1.225–1.876), and abdominal pains (AOR = 1.404; C.I 1.011–1.949) or any of these signs and symptoms poses a higher risk for testing positive for bacterial meningitis adjusting for age. Patients presenting one and/or more of these signs and symptoms (neck stiffness, convulsion, altered consciousness, and abdominal pain) have a higher risk of testing positive for bacterial meningitis after statistically adjusting for age.
Similar content being viewed by others
Introduction
Bacterial meningitis is one of the most prevalent public health diseases affecting approximately 1.7 million people with roughly 170,000 deaths yearly in the world’s population1. It remains one of the most serious kinds of meningitis known to attack the focal sensory system in people. The four main causes of acute bacterial meningitis are Neisseria meningitidis, Streptococcus pneumoniae, Haemophilus influenzae, and Streptococcus agalactiae.
The most prevalent strains remain to be Neisseria meningitides serogroups A, B, C, W135 and Y, Streptococcus pneumoniae serotype St1, St14, St19A, and Haemophilus influenza type b.
Bacterial meningitis is substantially a more serious disease and more likely to cause death compared to viral meningitis. Its case fatality rate remains at 100% if untreated2.
Survivals of bacterial meningitis can experience the ill effects of genuine neurological confusions for instance, deafness, visual deficiency, mental and scholarly disability which frequently is endured over the lifetime of the person3. A key factor that contributes to this high morbidity is our incomplete understanding of the pathogenesis of the disease resulting in it being one of the leading causes of mortality in the world due to its mode of transmission4.
The African meningitis belt (AMB) consist of 26 nations extending between Senegal toward the west to Ethiopia in the east. These nations are known for having a relatively high yearly incidence of bacterial meningitis5. It is estimated that, frequency rates during pandemics have reached as high as 100–1000 cases for every 100,000 population which are remarkably high rates for an obtrusive bacterial infection. The case fatality rates ranges from 6.6 to 10.0% and about 30–50% of the survivors sustain neurological sequelae6.
In Ghana, Neisseria meningitidis, Streptococcus pneumonia and Haemophilus influenzae are the most common species found around the meningitis belt spanning from Brong Ahafo through to Upper East regions7. Bacterial Meningitis is a public health problem in Ghana contributing to the high burden of disease and can cause mortality up to 10% of the victims yearly7. Approximately 20% of the people who get the infection experience disorders or neurological sequelae1. However bacterial meningitis has vaccines to protect against some strains of the bacteria in the name of MenACWY for meningococcal groups A, C, W and Y, PPSV 23, and PCV 13, 15, and 20 for streptococcus pneumoniae, and DTaP-IPV/Hib for haemophilus influenzae B.
Lastly, the review of literature points towards giving quantitative evaluation of the prescient signs and symptoms of bacterial meningitis in Northern Ghana and to give results that is summed up over the entire northern beltf with respect to bacterial meningitis in Ghana.
Study design
This was a retrospective, cross-sectional study conducted using a consolidated database from the Disease Control and Surveillance Unit and the Zonal Public Health and Reference Laboratory, Tamale-Ghana. The measure was observational with an analytical component to establish the risk factors associated with the disease outcomes. The research was a quantitative measure that involve capturing of data using case investigation forms to identify association between diagnosis and signs and symptoms of bacterial meningitis.
Study setting
The study data covered all the districts and regions in Northern Ghana. The population of Ghana is 30,800,000 with the Northern zone having a total of 8,237,660 population8. The northern zone of Ghana consists of Northern region, Upper East, Upper West, Brong Ahafo and some part of Volta region. The study was carried out at the Tamale Public Health Reference Laboratory, Tamale-Ghana (TPHRL). The facility is referred to a zonal reference laboratory for bacterial meningitis in Ghana and West Africa which also serves as the reference public health laboratory for the northern zone of Ghana.
Study population
All patients who presented with signs and symptoms suggestive of bacterial meningitis per the Ghana Health Service case definition for bacterial meningitis were included in the study. All samples collected across the country were brought to the TPHRL for rT-PCR testing and or confirmation.
Case definition
The study classifies the cases according to the clinical case presentation, laboratory criteria for diagnosis, and case identification.
Clinical case definition
An illness with sudden onset of fever (> 38.5 °C rectal or > 38.0 °C axillary) and one or more of the following: neck stiffness, altered consciousness, another meningeal sign or petechial or purpureal rash9. In patients less than one (1) year, suspect meningitis when fever accompanied by bulging fontanelle9.
Laboratory criteria for diagnosis
Lumbar puncture was performed at peripheral facilities in the districts level, aliquoted and sent to the TPHRL for rT-PCR analysis. Positive CSF rapid test (i.e. Latex agglutination test, Wellcogen test, Gram stain) or Positive culture test for screening at district or health facility level and confirmed by rT-PCR test within 72 hours of disease presentation at the TPHRL9.
Case classification
Suspected case is that which meets the clinical case definition, probable case is a suspected case as defined (with or without positive rapid test results) or ongoing epidemic and epidemiological link to a confirmed case, and confirmed case is a suspected or probable case with Polymerase Chain Reaction positive outcome at the TPHRL9.
Outcome of cases
The outcome of cases in the study is defined by the rT-PCR results for each suspected case. The outcomes are binary in nature and is described as “negative” or “positive”.
Laboratory confirmation
Confirmation by direct real-time PCR for the purpose of species identification, were all done in the TPHRL. Using Cy5, HEX, and FAM as differentiating dyes, a triplex detection technique was employed to determine the S. pneumoniae serotype. Using FAM and ROX dyes, with ROX serving as the reference dye, the serogroups of N. meningitidis and H. influenzae were identified using monoplex detection. In order to simultaneously detect N. meningitidis, S. pneumoniae, and H. influenzae species, a single master mix was created and employed for triplex detection. The constituents of the master mix included primers (both forward and reverse) and probes of all the species tested in equal volumes, PCR grade water, and Multiplex Quanta. The ratios were 12.5 µL:7.5 µL:1 µL for the master mix, PCR grade water, and primers and probes, respectively, for a sample10. The target genes for PCR detection were the Cu and Zn superoxide dismutase gene, sodC, autolysin gene (lytA), and protein D encoding gene, hpd, for N. meningitidis, S. pneumoniae, and H. infuenzae, respectively. All samples which tested positive for N. meningitidis were selected, and their serogroups were identifed using the monoplex detection method. Serogroup identifcation using a slide agglutination procedure with polyclonal antisera was not considered because it is usually associated with non-specific or cross-reactions11. Each of the six tested serogroups had its own master mix created. The constituents of the master mix included primers (forward and reverse) and probes of targeted serogroup as well as a monoplex Quanta with low ROX according to ratios for each triplex detection. The reaction templates was prepared based on the amount of samples analyzed, and the master mix was created appropriately. The master mix and samples were added to the PCR reaction plate wells at a ratio of 23 µL: 2 µL, respectively10. The controls were run simultaneously with the samples. When new dilutions of primers and probes were prepared, they were controlled before testing the patient samples.
Sample size determination
No sample size was determined or calculated as all suspected cases of bacterial meningitis brought to the Disease Control and Surveillance Unit, Ghana Health Service, Northern region were included in the study from 2015 to 2019.
Patient and public involvement
Data collected by the Ghana Health Service (GHS) on patients’ information were investigated by clinicians and necessary data collected in a predesigned case investigation form by Ghana Health Service. Patient information and laboratory outcomes were key in the findings and results. Patients involved in the recruitment process were seeking medical care at their respective facilities but not with researcher since the study was retrospective. Results and findings of the study are made available to the Ghana Health Service, health promotion department to share the findings to communities during health promotion talks.
Data analysis
Data was extracted from the case reporting forms unto a pre-designed Microsoft excel template. The data was cleaned twice and exported to SPSS Version 26, for analysis. Descriptive analysis was performed and presented in graphs and tables. A chi-square analysis was performed for associated signs/symptoms of bacterial meningitis whiles binary logistics regression model was adopted to determine the clinical signs and symptoms that are predictive of a person likely to be tested positive for bacterial meningitis using the five years retrospective data. Likelihood Ratio Test (LRT) was used to determine the best fit of the logistic regression during analysis. The dependent variable remained to be the test outcomes for the Polymerase Chain Reaction (rT-PCR) (Positive and Negative).
Inclusion criteria
All patients that fulfilled the case definition criteria for bacterial meningitis were included to the study as collated by the Disease Control and Surveillance Unit and the TPHRL.
Exclusion criteria
All patients with inadequately filled case investigation forms, cases that were not having samples accompanying the case investigation forms and cases that had no rapid test results and or culture and rT-PCR results.
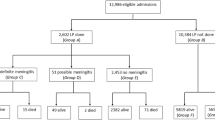
Selection criteria summary
The diagram below gives a breakdown of the summary of the selection criteria and data screening processes as shown in Fig. 1.
Ethical approval
The Kwame Nkrumah University of Science and Technology's (KNUST) Committee on Human Research and Publication Ethics (CHRPE) gave its approval to this work (Ref: CHRPE/AP/469/20). The committee (KNUST Committee on Human Research and Publication Ethics) has accepted both the protocol revision and the waiver of informed consent. The waiver for inform consent was provided by the KNUST CHRPE through the combined application (Ref: CHRPE/AP/469/20). The Northern Regional Health Directorate also gave their approval and permission (Ref: GHS/TPHRL/0014/20). Every technique was used in conformity with the laws and ethical standards that were applicable. The researchers confirm that all experiments and method were performed in accordance with relevant guidelines and regulations.
Findings and results
The burden of bacterial meningitis is disproportionately distributed by place, time, and age but nearly equally distributed by sex. Within the study period, a total of two thousand, four hundred and forty-six (2446) cases were recorded and tested by both culture and Real Time Polymerase Chain Reaction (rT-PCR) methods for pathogens responsible for bacterial meningitis. A total of 2587 suspected cases were identified over the period with 2446 (94.6%) suspected cases included in the study; males were predominant (52.7%), the upper west and northern regions recorded the highest suspected cases within the study period (40.6%) with northern region having the highest positivity rate. The study had an overall prevalence of bacterial meningitis to be 34.4 percent with majority of the participants within the age group 5–14 years (Table 1).
Regional distribution of suspected bacterial meningitis cases
The northern and upper west regions recorded the highest and lowest suspected cases of meningitis in 2015 and 2016 respectively (Fig. 2). Between 2017 and 2019 however, the upper west region consistently recorded more suspected cases than the other two regions (Fig. 2).
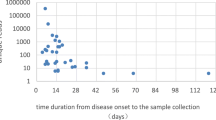
Trend of confirmed bacterial meningitis cases from 2015 to 2019
Figure 3 graphically represents population of “not a case” and “confirmed case” rT-PCR outcomes for suspected bacterial meningitis cases across the northern zone of Ghana. Greater proportion of the population of confirmed and not a case is dense within the ages of 0 to 24 years. Positivity rates are also higher in the ages ranging from 0 to 24 years (Fig. 3).
Table 2 gives a breakdown of confirmed cases according to year specific and regional distribution of cases. Majority (50.7%) of the cases were from northern region. Also, northern region recorded the highest prevalence across the years except 2019 where Upper West recorded the highest prevalence rate (Table 2).
The case incidence rate for the population at risk is 10.4775 per 100,000 population within the study period with a 34.4% (842/2446) positivity rate. However, 2017 recorded the highest positivity rate of 35.7% (3.9210/100,000) and 2015 the lowest positivity rate of 6.9% (0.7915/100,000) shown in Table 2. Overall, the 0–14 and 60+ years age category had the highest incidence rate across the study period (Table 3).
Real time polymerase chain reactions for bacterial causative agents of meningitis
Table 4 shows the real time rT-PCR confirmed bacterial causative agents of meningitis over the years studied. It was denoted that, from the 842 cases, Streptococcus pneumonia (Spn) accounted for 53.0% (446) of all confirmed cases of bacterial meningitis trailed by Neisseria meningitis (Nm) (43.7%; 368) and Haemophilus influenzae (3.3%; 28) from 2015 to 2019. Except for 2015 and 2016 where Neisseria meningitis was equal and more as causative agent of bacterial meningitis, Streptococcus pneumonia was implicated in most of the cases with Haemophilus influenzae accounting for a small proportion of the cases (shown in Table 4).
Serogroups of Neisseria meningitis implicated in bacterial meningitis (2015–2019)
Table 5 indicates the cross tabulation of the serogroups of Neisseria meningitis causing bacteria meningitis from 2015 to 2019. Of the 368 cases of Neisseria meningitis, serogroup NmW accounted for about 84.0% (309) of the cases followed by serogroups NmX (11.7%; 43), NmNG (2.7%; 10), NmC (1.1%; 4) and NmB (0.5%; 2).
Notwithstanding that, indications shows that 2017 had the highest frequency of Neisseria meningitis cases with 125 representing 34.0% whiles 2015 recorded the least frequency of cases with 28 (7.6%) (Table 5).
Serotypes of Streptococcus pneumoniae implicated in bacterial meningitis (2015–2019)
Table 6 relates to the cross tabulation of polymerase chain reaction results for serotypes of Streptococcus pneumoniae causes of meningitis over the five years period under review. In indication, Spn Serotype 1 (St. 1) recorded the majority of cases representing almost half of the cases (49.6%). Furthermore, relative to Spn cases recorded over the period, it was realized that St 18C/18B/18A/18F had the least counts of 1 (0.2%) case. Other cases like St. 12F/12A/12B/44/4 and St. 14 had frequencies of 45 (10.1%) and 21(4.7%) respectively. It was worth noting that non-typable cases of Streptococcus pneumoniae cases had a significant frequency of 61 (13.7%).
Notwithstanding, the year that recorded the highest frequency of Spn cases was 2017 with 166 (37.2%) whiles 2015 recorded the least with 28 (6.3%).
Serogroups of Haemophilus influenzae implicated in bacterial meningitis (2015–2019)
Table 7 represents the cross tabulation of cases of bacterial meningitis pathogen Haemophilus influenzae (HI) from 2015 to 2017. It was revealed that, from the 28 cases of Haemophilus influenzae, only Haemophilus influenzae serogroup B was isolated during the period with 17 (60.7%). Also, the non-groupable Haemophilus influenzae cases accounted for 11 cases representing 39.3 percent. Lastly, it was shown that 2017 had the majority of cases of HI with 10 (35.7%) cases whiles 2015 had the lowest with 2 (7.1%) (Shown in Table 7).
Signs and symptoms associated with bacterial meningitis
Fever (72.9%), neck stiffness (69.3%), headache (56.6%), Convulsion (22.9%) and altered consciousness (21.5%) were the most reported signs and symptoms for suspected bacterial meningitis. However, signs and symptoms that were associated with bacterial meningitis were neck stiffness (72.6%), fever (71.3%), headache (60.1%), convulsion (26.5%), and altered consciousness (26.0%). Notwithstanding that, neck stiffness (X2 = 6.215; p < 0.05), headache (X2 = 6.233; p < 0.05), convulsion (X2 = 14.687; p < 0.001), altered consciousness (X2 = 15.033; p < 0.001), abdominal pain (X2 = 12.038; p < 0.001), backpain (X2 = 6.509; p < 0.05), and kenning signs (X2 = 6.523; p < 0.05) were found to be statistically significantly associated with bacterial meningitis rT-PCR outcomes (Table 8).
Signs and symptoms predictive of bacterial meningitis
The statistical model for prediction of bacterial meningitis adjusting for age in the model indicates that suspected cases with neck stiffness (AOR = 1.244; C.I 1.026–1.508) has a 24.4 percent more likely to test positive than others. Patients with convulsion (AOR = 1.338; C.I 1.083–1.652), altered consciousness (AOR = 1.516; C.I 1.225–1.876), and abdominal pains (AOR = 1.404; C.I 1.011–1.949) has to greater risk of 33.8, 51.6, and 40.4 percent respectively (Table 9).
Discussion
In the study, it was worth noting that 2017 had the highest total case positivity rates of 30.7%, while 2015 had the least total case positivity rate of 8.6%. This finding clearly shows that males in all instances have higher rates compared to females and this could be as a result of population dynamics of the respective regions under the study where males to females ratio is estimated at approximately 93%12. Also, it could be as a result of stronger immune system in women than men against viruses and bacteria infections13. This finding is discordant with a similar study conducted by Kwambana-Adams et al. (2016) on pneumococcal meningitis outbreak and its associated factors in six districts of Brong Ahafo region, Ghana14. The researchers documented that 55.9% of the confirmed cases were females compared to 44.1% males. This disparity could be due to the study period within which both studies were conducted. Whilst our study span a five-year period (2015–2019), the other was done within a year (2015–2016).
Geographical distribution of confirmed cases across the five-year period denoted a general increase in confirmed cases of bacterial meningitis. The study revealed that over the five-year period, the Northern and Upper West regions reported the highest number of suspected cases (993; 40.6%) respectively whiles Upper East had the least suspected cases with 466 (18.8%). This outcome might be because of the strong interconnected surveillance system being active and operational in the Upper West region compared to the other regions. Further analysis reveals that, out of these suspected cases across the three regions, the northern region had 50.7% of confirmed cases of bacterial meningitis compared to the Upper East region which recorded a positivity rate of 21.0%. The UWR also recorded significant positivity rate of 28.3%. These findings are consistent with a study done by Codjoe & Nabies, (2014). The authors shared that the suspected and confirmed case of bacterial meningitis were highest in Northern region and Upper West regions within the meningitis belt in Ghana15.
Meningitis cases was higher among younger age groups and adults below 44 years. This could be due to the increased likelihood of these groups of people participating in activities within overcrowded places such as schools, markets and other workplaces as well as type of settlement. The finding is in line with Amadu et. al., 2019 who had similar outcomes and trends in the demographic features of the cases16. The most suspected and confirmed cases of the bacterial meningitis in these regions remains among the 15–44 years age group with a total of 981 cases (40.1%). The confirmation of suspected cases by rT-PCR denoted that child within the 0–14 age bracket had a total of 52.4% positivity rate compared to adults within the 15–60 age group that had a positivity rate of 41.8%16. These outcomes might be as a result of the vulnerability of children to infectious diseases of which bacterial meningitis is not an exception. This supports the argument that children younger than 15 years of age accounts for majority of all infections across the world17,18,19,20,21. Our finding is also comsistent with that of Nyarko (2016) who identified that 77.3% (761/980) of the confirmed meningitis cases were among children below the ages of 15 years in the Upper West region22.
In 2016 a total of 61.4% of the suspected cases were positive for bacterial meningitis compared to the other years. The number of confirmed positive cases over the period denoted an increased pattern from 2015 with 6.9% of the total positives to 35.7% in 2018. This pattern dropped sharply in 2019 to 19.0% indicating a significant decline in cases over the one-year period. This patterns and trends seen over the period is in congruent with a study conducted on the US Centers for Disease Control and Prevention’s (CDC) surveillance data on bacterial meningitis from 1998 to 2003, where there was a significant reduction in the incidence of cases of bacterial meningitis cases23.
The common signs and symptoms being neck stiffness (72.6%), headache (60.1%), convulsion (26.5), altered consciousness (26.0), abdominal pain (10.7%), backpain (9.3%), and kenning signs (13.4%) were associated with bacterial meningitis. However, binary logistics regression revealed that the presence of one or more of the following signs and symptoms; neck stiffness (AOR = 1.244; C.I 1.026–1.508), convulsion (AOR = 1.338; C.I 1.083–1.652), altered consciousness (AOR = 1.516; C.I 1.225–1.876), and abdominal pains (AOR = 1.404; C.I 1.011–1.949) as risk factors of confirmed bacterial meningitis cases. This aligns with little variation with an earlier publication by the CDC team in 2012 who found fever, headache, stiff neck, nausea, vomiting, photophobia, altered mental status remain as the major signs and symptoms of bacterial meningitis24.
Conclusions and recommendation
Bacterial meningitis continues to be an important cause of morbidity and mortality throughout the world, with differential risk among gender, age and geographic location. There is an increase in the rates of the disease pathogen over the period of the study. Children aged 0–14 years, males and northern region are the most affected. Neck stiffness, convulsion, altered consciousness and abdominal pains are risk factors associated with bacterial meningitis.
We recommended that peripheral health facilities should be keen in the identification of predictive signs and symptoms with particular attention to associated risk factors identified in the study. This study is made available to Ghana Health Service to serve as source of information in the review of protocols used to suspect or manage clinician suspicion levels of cases of bacterial meningitis.
Data availability
The Ghana Health Service are the custodians of the data that supported the study findings, but access to it is restricted because it was obtained under application and granted permission, therefore not available to the general public. However, the data can be obtained from the authors with the agreement and/or permission of the Ghana Health Service, Northern Regional Directorate of Health Service upon reasonable request. Request can be made through to the regional health director of health service by emailing (braimababa@gmail.com).
References
World Health Organization. Meningitis. WHO 2017. https://www.who.int/health-topics/meningitis#tab=tab_1. Accessed 7 June 2021 (2021).
Tacon, C. L. & Flower, O. Diagnosis and management of bacterial meningitis in the paediatric population: A review. Emerg. Med. Int. 2012–4, 1–8. https://doi.org/10.1155/2012/320309 (2012).
Gilhus, N. E., Barnes, M. P. & Brainin, M. Management of community acquired bacterial meningitis. Eur Handb Neurol Manag 2, 135 (2011).
Hoffman, O. & Weber, J. R. Pathophysiology and treatment of bacterial meningitis. Ther Adv Neurol Disord https://doi.org/10.1177/1756285609337975 (2009).
Bahr, N. C. et al. Diagnostic accuracy of Xpert MTB/RIF Ultra for tuberculous meningitis in HIV-infected adults: A prospective cohort study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(17)30474-7 (2018).
Mustapha, M. M. & Harrison, L. H. Vaccine prevention of meningococcal disease in Africa: Major advances, remaining challenges. Hum. Vaccines Immunother. 14, 1107–1115. https://doi.org/10.1080/21645515.2017.1412020 (2018).
Owusu, M. et al. Aetiological agents of cerebrospinal meningitis: A retrospective study from a teaching hospital in Ghana. Ann. Clin. Microbiol. Antimicrob. 11, 1. https://doi.org/10.1186/1476-0711-11-28 (2012).
Service Ghana Statistical. 2021 Population and Housing Census. (Ghana Stat Serv, 2022).
Ministry of Health. Standard Treatment Guideline. (Ministry of Health, 2017).
Ouattara, M. et al. Triplex real-time PCR assay for the detection of Streptococcus pneumoniae, Neisseria meningitidis and Haemophilus infuenzae directly from clinical specimens without extraction of DNA. Diagn. Microbiol. Infect. Dis. 3, 188–190 (2019).
Durey, A. et al. Carriage rates and serogroups of Neisseria meningitidis among freshmen in a University Dormitory in Korea. Yonsei Med. J. 4, 742–747 (2012).
Ghana Statistical Service. Ghana Demographic and Health Survey, 2014. (Ghana Statistical Service, 2014).
Chiaroni-Clarke, R. C., Munro, J. E. & Ellis, J. A. Sex bias in paediatric autoimmune disease—Not just about sex hormones?. J. Autoimmun. 69, 12–23. https://doi.org/10.1016/j.jaut.2016.02.011 (2016).
Kwambana-Adams, B. A. et al. An outbreak of pneumococcal meningitis among older children (≥ 5 years) and adults after the implementation of an infant vaccination programme with the 13-valent pneumococcal conjugate vaccine in Ghana. BMC Infect. Dis. https://doi.org/10.1186/s12879-016-1914-3 (2016).
Codjoe, S. N. A. & Nabie, V. A. Climate change and cerebrospinal meningitis in the Ghanaian meningitis belt. Int. J. Environ. Res. Public Health 11(7), 6923–6939. https://doi.org/10.3390/ijerph110706923 (2014).
Amidu, N. et al. Diagnosis of bacterial meningitis in Ghana: Polymerase chain reaction versus latex agglutination methods. PLoS ONE 2019, 14. https://doi.org/10.1371/journal.pone.0210812 (2019).
Conen, A. et al. Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: A retrospective analysis over an year period. Clin. Infect. Dis. 11–47, 73–82 (2008).
World Health Organization. Bacterial meningitis. Wkly. Epidemiol. Rec. WHO 80, 313–320 (2005).
Falade, A. G., Lagunju, I. A., Bakare, R. A., Odekanmi, A. A. & Adegbola, R. A. Invasive pneumococcal disease in children aged 5 years admitted to 3 urban hospitals in Ibadan, Nigeria. Clin. Infect. Dis. 48, S190–S196 (2009).
Franco-Paredes, C., Lammoglia, L., Hernandez, I. & SantosPreciado, J. I. Epidemiology and outcomes of bacterial meningitis in Mexican children: 10-year experience (1993–2003). Int. J. Infect. Dis. 12, 380–386 (2008).
Saez-Llorens, X. & McCracken, J. R. Bacterial meningitis in children. Lancet Infect. Dis. 361, 2139–2148 (2003).
Nyarko, K.M., Sackey, S.O., & Noora, C. Supplement article Review of meningitis surveillance data, upper West Region, Ghana 2009–2013. Pan Afr. Med. J. https://doi.org/10.11604/pamj.supp.2016.25.1.6180 (2016).
Thigpen, M. C., Whitney, C. G., Messonnier, N. E., Zell, E. R., Lynfield, R., Hadler, J. L. H, L. H., Farley, M. M., Reingold, A., Bennett, N. M., Craig, A. S., Schaffner, W., Thomas A, Lewis, M. M., Scallan, E. & Schuchat A. Bacterial meningitis in the United States, 1998–2007. N. Engl. J. Med. (England) (2011).
CDC. Epidemiology and Prevention of Vaccine-Preventable Diseases. Vol. B. (CDC, 2012).
Acknowledgements
The authors wish to thank the leadership of Ghana Health Service, Public Health Division and the Disease Surveillance Unit for their support and guidance. We also want to thank the leadership of the TPHRL add the rest for the immense support given to us through the period of data collection and processing. The researcher wishes to thank all patients, guardians, and advisers who allowed/advised patients to participate and provide the GHS with adequate information.
Author information
Authors and Affiliations
Contributions
The authors of the research contributed to diverse areas with specific roles and responsible as denoted; The research work was design and created by E.W.W., B.B.A., E.D.K., B.N., E.B.Y., V.C.K., R.K.A., and A.K.A. who were responsible for data acquisition and retrieval. Data curation was manned by E.W.W., E.B.Y., B.B.A., B.N., and B.A.W. managed the formal data cleaning and analysis. Original draft of the manuscript was owned by E.W.W., B.N., E.D.K., S.A., and A.Y. Revisions and editing of the manuscript were conducted by N.B., E.D.K., H.A.K.A., B.B.A., A.A.K., A.Y., S.Z., and B.A.W. The supervision of the study was done by E.D.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weyori, E.W., Abubakari, B.B., Nkrumah, B. et al. Predictive signs and symptoms of bacterial meningitis isolates in Northern Ghana. Sci Rep 13, 13400 (2023). https://doi.org/10.1038/s41598-023-38253-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38253-z
- Springer Nature Limited