Abstract
This study aimed to analyze the epidemiological characteristics of cleft lip and/or palate (CL/P) and CL/P-related perinatal deaths, provide some information for intervention programs to reduce the incidence of CL/P and provide clues for future researchers. Data were obtained from the Birth Defects Surveillance System in Hunan Province, China, 2016–2020. Incidences of CL/P [number of cases per 1000 fetuses (births and deaths at 28 weeks of gestation and beyond)] with 95% confidence intervals (CI) were calculated by residence, gender, maternal age, year, and major types [cleft lip only (CL), cleft palate only (CP), and cleft lip with palate (CLP)]. Crude odds ratios (ORs) were calculated to examine the association of each maternal characteristic with CL/P. Pearson chi-square tests (χ2) were used to examine the association of each maternal characteristic with CL/P-related perinatal deaths. A total of 847,755 fetuses were registered, and 14,459 birth defects were identified, including 685 CL/P (accounted for 4.74% of all birth defects). CL, CP, and CLP accounted for 24.67% (169 cases), 36.79% (252 cases), and 38.54% (264 cases) of all CL/P, respectively. The incidence of CL/P was 0.81‰ (95%CI 0.75–0.87). The incidence of CL was 0.20‰ (95%CI 0.17–0.23) (169 cases), of CP was 0.30‰ (95%CI 0.26–0.33) (252 cases), and of CLP was 0.31‰ (95%CI 0.27–0.35) (264 cases). CL was more common in males than females (0.24‰ vs. 0.15‰, OR = 1.62, 95%CI 1.18–2.22). CP was more common in urban than rural (0.36‰ vs. 0.25‰, OR = 1.43, 95%CI 1.12–1.83), and less common in males than females (0.22‰ vs. 0.38‰, OR = 0.59, 95%CI 0.46–0.75). CLP was more common in males than females (0.35‰ vs. 0.26‰, OR = 1.36, 95%CI 1.06–1.74). Compared to mothers 25–29 years old, mothers < 20 years old were risk factors for CLP (OR = 3.62, 95%CI 2.07–6.33) and CL/P (OR = 1.80, 95%CI 1.13–2.86), and mothers ≥ 35 years old was a risk factor for CLP (OR = 1.43, 95%CI 1.01–2.02). CL/P-related perinatal deaths accounted for 24.96% (171/685) of all CL/P, of which 90.64% (155/171) were terminations of pregnancy. Rural residents, low income, low maternal age, and early prenatal diagnosis are risk factors for perinatal death. In conclusion, we found that CP was more common in urban areas and females, CL and CLP were more common in males, and CL/P was more common in mothers < 20 or ≥ 35 years old. In addition, most CL/P-related perinatal deaths were terminations of pregnancy. CL/P-related perinatal deaths were more common in rural areas, and the proportion of CL/P-related perinatal deaths decreased with the increase in maternal age, parity, and per-capita annual income. Several mechanisms have been proposed to explain these phenomena. Our study is the first systematic research on CL/P and CL/P-related perinatal deaths based on birth defects surveillance. It is significant for intervention programs to prevent CL/P and CL/P-related perinatal deaths. As well, more epidemiological characteristics of CL/P (such as the location of CL/P) and approaches to reduce CL/P-related perinatal deaths need to be studied in the future.
Similar content being viewed by others
Introduction
Cleft lip and/or palate (CL/P) are classified as cleft lip only (CL), cleft palate only (CP), and cleft lip with palate (CLP)1. It significantly impacts life quality, healthcare use, and costs of patients and their families2,3 and increases the risk of perinatal deaths.
CL/P are common congenital malformations affecting the head and neck and one of the most common birth defects4. The global incidence of CL/P is reported to be 1.08‰5. Previous studies have shown Asia's highest incidence of CL/P4,6,7,8. China is one of the regions with the highest incidence of CL/P. E.g., a meta-analysis in China (1986–2015) showed that the overall incidence of orofacial clefts [referred to all types of clefts (CP, CL, or CLP; syndromic or nonsyndromic forms)] was 1.4 per 1000 live births9.
Through prenatal screening and diagnosis, doctors can diagnose CL/P early and reduce the incidence10. Therefore, studies on the epidemiological characteristics of CL/P are essential for providing evidence for future intervention. However, the epidemiology of CL/P and CL/P-related perinatal deaths have rarely been reported recently. More studies need to be included.
Therefore, we investigated the epidemiology of CL/P and CL/P-related perinatal deaths in Hunan Province, China, using data from the Birth Defects Surveillance System in Hunan Province, 2016–2020. This study aimed to provide some information for intervention programs to reduce the incidence of CL/P and to provide clues for future researchers.
Methods
Data sources
This study used data from the Birth Defects Surveillance System in Hunan Province, China, 2016–2020, which is run by the Hunan Provincial Health Commission and involves 52 representative registered hospitals in Hunan Province. Surveillance data of fetuses (births and deaths at 28 weeks of gestation and beyond) and all birth defects (between 28 weeks of gestation and 7 days after delivery) included demographic characteristics such as residence, gender, maternal age, and other key information.
According to the WHO International Classification of Diseases (Ninth Revision, ICD-9), the ICD code of CL is Q36, CP is Q35, and CLP is Q37.
Informed consents
We confirmed that informed consent was obtained from all subjects and/or their legal guardian(s). Doctors obtain consent from pregnant women before collecting surveillance data, which is witnessed by their families and the heads of the obstetrics or neonatal departments. Doctors obtain consent from their parents or guardians for live births, which are witnessed by their families and the heads of the obstetrics or neonatal departments. Since the Health Commission of Hunan Province collects those data and the government has emphasized the privacy policy in the “Maternal and Child Health Monitoring Manual in Hunan Province”, there is no additional written informed consent.
Ethics guideline statement
The Medical Ethics Committee of Hunan Provincial Maternal and Child Health Care Hospital approved the study (NO: 2022-S94). It is a retrospective study of medical records; all data were fully anonymized before we accessed them. Moreover, we de-identified the patient records before analysis. We confirmed that all experiments were performed following relevant guidelines and regulations.
Data quality control
To carry out surveillance, the Hunan Provincial Health Commission formulated the “Maternal and Child Health Monitoring Manual in Hunan Province”. Data were collected and reported by experienced doctors. To reduce the integrity rate and information error rate, we asked the technical guidance departments to carry out comprehensive quality control each year.
Statistical analysis
The incidence of CL/P is defined as the number of cases per 1000 fetuses (births and deaths at 28 weeks of gestation and beyond) (‰). We computed the incidences of CL/P (CL, CP, and CLP) and 95% confidence intervals (CI) by Poisson’s regression. Crude odds ratios (ORs) were calculated to examine the association of each maternal characteristic with CL/P. Chi-square trend tests (χ2trend) were used to determine trends in incidences of CL/P by year. Pearson Chi-Square tests (χ2) were used to examine the association of each maternal characteristic with CL/P-related perinatal deaths.
All statistical analyses in this study were performed using SPSS 18.0 (International Business Machines Corporation, New York City, United States).
Results
CL/P in Hunan Province, China, 2016–2020
Our study included 847,755 fetuses, and 14,459 birth defects were identified, including 685 CL/P (accounted for 4.74% of all birth defects). CL, CP, and CLP accounted for 24.67% (169 cases), 36.79% (252 cases), and 38.54% (264 cases) of all CL/P, respectively. Table 1 shows the details of CL/P by year.
Incidences of CL/P by residence, gender, and maternal age
The incidence of CL/P was 0.81‰ (95%CI 0.75–0.87). The incidence of CL was 0.20‰ (95%CI 0.17–0.23) (169 cases), of CP was 0.30‰ (95%CI 0.26–0.33) (252 cases), and of CLP was 0.31‰ (95%CI 0.27–0.35) (264 cases).
CL was more common in males than females (0.24‰ vs. 0.15‰, OR = 1.62, 95%CI 1.18–2.22). CP was more common in urban than rural (0.36‰ vs. 0.25‰, OR = 1.43, 95%CI 1.12–1.83) and less common in males than females (0.22‰ vs. 0.38‰, OR = 0.59, 95%CI 0.46–0.75). CLP was more common in males than females (0.35‰ vs. 0.26‰, OR = 1.36, 95%CI 1.06–1.74). Compared to mothers 25–29 years old, mothers < 20 years old were a risk factor for CLP (OR = 3.62, 95%CI 2.07–6.33) and CL/P (OR = 1.80, 95%CI 1.13–2.86), and mothers ≥ 35 years old was a risk factor for CLP (OR = 1.43, 95%CI 1.01–2.02). Table 2 shows the detailed incidences and ORs of CL/P by residence, gender, and maternal age.
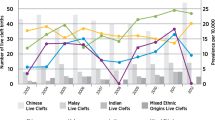
Incidences of CL/P by year
From 2016 and 2020, the incidences of CL/P were 0.88‰ (95%CI 0.74, 1.03), 0.85‰ (95%CI: 0.72, 0.97), 0.73‰ (95%CI 0.61, 0.86), 0.76‰ (95%CI 0.63, 0.89), and 0.82‰ (95%CI 0.67, 0.97), respectively, and showed generally steady (χ2trend = 1.19, P = 0.28). Table 3 shows the detailed incidences of CL/P by year.
CL/P-related perinatal deaths
CL/P-related perinatal deaths accounted for 24.96% (171/685) of all CL/P, and 90.64% (155/171) of CL/P-related perinatal deaths were terminations of pregnancy. Perinatal deaths due to CL, CP, and CLP accounted for 8.88%, 3.97%, and 55.30% of all cases, respectively. And terminations of pregnancy due to CL, CP, and CLP accounted for 80.00%, 50.00%, and 94.52% of all deaths, respectively. The proportion of CLP-related perinatal deaths was relatively high. (χ2 = 212.38, P = 0.00). Table 4 shows the details of CL/P-related perinatal deaths.
Epidemiology of CL/P-related perinatal deaths
Table 5 showed the following epidemiological characteristics of CL/P-related perinatal deaths: (1) CL/P-related perinatal deaths were more common in rural than urban areas. (2) The proportion of CL/P-related perinatal deaths decreased with the increase in maternal age, parity, and per-capita annual income. (3) The proportion of CL/P-related perinatal deaths was higher in the B-Ultrasound diagnosis group. And the earlier the diagnosis, the higher the proportion of CL/P-related perinatal deaths. Table 5 shows the detailed epidemiology of CL/P-related perinatal deaths.
Discussion
Overall, we found a relatively high incidence of CL/P, and residence, gender, and maternal age impacted the incidence of CL/P. In addition, we found that CL/P-related perinatal deaths were associated with some epidemiological characteristics.
The incidence of CL/P (0.81‰) in our study is lower than the global incidence (1.08‰) or the reported incidence in China (1.4‰)5,9. Another comprehensive study by Cooper et al. also reported higher incidences of CL/P than ours: the incidences of CL/P in Chinese, Japanese, and other Asians were 1.30‰, 1.34‰ and 1.47‰, and the total incidence of CL/P in Asians was 1.33‰ (2006)11. The following are incidences of CL/P reported in some regions: 1.11‰ in South Korea, 2005–200612, 1.5‰ in the Netherlands, 2008–201213, 1.64‰ in the Czech Republic, 1994–200814, 0.6‰ in Colombia, 2009–201715, 0.65‰ in Saudi Arabia, 2013–201616, and 0.76‰ in Guangdong Province, China, 2015–201817. There are significant differences between them. And it seems the incidences of CL/P were higher in high-income countries. Several studies have also reported incidences of CL, CP, and CLP. E.g., the global incidences of CL, CP, and CLP were 0.3‰, 0.33‰, and 0.45‰, respectively5; The incidences of CL, CP, and CLP in South Korea were 0.28‰, 0.56‰ and 0.27‰ respectively12; The incidences of CL, CP, and CLP in Guangdong Province, China, were 0.23‰, 0.22‰ and 0.30‰, respectively17; The incidences of CL, CP, and CLP in Fangshan District, Beijing, China, were 0.62‰, 0.34‰ and 0.94‰, respectively18. There are also significant differences between them.
We infer that several factors may be related to these differences. First, it may reflect the frequency of defective genes for CP/L in different regions. E.g., Mitchell et al. found that the incidence of CL/P was higher in Asians than Caucasians than Africans6. Second, differences in access to diagnostic services may contribute to these results. Better access to diagnostic services for pregnant women in high-income countries resulted in more defects being detected19. The reason for the lower incidence of CL/P in this study may also be mainly related to prenatal screening and diagnosis (such as the use of B-ultrasound), and many fetuses with CL/P were diagnosed and terminated before 28 weeks of gestation. Third, some other factors may also be related to these differences. E.g., many studies mentioned above include relatively few cases or limited data.
We also found that CL/P was associated with residence, gender, and maternal age. E.g., CP was more common in urban than rural areas. It is consistent with some studies in low- and middle-income countries, such as Brazil and Jordan20,21, and inconsistent with some studies in high-income countries, such as the US and South Korea22,23. It may be mainly related to lower access to healthcare and diagnostic technologies for birth defects in rural areas24. In addition, some adverse conditions in urban areas may also contribute to this phenomenon, such as air pollution25,26,27,28. CL and CLP were more common in males, while CP was more common in females. It is consistent with previous studies14,29,30,31,32. The higher incidences of CL and CLP in males might be caused by the higher sensitivity of male fetuses to environmental stress, leading to the appearance of congenital birth defects14,33. CL/P was more common in mothers < 20 or ≥ 35 years old. It is consistent with previous studies34,35,36,37,38. It may be related to low-quality oocytes and semen for parents aged ≥ 35 years old34,39,40,41. And mothers < 20 years old may lack physical maturity and have a deficiency in vitamins (such as folic acid), which has been associated with birth defects42.
In addition, we found that CL/P-related perinatal deaths were associated with residence, maternal age, income, parity, methods, and time of diagnosis. It has been rarely reported recently. First, CL/P-related perinatal deaths were more common in rural areas, and the proportion of CL/P-related perinatal deaths decreased with the increase in maternal age, parity, and per-capita annual income. And more than 90% of CL/P-related perinatal deaths were terminations of pregnancy. It suggests that CL/P-related perinatal deaths may be mainly related to economic conditions43,44,45,46. CL/P significantly impacts babies’ life quality, healthcare use, and costs of patients and their families7. Therefore, better economic conditions benefit children's treatment and may make birth more likely. Second, CL/P-related perinatal deaths were associated with the methods and time of diagnosis. It is mainly concerned with the health of mothers. On the one hand, most CL/P-related perinatal deaths are therapeutic terminations of pregnancy4,47. On the other hand, the earlier CL/P is diagnosed and terminated, the less adverse impact termination has on mothers and their families. Therefore, most mothers terminate as soon as possible after diagnosing CL/P. Currently, B-Ultrasound is the most common and effective prenatal screening and diagnostic method, and many CL/P can be detected early in pregnancy by B-Ultrasound. Therefore, the proportion of CL/P-related perinatal deaths was higher in the B-Ultrasound diagnosis group.
Some things could be improved in our study. E.g., we did not analyze some epidemiological features due to data limitations, including the father’s information and the location of CL/P (left, center, or right). To address these limitations, first, the Monitoring Manual for Birth Defects Surveillance needs improvement; second, more studies should focus on the epidemiological characteristics of CL/P.
Conclusion
In conclusion, we found that CP was more common in urban areas and females, CL and CLP were more common in males, and CL/P was more common in mothers < 20 or ≥ 35 years old. In addition, most CL/P-related perinatal deaths were terminations of pregnancy. CL/P-related perinatal deaths were more common in rural areas, and the proportion of CL/P-related perinatal deaths decreased with the increase in maternal age, parity, and per-capita annual income. Several mechanisms have been proposed to explain these phenomena. Our study is the first systematic research on CL/P and CL/P-related perinatal deaths based on birth defects surveillance. It is significant for intervention programs to prevent CL/P and CL/P-related perinatal deaths. As well, more epidemiological characteristics of CL/P (such as the location of CL/P) and approaches to reduce CL/P-related perinatal deaths need to be studied in the future.
Data availability
All data generated or analysed during this study are included in this published article.
References
Allori, A. C., Mulliken, J. B., Meara, J. G., Shusterman, S. & Marcus, J. R. Classification of cleft lip/palate: Then and now. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 54, 175–188. https://doi.org/10.1597/14-080 (2017).
Wehby, G. L. & Cassell, C. H. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis. 16, 3–10. https://doi.org/10.1111/j.1601-0825.2009.01588.x (2010).
Martín-Del-Campo, M., Rosales-Ibañez, R. & Rojo, L. Biomaterials for cleft lip and palate regeneration. Int. J. Mol. Sci. 20, 2176. https://doi.org/10.3390/ijms20092176 (2019).
Worley, M. L., Patel, K. G. & Kilpatrick, L. A. Cleft lip and palate. Clin. Perinatol. 45, 661–678. https://doi.org/10.1016/j.clp.2018.07.006 (2018).
Salari, N. et al. Global prevalence of cleft palate, cleft lip and cleft palate and lip: A comprehensive systematic review and meta-analysis. J. Stomatol. Oral Maxillofac. Surg. 123, 110–120. https://doi.org/10.1016/j.jormas.2021.05.008 (2022).
Mitchell, L. E. Genetic epidemiology of birth defects: Nonsyndromic cleft lip and neural tube defects. Epidemiol. Rev. 19, 61–68. https://doi.org/10.1093/oxfordjournals.epirev.a017947 (1997).
Setó-Salvia, N. & Stanier, P. Genetics of cleft lip and/or cleft palate: Association with other common anomalies. Eur. J. Med. Genet. 57, 381–393. https://doi.org/10.1016/j.ejmg.2014.04.003 (2014).
IPDTOC Working Group. Prevalence at birth of cleft lip with or without cleft palate: Data from the International Perinatal Database of Typical Oral Clefts (IPDTOC). Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 48(66–81), 2011. https://doi.org/10.1597/09-217 (2011).
Wang, M. et al. Prevalence of orofacial clefts among live births in China: A systematic review and meta-analysis. Birth Defects Res. 109, 1011–1019. https://doi.org/10.1002/bdr2.1043 (2017).
Paaske, E. B. & Garne, E. Epidemiology of orofacial clefts in a Danish county over 35 years—Before and after implementation of a prenatal screening programme for congenital anomalies. Eur. J. Med. Genet. 61, 489–492. https://doi.org/10.1016/j.ejmg.2018.05.016 (2018).
Cooper, M. E., Ratay, J. S. & Marazita, M. L. Asian oral-facial cleft birth prevalence. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 43, 580–589. https://doi.org/10.1597/05-167 (2006).
Lee, C. W., Hwang, S. M., Lee, Y. S., Kim, M. A. & Seo, K. Prevalence of orofacial clefts in Korean live births. Obstet. Gynecol. Sci. 58, 196–202. https://doi.org/10.5468/ogs.2015.58.3.196 (2015).
Fleurke-Rozema, J. H. et al. Prevalence, diagnosis and outcome of cleft lip with or without cleft palate in The Netherlands. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 48, 458–463. https://doi.org/10.1002/uog.15834 (2016).
Urbanova, W., Kotova, M. & Vankova, Z. The incidence of cleft lip and palate in the Czech Republic in 1994–2008. Bratisl. Lekarske Listy 114, 474–479. https://doi.org/10.4149/bll_2013_099 (2013).
Alonso, R. R. H. & Brigetty, G. P. S. Analysis of the prevalence and incidence of cleft lip and palate in Colombia. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 57, 552–559. https://doi.org/10.1177/1055665619886455 (2020).
Alyami, B. et al. Prevalence and clinical case series of syndromic and nonsyndromic cleft lip and palate in a Saudi Arabian Neonatal Population. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 57, 1259–1265. https://doi.org/10.1177/1055665620929247 (2020).
Zhu, Y. et al. Prevalence of cleft lip and/or cleft palate in Guangdong province, China, 2015–2018: A spatio-temporal descriptive analysis. BMJ Open 11, e046430. https://doi.org/10.1136/bmjopen-2020-046430 (2021).
Yang, Y., Liu, H., Ma, R. & Jin, L. Prevalence of cleft lip/palate in the Fangshan District of Beijing, 2006–2012. Cleft Palate-Craniofacial J. Off. Publ. Am. Cleft Palate-Craniofacial Assoc. 55, 1296–1301. https://doi.org/10.1177/1055665618767115 (2018).
Liu, Y. et al. Global birth prevalence of congenital heart defects 1970–2017: Updated systematic review and meta-analysis of 260 studies. Int. J. Epidemiol. 48, 455–463. https://doi.org/10.1093/ije/dyz009 (2019).
Rios Moura, J. et al. Clinical-epidemiological profile of orofacial fissures in a reference center from northeast Brazil. Rev. Salud Publica (Bogota Colombia) 21, 209–216. https://doi.org/10.15446/rsap.V21n2.74065 (2019).
Alfwaress, F. S. D., Khwaileh, F. A., Rawashdeh, M. A., Alomari, M. A. & Nazzal, M. S. Cleft lip and palate: Demographic patterns and the associated communication disorders. J. Craniofacial Surg. 28, 2117–2121. https://doi.org/10.1097/scs.0000000000003984 (2017).
Kapos, F. P., White, L. A., Schmidt, K. A., Hawes, S. E. & Starr, J. R. Risk of non-syndromic orofacial clefts by maternal rural–urban residence and race/ethnicity: A population-based case-control study in Washington State 1989–2014. Paediatr. Perinat. Epidemiol. 35, 292–301. https://doi.org/10.1111/ppe.12727 (2021).
Shin, H., Ahn, E. & Choi, E. J. Access to antenatal healthcare and the prevalence of oral clefts: A spatial analysis. Eur. J. Oral Sci. 128, 145–152. https://doi.org/10.1111/eos.12688 (2020).
Cui, M. et al. Knowledge and intake of folic acid to prevent neural tube defects among pregnant women in urban China: A cross-sectional study. BMC Pregnancy Childbirth 21, 432. https://doi.org/10.1186/s12884-021-03893-4 (2021).
Benavides, E. et al. Urban-rural residence and birth defects prevalence in Texas: A phenome-wide association study. Pediatr. Res. https://doi.org/10.1038/s41390-021-01700-6 (2021).
Sun, S. et al. Associations between air pollution exposure and birth defects: A time series analysis. Environ. Geochem. Health 43, 4379–4394. https://doi.org/10.1007/s10653-021-00886-2 (2021).
Rao, A., Ahmed, M. K., Taub, P. J. & Mamoun, J. S. The correlation between maternal exposure to air pollution and the risk of orofacial clefts in infants: A systematic review and meta-analysis. J. Oral Maxillofac. Res. 7, e2. https://doi.org/10.5037/jomr.2016.7102 (2016).
Xing, Z., Zhang, S., Jiang, Y. T., Wang, X. X. & Cui, H. Association between prenatal air pollution exposure and risk of hypospadias in offspring: A systematic review and meta-analysis of observational studies. Aging (Albany NY) 13, 8865–8879. https://doi.org/10.18632/aging.202698 (2021).
Stoll, C., Alembik, Y., Dott, B. & Roth, M. P. Epidemiological and genetic study in 207 cases of oral clefts in Alsace, north-eastern France. J. Med. Genet. 28, 325–329. https://doi.org/10.1136/jmg.28.5.325 (1991).
Milan, M. et al. 766 cases of oral cleft in Italy. Data from Emilia Romagna (IMER) and northeast Italy (NEI) registers. Eur. J. Epidemiol. 10, 317–324. https://doi.org/10.1007/bf01719356 (1994).
Croen, L. A., Shaw, G. M., Wasserman, C. R. & Tolarová, M. M. Racial and ethnic variations in the prevalence of orofacial clefts in California, 1983–1992. Am. J. Med. Genet. 79, 42–47. https://doi.org/10.1002/(sici)1096-8628(19980827)79:1%3c42::aid-ajmg11%3e3.0.co;2-m (1998).
Lithovius, R. H., Ylikontiola, L. P., Harila, V. & Sándor, G. K. A descriptive epidemiology study of cleft lip and palate in Northern Finland. Acta Odontol. Scand. 72, 372–375. https://doi.org/10.3109/00016357.2013.840737 (2014).
Wells, J. C. Natural selection and sex differences in morbidity and mortality in early life. J. Theor. Biol. 202, 65–76. https://doi.org/10.1006/jtbi.1999.1044 (2000).
Herkrath, A. P., Herkrath, F. J., Rebelo, M. A. & Vettore, M. V. Parental age as a risk factor for non-syndromic oral clefts: A meta-analysis. J. Dent. 40, 3–14. https://doi.org/10.1016/j.jdent.2011.10.002 (2012).
Shapira, Y., Haklai, Z., Blum, I., Shpack, N. & Amitai, Y. Prevalence of non-syndromic orofacial clefts among Jews and Arabs, by type, site, gender and geography: A multi-center study in Israel. Isr. Med. Assoc. J. IMAJ 16, 759–763 (2014).
Luo, Y. L. et al. Birth prevalence of orofacial clefts among perinatal infants: A register-based study in Bao’an district, Shenzhen, China. Birth Defects Res. 111, 353–359. https://doi.org/10.1002/bdr2.1467 (2019).
James, O. et al. Parental age and the risk of cleft lip and palate in a Nigerian population—A case-control study. Ann. Maxillofac. Surg. 10, 429–433. https://doi.org/10.4103/ams.ams_134_20 (2020).
Li, L. et al. Analysis of birth defect rate trend of cleft lip and palate in Shanghai from 2007 to 2016. Zhonghua kou qiang yi xue za zhi Zhonghua kouqiang yixue zazhi Chin. J. Stomatol. 53, 301–306. https://doi.org/10.3760/cma.j.issn.1002-0098.2018.05.003 (2018).
Mikwar, M., MacFarlane, A. J. & Marchetti, F. Mechanisms of oocyte aneuploidy associated with advanced maternal age. Mutat. Res. Rev. Mutat. Res. 785, 108320. https://doi.org/10.1016/j.mrrev.2020.108320 (2020).
Janeczko, D., Hołowczuk, M., Orzeł, A., Klatka, B. & Semczuk, A. Paternal age is affected by genetic abnormalities, perinatal complications and mental health of the offspring. Biomed. Rep. 12, 83–88. https://doi.org/10.3892/br.2019.1266 (2020).
Hermann, N. V., Darvann, T. A., Munch, A. & Kreiborg, S. Parental age in relation to the severity of cleft lip and/or palate. Orthod. Craniofacial Res. 21, 236–241. https://doi.org/10.1111/ocr.12241 (2018).
DeRoo, L. A., Gaudino, J. A. & Edmonds, L. D. Orofacial cleft malformations: associations with maternal and infant characteristics in Washington State. Birth Defects Res. Part A Clin. Mol. Teratol. 67, 637–642. https://doi.org/10.1002/bdra.10114 (2003).
Holzmer, S., Davila, A. & Martin, M. C. Cost utility analysis of staged versus single-stage cleft lip and palate repair. Ann. Plast. Surg. 84, S300-s306. https://doi.org/10.1097/sap.0000000000002255 (2020).
McIntyre, J. K. et al. Number of surgical procedures for patients with cleft lip and palate from birth to 21 years old at a single children’s hospital. Ann. Plast. Surg. 76(Suppl 3), S205-208. https://doi.org/10.1097/sap.0000000000000765 (2016).
Harb, J. L., Crawford, K. L., Simmonds, J. C., Roberts, C. & Scott, A. R. Race, income, and the timeliness of cleft palate repair in the United States. Cureus 13, e13414. https://doi.org/10.7759/cureus.13414 (2021).
Carlson, L. C. et al. A model of the unmet need for cleft lip and palate surgery in low- and middle-income countries. World J. Surg. 40, 2857–2867. https://doi.org/10.1007/s00268-016-3637-4 (2016).
Michel, B. et al. Pregnancy and neonatal outcome following an antenatal diagnosis of cleft lip and palate. J. Perinat. Med. 41, 287–294. https://doi.org/10.1515/jpm-2012-0137 (2013).
Acknowledgements
The authors wish to thank the staff working for the Birth Defects Surveillance System of Hunan Province, China, from 2016 to 2020.
Author information
Authors and Affiliations
Contributions
X.Z., T.L., H.K., Q.L., D.X. and J.H. contributed to data collection. X.Z., Y.J., J.F. and H.W. analyzed the data, and manuscript preparation. All authors contributed to the study conception, design, and read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, X., Jiang, Y., Fang, J. et al. Incidence of cleft lip and palate, and epidemiology of perinatal deaths related to cleft lip and palate in Hunan Province, China, 2016–2020. Sci Rep 13, 10304 (2023). https://doi.org/10.1038/s41598-023-37436-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37436-y
- Springer Nature Limited
This article is cited by
-
Fetal deaths from birth defects in Hunan Province, China, 2016–2020
Scientific Reports (2024)
-
Perinatal deaths from birth defects in Hunan Province, China, 2010–2020
BMC Pregnancy and Childbirth (2023)