Abstract
Little is known about the demographics of people who use cannabis, including how use trends within population subgroups have evolved over time. It is therefore challenging to know if the demographics of participants enrolled in cannabis clinical trials are representative of those who use cannabis. To fill this knowledge gap, data from the National Survey on Drug Use and Health (NSDUH) on “past-month” cannabis use across various population subgroups in the United States was examined from 2002 to 2021. The most notable increases in “past-month” cannabis use prevalence occurred in those aged 65 and older (2,066.1%) and 50–64-year-olds (472.4%). In 2021, people reporting “past-month” cannabis use were 56.6% male and 43.4% female. Distribution across self-reported race and ethnicity was 64.1% White, 14.3% Black, 14.1% Hispanic, and 3.1% more than one race. And many ages were represented as 24.4% were 26–34, 24.1% were 35–49, 22.4% were 18–25, and 17.6% were 50–64 years old. To understand if these population subgroups are represented in cannabis clinical trials, participant demographics were extracted from peer-reviewed clinical trials reporting on pharmacokinetic and/or pharmacodynamic models of cannabis or cannabinoids. Literature was grouped by publication year (2000–2014 and 2015–2022) and participant prior exposure to cannabis. Results identified that cannabis clinical trial participants are skewed toward overrepresentation by White males in their 20s and 30s. This represents structural discrimination in the research landscape that perpetuates social and health inequities.
Similar content being viewed by others
Introduction
The shifting legal status of cannabis in the United States (US) and internationally is resulting in increased research interest into cannabis and cannabinoid pharmacokinetics and pharmacodynamics1,2,3,4. Cannabis and cannabinoid pharmacology and epidemiology are the focus of several federal Requests for Proposals and Notices of Special Interest. Despite renewed pharmacological research interest, little is known about the demographics of people who currently or have recently used cannabis, including how use trends have evolved over time. In 2018, an extensive review on national trends in adult cannabis use was published5, considering data from 2002 through 2014 in participants aged 18–25 and those aged 26 and older6,7. It was noted that increases in cannabis use occurred across sex, region, educational level, and employment status6,8. However, the detailed demographics of people who use cannabis was not critically assessed nor reported. In 2019, Cerdá et. al. found that recreational cannabis legalization was associated with increases in frequent cannabis use among adults9. However, impacts of demographic variables beyond age were not assessed. Also in 2019, Hasin et. al. published a narrative review on cannabis use trends by sociodemographic subgroups, summarizing data from several national surveys and a literature review10. They concluded that cannabis use had increased across all sociodemographic subgroups including age sex, race, ethnicity, educational level, and location10. While this work was comprehensive and complete, survey results through 2015 were considered, and an update is required. In 2022, Waddell et. al. reported on the age, sex, and race-varying rates of cannabis use in veterans and non-veterans11. Although the demographic characteristics of these populations were assessed, this work focused on interactions of demographic details and veteran status as risk factors for alcohol and cannabis use11.
It is well known that cannabis pharmacokinetics and pharmacodynamics vary intra- and inter-personally12. Cannabis effects may be moderated by a wide range of factors such as sex, age, race, and ethnicity. For example, preclinical work from rodent ∆9-tetrahydrocannabinol (∆9-THC) dosing studies demonstrates that metabolism and bioaccumulation of ∆9-THC and psychoactive metabolites are significantly impacted by rodent sex. Human studies have also identified sex differences in subjective cannabis effects13,14,15,16, although additional exploration is needed. Similarly, aging is associated with metabolic changes, morbidities, and an overall decline in functioning17, likely impacting cannabis pharmacology. However, only a few studies have evaluated the pharmacology of cannabis in older adults18,19,20,21. The authors were unable to find literature describing demographics of people who currently or have recently used cannabis. However, two recent reviews and meta-analysis of published works on cannabis use disorder and behavioral health found that approximately 70% of study participants were male, 72% were non-Hispanic White, and the median participant age (SD) was 29.9 (9)22,23,24. However, balanced clinical trial participant pools must be demographically representative of those who use cannabis to gather generalizable results translatable to public policy. We hypothesize that cannabis clinical trial participants do not represent the sex, race, ethnicity, and age characteristics of people who use cannabis. One may argue that most fundamental pharmacokinetics and pharmacodynamics assessments of cannabis or cannabinoids do not aim to inform statutory or policy language. However, the lack of knowledge surrounding cannabis pharmacokinetics and impairment forces policy makers, enforcement officials, and other stakeholders to apply any available works to their immediate public health and safety needs. That is, results from any cannabis pharmacokinetics or pharmacodynamics studies in humans are likely to be read by and applied to those tasked with crafting evidence-based policies, recommendations, or assessments. This begs the question, what are the demographics of cannabis clinical trial participants, and do they reflect those of people who use cannabis? To begin answering this question, we will consider two data sources: (1) participant demographics extracted from a systematic review of cannabis pharmacokinetics and/or pharmacodynamics studies and (2) results from the United States National Survey on Drug Use and Health (NSDUH) from years 2002–2021. To the best of our knowledge, this is the first study comparing the demographics of cannabis clinical trial participants to those of people who use cannabis.
Methods
NSDUH survey results
The National Survey on Drug Use and Health (NSDUH) is a nationally representative and cross-sectional survey of individuals aged 12 years or older living in households or non-institutional group housing (e.g., college dormitories, but not jails or prisons) or with no permanent housing (e.g., residence in a shelter). The NSDUH uses a multistage area probability sample for each US state and the District of Columbia and an audio computer-assisted interviewing method to support confidential and private responses25. It is a key source of national and state-level data on the prevalence of substance use and health in the US.
Self-reported “past-month” cannabis use was examined by demographic characteristics within the 2002–2021 NSDUH data. All analyses used the Substance Abuse & Mental Health Data Archive (SAMHDA) Public-use Data Analysis System (PDAS) to query the NSDUH data. Self-reported “past-month” cannabis use (MRJMON, Rc-Marijuana—Past Month Use) was considered as a function of respondent sex (IRSEX, Imputed Revised Gender). Similarly, other variables were considered such as reported race and ethnicity (NEWRACE2, Rc-Race/Hispanicity Recode, 7 Levels). This included the following options: non-Hispanic White, non-Hispanic Black/African American, non-Hispanic Native American or Alaskan Native, non-Hispanic Native Hawaiian or Other Pacific Islander, non-Hispanic Asian, non-Hispanic more than one race, or Hispanic. A combined sex by race variable was also used (SEXRACE, Rc-Combined Gender by Race Indicator) for those who identify as non-Hispanic White, non-Hispanic Black, or Hispanic. Similarly, age was considered (CATAG6, Rc-Age Category Recode, 6 Levels) in the ranges of 12–17, 18–25, 26–34, 35–49, 50–64, and 65 + years old. Prior to 2005, the 6-Level age category was not available. Therefore, CATAG5 (Rc-Age Category Recode, 5 Levels) was used for years 2002 through 2004 for the age ranges of 12–17, 18–25, 26–34, and 35–49 years old. A combination of sex and age category was also used (SEXAGE, Rc-Combined Gender by Age Category Indicator) which identified the distribution of males and females within 12–17 and 18–25 age groups.
“Past-month” cannabis use was reported in eSupplement Table S1 as the weighted count, prevalence, and distribution within a population subgroup. Prevalence and distribution estimates were reported alongside their 95% confidence interval (CI). The prevalence was found by dividing the weighted count of “past-month” cannabis use by the weighted count of the population subgroup surveyed. For example, an estimated 12,861,131 non-Hispanic White males engaged in “past-month” cannabis use out of an estimated total of 84,158,445 non-Hispanic White males in the US. Therefore, it is estimated that 15.3% of non-Hispanic White males engaged in “past-month” cannabis use. The distribution was found by dividing the weighted count of “past-month” cannabis use by the weighted count of all who engaged in “past-month” cannabis use. For example, an estimated 12,861,131 non-Hispanic White males used cannabis in the “past-month” out of an estimated total of 36,172,820 people engaging in “past-month” cannabis use. This means non-Hispanic White males represent 35.6% of all people estimated to engage in “past-month” cannabis use.
Our study was exempt from IRB approval per the University of Wisconsin-Madison’s policy on publicly available, de-identified data sets. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies (e.g., clear variable specification, description of statistical analysis, and reporting 95% confidence intervals)26.
Statistical analysis
Weighted crosstab analysis was used to identify and extract self-reported “past-month” cannabis use by age, sex, and race and ethnicity from 2002 through 2021. Results were displayed as weighted count, prevalence, and distribution (see eSupplement Table S1). Prevalence and distribution estimates also included 95% confidence intervals (CI). Time trends in “past-month” use prevalence across relevant population subgroups were calculated for 2002 through 2021. Logistic regression analysis was performed on annual prevalence estimates to identify statistically significant trend directionality (i.e., increase, decrease, no change) over time using R version 4.2.3 for Windows27. Regression lines were fitted to prevalence estimates using linear regression fits in which the dependent variable was the annual prevalence estimates. Linear regression models include slope (β), y-intercept (α), and their standard errors. Results from linear regression models are included as eSupplement Table S2. Goodness of fit was assessed through the residual standard error and coefficient of determination (R2) values. Residual standard error was found as the standard deviation of residuals using 18 degrees of freedom. A right-tailed F-test was used to identify model significance through the F-statistic (F) and p-value (p). Due to methodological changes in the 2005 NSDUH, the 6-level age category was not available for the 50–64 and 65 and older age ranges in years 2002 through 2004.
Literature search strategy and study eligibility
Literature was identified that described the pharmacokinetics and/or pharmacodynamics of cannabis or cannabinoids in humans. Search terms included “cannabis”, “cannabinoids”, “cannabidiol”, “CBD”, “tetrahydrocannabinol”, “THC”, “pharmacokinetics”, “PK”, “pharmacodynamics”, and “PD” alone and in combination with one another. The search focused on literature presenting relevant models derived from data on humans published between January of 2000 and May of 2022. PubMed and Web of Science were searched and, following guidance from the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA)28,29. This review was not registered with any databases and no protocol was prepared prior to literature search. The reference list was screened by both authors for inclusion in this work. After removal of duplicates, article titles and abstracts were considered by at least one author. Inclusion criteria included literature subjected to peer-review, data originating from a clinical trial, and description of a pharmacokinetics and/or pharmacodynamics model of one or more cannabinoids. Exclusion criteria included pre-clinical works, reviews, meta-analyses, novel drug delivery investigations, and efficacy-focused studies. Each full-text article was then assessed by both authors for inclusion in this work. Studies that re-analyzed data from previously published works or had clinical trials that generated multiple publications were coalesced.
Data extraction
Both authors independently extracted the following data from each article: (1) participant type (i.e. healthy vs. patient), (2) previous cannabis exposure (i.e., naïve, mild, severe), (3) total number of participants, (4) administration route, (5) time of last plasma sample, (6) pharmacokinetics model (yes/no), (7) pharmacodynamics model (yes/no), (8) pharmacodynamics indicator reported, (9) participant sex, (10) participant age, and (11) participant race and ethnicity. Not all articles reported participant sex, age, race, and ethnicity.
Results
Shifting trends in recent cannabis use demographics
In 2021, NSDUH estimates 12.9% of Americans (representing an estimated 36,172,820 people) used cannabis in the “past-month”30. This striking proportion of the population using cannabis recently and/or regularly is the culmination of a steady increase in societal acceptance of cannabis and cannabis use. Linear regression analysis identified trend directionality, and detailed results are provided in eSupplement Table S2. All population subgroups experienced significant changes in “past-month” cannabis use prevalence. Increases were identified in all age groups, Fig. 1, except 12–17-year-olds which decreased. The weighted counts of “past-month” cannabis use among 12–17-year-olds decreased 26.9% from 2002 to 2021 whereas 18–25-year-olds increased 50.9%. Similarly, the increase for 26–34-year-olds was 224.9% and 35–49-year-olds was 148.0%. Older Americans saw larger increases with 50–64-year-olds increasing 472.4% and those aged 65 and older increasing 2,066.1% from 2005 to 2021.
Increasing cannabis use is also observed, although unevenly, across sex and racial and ethnic groups, Fig. 2. Weighted counts of “past-month” cannabis use increased in non-Hispanic White males by 90.9%, non-Hispanic Black males by 115.8%, and Hispanic males by 292.7% from 2002 to 2021. Estimated increases in “past-month” cannabis use were larger for females as non-Hispanic White females increased by 153.4%, non-Hispanic black females by 258.6%, and Hispanic females by 332.4% from 2002 to 2021. These disproportionate increases in “past-month” cannabis use by females are closing the long-standing cannabis use sex gap. In 2021, 43.4% of people reporting “past-month” cannabis use were female.
NSDUH data including the percentage of each group engaging in “past-month” cannabis use (prevalence) for years 2002 through 2021 for (A) non-Hispanic White males (black squares) and females (red circles), (B) non-Hispanic Black males (black squares) and females (red circles), and (C) Hispanic males (black squares) and females (red circles).
Recent cannabis use demographics
The demographics of people who have recently used cannabis was identified from 2021 NSDUH data. In 2021, a total of 69,850 US residents completed the NSDUH. Weighted demographics of respondents, as shown in eSupplement Table S3, were 48.9% male, 61.1% non-Hispanic White, 17.8% Hispanic, 12.2% non-Hispanic Black, and 5.8% non-Hispanic Asian. Due to the SARS-CoV-2 pandemic, NSDUH introduced web-based interviewing and the total number of completed interviews in 2020 was about half of prior years. A smaller sample size in 2020 impacts estimates for small population subgroups and rare behaviors. While the total number of completed interviews in 2021 returned to the annual goal of nearly 70,000, web-based interviewing persisted. For this work, 2020 response rates were adequate to generate national estimates of “past-month” cannabis use across the demographic variables considered. Therefore trend analysis included 2020 and 2021 data.
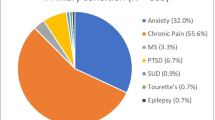
Overall, 12.9% of the 2021 respondents reported “past-month” cannabis use. Considering all people engaging in “past-month” cannabis use, demographic distributions were 43.4% female, 64.1% White, 14.3% Black or African American, 1.3% Native American or Alaskan Native, 2.5% Asian, 3.2% two or more races, and 14.1% Hispanic (see Fig. 3A). Those identifying as non-Hispanic White, non-Hispanic Black, and Hispanic were further broken down into male and female population subgroups, as shown in eSupplement Table S1. Within these population subgroups, males continue to report “past-month” cannabis use more often than females, although the gap has been shrinking in recent years (see Fig. 2). Considering age, the distribution of “past-month” cannabis use was predominantly in the 18–25 (22.4%), 26–34 (24.4%), 35–49 (24.1%), and 50–64 (17.6%) age ranges. However, as Fig. 1F shows, the prevalence of “past-month” cannabis use within the 65 years of age and older category is steadily increasing.
Comparison of the race and ethnicity of (A) people reporting “past-month” cannabis use via the NSDUH and (B) cannabis clinical trials including healthy participants with prior (mild or severe) cannabis experience which were published from 2015 to 2022. Herein Black represents Black or African American, NA/AK represents Native American or Alaskan Native, NH/OPI represents Native Hawaiian or Other Pacific Islander, and > 1 race represents two or more races. It must be noted that the NSDUH requires respondents to select their race and ethnicity simultaneously whereas clinical trial studies that reported these details treated race and ethnicity as separate, overlapping entities.
Cannabis clinical trial participant demographics
Results of the literature search and selection process are detailed in Fig. 4. A total of 41 publications16,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70 fit the search criteria and included unique participant pools, totaling 967 participants, see details in Table 1. Of those, 39 publications16,31,32,33,34,35,36,37,38,39,40,41,42,43,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,65,66,67,68,69,70 including 847 participants reported the number of males (573, 67.7%) and females (274, 32.3%). Only 20 publications16,32,37,40,41,42,45,46,48,50,51,58,59,60,61,62,63,65,66,70 reported at least some participant race information, see eSupplement Table S4. These publications included 404 (47.7% of total) participants, but race information was reported for 377 (93.3%) of those participants. From available information, participants were White (313, 83.0%), Black (24, 6.4%), Asian (9, 2.4%), two or more races (12, 3.2%), Native American (2, 0.5%), or "other" (3, 0.8%). Participant ethnicity was reported in 5 publications45,48,60,65,70 (11.9%), including 139 (16.4%) total participants and 14 (10.1%) who identified as Hispanic.
PRISMA 2020 flow diagram29.
Detailed participant age information was available in 6 publications38,41,43,55,58,63 including 155 participants. Those works included participants in the following age ranges: 14–15 (1, 0.6%), 16–17 (1, 1.3%), 18–19 (25, 16.1%), 20–29 (79, 51%), 30–39 (19, 12.3%), 40–49 (10, 6.5%), 50–59 (9, 5.8%), and 60–69 (10, 6.5%). In addition, 37 publications16,32,33,34,35,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,65,66,68,69,70 reported age ranges including 907 participants. The minimum age considered was 15 and maximum was 79 years old. Considering the minimum age, the mean was 23.9, the median was 21, and the range was 15–52 years old. Considering the maximum age, the mean was 44.3, the median was 43, and the range was 25–79 years old.
Participant demographics from cannabis clinical trials published in 2000–2014 versus 2015–2022
To assess for shifts in cannabis clinical trial participant demographics over time, the above described data was partitioned into works published in 2000–2014 and those published in 2015–2022. Summaries of participant demographic characteristics for each literature analysis subgroup are included in eSupplement Table S4. A total of 12 manuscripts31,32,33,34,35,36,37,38,39,40,41,42 were published in 2000–2014 that met the inclusion criteria of this work. These studies included 187 participants of which most (144, 77.0%) were male. When race was reported, 100.0% of participants were White. Conversely, 29 manuscripts16,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70 were published in 2015–2022 and met the inclusion criteria of this work. These studies included 780 participants of which 429 (65.0%) were male. Race was reported for 338 participants, including While (274, 81.1%), Black (24, 7.1%), Asian (9, 2.7%) Asian, two or more races (12, 3.6%), Native American (2, 0.6%), or "other" (3, 0.9%) participants. In this cohort (2015–2022), ethnicity was reported for 139 participants, with 14 (10.1%) identifying as Hispanic. Minimum and maximum age ranges were similar, when reported, for these works.
Participant demographics from cannabis clinical trials including only healthy participants with prior cannabis exposure
When applying cannabis clinical trial results to people who use cannabis, readers must consider if the clinical trial participants were patients or healthy and if they have prior experience with cannabis. To that end, we also considered cannabis clinical trial participant demographic characteristics (published in 2000-2022) when all “patients” and “no prior cannabis exposure” participants were removed, see eSupplement Table S4. This subgroup, called herein “prior cannabis exposure” included 26 publications16,31,32,33,35,36,37,38,39,40,41,43,44,45,46,48,52,53,54,56,57,58,59,60,64,67 including 715 participants of which 430 (72.3%) were male. Race was reported for 240 of these participants, including White (170, 78.3%), Black (17, 7.8%), Asian (7, 3.2%), two or more races (9, 4.1%), Native American (1, 0.5%), or other (3, 1.4%). Ethnicity was reported for 78 participants and 10 (12.8%) were Hispanic.
Participant demographics from cannabis clinical trials including only healthy participants with prior cannabis exposure published in 2015–2022
Within the above described “prior cannabis exposure” cohort, 10 manuscripts were published between 2000 and 2014. Removing those, a final subgroup was created including “prior cannabis exposure” participants that were published between 2015 and 2022, see eSupplement Table S4. This group included 16 works16,43,44,45,46,48,52,53,54,56,57,58,59,60,64,67 and 545 participants that should be most similar to the demographic characteristics of NSDUH “past-month” cannabis use survey results. Within this group, 297 (69.9%) participants were male. Race was reported for 187 participants including those who identified as White (140, 74.9%), Black (17, 9.1%), Asian (7, 3.7%), two or more races (9, 4.8%), Native American (1, 0.5%), or "other" (3, 1.6%). The distribution of racial groups (when available) included in cannabis clinical trials reporting pharmacokinetics and/or pharmacodynamics models are shown in Fig. 3B. It must be noted that the NSDUH requires respondents to select their race and ethnicity simultaneously whereas clinical trial studies that reported these details treated race and ethnicity as separate, overlapping entities. Therefore, Hispanic ethnicity totals were not included in Fig. 3B as only 3 publications45,48,60 reported the participant’s ethnicity, including 78 total participants and 10 (12.8%) who identified as Hispanic. Participant ages were primarily reported as minimum to maximum age ranges. The range of minimum ages was 15–29 years old, with an average minimum age of 21.2 years old. The range of maximum ages was 25–52 years old, with an average maximum age of 35.7 years old.
Discussion
This is the first study to compare the NSDUH demographics of people reporting “past-month” cannabis use to cannabis clinical trial participants. The main finding of this study is that demographics of those reporting “past-month” cannabis use are quite diverse, with significant prevalence increases between 2002 and 2021 in older Americans, women, and historically underrepresented groups. However, cannabis clinical trial participants continue to be majority White males in their 20s and 30s. Literature published recently (2015–2022) have included more women and racial minorities compared to literature from 2000–2014. However, this chasm between the demographics of people reporting recent cannabis use and clinical trial participants is concerning. It is well known that demographic differences are an important factor in interpersonal variability in the pharmacokinetics and pharmacodynamics of a substance71. Therefore, any pharmacokinetics or pharmacodynamics models generated from these cannabis clinical trials may not be generalizable to the increasingly diverse population of people who use cannabis.
Over the past 18 years, the prevalence of “past-month” cannabis use increased across all age categories except 12–17-year-olds. While decreasing prevalence of “past-month” cannabis use in the pediatric population is encouraging, significant increases in other age groups warrants increased awareness and scientific inquiry. Increases in “past-month” cannabis use prevalence was not evenly distributed across all age groups considered. For example, “past-month” cannabis use prevalence increased 50.9% in 18–25-year-olds from 2002 to 2021 whereas the increase was 224.9% in 26–34 and 148.0% in 35–49-year-olds. Increases were even larger for 50–64-year-olds at 472.4% and use by those aged 65 and older increased an astonishing 2,066.1%. Significant increases in “past-month” cannabis use by older Americans has not received a commiserate increase in research interest and clinical investigation72,73,74. In cannabis clinical trials, age ranges were reported for most participants (94.0%), but detailed age information down to the decade was only reported on some (15.6%) participants. Furthermore, removal of patient participant works reduced the overall age range of participants included in studies. Pharmacokinetics and pharmacodynamics clinical trials are inherently limited by small sample size and stringent inclusion and exclusion criteria. Despite these limitations, the rapid expansion of “past-month” cannabis use by adults aged 50 and older warrants additional clinical investigation.
To understand how cannabis clinical trial participant demographic characteristics have changed over time, data extracted from the literature was divided into several subgroups. These subgroups were: works published in 2000–2014, works published in 2015–2022, works including healthy participants with prior cannabis experience, and works including healthy participants with prior cannabis experience which were published from 2015 to 2022. With respect to publication date, promising improvements in participant demographic characteristics are apparent. Works published in the years 2015–2022 included more women and historically underrepresented racial and ethnic groups than those published in 2000–2014. Including participant eligibility criteria (i.e., healthy with prior cannabis experience) alongside publication years of 2015–2022 boosted the racial and ethnic diversity of participants, but decreased female representation. Furthermore, removal of patients (studies assessing cannabis for therapeutic applications) reduced the age range of included participants.
Cannabis clinical trial participant demographic information was significantly lacking in the works considered here. Participant sex was commonly (87.9%) reported, but race (39.1%) and ethnicity (14.0%) details were deficient. When participant demographic data is missing, the reader is unable to critically assess the translatability of reported results to “real world” cannabis use. Even when available, race and ethnicity data is oversimplified and incomplete. For example, NSDUH crudely aggregates all those identifying as Hispanic together, limiting our ability to consider how ethnicity overlaps with different racial groups in those who report “past-month” cannabis use. However, cannabis clinical trial participant demographics largely failed to capture any ethnicity information. This represents structural discrimination in the research landscape that perpetuates social and health inequities. Overall, there needs to be greater transparency and reporting of participant demographics.
This study had several limitations. Cannabis clinical trial participant data was derived from peer-reviewed literature, which introduces publication bias. That is, this work fails to capture any studies that were completed but not published, for whatever reason. Additionally, cannabis clinical trials often include intentionally stringent participant eligibility and ineligibility criteria. For example, females of reproductive potential may be ineligible due to teratogenicity risk. Additionally, the small sample sizes used in pharmacokinetics and pharmacodynamics studies may result in narrow eligible age ranges, preventing consideration of older adults. This is exemplified by studies on therapeutic potential of cannabis and cannabinoids (i.e., participants were patients) for certain indications which tended to include older adults.
Conclusion
Significant investments have facilitated the wide availability of NSDUH results and datasets to the public through the Substance Abuse and Mental Health Data Archive (https://pdas.samhsa.gov/). Therefore, demographic details on people reporting cannabis use, including “past-month”, “past-year”, or “lifetime” cannabis use, is available. This data and online data exploration tool was chosen to promote its use when designing future cannabis clinical trials. As shown in this work, the demographics of people reporting “past-month” cannabis use has changed over time. These changes across age, sex, and race and ethnicity necessitate annual reconsideration of the demographics of people who use cannabis. However, cannabis clinical trials seeking to generate pharmacokinetics and/or pharmacodynamics models of cannabis or cannabinoids do not include participants whose demographics are representative of those who use cannabis. This disconnect is problematic for those seeking translatable data to inform public policy on cannabis use and cannabis products. Well-crafted clinical trials should consider the demographics described in this work and updated annually through the Substance Abuse and Mental Health Data Archive. Funding agencies should also consider this data when evaluating funding proposals and crafting Requests for Proposals and Notices of Special Interest announcements.
Data availability
All data used in this work is publicly available through the Substance Abuse and Mental Health Data Archive (https://pdas.samhsa.gov/#/).
References
Zamarripa, C. A., Vandrey, R. & Spindle, T. R. Factors that impact the pharmacokinetic and pharmacodynamic effects of cannabis: A review of human laboratory studies. Curr. Addict. Rep. 9, 608–621. https://doi.org/10.1007/s40429-022-00429-4 (2022).
Alves, P., Amaral, C., Teixeira, N. & Correia-da-Silva, G. Cannabis sativa: Much more beyond Δ9-tetrahydrocannabinol. Pharmacol. Res. 157, 104822. https://doi.org/10.1016/j.phrs.2020.104822 (2020).
Schmitz, N. & Richert, L. Pharmacists and the future of cannabis medicine. J. Am. Pharm. Assoc. 60, 207–211. https://doi.org/10.1016/j.japh.2019.11.007 (2020).
Lucas, C. J., Galettis, P. & Schneider, J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br. J. Clin. Pharmacol. 84, 2477–2482. https://doi.org/10.1111/bcp.13710 (2018).
Hasin, D. S. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology 43, 195–212. https://doi.org/10.1038/npp.2017.198 (2018).
Azofeifa, A. et al. National estimates of marijuana use and related indicators—National Survey on Drug Use and Health, United States, 2002–2014. Morb. Mortal. Weekly Rep. (MMWR) Surveill. Summ. 65, 1–28. https://doi.org/10.15585/mmwr.ss6511a1 (2016).
Compton, W. M., Han, B., Jones, C. M., Blanco, C. & Hughes, A. Marijuana use and use disorders in adults in the USA, 2002–2014: Analysis of annual cross-sectional surveys. Lancet Psychiat. 3, 954–964. https://doi.org/10.1016/s2215-0366(16)30208-5 (2016).
Carliner, H. et al. The widening gender gap in marijuana use prevalence in the US during a period of economic change, 2002–2014. Drug Alcohol Depend. 170, 51–58. https://doi.org/10.1016/j.drugalcdep.2016.10.042 (2017).
Cerda, M. et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiat. 77, 165–171. https://doi.org/10.1001/jamapsychiatry.2019.3254 (2020).
Hasin, D. S., Shmulewitz, D. & Sarvet, A. L. Time trends in US cannabis use and cannabis use disorders overall and by sociodemographic subgroups: A narrative review and new findings. Am. J. Drug Alcohol Abuse 45, 623–643. https://doi.org/10.1080/00952990.2019.1569668 (2019).
Waddell, J. T., Gress-Smith, J. L., Hartman, J. D., Doran, N. & Reed, B. Age, sex, and race-varying rates of alcohol use, cannabis use, and alcohol and cannabis co-use in veterans versus non-veterans. Addict. Behav. 134, 107418. https://doi.org/10.1016/j.addbeh.2022.107418 (2022).
McCartney, D., Arkell, T. R., Irwin, C. & McGregor, I. S. Determining the magnitude and duration of acute Δ9-tetrahydrocannabinol (Δ9-THC)-induced driving and cognitive impairment: A systematic and meta-analytic review. Neurosci. Biobehav. Rev. 126, 175–193. https://doi.org/10.1016/j.neubiorev.2021.01.003 (2021).
Cooper, Z. D. & Haney, M. Investigation of sex-dependent effects of cannabis in daily cannabis smokers. Drug Alcohol Depend. 136, 85–91. https://doi.org/10.1016/j.drugalcdep.2013.12.013 (2014).
Fogel, J. S., Kelly, T. H., Westgate, P. M. & Lile, J. A. Sex differences in the subjective effects of oral Δ9-THC in cannabis users. Pharmacol. Biochem. Behav. 152, 44–51. https://doi.org/10.1016/j.pbb.2016.01.007 (2017).
Matheson, J. et al. Sex differences in the acute effects of smoked cannabis: Evidence from a human laboratory study of young adults. Psychopharmacology 237, 305–316. https://doi.org/10.1007/s00213-019-05369-y (2020).
Sholler, D. J., Strickland, J. C., Spindle, T. R., Weerts, E. M. & Vandrey, R. Sex differences in the acute effects of oral and vaporized cannabis among healthy adults. Addict. Biol. 26, e12968. https://doi.org/10.1111/adb.12968 (2021).
Solomon, H. V., Greenstein, A. P. & DeLisi, L. E. Cannabis use in older adults: a perspective. Harv. Rev. Psychiatry 29, 225–233. https://doi.org/10.1097/hrp.0000000000000289 (2021).
Carroll, C. B. et al. Cannabis for dyskinesia in Parkinson disease—A randomized double-blind crossover study. Neurology 63, 1245–1250. https://doi.org/10.1212/01.wnl.0000140288.48796.8e (2004).
Ahmed, A. I. A. et al. Safety and pharmacokinetics of oral delta-9-tetrahydrocannabinol in healthy older subjects: A randomized controlled trial. Eur. Neuropsychopharmacol. 24, 1475–1482. https://doi.org/10.1016/j.euroneuro.2014.06.007 (2014).
Ahmed, A. I. A. et al. Safety, pharmacodynamics, and pharmacokinetics of multiple oral doses of delta-9-tetrahydrocannabinol in older persons with dementia. Psychopharmacology 232, 2587–2595. https://doi.org/10.1007/s00213-015-3889-y (2015).
Benitez, A., Lauzon, S., Nietert, P. J., McRae-Clark, A. & Sherman, B. J. Self-reported cognition and marijuana use in older adults: Results from the national epidemiologic survey on alcohol and related conditions-III. Addict. Behav. 108, 106437. https://doi.org/10.1016/j.addbeh.2020.106437 (2020).
Bahji, A., Stephenson, C., Tyo, R., Hawken, E. R. & Seitz, D. P. Prevalence of cannabis withdrawal symptoms among people with regular or dependent use of cannabinoids: A systematic review and meta-analysis. JAMA Netw. Open 3, e202370. https://doi.org/10.1001/jamanetworkopen.2020.2370 (2020).
Bidwell, L. C., Martin-Willett, R. & Karoly, H. C. Advancing the science on cannabis concentrates and behavioural health. Drug Alcohol. Rev. 40, 900–913. https://doi.org/10.1111/dar.13281 (2021).
Baglot, S. L. et al. Pharmacokinetics and central accumulation of delta-9-tetrahydrocannabinol (THC) and its bioactive metabolites are influenced by route of administration and sex in rats. Sci. Rep. 11, 23990. https://doi.org/10.1038/s41598-021-03242-7 (2021).
National Survey on Drug Use and Health. About the Survey https://nsduhweb.rti.org/respweb/about_nsduh.html (2022).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 12, 1495–1499. https://doi.org/10.1016/j.ypmed.2007.08.012 (2014).
Balduzzi, S., Rucker, G. & Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 22, 153–160. https://doi.org/10.1136/ebmental-2019-300117 (2019).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 21, e1000097. https://doi.org/10.7326/0003-4819-151-4-200908180-00135 (2009).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. (BMJ) https://doi.org/10.1136/bmj.n71 (2021).
Substance Abuse and Mental Health Services Administration. Substance Abuse and Mental Health Data Archive https://pdas.samhsa.gov/#/ (2023).
Huestis, M. A. & Cone, E. J. Relationship of Delta 9-tetrahydrocannabinol concentrations in oral fluid and plasma after controlled administration of smoked cannabis. J. Anal. Toxicol. 28, 394–399. https://doi.org/10.1093/jat/28.6.394 (2004).
Guy, G. & Robson, P. A Phase I, open label, four-way crossover study to compare the pharmacokinetic profiles of a single dose of 20 mg of a cannabis based medicine extract (CBME) administered on 3 different areas of the buccal mucosa and to investigate the pharmacokinetics of CBME per oral in healthy male and female volunteers (GWPK0112). J. Cannabis Ther. 3, 79–120. https://doi.org/10.1300/J175v03n04_01 (2004).
Guy, G. & Robson, P. A phase I, double blind, three-way crossover study to assess the pharmacokinetic profile of cannabis based medicine extract (CBME) administered sublingually in variant cannabinoid ratios in normal healthy male volunteers (GWPK0215). J. Cannabis Ther. 3, 121–152. https://doi.org/10.1300/J175v03n04_02 (2004).
Naef, M., Russmann, S., Petersen-Felix, S. & Brenneisen, R. Development and pharmacokinetic characterization of pulmonal and intravenous delta-9-tetrahydrocannabinol (THC) in humans. J. Pharm. Sci. 93, 1176–1184. https://doi.org/10.1002/jps.20037 (2004).
Nadulski, T. et al. Randomized, double-blind, placebo-controlled study about the effects of cannabidiol (CBD) on the pharmacokinetics of Δ9-tetrahydrocannabinol (THC) after oral application of THC verses standardized cannabis extract. Ther. Drug Monit. 27, 799–810. https://doi.org/10.1097/01.ftd.0000177223.19294.5c (2005).
Strougo, A. et al. Modelling of the concentration-effect relationship of THC on central nervous system parameters and heart rate—Insight into its mechanisms of action and a tool for clinical research and development of cannabinoids. J. Psychopharmacol. 22, 717–726. https://doi.org/10.1177/0269881108089870 (2008).
Cooper, Z. D. & Haney, M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol. Depend. 103, 107–113. https://doi.org/10.1016/j.drugalcdep.2009.01.023 (2009).
Hunault, C. C. et al. Disposition of smoked cannabis with high Δ(9)-tetrahydrocannabinol content: A kinetic model. Toxicol. Appl. Pharmacol. 246, 148–153. https://doi.org/10.1016/j.taap.2010.04.019 (2010).
Brenneisen, R., Meyer, P., Chtioui, H., Saugy, M. & Kamber, M. Plasma and urine profiles of Δ9-tetrahydrocannabinol and its metabolites 11-hydroxy-Δ9-tetrahydrocannabinol and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol after cannabis smoking by male volunteers to estimate recent consumption by athletes. Anal. Bioanal. Chem. 396, 2493–2502. https://doi.org/10.1007/s00216-009-3431-3 (2010).
Schoedel, K. A. et al. A randomized, double-blind, placebo-controlled, crossover study to evaluate the subjective abuse potential and cognitive effects of nabiximols oromucosal spray in subjects with a history of recreational cannabis use. Hum. Psychopharmacol. Clin. Exp. 26, 224–236. https://doi.org/10.1002/hup.1196 (2011).
Karschner, E. L., Darwin, W. D., Goodwin, R. S., Wright, S. & Huestis, M. A. Plasma cannabinoid pharmacokinetics following controlled oral Δ9-tetrahydrocannabinol and oromucosal cannabis extract administration. Clin. Chem. 57, 66–75. https://doi.org/10.1373/clinchem.2010.152439 (2011).
Joerger, M. et al. Single-dose pharmacokinetics and tolerability of oral delta-9-tetrahydrocannabinol in patients with amyotrophic lateral sclerosis. Drug Metab. Lett. 6, 102–108. https://doi.org/10.2174/1872312811206020102 (2012).
Lee, D. et al. Plasma cannabinoid pharmacokinetics after controlled smoking and ad libitum cannabis smoking in chronic frequent users. J. Anal. Toxicol. 39, 580–587. https://doi.org/10.1093/jat/bkv082 (2015).
Heuberger, J. A. A. C. et al. Population pharmacokinetic model of THC integrates oral, intravenous, and pulmonary dosing and characterizes short- and long-term pharmacokinetics. Clin. Pharmacokinet. 54, 209–219. https://doi.org/10.1007/s40262-014-0195-5 (2015).
Vandrey, R. et al. Pharmacokinetic profile of oral cannabis in humans: blood and oral fluid disposition and relation to pharmacodynamic outcomes. J. Anal. Toxicol. 41, 83–99. https://doi.org/10.1093/jat/bkx012 (2017).
Marsot, A. et al. Population pharmacokinetics model of THC used by pulmonary route in occasional cannabis smokers. J. Pharmacol. Toxicol. Methods 85, 49–54. https://doi.org/10.1016/j.vascn.2017.02.003 (2017).
van Amerongen, G. et al. Effects on spasticity and neuropathic pain of an oral formulation of Δ9-tetrahydrocannabinol in patients with progressive Multiple Sclerosis. Clin. Ther. 40, 1467–1482. https://doi.org/10.1016/j.clinthera.2017.01.016 (2018).
Schoedel, K. A. et al. Abuse potential assessment of cannabidiol (CBD) in recreational polydrug users: A randomized, double-blind, controlled trial. Epilepsy Behav. 88, 162–171. https://doi.org/10.1016/j.yebeh.2018.07.027 (2018).
Awasthi, R., An, G., Donovan, M. D. & Ponto, L. L. B. Relating observed psychoactive effects to the plasma concentrations of delta-9-tetrahydrocannabinol and its active metabolite: An effect-compartment modeling approach. J. Pharm. Sci. 107, 745–755. https://doi.org/10.1016/j.xphs.2017.09.009 (2018).
Birnbaum, A. K. et al. Food effect on pharmacokinetics of cannabidiol oral capsules in adult patients with refractory epilepsy. Epilepsia 60, 1586–1592. https://doi.org/10.1111/epi.16093 (2019).
Wolowich, W. R., Greif, R., Kleine-Brueggeney, M., Bernhard, W. & Theiler, L. Minimal physiologically based pharmacokinetic model of intravenously and orally administered delta-9-tetrahydrocannabinol in healthy volunteers. Eur. J. Drug Metab. Pharmacokinet. 44, 691–711. https://doi.org/10.1007/s13318-019-00559-7 (2019).
Brands, B. et al. Acute and residual effects of smoked cannabis: Impact on driving speed and lateral control, heart rate, and self-reported drug effects. Drug Alcohol. Depend. 205, 107641. https://doi.org/10.1016/j.drugalcdep.2019.107641 (2019).
Sempio, C. et al. Population pharmacokinetic modeling of plasma delta 9-tetrahydrocannabinol and an active and inactive metabolite following controlled smoked cannabis administration. Br. J. Clin. Pharmacol. 86, 611–619. https://doi.org/10.1111/bcp.14170 (2020).
Liu, Z. et al. Model-based analysis on systemic availability of co-administered cannabinoids after controlled vaporised administration. Intern. Med. J. 50, 846–853. https://doi.org/10.1111/imj.14415 (2020).
Almog, S. et al. The pharmacokinetics, efficacy, and safety of a novel selective-dose cannabis inhaler in patients with chronic pain: A randomized, double-blinded, placebo-controlled trial. Eur. J. Pain 24, 1505–1516. https://doi.org/10.1002/ejp.1605 (2020).
Alvarez, J. C. et al. Population pharmacokinetic model of blood THC and its metabolites in chronic and occasional cannabis users and relationship with on-site oral fluid testing. Br. J. Clin. Pharmacol. 87, 3139–3149. https://doi.org/10.1111/bcp.14724 (2021).
Spindle, T. R. et al. Pharmacokinetics of cannabis brownies: a controlled examination of Δ9-tetrahydrocannabinol and metabolites in blood and oral fluid of healthy adult males and females. J. Anal. Toxicol. 44, 661–671. https://doi.org/10.1093/jat/bkaa067 (2020).
Schuster, R. M. et al. Urinary 11-nor-9-carboxy-tetrahydrocannabinol elimination in adolescent and young adult cannabis users during one month of sustained and biochemically-verified abstinence. J. Psychopharmacol. 34, 197–210. https://doi.org/10.1177/0269881119872206 (2020).
Spindle, T. R. et al. Pharmacodynamic effects of vaporized and oral cannabidiol (CBD) and vaporized CBD-dominant cannabis in infrequent cannabis users. Drug and Alcohol. Depend. 211, 107937. https://doi.org/10.1016/j.drugalcdep.2020.107937 (2020).
Schlienz, N. J. et al. Pharmacodynamic dose effects of oral cannabis ingestion in healthy adults who infrequently use cannabis. Drug Alcohol. Depend. 211, 107696. https://doi.org/10.1016/j.drugalcdep.2020.107969 (2020).
Hosseini, A., McLachlan, A. J. & Lickliter, J. D. A phase I trial of the safety, tolerability and pharmacokinetics of cannabidiol administered as single-dose oil solution and single and multiple doses of a sublingual wafer in healthy volunteers. Br. J. Clin. Pharmacol. 87, 2070–2077. https://doi.org/10.1111/bcp.14617 (2021).
Crockett, J., Critchley, D., Tayo, B., Berwaerts, J. & Morrison, G. A phase 1, randomized, pharmacokinetic trial of the effect of different meal compositions, whole milk, and alcohol on cannabidiol exposure and safety in healthy subjects. Epilepsia 61, 267–277. https://doi.org/10.1111/epi.16419 (2020).
Dahlgren, M. K., Sagar, K. A., Lambros, A. M., Smith, R. T. & Gruber, S. A. Urinary tetrahydrocannabinol after 4 weeks of a full-spectrum, high-cannabidiol treatment in an open-label clinical trial. JAMA Psychiat. 78, 335–337. https://doi.org/10.1001/jamapsychiatry.2020.3567 (2021).
Sempio, C. et al. Using population pharmacokinetic modeling to estimate exposure to delta 9-tetrahydrocannabinol in an observational study of cannabis smokers in Colorado. Ther. Drug Monit. 43, 536–545. https://doi.org/10.1097/ftd.0000000000000882 (2021).
Peters, E. N. et al. Safety, pharmacokinetics and pharmacodynamics of spectrum yellow oil in healthy participants. J. Anal. Toxicol. 46, 393–407. https://doi.org/10.1093/jat/bkab026 (2022).
Schultz, H. B., Hosseini, A., McLachlan, A. J. & Reuter, S. E. Population pharmacokinetics of oral-based administration of cannabidiol in healthy adults: Implications for drug development. Cannabis Cannabinoid Res. https://doi.org/10.1089/can.2021.0202 (2022).
Sempio, C. et al. Urinary clearance of 11-nor-9-carboxy-Δ9-tetrahydrocannabinol: A detailed pharmacokinetic analysis. Drug Test. Anal. 14, 1368–1376. https://doi.org/10.1002/dta.3259 (2022).
Lorenzl, S. et al. A phase I trial to determine the pharmacokinetics, psychotropic effects, and safety profile of a novel nanoparticle-based cannabinoid spray for oromucosal delivery. Med. Cannabis Cannabinoids. 5, 9–19. https://doi.org/10.1159/000521352 (2022).
Bonomo, Y. et al. Pharmacokinetics, safety, and tolerability of a medicinal cannabis formulation in patients with chronic non-cancer pain on long-term high dose opioid analgesia: A pilot study. Pain Ther. 11, 171–189. https://doi.org/10.1007/s40122-021-00344-y (2022).
Sholler, D. J. et al. Urinary pharmacokinetic profile of cannabidiol (CBD), Δ9-tetrahydrocannabinol (THC) and their metabolites following oral and vaporized CBD and vaporized CBD-dominant cannabis administration. J. Anal. Toxicol. 46, 494–503. https://doi.org/10.1093/jat/bkab059 (2022).
Gross, A. S., Harry, A. C., Clifton, C. S. & Della Pasqua, O. Clinical trial diversity: An opportunity for improved insight into the determinants of variability in drug response. Br. J. Clin. Pharmacol. 88, 2700–2717. https://doi.org/10.1111/bcp.15242 (2022).
Briscoe, J. & Casarett, D. Medical marijuana use in older adults. J. Am. Geriatr. Soc. 66, 859–863. https://doi.org/10.1111/jgs.15346 (2018).
Han, B. J. H. & Palamar, J. J. Trends in cannabis use among older adults in the United States, 2015–2018. JAMA Intern. Med. 180, 609–611. https://doi.org/10.1001/jamainternmed.2019.7517 (2020).
Kaufmann, C. N., Kim, A., Miyoshi, M. & Han, B. H. Patterns of medical cannabis use among older adults from a cannabis dispensary in New York State. Cannabis Cannabinoid Res. 7, 224–230. https://doi.org/10.1089/can.2020.0064 (2022).
Author information
Authors and Affiliations
Contributions
H.B. and M.B. performed the systematic review, extracted data, and wrote the main manuscript text. HB prepared figures 1-4 and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barkholtz, H., Bates, M. Measuring the diversity gap of cannabis clinical trial participants compared to people who report using cannabis. Sci Rep 13, 9787 (2023). https://doi.org/10.1038/s41598-023-36770-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36770-5
- Springer Nature Limited