Abstract
To explore the feasibility of mesangium or membrane anatomy theory in thoracolaparoscopic radical esophagectomy for esophageal cancer, 98 patients with esophageal cancer were enrolled including 45 patients in the mesoesophageal esophagectomy group and 53 patients in the non-mesoesophageal esophagectomy group. Thoracolaparoscopic radical esophagecotmy was technically successful in all patients. Compared the non-mesoesophageal group, the mesoesophageal group had significantly (P < 0.05) shorter surgical duration (211.9 ± 42.0 min vs. 282.0 ± 44.5 min), less blood loss during the procedure (68.9 ± 45.9 ml vs. 167.0 ± 91.4 ml), more harvested lymph nodes (25.9 ± 6.3 vs. 21.8 ± 7.3), shorter hospital stay after surgery (10.5 ± 2.5 d vs. 12.5 ± 4.2 d), shorter fasting time or quicker postoperative feeding time (7.3 ± 1.2 d vs. 9.5 ± 3.9 d), and quicker removal of the thoracic drainage tube after surgery (7.7 ± 2.0 d vs. 9.2 ± 4.1 d). The overall incidence of postoperative complications was 46.7% (21/45) in the mesoesophageal group, which was significantly (P = 0.02) fewer than that (69.8% or 37/53) of the non-mesoesophageal group (P = 0.020). During follow-up 20.6 ± 4.3 or 20.8 ± 3.4 months after esophagectomy, liver metastasis occurred in 1 case and lung metastasis in 1 in the mesoesophageal group, whereas liver metastasis occurred in 2 cases, mediastinal metastasis in 2, and anastomotic recurrence in 1 in the non-mesoesophageal group. The mesoesophageal group had significantly better physical function (81.9 ± 7.3 vs. 78.3 ± 7.6), social function (65.1 ± 7.1 vs. 56.2 ± 18.2), global health status (65.3 ± 10.1 vs. 58.7 ± 12.4), and pain improvement (29.5 ± 9.5 vs. 35.6 ± 10.6). The overall survival rate was 82.2% (37/45) in the mesoesophageal group and 71.7% (38/53) in the non-mesoesophageal group (P = 0.26). The disease-free survival rate was 77.8% (35/45) for the mesoesophageal group and 62.3% (33/53) for the non-mesoesophageal group (P = 0.13). In conclusion:, the mesangium or membrane anatomy theory can be used safely and effectively to guide thoracolaparoscopic radical esophagectomy for esophageal cancer, with advantages of shorter surgical time, less bleeding, more lymph node harvest, fewer complications, and faster postoperative recovery.
Similar content being viewed by others
Introduction
Esophageal cancer is one of the most frequently diagnosed malignancies throughout the world and is the sixth commonest cause of deaths related to cancers1. The incidence of this cancer in the world has risen by approximately 50% over the past twenty years2. Radical esophagectomy remains the optimal approach of treatment for resectable esophageal malignancies. Nonetheless, traditional open surgical procedures have resulted in massive blood loss as well as high complication rates3,4. Because of fast advances in endoscopic technology and wide-spread concept of minimal invasiveness, an increasing number of medical centers have begun to use endoscopic techniques in radical resection of esophageal cancer1,5,6,7,8. Compared with open surgery, the field of vision is clearer, the operation is minimally invasive and more precise, and better surgical outcomes have been achieved with the endoscopic technique. However, radical esophagectomy has to eliminate possible draining lymphatic systems including lymphatic nodes and tubes near the esophagus and at the mediastina, which may possibly increase surgical trauma, duration, and complication rates even with use of the endoscopic technique for esophagectomy. Radical excision of gastrointestinal cancers with complete removal of organ-specific mesentery has been proposed for total dissection of the original malignant lesion and the relevant lymphovascular drainage system9,10,11,12. Complete removal of the mesentery and the lymphovascular drainage system within the mesentery can stop cancer cells from dissemination and metastasis through the draining system to other locations. This concept has been applied in total mesorectal excision (TME) and complete mesocolic excision (CME) and has resulted in improved prognoses9,10,11.
However, this mesangium or membrane theory has not been widely accepted in radical esophagectomy for esophageal cancers. The mesoesophagus is a two-layer membranous structure of connective tissue linking the aorta and the left lateral surface of the esophagus, which has been described in previous studies and confirmed in cadaver and imaging research12,13,14,15,16. Some studies have applied the knowledge of mesoesophagus in total esophagectomy as in TME and CME, which has been named as mesoesophageal esophagectomy12,13,17. In this study, we applied this concept to endoscopic esophagectomy for esophageal cancer with the hypothesis that this approach of mesoesophageal esophagectomy would significantly improve the outcome of esophagectomy.
Materials and methods
Subjects
This retrospective one-center case–control study was approved by the ethics committee of the First Affiliated Hospital of Zhengzhou University, and all patients or their family members had provided written informed consent to participate. All methods were performed in accordance with the relevant guidelines and regulations. Patients with esophageal cancer treated with thoracolaparoscopic radical esophagectomy between July 2017 and July 2018 were enrolled (Fig. 1). The inclusion criteria were patients with esophageal cancer confirmed by preoperative endoscopic biopsy, no distal metastasis on thoracic and abdominal medical imaging, treated with thoracolaparoscopic radical esophagectomy and R0 resection confirmed on postoperative pathology, and cancer stage of Tis-T3NxM0 based on the tumor stage according to the TNM score of esophageal cancer in the eighth edition of AJCC18. The exclusion criteria were patients with extensive or disseminated metastases on intraoperative endoscopic exploration, preoperative neoadjuvant chemotherapy or radiotherapy or incomplete postoperative pathological data. Patients were enrolled and divided into the mesoesophageal esophagectomy group and non-mesoesophageal esophagectomy group. In the mesoesophageal group, radical mesoesophageal esophagectomy was performed according to the membrane theory, with the mesoesophagus and its contents being completely dissected, including the esophagus, lymph nodes, nerves, blood vessels, and adipose tissues as one intact package. The mesoesophagus indicates the periesophageal connective layers as described in studies of minimally invasive esophagectomy and magnetic resonance imaging12,13,14,15,16. In the non-mesoesophageal group, radical esophagectomy was not performed according to the mesoesophageal anatomy.
Surgical approaches
The surgical procedure for both groups were divided into thoracic, abdominal and neck procedures. In the thoracic operation, thoracic esophageal dissociation and lymph node dissection were performed. In the abdominal operation, the stomach was dissociated, and perigastric lymph node dissection and tubular stomach reconstruction were carried out. In the neck procedure, transection of esophagus and reconstruction of digestive tract were performed.
Surgery for the mesoesophageal group
Thoracic operation (Fig. 2)
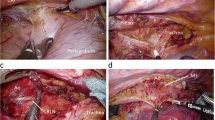
Surgical comparison between two groups. A-C. Throacolaparoscopic radical mesoesophageal esophagectomy. A. During separation between membranes, a fused fascial space was shown to be a white bloodless operation field between the esophagus and esophageal bed. B. The esophagus and lymph nodes were dissociated en bloc according to the membrane separation principle. C. White loose tissue was seen in the fascial space after dissociation of the esophagus, tracheal membrane and esophageal bed. D-F. Throacolaparoscopic non-mesoesophageal radical esophagectomy. D. In dissociation of the posterior mediastinum without adherence to the principle of membrane separation, more blood was present in the operation field. More blood was present when dissociating the esophagus. F. The integrity of esophagus and fascia was destroyed.
The thoracoscopic procedure was performed under general anesthesia with the patient in the prone position using the three trocar technique. After establishment of pneumothorax, the posterior mediastinum was exposed, and the azygos vein was severed. After the esophagus was pressed down, dissection was performed at the obvious intersection of the external esophageal fascia and the thoracic aortic wall to find the fusion space between the esophageal fascia and the thoracic aortic wall. By performing along the aortic wall, the fusion space was expanded to the left until the left mediastinal pleura was reached. The fascia attached to the esophagus was completely separated along the mediastinal pleura, and lymph nodes within the fascia were all dissected. Dissociation was performed downwards to the diaphragmatic hiatus and the cardia and up to the tracheal bifurcation. At the obvious intersection of the extraesophageal fascia and pericardium, the same fusion fascia space was identified to enter the posterior pericardial space. The esophagus was dissociated, and lymph nodes within the esophageal fascia were dissected in the same way. The posterior pericardial space was expanded up to the thoracic inlet and down to the diaphragmatic hiatus to meet the anterior thoracic aortic space. The vagus nerve was disconnected at the right main bronchial membrane, and the esophagus was dissociated along one side of the tracheal membrane to the level of the thoracic inlet. The chest was closed after inserting a thoracic drainage tube.
Abdominal procedure (Fig. 3)
Dissociation of left gastric mesangium in thoracolaparoscopic radical mesoesophageal esophagectomy. A. The left gastric mesangium was lifted and dissociated along the fascial space. B. After separation between membranes, the root of the left gastric vessels was exposed, with the upper left gastric mesangium being kept intact. C. The left gastric vessels were shown after dissociation.
The patient was changed to the supine position, and the five-hole method for laparoscopic surgery was performed. The principle of separation between membranes was followed. The left and posterior gastric mesangium was exposed, and the left gastric blood vessels were disconnected at the root of left gastric mesangium. The lymph nodes were dissected as a whole. The hepatogastric ligament was dissociated to the right diaphragm angle. The diaphragmatic esophageal ligament was disconnected transversely near the diaphragm angle above the cardia, and the left mesentery of the stomach was kept intact before the esophageal hiatus was cut open.
Neck procedure
An oblique incision was made on the left of the neck along the front edge of the sternocleidomastoid muscle, and the esophagus was pulled out and disconnected. A 3 cm incision was made in the middle of the upper abdomen, and the esophagus and stomach were pulled out of the abdominal cavity. A tubular stomach was constructed, and the specimen was removed. The tubular stomach was pulled out from the neck incision along the esophageal bed and anastomosed with the proximal end of the esophagus.
Surgery for non-mesoesophageal group (Fig. 2)
During thoracic operation, the patient took the lateral position, the azygos vein arch was disconnected, and the esophagus was directly dissociated. During the operation, the space of esophageal fascia was not specially searched, the esophagus and surrounding tissues were separated and disconnected, and visible thoracic lymph nodes were cleaned according to the area. After reaching the upper part of the pancreas during abdominal operation, the left mesangium of the stomach was not deliberately dissociated, the stomach was dissociated, and lymph nodes were cleaned in a conventional way. Digestive tract reconstruction was carried out in the neck in the same was as in the mesoesophageal group.
Quality of life assessment
Postoperative quality of life was assessed according to the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire-Core Questionnaire (EORTC QLQ-C30)19 and Esophageal Cancer Module (EORTC QLQ- OES18)20. The QLQ-C30 consists of 5 functional scales (physical, role, cognition, emotional, and social function), a global health status and quality of life scale, 3 symptom scales (pain, fatigue, and nausea/vomiting), 6 single items (dyspnea, appetite loss, insomnia, diarrhea, constipation, and financial difficulties). QLQ-OES18 is comprised of 4 scales (dysphagia, reflux, eating, and pain) and 6 single items (trouble swallowing saliva, choking, taste, dry mouth, cough, and speech problems). The scores ranged from 0 to 100. A high score on the functional scale represents a higher level of functionality, whereas a high score on the symptom scale represents severe symptoms.
Parameters for investigation
Surgical duration, intraoperative bleeding, total postoperative hospital stay, thoracic drainage tube extraction time, postoperative feeding time, number of lymph node dissections, and postoperative complications were recorded. The postoperative complications of the two groups were graded by using the Clavien Dindo complication grading method21. Follow-up was performed three months later for the short-term effect of treatment through clinic visit or telephone contact until June 2021.
Statistical analysis
The statistical analysis was performed with the SPSS software (version 24.0, IBM, Chicago, IL, USA). Measurement data in the normal distribution were presented as a mean ± standard deviation and tested between two groups with the independent t test, and measurement data in the skew distribution were presented as a median and interquartile range and tested with the Rank sum test. Enumeration data were presented as numbers and percentages and tested with the Chi square test or Fisher exact test. Survival analysis was performed with the Kaplan Meier method to plot survival curves, and the Log rank method was applied to test the difference in survival rates between the two groups. The significant statistical P value was set at < 0.05.
Results
Ninety-eight patients with esophageal cancer were enrolled including 45 patients in the mesoesophageal esophagectomy group and 53 patients in the non-mesoesophageal group (Table 1). No significant (P > 0.05) differences were found in the baseline data between two groups.
Thoracolaparoscopic radical esophagectomy was technically successful in all patients with no patients being converted to open thoracotomy or laparotomy. Compared with patients in the non-mesoesophageal group, patients in the mesoesophageal group had significantly (P < 0.05) shorter surgical duration (211.9 ± 42.0 min vs. 282.0 ± 44.5 min), less blood loss during the procedure (68.9 ± 45.9 ml vs. 167.0 ± 91.4 ml), more harvested lymph nodes (25.9 ± 6.3 vs. 21.8 ± 7.3), shorter hospital stay after surgery (10.5 ± 2.5 d vs. 12.5 ± 4.2 d), shorter fasting time or quicker postoperative feeding time (7.3 ± 1.2 d vs. 9.5 ± 3.9 d), and quicker removal of the thoracic drainage tube after surgery (7.7 ± 2.0 d vs. 9.2 ± 4.1 d) (Table 2). No significant (P > 0.05) difference was found in postoperative albumin reduction (8.0 ± 4.1 g/L vs. 8.9 ± 3.7 g/L).
In the mesoesophageal group, anastomotic leakage occurred in 2 cases, massive pleural effusion in 3, and esophagotracheal fistula in 1. In the non-mesoesophageal group, anastomotic leakage occurred in 3 cases, massive pleural effusion in 4, and esophagotracheal fistula in 1. All patients were improved after active drainage or surgical treatment. In the mesoesophageal group, recurrent laryngeal nerve paralysis occurred in 1 case, chylothorax in 1, gastric acid reflux in 4, and atelectasis in 8. In the non-mesoesophageal group, recurrent laryngeal nerve paralysis took place in 3 cases, chylothorax in 2, gastric acid reflux in 4, and atelectasis in 13. All complications were relieved after conservative treatment.
Postoperative pulmonary infection occurred in 1 case in the mesoesophageal group but in 6 cases in the non-mesoesophageal group, but was improved after treatment with antibiotics. Massive intraoperative bleeding occurred in 1 case in the non-mesoesophageal group and was treated with hemostasis and blood transfusion. Clavien-Dindo grade I-II complications occurred in 17 cases in the mesoesophageal group and 30 cases in the non-mesoesophageal group, and Clavien-Dindo grade III or above complications occurred in 4 cases in the mesoesophageal group and 7 cases in the non-mesoesophageal group (Table 3).
The overall incidence of postoperative complications was 46.7% (21 / 45) in the mesoesophageal group, which was significantly (P = 0.02) fewer than that (69.8% or 37 / 53) in the non-mesoesophageal group (P = 0.020).
Follow-up was performed for 20.6 ± 4.3 months in the mesoesophageal group and 20.8 ± 3.4 months in the non-mesoesophageal group. At follow-up, liver metastasis occurred in 1 case and lung metastasis in 1 in the mesoesophageal group. In the non-mesoesophageal group, liver metastasis occurred in 2 cases, mediastinal metastasis in 2, and anastomotic recurrence in 1. During the follow-up, there was no death within 30 days after surgery in both groups.
At 12-month follow-up, one patient died, one patient experienced recurrent esophageal cancer, and 43 patients were finally evaluated with the postoperative quality of life scores using the QLQ-C30 and –OES18 scales in the mesoesophageal esophagectomy group. In the non-mesoesophageal group, two patients experienced recurrence of the esophageal cancer within one year, and 51 patients were entered for the quality of life assessment (Tables 4 and 5).
Compared with the QLQ-C30 data in the non-mesoesophageal group (Table 4), the mesoesophageal group had significantly better physical function (81.9 ± 7.3 vs. 78.3 ± 7.6), social function (65.1 ± 7.1 vs. 56.2 ± 18.2), global health status (65.3 ± 10.1 vs. 58.7 ± 12.4), and pain improvement (29.5 ± 9.5 vs. 35.6 ± 10.6). No significant (P > 0.05) differences were found in the other parameters. Compared with the QLQ-OES18 data in the non-mesoesophageal group (Table 5), the pain in the mesoesophageal group was significantly (P < 0.05) improved (18.3 ± 11.3vs. 25.1 ± 10.8). No significant (P > 0.05) differences were detected in the other parameters.
In the final follow-up of 20.6 ± 4.3 months in the mesoesophageal group and 20.8 ± 3.4 months in the non-mesoesophageal group, the overall survival rate was 82.2% (37/45) in the mesoesophageal group and 71.7% (38/53) in the non-mesoesophageal group, with no significant difference (P = 0.26, Fig. 4). The disease-free survival rate was 77.8% (35/45) for the mesoesophageal group and 62.3% (33/53) for the non-mesoesophageal group (P = 0.13, Fig. 4).
Discussion
This study investigated the feasibility, effects and complications of membrane theory in thoracolaparoscopic radical esophagectomy for esophageal cancer. It was found that the mesoesophageal theory could be used safely and effectively to guide thoracolaparoscopic radical esophagectomy for esophageal cancer, with the advantages of shorter surgical time, less bleeding, more lymph nodes harvested, fewer complications, and faster postoperative recovery.
Compared with traditional open esophagectomy, endoscopic radical esophagectomy has the advantages of less intraoperative bleeding, lower incision infection and lower local recurrence rates1. In order to achieve the ideal surgical effect, the key to successful cancer dissection is to achieve real R0 resection and avoid cancer leakage or residue. Therefore, it is necessary to further optimize the surgical concept and surgical details. The TME theory was proposed in 1986 by Heald et al.10 in total resection of rectal cancer and had resulted in better outcomes because the TME theory focuses on complete removal of the malignant lesion together with the primary lymphatic and vascular draining system in the mesorectum as one intact package, including the cancerous lesion, regional lymph nodes, blood vessels, and adipose tissues within the mesorectum. The CME was proposed by Hohenberger et al. in 2009 to resect the primary cancer and relevant draining lymph nodes and vessels within the mesocolon as one intact package11. Both the TME and CME surgical techniques have greatly reduced local cancer recurrence and improved the prognosis.
Gong et al.22,23,24 had proposed a mesangium or membrane anatomy theory and the fifth metastasis theory of tumor and considered the mesangial and fascial structures around the digestive tract as an "envelope" structure. According to the theory of mesangium, all internal organs have a generalized mesangium and mesangial bed. During embryonic development, part of the mesangium and the serosa of the mesangial bed fuse and degenerate to form a fused fascia space. Radical tumor resection must adhere to the principle of separation between membranes, dissecting and dissociating along the fascia space. The integrity of the medial mesangium of the space should be maintained to avoid cancer leakage while at the same time maintaining the integrity of the mesangial bed from additional injury23. In a word, the tumor lesion together with the surrounding connective tissue, blood vessels, nerves, and lymph nodes within the mesangium should be dissected as a whole so as to reduce the probability of intramesenteric metastasis of cancer. They consequently applied this theory in radical gastrectomy, resulting in good curative effects22,23. In clinical practice, some researchers have unconsciously applied mesoesophageal or en bloc esophagectomy for radical treatment of esophageal cancer12,13,17, which is in line with the mesangium theory.
From the perspective of embryology, esophagus and stomach are organs developed from the foregut15, which may also be used to guide radical esophagectomy. According to the theory of mesangium, the generalized mesangium has the characteristics of common structure, different morphology and widespread existence. Blood vessels and lymph nodes exist only in the mesangium. According to this principle, in radical esophagectomy, it is also necessary to follow the mesangium theory, adhere to separation between membranes, and maintain the integrity of the primary fascia inside the fusion fascia space so as to avoid cancer leakage and reduce bleeding. At the same time, the integrity of the lateral mesangial bed of the gap should be maintained to avoid additional injury23.
In our study, the radical esophagectomy in the mesoesophageal group was performed according to the principle of separation between two membranes so as to maintain the integrity of fascia or serosa on both sides of fascial space, whereas that in the non-mesoesophageal group did not adhere to the principle of membrane separation in the fascia space, with dissection and dissociation through traditional surgical techniques. The fascial space was not deliberately pursued for dissociation between two membranes. In comparison of the outcomes between two groups, the mesoesophageal group was significantly better than the non-mesoesophageal group in terms of intraoperative bleeding, surgical time, numbers of lymph nodes harvested, and total incidences of complications (P < 0.05). In adherence to the principle of separation between membranes during mesoesophageal esophagectomy, a clear fusion fascial space can be clearly demonstrated under the highly-magnified endoscope between the inherent fascia of the esophagus and the esophageal bed, and the white bloodless surgical field can also be displayed under the endoscope. Performance in the abdominal cavity is also based on the principle of separation between membranes. Our previous study has revealed that the left gastric lymph node is a high-risk area for esophageal cancer metastasis25. Clamping the severed blood vessel at the root of the left gastric mesangium is in line with the principle of "en bloc resection". However, traditional radical esophagectomy does not adhere to the principle of membrane separation, which is bound to destroy the integrity of the fascia on both sides of the fusion fascial space, resulting in more bleeding, unclear visual field, damage to the visceral proper fascia, increases of cancer cell leakage, and damage to the parietal fascia (causing additional injury)23,24. No significant differences were found in cancer recurrence or metastasis during follow-up. Even though more cases and longer follow-up are necessary to confirm the outcome, mesoesophageal radical esophagectomy abides by the gastroenterological mesangial theory which adopts the en bloc radical resection. In the en bloc radical resection, the malignant lesion together with the primary lymphatic and vascular draining system in the mesangium, including the cancerous lesion, regional lymph nodes, blood vessels and adipose tissues, is completely removed, resulting in reduction of local cancerous recurrence.
Our study showed that the mesangium theory could be used to guide radical esophagectomy, and adherence to the principle of membrane separation for anatomical dissociation was in line with the principle of "en bloc resection", leading to increased numbers of lymph nodes harvested, reduced bleeding and injury, faster recovery, and better surgical effects.
Some limitations existed in this study, including the retrospective and one-center study nature, a small cohort of patients, Chinese patients enrolled only, no randomization, shorter follow-up, which may all affect the outcome and the generalization. Future prospective, randomized, controlled studies involving a large cohort of patients, multiple centers and longer follow-up are necessary to resolve all these issues for better outcomes.
In conclusion, the mesoesophageal theory can be used safely and effectively to guide thoracolaparoscopic radical esophagectomy for esophageal cancer, with the advantages of shorter surgical time, less bleeding, more lymph node harvest, fewer complications, and faster postoperative recovery. Further studies with a longer follow-up are necessary to confirm these effects.
Data availability
The datasets generated and/or analysed during the current study are not publicly available because these datasets are owned by our hospital and are not allowed to be made publically available but are available from the corresponding author on reasonable request.
References
Guo, W. et al. Combined thoracoscopic-laparoscopic esophagectomy versus open esophagectomy: A meta-analysis of outcomes. Surg. Endosc. 30, 3873–3881 (2016).
Jemal, A. et al. Global cancer statistics. CA Cancer J. Clin. 61, 69–90 (2011).
Birkmeyer, J. D. et al. Hospital volume and surgical mortality in the united states. N. Engl. J. Med. 346, 1128–1137 (2002).
D’Amico, T. A. Improving outcomes after esophagectomy: The importance of preventing postoperative pneumonia. Zhonghua Wei Chang Wai Ke Za Zhi 14, 660–666 (2011).
Abbassi, O., Patel, K. & Jayanthi, N. V. Three-dimensional vs two-dimensional completely minimally invasive 2-stage esophagectomy with intrathoracic hand-sewn anastomosis for esophageal cancer: Comparison of intra-and postoperative outcomes. Surg. Innov. 28, 582–589 (2021).
Bao, T., Zhao, X. L., Li, K. K., Wang, Y. J. & Guo, W. Effect of surgical start time on short- and long-term outcomes after minimally invasive esophagectomy: A propensity-score matching analysis. Dis. Esophagus 34, doaa108 (2021).
Latzko, M., Ahmed, B. & Awad, Z. Minimally invasive ivor-lewis esophagectomy for esophageal cancer after gastric bypass. Ann. Surg. Oncol. 28, 203 (2021).
Nozaki, I. et al. Long-term survival of patients with t1bn0m0 esophageal cancer after thoracoscopic esophagectomy using data from jcog0502: A prospective multicenter trial. Surg. Endosc. https://doi.org/10.1007/s00464-021-08768-5 (2021).
Heald, R. J. Total mesorectal excision is optimal surgery for rectal cancer: A scandinavian consensus. Br. J. Surg. 82, 1297–1299 (1995).
Heald, R. J. & Ryall, R. D. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1, 1479–1482 (1986).
Hohenberger, W., Weber, K., Matzel, K., Papadopoulos, T. & Merkel, S. Standardized surgery for colonic cancer: Complete mesocolic excision and central ligation–technical notes and outcome. Colorectal Dis. 11, 354–364 (2009).
Tachimori, Y. Total mesoesophageal esophagectomy. Chin. Med. J. (Engl.) 127, 574–579 (2014).
Cuesta, M. A. Minimally invasive mesoesophageal resection. J. Thorac. Dis. 11, S728–S734 (2019).
Cuesta, M. A. et al. A new concept of the anatomy of the thoracic oesophagus: The meso-oesophagus. Observational study during thoracoscopic esophagectomy. Surg. Endosc. 29, 2576–2582 (2015).
Hwang, S. E. et al. Mesoesophagus and other fascial structures of the abdominal and lower thoracic esophagus: A histological study using human embryos and fetuses. Anat. Cell Biol. 47, 227–235 (2014).
Weijs, T. J. et al. The peri-esophageal connective tissue layers and related compartments: Visualization by histology and magnetic resonance imaging. J. Anat. 230, 262–271 (2017).
Rizzetto, C. et al. En bloc esophagectomy reduces local recurrence and improves survival compared with transhiatal resection after neoadjuvant therapy for esophageal adenocarcinoma. J. Thorac. Cardiovasc. Surg. 135, 1228–1236 (2008).
Escrig Sos, J., Gomez Quiles, L. & Maiocchi, K. The 8th edition of the ajcc-tnm classification: New contributions to the staging of esophagogastric junction cancer. Cir. Esp. 97, 432–437 (2019).
Aaronson, N. K. et al. The european-organization-for-research-and-treatment-of-cancer qlq-c30—A quality-of-life instrument for use in international clinical-trials in oncology. J. Natl Cancer Inst. 85, 365–376 (1993).
Blazeby, J. M. et al. Clinical and psychometric validation of an eortc questionnaire module, the eortc qlq-oes18, to assess quality of life in patients with oesophageal cancer. Eur. J. Cancer 39, 1384–1394 (2003).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213 (2004).
Gong, J. D2 gastrectomy and complete mesentery excision based on metastasis iiiii and membrane anatomy. Zhonghua Wei Chang Wai Ke Za Zhi 18, 121–122 (2015).
Gong, J. P. The fifth metastasis route of gastric cancer and the third principle of radical operation. Zhonghua Wei Chang Wai Ke Za Zhi 16, 109–110 (2013).
Xie, D. et al. Mesogastrium: A fifth route of metastasis in gastric cancer?. Med. Hypotheses 80, 498–500 (2013).
Deng, X. M. et al. Lymph node metastasis pattern and significance of left gastric artery lymph node dissection in esophagectomy for esophageal cancers. World J. Surg. Oncol. 19, 296 (2021).
Funding
This study was supported by the Key Research, Development, and Promotion Projects of Henan Province in 2020 (202102310117) and Key Scientific Research Projects of Colleges and Universities in Henan Province 20B320029.
Author information
Authors and Affiliations
Contributions
Study concept and design: G.-J.W., B.-L.G.; Acquisition of data: Y.-X.S., T.-Y.Z., R.-X.L., J.-T.W.; Analysis and interpretation of data: G.-J.W., B.-L.G.; Drafting of the manuscript: T.-Y.Z.; Critical revision of the manuscript for important intellectual content: Y.-X.S., and B.-L.G.; Statistical analysis: Y.-X.S. and B.-L.G.; Technical, or material support: G.-J.W.; Study supervision: G.-J.W.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, YX., Zhu, TY., Wang, GJ. et al. Thoracolaparoscopic radical esophagectomy for esophageal cancer based on the mesoesophageal theory. Sci Rep 13, 8760 (2023). https://doi.org/10.1038/s41598-023-35513-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35513-w
- Springer Nature Limited
This article is cited by
-
Short-term efficacy of additional laparoscopic-assisted radical gastrectomy after non-curative endoscopic submucosal dissection for early gastric cancer
Langenbeck's Archives of Surgery (2023)