Abstract
We investigated the relationship between dyslipidemia and drug-induced liver injury (DILI), especially the level of triglyceride to high-density lipoprotein cholesterol ratio (TG/HDL-C) in severe DILI. In this single-centered retrospective study, of 326 patients with DILI, 221 patients were analyzed. Control groups include medication using group and acute hepatitis B group. The relationship between dyslipidemia and DILI was estimated. Demographic and clinical features were analyzed. Dyslipidemia and TG/HDL-C ratios were compared between DILI and control groups, DILI mild group and severe group. The area under the receiver-operating characteristic curve (AUC) was used to evaluate the credibility of the relationship and to find cut-off points. Dyslipidemia is related to DILI when compared with medication using control group (AOR 4.60; 95% CI 2.81–7.54; P < 0.01) and compared with acute hepatitis B group (AOR 2.12; 95% CI 1.37–3.29; P < 0.01). Dyslipidemia is associated with the severity of DILI (AOR 25.78; 95% CI 7.63–87.1; P < 0.01). TG/HDL-C ratio is higher in DILI group than that of medication using control group, also higher in severe DILI group than that of mild DILI group. AUCs for TG/HDL-C ratio to indicate the severity of DILI was 0.89 (P < 0.05), the cut-off point was 2.35. Dyslipidemia and TG/HDL-C ratio were related to DILI occurrence. Severe liver injury in DILI was associated with dyslipidemia and elevated TG/HDL-C ratio.
Similar content being viewed by others
Introduction
Drug-induced liver injury (DILI) is the most common causation of acute liver failure in the West1. In some Asian countries, patients with herb-induced liver injury (HILI) caused by traditional Chinese medicines have been analyzed in some medical reviews2,3. DILI is caused by adverse reactions to a medicine or drug combination. Risk factors for DILI are associated with metabolic, immunological, and genetic factors of the individuals4,5. Individuals who are aged, female, or have chronic liver injuries are more likely to suffer from DILI6. Recent studies found that dyslipidemia is a risk factor for DILI, and the relation between dyslipidemia and DILI has been studied7.
Dyslipidemia is a common, multifactorial disease that is a major determinant of the cardiovascular risk. Dyslipidemia includes high level of triglyceride (TG), cholesterol (Cho) and low-density lipoprotein (LDL-C), and low level of high-density lipoprotein cholesterol (HDL-C). The TG to HDL-C (TG/HDL-C) ratio summarizes some serum lipid levels, which has been confirmed to be a valuable predictor for cardio-metabolic risk, insulin resistance, cardiovascular diseases and the incidence of chronic kidney diseases8,9,10,11. Dyslipidemia and TG/HDL-C ratio has been reported to be associated with NAFLD12,13. Free fatty acid-induced lipotoxicity is an important feature of non-alcoholic fatty hepatitis pathogenesis14. Dyslipidemia has been estimated to be a risk factor for DILI7.
Few studies have been designed to investigate the relationship between dyslipidemia and severity of DILI to date. This study was performed to explore dyslipidemia and the level of TG/HDL-C ratio in DILI in China.
Results
Characteristics of DILI and control group members
326 patients with DILI were assessed and 105 patients were excluded for a variety of reasons (Fig. 1). Demographic and clinical characteristics of 221 DILI patients, 246 medication using controls and 261 acute hepatitis B participants are shown in Table 1. Among DILI patients, 42.08% were males and 57.92% were females. The average age of the DILI group was 50.97. In the control group, 55.69% were males and 44.31% were females, and their average age was 55.15. In the acute hepatitis B group, 78.16% were males and 21.84% were females, with an average age of 43.17.
According to Chinese Society of Hepatology Guidelines, the severity of DILI was defined in 5 levels15. To investigate the severity of DILI, patients were divided into two groups, mild (level 0–2, 148 patients) group and severe (≥ level 3, 73 patients) group. Of the mild group, 37.84% were males and 62.16% were females, with an average age of 50.84. Then in the severe group, 50.68% were males and 49.32% were females, and their average age was 51.23 (Table 2).
Drug classes in the DILI group and control group were listed in Tables 1 and 3. In DILI group, 75 patients (33.94%) used western medicines, 112 patients (50.68%) used Chinese herbal medicines, and 34 patients (15.38%) used a combination of the two. In medication using control group, 176 patients (71.54%) used western medicines, 14 patients (5.69%) used Chinese herbal medicines, and 56 patients (22.76%) used a combination of the two. There is a significant difference between drug classes of DILI and control groups with P < 0.01. In mild DILI group, 46.62% patients used Chinese herbal medicines, 38.51% patients used western medicines, and 14.86% patients used a combination of the two. In severe DILI group, 63.01% patients used Chinese herbal medicines, 23.29% patients used western medicines, and 13.70% patients used a combination of the two (Table 2). Liver injury classes of DILI were also investigated, 86 patients (38.91%) mainly had hepatocellular injury, 104 patients (47.06%) mainly had cholestatic injury, and 31 patients (14.03%) had mixed injuries (Table 3). In DILI group, 177 patients (80.09%) had medication less than 31 days, 34 patients (15.38%) had medication over 31 days but less than 1 year, 10 patients (4.52%) had medication more than 1 year (Table 3). The drug indication for DILI and medication using groups were shown in Table 3, with healthcare drugs, analgesics and antipyretics and antineoplastic drugs being the top three drugs inducing DILI, there is a significant difference between drug indications for DILI and medication using groups with P < 0.01.
Clinical and demographic characteristics associated with DILI
Compared with medication using group, results from the univariate analysis indicated that sex, age, hypertension, heart disease, diabetes, history of malignancy, allergic history, family chronic diseases, dyslipidemia and medication type had significant values less than 0.1 between patients in DILI and control group. Sex, age, hypertension, heart disease, diabetes, history of malignancy, allergic history, family chronic diseases, dyslipidemia and medication type were included in the multivariate analysis. DILI patients were more likely to have dyslipidemia with an adjusted odds ratio (AOR) of 4.6 (95% CI 2.81–7.54; P < 0.01). Patients who had hypertension had an AOR of 0.49 (95% CI 0.27–0.88; P = 0.02) to DILI compared with participants without hypertension. Patients who had malignant diseases had an AOR of 11.39 (95% CI 4.96–26.15; P < 0.01) to DILI compared with participants without malignant diseases. Participants who had family histories of chronic diseases had an AOR of 3.33 (95% CI 1.23–9.04; P = 0.02) to DILI compared with those without family histories of chronic diseases. When compared between participants using different types of drugs, participants using western medicine had lower risk of DILI when compared to participants with Chinese herbal medicine or both (AOR 0.24; 95% CI 1.23–9.04, .18–0.33; P < 0.01). There was no statistic significant association between age, smoking, alcohol abuse, CVD hypersensitivity, diabetes, or allergic history, and DILI. Above data were shown in Table 1.
Compared with acute hepatitis B group, results from the univariate analysis indicated that sex, age, smoking, alcoholic abuse, hypertension, heart disease, allergic history, family chronic diseases and dyslipidemia had significant value less than 0.1 between patients in DILI and acute hepatitis B group. Sex, age, smoking, alcoholic abuse, hypertension, heart disease, allergic history, family chronic diseases and dyslipidemia were included in the multivariate analysis. DILI participants were more likely to have dyslipidemia with an AOR of 2.12 (95% CI 1.37–3.29; P < 0.01) to DILI. DILI participants who were 60 or older had an AOR of 2.96 (95% CI 1.69–5.18; P < 0.01) to DILI compared with participants less than 60. Patients who had hypertension had an AOR of 2.48 (95% CI 1.34–4.61; P < 0.01) to DILI compared with participants without hypertension. Patients with hypersensitivity had an AOR of 3.84 (95% CI 1.98–7.43, P < 0.01) to DILI compared with those without hypersensitivity. Patients with family history of chronic diseases had an AOR of 0.44 (95% CI 0.23–0.84, P = 0.01) to DILI compared with those without family chronic diseases. There was no statistic significant association between smoking, alcoholic abuse, CVD, diabetes or malignant disease and the DILI. Above data were shown in Table 1.
DILI patients with dyslipidemia had an AOR of 25.78 (95% CI 7.63–87.1; P < 0.01) to severe DILI compared with patients with normal plasma lipid levels. DILI patients with malignant diseases had lower risk to severe DILI with an AOR of 0.32 (95% CI 0.1–0.97; P = 0.04). When compared between participants using different type of drugs, participants using western medicine had lower risk of severe DILI when compared to participants with Chinese herbal medicine or both(AOR: 0.65; 95% CI 0.44–0.95; P = 0.03) (Table 2).
Dyslipidemia and TG/HDL-C ratio associated with DILI
Among all patients with DILI in this study, 75.11% had dyslipidemia (Table 1). Levels of Cho, TG, free fatty acid (FFA) and TG/HDL-C ratio were significantly higher in DILI groups than those in medication using control group. Levels of HDL-C were significantly lower in DILI groups than those in medication using control group (Table 4, Fig. 2). Levels of Cho, TG and LDL-C were significantly higher in DILI group than those in acute hepatitis B group. (Table 4, Fig. 2).
Dyslipidemia and TG/HDL-C ratio in DILI and control groups. TG triglyceride, Cho cholesterol, LDL-C low-density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol, FFA free fatty acid, DILI drug induced liver injury. (a) Cho, TG, HDL-C and LDL-C levels in DILI and medication using control groups; (b) FFA level in DILI and medication using control groups; (c) TG/HDL-C ratio in DILI and medication using control groups; (d) Cho, TG, HDL-C and LDL-C levels in DILI and acute hepatitis B groups; (e) FFA level in DILI and acute hepatitis B groups; (f) TG/HDL-C ratio in DILI and acute hepatitis B groups; (g) Cho, TG, HDL-C and LDL-C levels in mild and severe DILI groups; (h) FFA level in mild and severe DILI groups; (i) TG/HDL-C ratio in mild and severe DILI groups.*P ≤ 0.05, **P ≤ 0.01.
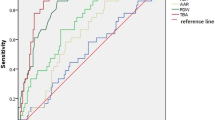
DILI patients were divided into mild and severe groups. 98.63% of patients had dyslipidemia in severe group, and 63.51% in mild group (Table 2). Levels of TG and FFA were significantly increased in severe group than those in mild group, and level of HDL-C was significantly lower in severe group than that in mild group. The TG/HDL-C ratio was significantly increased in severe group than that in mild group (Table 4, Fig. 2). To indicate the severity of DILI, AUCs of severe group for TG and HDL were 0.81 (P < 0.05) and 0.84 (P < 0.05) respectively, and the cut-off values were 1.80 mmol/L and 0.82 mmol/L respectively. AUC of severe group for TG/HDL-C ratio was 0.89 (P < 0.05), the cut-off point was 2.35, the youden index was 0.69 (Table 5, Fig. 3). Among liver injury classes, Cho and LDL-C were statistical significantly higher in cholestatic injury group than those in hepatocellular and mixed liver injury groups. Among medication classes of DILI groups, HDL-C was statistical significantly lower in Chinese herbal medicine group than that in western medicine group, TG/HDL-C ratio was significantly higher in Chinese herbal medicine group than western medicine group (Table 4). In mild DILI group, there is no significant difference of serum lipid levels between different medication classes of DILI. In severe DILI group, TG level in combined herbal and western medicine used group was significantly higher than that in western medicine used group. HDL-C level in herbal medicine used group was significantly lower than that in western medicine used group. Above data were shown in Table 6.
Receiver operating characteristic (ROC) curves of dyslipidemia and TG/HDL-C ratio for diagnosis of severe DILI. TG triglyceride, Cho cholesterol, LDL-C low-density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol, FFA free fatty acid, DILI drug induced liver injury. (a) AUC and cut-off value of Cho for diagnosis of severe DILI; (b) AUC and cut-off value of TG for diagnosis of severe DILI; (c) AUC and cut-off value of HDL-C for diagnosis of severe DILI; (d) AUC and cut-off value of LDL-C for diagnosis of severe DILI; (e) AUC and cut-off value of FFA for diagnosis of severe DILI; (f) AUC and cut-off value of TG/HDL-C ratio for diagnosis of severe DILI. **P ≤ 0.01.
Dyslipidemia and liver function in DILI
The liver function was compared between DILI group and acute hepatitis B group. Gamma-glutamyl transferase (GGT), alkaline phosphatase (AKP), total bilirubin (TBIL) and direct bilirubin (DBIL) were significantly higher in DILI than those in acute hepatitis B group. International normalized ratio (INR) of prothrombin time (PT) (PT-INR) was significantly lower in DILI than that in acute hepatitis B group. The liver function was also compared between different classes of DILI. Among liver injury classes of DILI, levels of ALT and AST were significantly higher in mixed and hepatocellular liver injury group than those in cholestatic liver injury group. GGT in cholestatic liver injury group was higher than that in hepatocellular liver injury group. AKP in cholestatic and mixed liver injury groups were higher than those in hepatocellular liver injury group. Levels of TBIL and DBIL were higher in mixed group than those in hepatocellular liver injury group. Among differnet medication classes of DILI groups, levels of ALT, AST, TBIL, DBIL and PT-INR in herbal medication group were significantly higher than those in western medication group. Above data were shown in Table 7. The relationship between dyslipidemia and liver function were investigated in DILI and acute hepatitis B groups. The result showed that dyslipidemia was related to liver function. TG/HDL-C ratio was related to TBIL in DILI and acute hepatitis B group, with the correlation coefficient 0.648 and 0.634 (P < 0.01), respectively. In different classes of DILI, TG/HDL-C ratio were related to TBIL and DBIL with significant correlation coefficient. Above data were shown in Fig. 4. Liver functions were compared between different liver injury classes of DILI. Alanine aminotransferase (ALT) and aspartate transaminase (AST) were significantly higher in hepatocellular injury participants and mixed injury participants than those in cholestatic injury participants. GGT level was significantly higher in cholestatic liver injury class than that in hepatocellular injury class. AKP, TBIL and DBIL levels were significantly higher in cholestatic liver injury class and mixed injury class than those in hepatocellular injury class. The result showed that TG/HDL-C ratio was related to TBIL in different classes of DILI, in liver injury classes, the correlation coefficients were 0.701, 0.609 and 0.716 (P < 0.01), respectively; in medication classes, the correlation coefficients were 0.796, 0.738 and 0.309 (P < 0.01), respectively (Fig. 4).
The correlation between liver function and serum lipid levels for different classes of DILI and acute hepatitis B groups. TG triglyceride, Cho cholesterol, LDL-C low-density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol, FFA free fatty acid, ALT aminotransferase, AST Aspartate transaminase, GGT gamma-glutamyl transferase, AKP alkaline phosphatase, TBIL total bilirubin, DBIL direct bilirubin, PT-INR International normalized ratio of prothrombin time, DILI drug induced liver injury. (a) the correlation between liver function and serum lipid levels of DILI patients. (b) the correlation between liver function and serum lipid levels of HBV patients. (c) the correlation between liver function and serum lipid levels of DILI patients with herbal medicine use. (d) the correlation between liver function and serum lipid levels of DILI patients with combined herbal and western medicine use. (e) the correlation between liver function and serum lipid levels of DILI patients with western medicine use. (f) the correlation between liver function and serum lipid levels of DILI patients with hepatocellular liver injury. (g) the correlation between liver function and serum lipid levels of DILI patients with cholestetic liver injury. (h) the correlation between liver function and serum lipid levels of DILI patients with mixed liver injury. *P ≤ 0.05, **P ≤ 0.01.
Discussion
Although many drugs are within the range of safe dosage, there is still an increased potential risk for hepatotoxicity. The risk factors of DILI include genetic polymorphisms for xenobiotic-metabolizing enzymes, genetic mitochondrial diseases and pre-existing liver diseases such as NAFLD, alcoholic liver disease, viral hepatitis and liver carcinoma16. A retrospective research in Spanish showed that dyslipidemia is a risk factor for chronic liver injury following acute idiosyncratic DILI17. However, its mechanism is unclear.
In our study, we have found that dyslipidemia is an independent risk factor of DILI (AOR 4.6; 95% CI 2.81–7.54; P < 0.01) compared to participants without dyslipidemia when compared to medication using group, and compared to acute hepatitis B group (AOR 2.12; 95% CI 1.37–3.29; P < 0.01). The mechanisms are supposed to be the following: First, malnutrition such as high fat diet could decrease medication clearance and lead to slowed elimination and high plasma levels of drugs16. Second, the liver and biliary system is an integral part of the reverse cholesterol transport system which prevents accumulation of cholesterol, and liver diseases accompanied with biliary system injury are associated with dyslipidemia18.
The relationship between serum lipid and liver injury is still controversial. Previous study has shown that acetaminophen overdose in adult NMRI mice results in temporal homeostasis in hepatic concentrations of free fatty acids and expression of key genes underlying liver lipid metabolism19. The results from our study revealed that dyslipidemia is an independent risk factor of severe DILI (AOR 25.31; 95% CI 7.62–83.99; P < 0.01), TG/HDL-C ratio can be used as an indicator of severe DILI (AUC 0.89; p < 0.05). TG/HDL-C ratio was related to TBIL level, with correlation coefficient 0.648 and 0.634 in DILI group and acute hepatitis B group (P < 0.01). As the severity of DILI is directly related to the bilirubin level, the relationship between TG/HDL-C ratio and severe DILI is due to the elevated bilirubin level of severe DILI. Previous studies have showed that cholestatic liver injury is related to dyslipidemia through bile acid-FXR expression20,21,22. Researches showed that liver function in patients with obstructive jaundice accompanied by dyslipidemia was more aggravated than that in patients with simple obstructive jaundice23, which is in keeping with our findings. Besides, Cho and LDL-C levels were higher in cholestatic liver injury group than those in hepatocellular and mixed liver injury groups in this study. Cholesterol could synthesize bile acid in liver, liver cholesterol overload could aggravate obstructive cholestasis in mice, and cholestasis resulted in hypercholesterolemia in clinical researches24,25,26.
Our study showed that Chinese herbal medicine is an independent risk factor of DILI and severe DILI. Liver function in herbal medicine group was severe than that in western medicine group in our study, which may result from the increasing prevalence of Herbal medicine as complementary and alternative medicine therapies27. It was observed that more than 18.6% of the adult population in America used herbs for the benefit of their health28,29. The World Health Organization has estimated that 80% of people worldwide rely on herbal medicines for part of their primary health care needs30. In our research, 66.06% (50.68% + 15.38%) of DILI patients used herbal medicines and 28.45% (5.69% + 22.76%) of medication control participants in hospital used herbal medicines. Recent studies have reported a large amount of herbal induced liver injury31. It has been shown that herb-induced liver injury is associated with a higher frequency of hepatocellular injury and cholestatic liver injury in females32,33. Herbal products need to be carefully separated into multiple components and toxicological studies should be conducted to determine their adverse effects. Previous studies have demonstrated that DILI occurs more frequently in females34,35. Our research found that males had a lower risk of DILI compared with females when compared with medication using control group and liver injury control group, which is in keeping with previous findings.
Conclusion
Our study confirmed the relationship between TG/HDL-C ratio and the severity of DILI, and the association between TG/HDL-C and TBIL level in liver injury diseases. This feasible index could be applied to better treatment of DILI in clinical practice. The results also implied that the effects of dyslipidemia should be evaluated after DILI regression. The mechanism of dyslipidemia in DILI needs further investigation.
Limitations
This was a single-centered retrospective study, which relied on the accuracy of medical records. This research only applies to untreated patients with dyslipidemia, but patients with DILI caused by lipid-lowering drugs were not analyzed. There was also limited available data, for instance, the body mass index (BMI) and bile acid in the patient population. The relationships between BMI, bile acid and DILI are unclear. Animal and molecular biology researches need to be investigated.
In our research, hospitalized participants who had long-term medication use were enrolled in the medication using group. However, information of outpatients with long-term medication especially herbal medicine use was incomplete and difficult to obtain. There is a consistent disproportion significant difference of drug indications between DILI cases and controls, even if we have corrected for drug exposures, the results from the comparison with medication control group are possibly due to the underlying medical conditions associated with the selection of the controls. The medication using group size should increase and outpatients’ information should be collected in future studies.
Materials and method
In this single-centered observational study, we retrospectively collected the information of participants from Jan. 1, 2017 to Dec. 31, 2021 from Qilu Hospital of Shandong University. The Independent Institutional Review Board of Qilu Hospital approved the study protocol (No. KYLL-202008-097). All the clinical information was directly from hospital electronic medical records. Since all the data are anonymous, the informed consent waiver statement was approved by the ethics committee of Qilu Hospital. All methods were performed according to the relevant regulations and guidelines.
Sample size was calculated by the corresponding formula using PASS version 11.0 for windows. The ratio of dyslipidemia in control group was 34.4% in our research, and the expected odd ratio was 2.173 in a recent study7 (α = 0.05, β = 0.2). After calculation, the sample size of DILI group and the control group were at least 108.
Study population
A study of all medical registries with International Classification of Disease-10(ICD-10) diagnoses related to DILI was performed from Jan. 2017 to Dec. 2021 in Qilu hospital, and exclusion criteria were as follows:
-
(1)
Incomplete serological test results.
-
(2)
Participants with known pre-existing liver injuries, including viral hepatitis, autoimmune liver disease, and liver cancer according to medical records.
-
(3)
Use of lipid-lowering drugs including fibrates, statin or herbal medicines.
-
(4)
RUCAM score < 6.
-
(5)
Malignant tumor patients with multiorgan metastasis.
-
(6)
Under 18 years of age.
Participants with chronic diseases like rheumatoid arthritis, ankylosing spondylitis, hypertensions or diabetes who had long-term medication use were enrolled in the medication using group. Medication used especially western medicine in control group had liver toxicity in the pharmaceutical directions. Exclusion criteria include less than 18 years old, using fibrates or statins, pre-existing liver diseases, pregnancy, malignant diseases with multiorgan metastases, or organ failure.
We couldn’t judge which medication is responsible of DILI in patients with concomitant medications, while we kept a record of all medications prescribed for each DILI cases. Medications were classified into Chinese herbal medicines, western medicines and both. Medications were also categorized according to drug indications in our research.
Participants with acute hepatitis B were enrolled in liver injury control group. Information of medical registries with International Classification of Disease-10(ICD-10) diagnoses related to acute hepatitis B was collected from Jan. 2017 to Dec. 2021 in Qilu hospital. The diagnosis of acute hepatitis B was defined as positive for HBsAg, the discrete onset of symptoms like fever, headache, malaise, anorexia, nausea, vomiting, diarrhea and abdominal pain, the presence of jaundice or elevated alanine aminotransferase (ALT) level36. The exclusion criteria include: less than 18, using fibrates or statins, pregnancy, malignant diseases with multiorgan metastases and organ failure.
Diagnoses of DILI
Roussel Uclaf Causality Assessment Method (RUCAM) is a scoring system to quantify the association between liver injury and implicated medicines37,38. In our study, all the patients diagnosed with DILI were assessed by RUCAM scale. A final summary score allows categorization of causality as excluded (< 0), unlikely (1–2), possible (3–5), probable (6–8), or highly probable (> 8). The study excluded patients with RUCAM score less than 6.
Diagnosis of dyslipidemia
Patients were considered to be with dyslipidemia if they had Cho > 6.00 mmol/L or 240 mg/dL, TG > 1.7 mmol/L or 200 mg/dL, HDL-C < 0.8 mmol/L or 40 mg/dL, or LDL-C > 3.37 mmol/L or 160 mg/dL.
Severity of DILI
The severity of DILI was identified as different levels according to Chinese Society of Hepatology Guidelines. Clinical and laboratory data were collected to calculate the severity score. DILI severities were classified as mild (level 1) for alkaline phosphatase (ALP) and/or serum ALT elevations in the absence of jaundice, with total bilirubin (TBil) < 2.5 ULN; moderate (level 2) by increased ALT and/or ALP, jaundice with TBil ≥ 2.5 ULN, or coagulopathy, with international normalized ratio (INR) ≥ 1.5; moderately severe (level 3) by increased jaundice with TBil ≥ 5 ULN or INR ≥ 1.5; severe (level 4) by jaundice with TBil ≥ 10 ULN or TBil elevation ≥ 17.1umol/L per day, INR ≥ 1.5 or prothrombin activity (PTA) < 40% and liver or other organ failure; and fatal (level 5) by death from liver disease or the need for liver transplantation surgery15.
Classification of DILI
First, DILI patients were divided into mild group (level 0–2) and severe group (≥ level 3) according to the severity of DILI. Second, DILI patients were divided into hepatocellular injury group (R ≥ 5), mixed liver injury group (2 < R < 5) and cholestatic liver injury group (R ≤ 2) (R is ALT to ALP ratio). Third, DILI patients were divided into Chinese herbal medicine-induced group, western medicine-induced group and combination-induced group according to the drug classes of DILI. Indications of drugs in DILI and medication using group were evaluated.
Demographic and clinical variables
The demographic characteristics were evaluated in this study, including sex, age, smoking history, alcoholic drinking history, hypersensitivity, cardiovascular disease (CVD), hypertension, malignancy, type 2 diabetes, and family chronic diseases. Data about the cause of liver damage, patterns of liver disease, and medications that cause DILI in patients were analyzed.
Biochemical parameters from routine laboratory tests of the patients were also evaluated at the time of admission in hospital, including ALT, AST, GGT, ALP, TBIL, DBIL and PT-INR. Serum lipid levels, including Cho, TG, HDL-C, LDL-C, and FFA were collected.
Statistic analysis
Percentages were used for qualitative parameters. Differences in proportions between groups were evaluated using χ2-test. Mean ± standard deviation (mean ± SD) was used for normally distributed continuous variables. Correlation coefficients were obtained using Pearson’s correlation. Bi-variate logistic regressions were used to investigate the relationship between variables. We used univariate analysis to select variables with P < 0.1 to adjust for potential confounding effects, and multivariate logistic regression analyses were performed, including adjusted odds ratios (AORs) and 95% confidence intervals (CIs). The area under the receiver-operating characteristic curve (AUC) was used to validate the effectiveness of the variable and to define optimal cut-off values. Data were examined graphically and numerically. P value less than 0.05 was considered statistically significant. SPSS version 17.0 (SPSS, Chicago, IL) and GraphPad Prism 8.0 for Windows were used to perform statistical analysis.
Data availability
All data generated or analyzed during this study are available from the corresponding author upon request.
Abbreviations
- DILI:
-
Drug-induced liver injury
- RUCAM:
-
Roussel Uclaf causality assessment method
- TG:
-
Triglyceride
- Cho:
-
Cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- FFA:
-
Free fatty acid
- ALT:
-
Alanine amino transferase
- AST:
-
Aspartate transaminase
- GGT:
-
Gamma-glutamyl transferase
- AKP:
-
Alkaline phosphatase
- TBIL:
-
Total bilirubin
- DBIL:
-
Direct bilirubin
- PT-INR:
-
International normalized ratio of prothrombin time
- AUC:
-
An area under the curve
References
Katarey, D. & Verma, S. Drug-induced liver injury. Clin. Med. 16, s104–s109 (2016).
Kaplowitz, N. Herb-induced liver injury: A global concern. Chin. J. Integr. Med. 24, 643–644 (2018).
Amadi, C. N. & Orisakwe, O. E. Herb-induced liver injuries in developing nations: An update. Chin. J. Integr. Med. 6, 1–10 (2018).
Benesic, A. Drug-induced liver injury (DILI). MMW Fortschr. Med. 161, 57–62 (2019).
Stickel, F. Liver injury from herbal and dietary supplements. Dtsch. Med. Wochenschr. 2015(140), 908–911 (1946).
Chen, M., Suzuki, A., Borlak, J., Andrade, R. J. & Lucena, M. I. Drug-induced liver injury: Interactions between drug properties and host factors. J. Hepatol. 63, 503–514 (2015).
Li, X., Wang, L., Li, D., Niu, J. & Gao, P. Dyslipidemia is a risk factor for the incidence and severity of drug-induced liver injury (DILI): A retrospective population-based study in China. Med. Sci. Monit. 25, 3344–3353 (2019).
McLaughlin, T. et al. Is there a simple way to identify insulin-resistant individuals at increased risk of cardiovascular disease?. Am. J. Cardiol. 96, 399–404 (2005).
Borrayo, G. et al. TG/HDL-C ratio as cardio-metabolic biomarker even in normal weight women. Acta Endocrinol. 14, 261–267 (2018).
NurZatiIwani, A. K. & Jalaludin, M. Y. TG: HDL-C ratio is a good marker to identify children affected by obesity with increased cardiometabolic risk and insulin resistance. Acta Endocrinol. 2019, 8586167 (2019).
Xia, W. et al. Elevated TG/HDL-C and non-HDL-C/HDL-C ratios predict mortality in peritoneal dialysis patients. BMC Nephrol. 21, 324 (2020).
Souza, M. R., Diniz Mde, F., Medeiros-Filho, J. E. & Araújo, M. S. Metabolic syndrome and risk factors for non-alcoholic fatty liver disease. Arq. Gastroenterol. 49, 89–96 (2012).
Wu, K. T. et al. Nonalcoholic fatty liver disease severity is associated with the ratios of total cholesterol and triglycerides to high-density lipoprotein cholesterol. J. Clin. Lipidol. 10, 420-425.e421 (2016).
Bechmann, L. P. et al. Free fatty acids repress small heterodimer partner (SHP) activation and adiponectin counteracts bile acid-induced liver injury in superobese patients with nonalcoholic steatohepatitis. Hepatology 57, 1394–1406 (2013).
Yu, Y. C. et al. CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hep. Intl. 11, 221–241 (2017).
Allard, J., Le Guillou, D., Begriche, K. & Fromenty, B. Drug-induced liver injury in obesity and nonalcoholic fatty liver disease. Adv. Pharmacol. 85, 75–107 (2019).
Medina-Caliz, I. et al. Definition and risk factors for chronicity following acute idiosyncratic drug-induced liver injury. J. Hepatol. 65, 532–542 (2016).
Brufau, G., Groen, A. K. & Kuipers, F. Reverse cholesterol transport revisited: Contribution of biliary versus intestinal cholesterol excretion. Arterioscler. Thromb. Vasc. Biol. 31, 1726–1733 (2011).
Suciu, M. et al. Acetaminophen-induced liver injury: Implications for temporal homeostasis of lipid metabolism and eicosanoid signaling pathway. Chem. Biol. Interact. 242, 335–344 (2015).
Zhan, Y., Xu, T., Chen, T. & Wang, X. Intrahepatic cholestasis of pregnancy and maternal dyslipidemia: A systematic review and meta-analysis. Chem. Biol. Interact. 101, 719–727 (2022).
de Aguiar Vallim, T. Q., Tarling, E. J. & Edwards, P. A. Pleiotropic roles of bile acids in metabolism. Cell Metab. 17, 657–669 (2013).
Fiorucci, S., Mencarelli, A., Palladino, G. & Cipriani, S. Bile-acid-activated receptors: targeting TGR5 and farnesoid-X-receptor in lipid and glucose disorders. Trends Pharmacol. Sci. 30, 570–580 (2009).
Zhao, Y. et al. Clinical laboratory characteristics of patients with obstructive jaundice accompanied by dyslipidemia. Clin. Biochem. 94, 42–47 (2021).
Li, T. & Apte, U. Bile acid metabolism and signaling in cholestasis, inflammation, and cancer. Adv. Pharmacol. 74, 263–302 (2015).
Nuño-Lámbarri, N. et al. Liver cholesterol overload aggravates obstructive cholestasis by inducing oxidative stress and premature death in mice. Adv. Pharmacol. 2016, 9895176 (2016).
Hofbauer, S. & Wiesli, P. C. M. E. Primary and secondary hypercholesterolemia. Praxis 109, 755–762 (2020).
Hsu, M. C. et al. Use of complementary and alternative medicine among adult patients for depression in Taiwan. J. Affect. Disord. 111, 360–365 (2008).
Tindle, H. A., Davis, R. B., Phillips, R. S. & Eisenberg, D. M. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern. Ther. Health Med. 11, 42–49 (2005).
Eisenberg, D. M. et al. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA 280, 1569–1575 (1998).
Duraz, A. Y. & Khan, S. A. Knowledge, attitudes and awareness of community pharmacists towards the use of herbal medicines in muscat region. Oman Med. J. 26, 451–453 (2011).
Byeon, J. H., Kil, J. H., Ahn, Y. C. & Son, C. G. Systematic review of published data on herb induced liver injury. J. Ethnopharmacol. 233, 190–196 (2019).
Chen, Y. & Wang, C. Epidemiology of drug- and herb-induced liver injury assessed for causality using the updated RUCAM in two hospitals from China. J. Ethnopharmacol. 2021, 8894498 (2021).
Lin, N. H., Yang, H. W., Su, Y. J. & Chang, C. W. Herb induced liver injury after using herbal medicine: A systemic review and case-control study. Medicine 98, e14992 (2019).
Larrey, D. Epidemiology and individual susceptibility to adverse drug reactions affecting the liver. Semin. Liver Dis. 22, 145–155 (2002).
de Abajo, F. J., Montero, D., Madurga, M. & Garcia Rodriguez, L. A. Acute and clinically relevant drug-induced liver injury: A population based case-control study. Br. J. Clin. Pharmacol. 58, 71–80 (2004).
Wilkins, T., Sams, R. & Carpenter, M. Hepatitis B: Screening, prevention, diagnosis, and treatment. Am. Fam. Physician 99, 314–323 (2019).
Danan, G. & Benichou, C. Causality assessment of adverse reactions to drugs–I. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J. Clin. Epidemiol. 46, 1323–1330 (1993).
Danan, G. & Teschke, R. RUCAM in drug and herb induced liver injury: The update. Int. J. Mol. Sci. 17, 1–10 (2015).
Author information
Authors and Affiliations
Contributions
Z.L., X.J. contributed to the conception of the study; Z.L., X.Z., R.L., N.Y. performed the data collection, statistical analysis and paper writing; X.J., D.S., M.Y. helped perform the analysis with constructive discussions. All of the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jia, X., Zhang, X., Yan, M. et al. Increased TG to HDL-C ratio is associated with severity of drug-induced liver injury. Sci Rep 13, 6897 (2023). https://doi.org/10.1038/s41598-023-34137-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34137-4
- Springer Nature Limited