Abstract
To develop a predictive model for successful cervical ripening in women that undergo induction of labour by means of a vaginal prostaglandin slow-release delivery system (Propess®). Prospective observational study on 204 women that required induction of labour between February 2019 and May 2020 at “La Mancha Centro” hospital in Alcázar de San Juan, Spain. The main variable studied was effective cervical ripening (Bishop score > 6). Using multivariate analysis and binary logistic regression, we created three initial predictive models (model A: Bishop Score + Ultrasound cervical length + clinical variables (estimated fetal weight, premature rupture of membranes and body mass index)); model B: Ultrasound cervical lenght + clinical variables; and model C: Bishop score + clinical variables) to predict effective cervical ripening. All three predictive models obtained (A, B and C) presented good predictive capabilities, with an area under the ROC curve ≥ 0.76. Predictive model C, composed of the variables: gestational age (OR 1.55, 95% CI 1.18–2.03, p = 0.002), premature rupture of membranes (OR 3.21 95% CI 1.34–7.70, p = 0.09) body mass index (OR 0.93, 95% CI 0.87–0.98, p = 0.012), estimated fetal weight (OR 0.99, 95% CI 0.99–1.00, p = 0.068) and Bishop score (OR 1.49 95% CI 1.18–1.81, p = 0.001), is presented as the model of choice with an area under the ROC curve of 0.76 (95% CI 0.70–0.83, p < 0.001). A predictive model composed of the variables: gestational age, premature rupture of membranes, body mass index, estimated fetal weight and Bishop score upon admission presents good capabilities in predicting successful cervical ripening following administration of prostaglandins. This tool could be useful in making clinical decisions with regard to induction of labour.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Cervical ripening is required in patients who present unfavourable cervical conditions prior to undergoing induction of labour (IoL), with the aim of increasing the probability of vaginal birth and reducing induction time1. This process can be done using pharmacological methods, such as the use of prostaglandins, or mechanical methods, such as insertion of balloon catheters2.
So far, no cervical ripening method has been demonstrated to be clearly superior to another in terms of cervical ripening, labour induction or reducing the risk of caesarean1,2,3. In the meta-analysis published by Chen W et al.2 in 2016, the use of vaginal misoprostol was demonstrated to be the most effective method for achieving vaginal birth in 24 h, in comparison with the use of vaginal dinoprostone or balloon catheters, and was associated with a lower rate of caesareans in IoL. However, this method presented a higher rate of uterine hyperstimulation with changes in fetal heart rate in comparison to other methods.
The use of vaginal dinoprostone (PGE2) is one of the most commonly used methods to achieve cervical ripening4. Many studies have been published in relation to its use, but few have aimed to determine which factors predict successful cervical ripening when dinoprostone is administered by means of the vaginal delivery system Propess® (Ferring Pharmaceutical, Saint-Prex, Switzerland)5,6,7. Additionally, there is high heterogeneity in these studies’ final results, as no specific distinction is made between the cervical ripening process and induction of labour, and different definitions of successful induction of labour are used8,9, making it difficult to compare results and draw definitive conclusions.
Knowing the factors associated with the cervical ripening process will allow us to improve success rates in this procedure and select the right pre-induction method for each patient. The objective of this study is therefore to create a model to predict which patients that undergo induction of labour will present successful cervical ripening, defined as a Bishop score (BS) > 6, through use of the vaginal prostaglandin delivery system (Propess®), independently of the final birth outcome.
Methods
Design and selection of subjects
We conducted a prospective observational study. A total of 223 women took part in the study between February 2019 and May 2020 at “La Mancha Centro” hospital in Alcázar de San Juan, Spain. Before collecting the data, we obtained written informed consent from the patients and approval from the hospital's clinical research ethics committee (CEIC), with protocol number 102-C. This study follows the principles of the Hensilki declaration.
The study included all women with single-gestation pregnancy that required IoL with cervical ripening through use of 10 mg vaginal prostaglandin (Propess®). Single-gestation pregnancies between weeks 34 and 41 with unfavourable cervix were included in this study. Multiple births, non-cephalic presentation, fetal malformations and inductions due to antepartum fetal death were excluded for ethical reasons. Cases in which the medication was removed due to changes in fetal heart rate during the cardiotocography (CTG) or in which there was secondary uterine hyperstimulation were also excluded from the study.
Procedure
Induction of labour in patients with an unfavourable cervix (Bishop ≤ 6) is done following the medical indications described by the Spanish Society of Obstetrics and Gynaecology (SEGO)10, which involves placing the slow-release delivery system (Propess®) in the posterior vaginal fornix. The device contains 10 mg prostaglandin, which is released at a rate of 0.3 mg/h in 24 h. Once the device has been placed, CTG is performed on the patient over a period of 2 h. If, after insertion, fetal heart rate falls into categories II or III (according to the system proposed by the National Institute of Child Health and Human Development—NICHD11) or a uterine tachysystole is observed (defined as more than five contractions in 10 min), the device is removed immediately. If no changes occur, a CTG is performed at 12 h and at 24 h and the device is removed either when the patient achieves favourable cervical ripening (Bishop > 6) and dilation of 3–4 cm with regular uterine contractions; or after 24 h, regardless of Bishop score. After the cervical ripening process, in cases in which it is required, induction of labour continues with intravenous administration of oxytocin in order to regulate uterine dynamics and move forward in the labour process. Artificial rupture of membranes is performed in women with intact membranes and who, after 24 h of cervical ripening, have not started the active phase of labor, if technically possible.
Information sources and study variables
To collect the information, a specific record was created including variables from the digitised hospital medical histories, additional information obtained from personal interviews, and clinical assessments in the form of the Bishop score and cervical length measured by ultrasound. The independent variables were sociodemographic, obstetric and neonatal in nature (Table 1). The main variable result was effective cervical ripening (BS > 6) obtained following application of vaginal dinoprostone, regardless of the final outcome of the birth (spontaneous, instrumental or caesarean). The Bishop score prior to IoL (BS) and the cervical length (CL) measured by ultrasound were collected by the gynaecologist in charge of the delivery room on the day of the IoL. To measure CL, the guidelines proposed by the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG)12 and the Fetal Medicine Foundation (FMF) were followed13.
Statistical analysis
Firstly, descriptive analysis was conducted with absolute and relative frequencies for categorical variables and mean with standard deviation (SD) for the quantitative variables.
We then conducted bivariate analysis with all potential variables associated with cervical ripening (Table 2) and we pre-selected those with a P value < 0.25 (Lemeshow test14), using either the Pearson chi-squared or the Student-Fisher t-test, depending on whether the independent variable was qualitative or quantitative. The next step was to perform multivariate analysis through binary logistic regression using the backward stepwise method in SPSS (Stadistical Package for the Social Sciences) to create three predictive models (Table 3), in which odds ratios (OR) were obtained with respective confidence intervals of 95% (CI).
Model (A) was composed of pre-selected variables plus BS and CL, model (B) was composed of pre-selected variables plus CL, and model (C) was made up of pre-selected variables plus BS.
The reason that we initially created three predictive models was to be able to compare their predictive capability and to identify which variable is a better predictor of response to cervical ripening with dinoprostone: Bishop score, cervical length, or a combination of both.
The predictive capability was determined using the area under the ROC curve, with respective confidence intervals of 95%. The final model was selected based on three criteria: clinical plausibility, predictive capability, and principle of parsimony (least number of variables). All calculations were done using the program SPSS v24.0.
Ethical approval
Ethical approval for this study was granted in February 2019 by the hospital’s clinical research ethics committee (CEIC) in Ciudad Real (Spain), with protocol number 102-C.
Informed consent
Written informed consent was obtained from all women included in the study before collecting the data.
Results
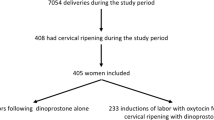
The total number of patients attended to during the period of study was 1061. Of the 223 inductions, 204 (91.47%) met the inclusion criteria, while 19 (8.52%) women were excluded from the study. Following insertion of the PROPESS, 91 (44.6%) patients achieved successful cervical ripening, while 113 (55.4%) presented a Bishop score < 6. The patient selection process is shown in Fig. 1.
Table 1 contains all of the obstetric and socioeconomic variables analysed. The main reason for induction was post-term pregnancy (67, 32.8%) followed by premature rupture of membranes (PROM) (39, 19.1%) and diabetes (15, 7.4%). The mean Bishop score (BS) was 2.78 (SD = 1.37) and the mean cervical length (CL) measured by ultrasound prior to IoL was 24.48 mm (SD = 9.14).
Next, the relationship between effective cervical ripening and the independent variables was studied by means of bivariate analysis, observing statistical relationships with gestational age (p = 0.037), body mass index (BMI) (p = 0.001), fetal sex (p = 0.028), CL measured by ultrasound prior to IoL (p < 0.001), BS upon admission (p = 0.001), PROM (p = 0.001) and time with Propess® (p < 0.001). Table 2 shows the bivariate analysis.
Finally, the multivariate analysis was conducted, obtaining three initial predictive models (Table 3) composed of the following variables: gestational age, premature rupture of membranes (PROM), body mass index (BMI), Estimated fetal weight (EFW), Bishop score (BS) upon admission and cervical lenght (CL) measured by ultrasound.
Model A presented an area under the ROC curve of 0.77 (95% CI 0.71–0.84, p < 0.001). Model B presented a ROC-AUC of 0.76 (95% CI 0.69–0.82, p < 0.001). Model C also presented a ROC-AUC of 0.76 (95% CI 0.70–0.83, p < 0.001). All three models presented good predictive capabilities, with an area under the ROC curve ≥ 0.76. Figure 2 shows the ROC curves for each model and compares them.
Predictive model C was chosen based on the criteria of clinical plausibility, predictive capability, and parsimony. It was composed of the variables: gestational age (odds ratio [OR]1.55, 95% confidence interval [CI] 1.18–2.03, p = 0.002), premature rupture of membranes (PROM) (OR 3.21 95% CI 1.34–7.70, p = 0.09) body mass index (BMI) (OR 0.93, 95% CI 0.87–0.98, p = 0.012), estimated fetal weight (EFW) (OR 0.99, 95% CI 0.99–1.00, p = 0.068) and BS (OR 1.49 95% CI 1.18–1.81, p = 0.001).
Discussion
The variables associated with successful cervical ripening (Bishop score > 6) were: gestational age, PROM and Bishop score upon admission. These results coincide with those reported in the literature in relation to the labour induction process overall15. Obesity and estimated fetal weight (EFW), factors widely known to be predictors of failure in IoL8,16, were also risk factors for failure in cervical ripening. In contrast, estimated fetal weight (EFW) is not reported to be a predictor of cervical ripening failure in studies conducted by Daykan6 and Hiersch5.
We did not find any association between successful cervical ripening and maternal age, parity, reason for induction, number of hours between rupture of membranes and placement of vaginal dinoprostone, or neonatal factors.
We only identified two studies in the literature that present models that predict success in the cervical ripening process with vaginal dinoprostone slow-release devices. Hiersch et al.5 presented an initial predictive model composed of parity, cervical dilation at admission and gestational age, with a ROC-AUC of 0.79 (95% CI 0.74–0.84) and a second, more complex, model composed of maternal age, BMI, parity, cervical dilation, effacement, indication for induction, gestational age and neonatal weight, with a ROC-AUC of 0.80 (95% CI 0.75–0.85). Melamed et al.7 identified maternal age > 30 years, nulliparity, BMI ≥ 25, cervical dilation < 1 cm, effacement ≤ 50% and gestational age > 37 weeks as predictors of failure of cervical ripening, and created a logistic regression model that can predict ≈50% of all cases of failed ripening (R2 = O.47).
However, we agree with the conclusions of Melamed et al.7 and must be cautious when interpreting results reported in the literature. Most studies analyse successful induction of labour, defined as vaginal birth within 24 h8,9,17, as the final result, without distinguishing induction from the prior cervical ripening process, so it is not possible to correctly evaluate cervical response to the action of vaginal dinoprostone without this result being affected by additional intrapartum factors.
With regard to the cervical ripening process, we must clarify that there is no universally accepted threshold score to define a favourable or unfavourable cervix that tells us how to begin an induction. High Bishop scores have traditionally been associated with higher vaginal birth success rates18,19. However, there are studies that question the reliability of Bishop scores in predicting the final birth outcome20. In our study, we considered the cervical ripening process to be successful after obtaining a BS > 6 with administration of vaginal dinoprostone, basing ourselves on the results obtained in the majority of randomised studies and in clinical guidelines for induction of labour21,22.
As for the selection of the most adequate predictive model, many studies have compared the predictive capability of cervical length (CL) measured by ultrasound versus Bishop score on induction of labour outcomes, with conflicting results23,24,25,26. A systematic review conducted by Cochrane in 201527 did not find significant differences between both methods (CL vs BS) in terms of rates of vaginal births, caesareans and admission into NICU, and concluded that there is not enough evidence to recommend the use of CL over the standard digital examination in assessing cervical ripening.
As well as cervical length (CL) measured by ultrasound, fetal fibronectin has also been studied in assessing cervical ripening, but it has not been found to be superior to the Bishop score15. Considering the evidence from the published data and the ease of reproducing it, model C, in which the only added variable was the Bishop score, was our chosen model.
The main limitations of this study are related to the sample size, which is relatively small in comparison to other studies5,8. Also, our predictive model is created based on the sociodemographic and obstetric characteristics of a Caucasian/Hispanic population, so it must be validated externally in another type of population before being used.
Additionally, this study only analyses the obstetric and sociodemographic characteristics that have traditionally been associated with success in the labour induction process15,28. However, these data must be interpreted with caution, as there is still a certain lack of understanding of the physiological phenomena involved in the onset of labour and cervical ripening, and there is wide biological variation among mothers in the normal labour process29.
As far as strong points, we can mention its prospective observational design, making the collection of variables more exhaustive and complete. What's more, all patients included in the study are treated based on a homogeneous labour indication protocol with clear indications on the end of the same, reducing possible biases related to its use.
Conclusion
In conclusion, successful cervical ripening through the administration of the vaginal prostaglandin slow-release delivery system (Propess®) can be predicted from specific variables: gestational age, BMI, PROM, EFW and BS upon admission, through the use of this predictive model (C). Including this predictive model in hospital labor induction protocols could help in decision-making regarding the indication of this procedure by using the variables that best predict the success of cervical ripening with this induction method.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Levine LD. Cervical ripening: Why we do what we do. Semin Perinatol. 44(2), 151216. https://doi.org/10.1016/j.semperi.2019.151216. (2020).
Chen, W. et al. A systematic review and network meta-analysis comparing the use of Foley catheters, misoprostol, and dinoprostone for cervical ripening in the induction of labour. BJOG. 123(3):346–354. https://doi.org/10.1111/1471-0528.13456. (2016).
Zhu, L. et al. Intracervical Foley catheter balloon versus dinoprostone insert for induction cervical ripening: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 97(48), e13251. https://doi.org/10.1097/MD.0000000000013251. (2018).
Shirley M. Dinoprostone Vaginal Insert: A Review in Cervical Ripening. Drugs. 78(15), 1615–1624. https://doi.org/10.1007/s40265-018-0995-2. (2018).
Hiersch, L. et al. Can we predict successful cervical ripening with prostaglandin E2 vaginal inserts? Arch Gynecol Obstet. 295(2):343–349. https://doi.org/10.1007/s00404-016-4260-1. (2017).
Daykan Y, Biron-Shental T, Navve D, Miller N, Bustan M, Sukenik-Halevy R. Prediction of the efficacy of dinoprostone slow release vaginal insert (Propess) for cervical ripening: A prospective cohort study. J Obstet Gynaecol Res. 44(9), 1739–1746. https://doi.org/10.1111/jog.13715. (2018).
Melamed, N. et al. Failure of cervical ripening with prostaglandin-E2 can it be predicted? J Matern Fetal Neonatal Med. 23(6), 536–540. https://doi.org/10.3109/14767050903197076. (2010).
Pevzner L, Rayburn WF, Rumney P, Wing DA. Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol. 114(2 Pt 1), 261–267. https://doi.org/10.1097/AOG.0b013e3181ad9377. (2009).
Rouzi AA, Alsibiani S, Mansouri N, Alsinani N, Darhouse K. Randomized clinical trial between hourly titrated oral misoprostol and vaginal dinoprostone for induction of labor. Am J Obstet Gynecol. 210(1), 56.e1–6. https://doi.org/10.1016/j.ajog.2013.08.033. (2014).
Sociedad Española de Ginecología y Obstetricia. Inducción de parto. GAP SEGO. 2013 Jun; 1–23.
Parer JT, Ikeda T, King TL. The 2008 National Institute of Child Health and Human Development report on fetal heart rate monitoring. Obstet Gynecol. 114(1):136–138. doi: https://doi.org/10.1097/AOG.0b013e3181ab475f. (2009).
Kagan KO, Sonek J. How to measure cervical length. Ultrasound Obstet Gynecol. 45(3), 358–362. https://doi.org/10.1002/uog.14742. (2015).
Fetal Medicine Foundation. Cervical assessment. www.fetalmedicine.org. Analizable at https://fetalmedicine.org/education/cervical-assessment
Hosmer, D. W., Lemeshow, S. & Sturdivant, R. X. 2013 Applied Logistic Regression. 3rd Edn, Hoboken. (Wiley, Newyork).
Crane, JM. Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol. 49(3), 573–584. https://doi.org/10.1097/00003081-200609000-00017. (2006).
Ennen CS, Bofill JA, Magann EF, Bass JD, Chauhan SP, Morrison JC. Risk factors for cesarean delivery in preterm, term and post-term patients undergoing induction of labor with an unfavorable cervix. Gynecol Obstet Invest. 67(2), 113–117. https://doi.org/10.1159/000166307. (2009).
Hou L, Zhu Y, Ma X, Li J, Zhang W. Clinical parameters for prediction of successful labor induction after application of intravaginal dinoprostone in nulliparous Chinese women. Med Sci Monit. 18(8), CR518–522. https://doi.org/10.12659/msm.883273. (2012).
BISHOP EH. PELVIC SCORING FOR ELECTIVE INDUCTION. Obstet Gynecol. 24, 266–268. (1964).
Teixeira C, Lunet N, Rodrigues T, Barros H. The Bishop Score as a determinant of labour induction success: a systematic review and meta-analysis. Arch Gynecol Obstet. 286(3), 739–753. https://doi.org/10.1007/s00404-012-2341-3. (2012).
Kolkman DG, Verhoeven CJ, Brinkhorst SJ, van der Post JA, Pajkrt E, Opmeer BC, Mol BW. The Bishop score as a predictor of labor induction success: a systematic review. Am J Perinatol. 30(8):625–630. https://doi.org/10.1055/s-0032-1331024. (2013).
Intrapartum fetal heart rate monitoring: nomenclature, interpretation and general management principles. ACOG practice bulletin No 106. American College of Obstetricians and Gynecologists Obstet Gynecol 114, 192–202. (2009).
Leduc, D., Biringer, A., Lee, L., Dy, J. CLINICAL PRACTICE OBSTETRICS COMMITTEE; SPECIAL CONTRIBUTORS. Induction of labour. J Obstet Gynaecol Can. 35(9), 840–857. https://doi.org/10.1016/S1701-2163(15)30842-2. (2013).
Verhoeven CJ, Opmeer BC, Oei SG, Latour V, van der Post JA, Mol BW. Transvaginal sonographic assessment of cervical length and wedging for predicting outcome of labor induction at term: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 42(5), 500–508. https://doi.org/10.1002/uog.12467. (2013).
Gabriel R, Darnaud T, Chalot F, Gonzalez N, Leymarie F, Quereux C. Transvaginal sonography of the uterine cervix prior to labor induction. Ultrasound Obstet Gynecol. 19(3), 254–257. https://doi.org/10.1046/j.1469-0705.2002.00643.x. (2002).
Hatfield AS, Sanchez-Ramos L, Kaunitz AM. Sonographic cervical assessment to predict the success of labor induction: a systematic review with metaanalysis. Am J Obstet Gynecol. 197(2), 186–192. https://doi.org/10.1016/j.ajog.2007.04.050. (2007).
Ben-Harush Y, Kessous R, Weintraub AY, Aricha-Tamir B, Steiner N, Spiegel E, Hershkovitz R. The use of sonographic cervical length assessment for the prediction of time from induction to delivery. J Matern Fetal Neonatal Med. 29(14), 2332–2336. https://doi.org/10.3109/14767058.2015.1085018. (2016).
Ezebialu IU, Eke AC, Eleje GU, Nwachukwu CE. Methods for assessing pre-induction cervical ripening. Cochrane Database Syst Rev. 12(6), CD010762. https://doi.org/10.1002/14651858.CD010762.pub2. (2015).
Gibson KS, Waters TP. Measures of success: Prediction of successful labor induction. Semin Perinatol. 39(6), 475–482. https://doi.org/10.1053/j.semperi.2015.07.012. (2015).
Yount SM, Lassiter N. The pharmacology of prostaglandins for induction of labor. J Midwifery Womens Health. 58(2), 133–144 quiz 238–9. https://doi.org/10.1111/jmwh.12022. (2013).
Funding
This study has not required financial support.
Author information
Authors and Affiliations
Contributions
Validation, R.H.P. and V.R.-Á.; formal analysis, A.H.-M.; investigation, N.L.-J.; resources, A.P.-P. and M.M.-C.; writing—original draft preparation, N.L.-J. and A.H.-M.; writing—review and editing, A.P.-P. and M.M.-C.; visualization, M.M.-A.; supervision, A.P.-P. and M.M.-C.; project administration, M.M.-A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López Jiménez, N., García Sánchez, F., Pailos, R.H. et al. Prediction of an effective cervical ripenning in the induction of labour using vaginal dinoprostone. Sci Rep 13, 6855 (2023). https://doi.org/10.1038/s41598-023-33974-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33974-7
- Springer Nature Limited