Abstract
T-cell large granular lymphocyte leukemia (T-LGL) is often accompanied by pure red cell aplasia (PRCA). A high depth of next generation sequencing (NGS) was used for detection of the mutational profiles in T-LGL alone (n = 25) and T-LGL combined with PRCA (n = 16). Beside STAT3 mutation (41.5%), the frequently mutated genes included KMT2D (17.1%), TERT (12.2%), SUZ12 (9.8%), BCOR (7.3%), DNMT3A (7.3%), and RUNX1 (7.3%). Mutations of the TERT promoter showed a good response to treatment. 3 of 41 (7.3%) T-LGL patients with diverse gene mutations were revealed as T-LGL combined with myelodysplastic syndrome (MDS) after review of bone marrow slide. T-LGL combined with PRCA showed unique features (low VAF level of STAT3 mutation, low lymphocyte count, old age). Low ANC was detected in a STAT3 mutant with a low level of VAF, suggesting that even the low mutational burden of STAT3 is sufficient for reduction of ANC. In retrospective analysis of 591 patients without T-LGL, one MDS patient with STAT3 mutation was revealed to have subclinical T-LGL. T-LGL combined with PRCA may be classified as unique subtype of T-LGL. High depth NGS can enable sensitive detection of concomitant MDS in T-LGL. Mutation of the TERT promoter may indicate good response to treatment of T-LGL, thus, its addition to an NGS panel may be recommended.
Similar content being viewed by others
Introduction
T-cell large granular lymphocyte leukemia (T-LGL) is a rare mature neoplasm of T cells induced by clonal expansion of large granular T lymphocytes, usually presenting with neutropenia1. Autoimmune diseases are often associated with T-LGL in Western countries, while pure red cell aplasia (PRCA) is more often reported in Asian countries2,3.
PRCA is characterized by anemia and severe erythroid hypoplasia in bone marrow (BM)4. Development of PRCA occurs along with various underlying diseases such as thymoma, T-LGL, and autoimmune diseases. It is also a bone marrow failure syndrome (BMFS), defined by failure to produce adequate hematopoietic cells in BM, along with aplastic anemia and myelodysplastic syndrome (MDS). BMFS is characterized by immune attack on stem cells via a T-cell mediated immune mechanism and expansion of T cells in BM has been detected5,6. It has not yet been determined whether expansion of T cells is simply a response to immune attack or clonal selection6.
The discovery of somatic mutations of STAT3 has led to a more optimistic outlook regarding the genetic basis of T-LGL pathogenesis7. Activation of STAT3 induced by somatic mutation is thought to facilitate proliferation of T cells through enhanced transcription of anti-apoptotic proteins and downregulation of TP538,9. Although specificity of STAT3 mutations for T-LGL has been reported10, it has also been reported in other conditions showing T cell expansion including PRCA, aplastic anemia, MDS, and other autoimmune disorders11,12. Detection of STAT5B mutations has been reported in 2% of cases of T-LGL, particularly in association with CD4 + T-LGL13,14. Despite frequent detection of STAT3 and STAT5B mutations in T-LGL, their clinical specificity for diagnosis of T-LGL has not been elucidated.
Although two whole-exome sequencing studies have reported on somatic mutation of genes other than STAT3 in T-LGL15,16, the two studies reported significantly different mutational spectrums. Because mutation of clonal hematopoiesis-related genes including TET2, DNMT3A, and BCOR often occurs in BMFS such as PRCA and aplastic anemia17,18 and a subset of T-LGL occurs concomitantly with BMFS6,12,19,20, the mutational patterns of T-LGL may differ according to the concomitant disorders. The significant variation in frequency of STAT3 mutation in PRCA reported in the literature, ranging from 0 to 63%, appears to depend on concomitant T-LGL21,22.
In this study, high depth of next generation sequencing (NGS) of 84 candidate genes including all genes detected in PRCA or aplastic anemia7,17,18,23,24,25 was performed in order to examine the mutational patterns in T-LGL with or without PRCA. Conduct of the study demonstrated the difference in mutational patterns according to the concomitant PRCA, STAT3 mutation, or treatment response and the association of mutational extent of STAT3 with clinical features. We also examined the frequency of STAT3 and STAT5B mutation in hematologic diseases without T-LGL.
Results
Patient characteristics
The median age was higher for patients with T-LGL combined with PRCA (T-LGL + PRCA) compared to those with T-LGL alone (Table 1). Significantly lower levels of hemoglobin and absolute reticulocyte count were detected in patients with T-LGL + PRCA compared to those with T-LGL. In addition, a higher absolute lymphocyte count (ALC) was detected in patients with T-LGL compared to those with T-LGL + PRCA, while a lower absolute neutrophil count (ANC) was detected in patients with T-LGL. There was no difference in platelet count. T-LGL + PRCA showed significantly higher RBC transfusion dependency compared to T-LGL. A higher percentage of patients with T-LGL had a history of infection compared to those with T-LGL + PRCA, but without statistical significance.
Mutational landscape in PRCA, T-LGL and T-LGL + PRCA
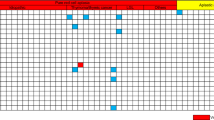
No mutation was detected in patients with PRCA (n = 3) (Fig. 1). Of 41 patients with T-LGL or T-LGL + PRCA, STAT3 mutation was detected in 17 patients (41.5%), nine (36.0%) of 25 patients with T-LGL, and eight (50.0%) of 16 patients with T-LGL + PRCA (Table 1 and Fig. 1). When aligning with the level of STAT3 VAF, a low level of VAF (< 10.0%) was detected in only two patients with T-LGL (22.2%, 2/9) compared to those with T-LGL + PRCA (87.5%, 7/8, P = 0.015, Fig. 1). STAT5B mutations were detected in two patients with STAT3 wild type.
Oncoplot of targeted gene mutations in pure red cell aplasia (PRCA, n = 3), T-cell large granular lymphocyte leukemia (T-LGL, n = 25) and T-LGL combined with PRCA (T-LGL + PRCA, n = 16). Among 84 genes tested, 28 genes in which one or more potential somatic mutations were detected were shown. The genes that were not detected any mutation were removed and are shown in Supplementary Table 5. In STAT3 mutation, variant allele fraction (VAF) percentage was shown in numbers and arranged in order of VAF (%). In some other mutations, the VAF was shown in numbers. Bottom annotations represent clinical parameters at diagnosis and treatment responses. Lower than 10 g/dL of hemoglobin was marked as “Low” and if it was higher than 10 g/dL, marked as “Normal”. Absolute neutrophil count (ANC) cut-off value was 1.8 × 109/L. Conventional cytogenetic results showed a normal karyotype in 42 patients, except for two patients (Y chromosome loss, 26.1% in patient number 9 and 20.0% in patient number 17). Treatment response definitions are described in the “Methods” section.
Mutations of diverse genes were detected in three patients (patient numbers 15, 36, 44) with VAF levels of 2~3% (Supplementary Table 2). Following review of BM slides, the three patients were additionally diagnosed with MDS combined with T-LGL (Supplementary Table 3). The three patients showed no abnormal cytogenetic results.
Excluding the three patients described above with a concomitant MDS clone, 65 mutations were detected in 28 genes (33.3%) of all 84 targeted genes in 32 patients with T-LGL or T-LGL + PRCA (Fig. 1 and Supplementary Table 4) and no mutation was detected in 56 genes (Supplementary Table 5). After excluding STAT3 mutations, the genes showing frequent mutation included KMT2D (17.1%), TERT (12.2%), SUZ12 (9.8%), BCOR (7.3%), DNMT3A (7.3%), and RUNX1 (7.3%). TERT mutations were detected in two STAT3 mutant patients (c.-124C > T in 2) and in three STAT3 wild type patients (c.-124C > T, c.-146C > T and c.81C > A). Among STAT3 mutant patients, the levels of VAF detected in TERT were similar to those detected in STAT3 in two patients with TERT promoter (patient numbers 4, 9).
Different mutational patterns were observed between STAT3 mutant and wild type. Mutations of SUZ12 (9.8%) and TNFAIP3 (4.9%) were only detected in STAT3 mutant, while mutations of DNMT3A (7.3%) and IDH1 (4.9%) were only detected in STAT3 wild type after excluding three patients with a concomitant MDS clone. TNFAIP3 mutations (nonsense mutation L303* in patient number 4, frameshift R141A*75 in patient number 7) showed comparable or a lower level of VAF than STAT3. NF1 and KRAS mutations were detected in both STAT3 mutant with the same frequencies (2.4%). TP53 mutation (patient number 17) showed comparable level of VAF to STAT3.
Changes of CBC parameters in terms of STAT3 mutations
A low level of hemoglobin was detected in STAT3 mutant patients (n = 17) compared with STAT3 wild type (n = 27) in all patients (n = 44), however statistical significance was not reached (Fig. 2a). When divided into subgroups, in T-LGL alone (n = 25), significantly lower levels of hemoglobin were detected for STAT3 mutant compared with those of STAT3 wild type. Significantly lower levels of ANC were detected in STAT3 mutant compared with STAT3 wild type in all patients (Fig. 2b). In the T-LGL + PRCA (n = 16), significantly low levels of ANC were detected in STAT3 mutant patients. No statistical difference in ALC was observed between STAT3 mutant patients and wild type patients across all three groups (Fig. 2c).
Changes of CBC parameters in terms of STAT3 mutation. (a) The hemoglobin level, (b) absolute neutrophil count (ANC) and (c) absolute lymphocyte count (ALC) were compared between STAT3 wild type (WT, n = 27) and STAT3 mutant (Mut, n = 17) in all patients (n = 44). After they were divided into two subgroups, comparisons were performed between STAT3 WT (n = 16) and STAT3 Mut (n = 9) in T-LGL (n = 25) and between STAT3 WT (n = 8) and STAT3 Mut (n = 8) in T-LGL + PRCA (n = 16). Boxplots show the median values and interquartile ranges of CBC parameters and Wilcox rank sum tests were used for statistics. Abbreviations: PRCA, pure red cell aplasia; T-LGL, T-cell large granular lymphocyte leukemia; T-LGL + PRCA, T-LGL combined with PRCA; STAT3, signal transducer and activator of transcription 3.
Association of STAT3 mutational burden with CBC parameters
The levels of VAF detected in the STAT3 mutation showed significant correlation with hemoglobin levels (Fig. 3a). Of note, seven patients (87.5%, 7/8) in the T-LGL + PRCA, marked by red dots, showed low (< 10%) levels of VAF, while only two patients (22.2%, 2/9) with T-LGL, marked by blue dots, showed low levels of VAF. A significantly lower median level of VAF was detected in STAT3 in T-LGL + PRCA (4.5%, IQR 3.5–6.6%) compared with T-LGL (24.8%, 22.1–29.4%) (Table 1).
Association of STAT3 mutational extent with CBC parameters. (a) The hemoglobin level, (b) absolute neutrophil count (ANC) and (c) absolute lymphocyte count (ALC) were presented with variant allele frequency (VAF) levels of STAT3 mutation in STAT3 mutant (n = 17). The red dots represent patients with T-LGL (n = 9) and blue dots represents patients with T-LGL + PRCA (n = 8). Linear lines are linear regression fits. (d) Mutation types of the STAT3 gene were presented with STAT3 VAF in order of detected frequency. Abbreviations: the same as shown in Fig. 2.
Among 17 STAT3 mutations, 16 mutations were localized in the src homology 2 domain where Y640F (n = 6), D661Y/V (n = 5), N647I (n = 3), and G618R (n = 2) were detected (Fig. 3d, Supplementary Fig. 1). In the DNA-binding domain, one H410R mutation was detected in T-LGL. The most frequent mutation, Y640F, was mainly observed in low level VAF (< 10%) and prevalent in T-LGL + PRCA (62.5%, 5/8), which differed significantly from the prevalence in T-LGL (11.1%, 1/9, P = 0.043, Fig. 3d). Of particular interest, Y640F was the most commonly detected mutation among patients with < 10% VAF of STAT3 mutation in our population (66.7%, 6/9) and in other reports (59.6%, 28/47)26 (Supplementary Fig. 2). ANC showed no correlation with the level of STAT3 VAF (Fig. 3b), however ALC showed significant correlation with the level of STAT3 VAF (Fig. 3c). Platelet count showed no correlation with STAT3 VAF.
Therapeutic effect according to mutations
CR or PR was achieved in 25 (80.6%) of 31 patients (Fig. 1). All STAT3 mutant patients showed CR or PR to treatments (100%, 13/13), which was higher compared with STAT3 wild type (66.6%, 12/18, P = 0.028). Of particular interest, patients with mutation of the TERT promoter (n = 4, marked in red in Fig. 1) showed CR (100%, 4/4), while 40.7% of patients without mutation of the TERT promoter showed CR (11/27, P = 0.043).
Specificity of STAT3 and STAT5B mutations in hematologic diseases without T-LGL
Conduct of a retrospective analysis of 591 hematologic patients without T-LGL resulted in identification of three patients with STAT3 (n = 1, 0.17%) or STAT5B (n = 2, 0.34%) mutations. One patient with STAT3 mutation (G618R, VAF 7.6%) had already been diagnosed with therapy-related MDS. Following performance of additional CD3, CD4, CD8, and granzyme B staining for reexamination of BM slides, increased interstitial infiltration of CD3, CD8 and granzyme B positive T cells was observed, demonstrating co-existence of T-LGL (ALC, 2.3 × 109/L; Large granular lymphocyte, 1.4 × 109/L). After all, because no STAT3 mutation was detected in 590 patients who did not have T-LGL, STAT3 mutation showed 100% specificity for diagnosis of T-LGL. Two patients with mutation of STAT5B were MDS-excess blasts-1 (N642H, VAF 4.8%) and idiopathic hypereosinophilia (V712E, VAF 7.9%) with no evidence of T cell infiltration.
Discussion
Mediation of idiopathic PRCA was originally considered to occur by way of autoreactive T cells capable of destroying erythroid colony-forming units by inhibition of erythropoiesis27. Expansion of T cells can be polyclonal or monoclonal with positive T cell receptor (TCR) rearrangement28. Activation of the STAT3 pathway occurs during development of T cells for undertaken mutagenesis29. Mutation of STAT3 may occur during the monoclonal expansion of T cells (Fig. 4). The occurrence of STAT3 mutation can proffer a survival benefit through the gain-of-function mutation, inducing malignant transformation and subsequent development of T-LGL.
Proposed pathogenesis of T-cell large granular lymphocyte leukemia (T-LGL) combined with pure red cell aplasia (PRCA) (T-LGL + PRCA). Various stimuli including infection, cytokines, autoimmune, or unknown antigens cause polyclonal expansion of T large granular lymphocytes (LGL). The ongoing antigen stimulation can induce monoclonal expansion of LGL. The expanded polyclonal or monoclonal LGL is capable of inhibiting erythroid colony-forming units (E-CFU) and inducing PRCA. During monoclonal expansion, the STAT3 mutations can occur or activation of STAT3 occur through another non-mutational mechanism. Although there was no report proving a direct inhibitory effect of STAT3 mutated T cells on myelopoiesis, our data suggest that low mutational burden of STAT3 in T-LGL + PRCA may induce a greater reduction of absolute neutrophil count (ANC) than wild type. Of note, high mutational burden of STAT3 observed in T-LGL alone may not only reduce ANC and hemoglobin, but also increase the circulating lymphocyte count. Conduct of further study of the mutational process of the STAT3 gene and the functional role of STAT3-mutated T cells will be required in the future.
In the T-LGL + PRCA, the low levels of hemoglobin detected in the STAT3 wild type were similar to those detected in the STAT3 mutant (Fig. 2a), suggesting the existence of a severe anemic state regardless of emergence of STAT3 mutation. In addition, the low level of ALC detected in patients with T-LGL + PRCA (Table 1) compared to those with T-LGL alone also suggests newly developing T-LGL in already existing PRCA. Beside the low levels of ALC, patients with T-LGL + PRCA were older in age, compared to those with T-LGL alone, implying that T-LGL + PRCA is a unique disease entity separate from T-LGL alone, which should be classified as a subtype of T-LGL.
Mutation of STAT3 has been reported to occur in 30~75% of patients with T-LGL6,15,16,30, similar to our result of 41.5% in patients with T-LGL. Shi et al. reported that mutation of STAT3 was not detected using Sanger sequencing in patients with T-LGL + PRCA21, while in our study, mutation of STAT3 was detected using a high depth of sequencing in 50% of patients with T-LGL + PRCA, particularly with mainly low levels of VAF. This may be attributable to differences in the technical sensitivity of the type of sequencing used. We were able to determine the characteristics of T-LGL + PRCA, which usually showed a low level of VAF in the STAT3 mutation resulting from use of high depth of sequencing. Use of a high depth of sequencing is important for detection of low mutant clones.
Since the lower limit of detection for Sanger sequencing is usually around 10%26, we arbitrarily defined the cut-off of STAT3 mutation as 10%. Interestingly, the low level of VAF (< 10.0%) was mostly detected in T-LGL + PRCA. Moreover, STAT3 Y640F mutation was the most common mutations in T-LGL + PRCA. These findings suggest T-LGL + PRCA is a unique disease entity that can be classified as a subtype of T-LGL. Jerez et al. suggested that STAT3 mutant immune attack itself can cause primary induction of BMFS, which may mean even a low mutational burden of STAT3 can influence disease progression12.
The VAF levels of mutated genes partly depend on the proportion of large granular lymphocytes in the analyzed samples. Therefore, the cell sorting has been tried to overcome the variation7,31. Using CD8 + T cell sorting technique, STAT3 mutations were exclusively detected in certain TCR Vβ population of CD8 + T cells31. Since our study did not use the cell sorting technique, we could not adjust STAT3 VAF levels according to the large granular lymphocyte counts. Recently, there has been a standardization approach in NGS that improve tumor purity metrics by using new computational algorithms for neoplastic cellularity32. It is worth applying the standardized approach to compare VAF levels in future study.
An association of STAT3 mutation with a low level of ANC has been reported16,33. Similarly, our results for all cases of T-LGL showed that the level of ANC was lower in the STAT3 mutant than in wild type. However, when divided into subgroups, a low level of ANC was detected in patients with T-LGL regardless of STAT3 mutation (Fig. 2b), indicating that the low level of ANC in T-LGL was independent of STAT3 mutation. Within patients with T-LGL + PRCA, STAT3 mutant patients with usually low levels of VAF showed lower levels of ANC compared with STAT3 wild type (Fig. 2b) and even patients with a high level of VAF in the STAT3 mutation showed similarly low levels of ANC along with low levels of VAF (Fig. 3b), suggesting that even the low mutational burden of STAT3 could sufficient to inhibit myelopoiesis (Fig. 4). Mariotti et al. suggested that STAT3 activation interacts with microRNA-146b and then regulates Fas ligand expression to induce neutrophil apoptosis34.
Although low levels of ANC have been detected in patients with STAT3 mutation, the association of STAT3 mutation with hemoglobin level remains unclear7,16,33. Recent study revealed that STAT3 mutation impaired the increase in erythropoietin-induced phosphorylation of STAT5 in erythroid precursors. Since the phosphorylation of STAT5 determines erythropoiesis rate, STAT3 mutation may induce anemia35. In the T-LGL, significantly decreased levels of hemoglobin were detected in the STAT3 mutant. However, in the T-LGL + PRCA, low levels of hemoglobin were detected regardless of STAT3 mutation. This finding suggests that combined PRCA by itself can cause a decrease in the level of hemoglobin even in STAT3 wild type; so that the difference in hemoglobin is obscured by the mutation.
Following STAT3, the genes showing frequent mutation in T-LGL included KMT2D, TERT, SUZ12, BCOR, DNMT3A, and RUNX1. Similar to findings reported in previous studies16,36, our results showed that the KMT2D mutation was the second most common mutation detected in T-LGL. KMT2D is regarded as a tumor suppressor, and its mutation leads to induction of lymphomas in mice37. A recent study reported on the association of KMT2D mutation with risk of lymphoid malignancy in the general population38.
Our results showed that four patients had mutations of the TERT promoter and showed a good response to treatment. Although the TERT gene has been detected in a few cases of aplastic anemia39, no study has reported on TERT mutation in T-LGL or PRCA even with whole exome sequencing. Application of high depth of sequencing to the proximal promoter region of the TERT gene enabled detection of the TERT mutation. These hot spot mutations (c.-124C > T and c.-146C > T) have been detected in variable proportions of solid tumors40 and in 33% of cases of mantle cell lymphoma41. The mutations can lead to increased telomerase activity through transcriptional activation of TERT, facilitating telomere maintenance and the subsequent tumorigenesis in human cancers42. In addition, the STAT3 gene can act on the 5’ end of the TERT promoter, leading to activation of TERT40,43. Considering that the VAF levels detected in the TERT promoter mutations (patient numbers 4, 9) were respectively similar to those of STAT3, the TERT mutation clone may be the same as the STAT3 clone and both mutations may exert a synergistic effect on telomerase activity. Of note, four patients with TERT mutations showed good responses to treatments, suggesting that TERT mutation-induced florid expansion of T cells may be a sensitive target for immunosuppressants44. However, one study reported contrasting results that showed poor prognosis in patients with mantle cell lymphoma, thus conduct of further study will be required41.
An association of TNFAIP3, another gene showing recurrent mutation in T-LGL, with mutation of STAT3 has been reported16,45. In these papers, the TNFAIP3 mutations co-occurred with STAT3 mutations were mostly nonsense or frameshift mutations (8/9, 88.9%). In our results, one nonsense and one frameshift TNFAIP3 mutations were detected in STAT3 mutants with VAF levels that were comparable or lower than those of STAT3, implying either co-presence as the same clone with STAT3 or subclone. TNFAIP3 encodes a regulator of nuclear factor kappa B (NF-kB) signaling; this mutation made truncate A20 protein and induce deregulation of NF-kB activity, with induction of the LGL phenotype45. In addition, SUZ12 regulates chromatin modification and the mutation can contribute to proliferation of cancer cell and T cells46. NF1 is a negative regulator of the Ras signaling pathway and the loss of function mutation results in cell proliferation. Considering that STAT3 activation in KRAS mutant pancreatic cancer was reported to facilitate cell progression47, the KRAS L19F mutation in our patient (patient number 10) may have interaction potential with STAT3 mutation. TP53 mutations could induce T cell proliferation through inhibition and apoptosis. In our result, DNMT3A mutations were detected exclusively in the STAT3 mutant, consistent with the previous report16.
Mutations of five genes (BCOR, BCORL1, PIGA, DNMT3A, and ASXL1) have been detected in 5~10% of cases of aplastic anemia17. Because the subclinical T cell clone may be detected in a subset of aplastic anemia, we attempted to examine these mutation frequencies in T-LGL. Contrary to our expectation, no mutation was detected in BCORL1, PIGA, and ASXL1, and only three mutations each were detected in BCOR and DNMT3A, respectively. The mutation spectrum of T-LGL is considered to differ from that of aplastic anemia.
T-LGL has been detected in 2.5~27% of cases of MDS12,48 and MDS has been detected in 5.4% of cases of T-LGL19. Our study showed similar results, where MDS was detected in 7.3% (3/41) of cases of T-LGL. There is an expectation that performance of high depth sequencing will lead to discovery of the existence of subclinical MDS. It is unclear whether clonal expansion of T cells occurs as a result of an immune surveillance response to an aberrant MDS clone in already existing MDS or MDS occurs as T-cell mediated DNA damage to myeloid cells and subsequent acquisition of somatic mutations in already existing T-LGL19,20. Considering the low levels of VAF detected in many mutations in three patients with T-LGL with concomitant MDS, emergence of a small MDS clone in already existing T-LGL is plausible.
According to our results, among 591 patients who were not diagnosed with T-LGL, STAT3 mutation was detected in one patient in whom subclinical T-LGL was detected later. Qu et al. reported similar results demonstrating that STAT3 mutations were predominantly detected in patients with T-LGL, except for six patients with unexplained cytopenia showing low levels of VAF STAT3 mutations, suggesting the potential for eventual development of T-LGL30. Although other study has reported on detection of STAT3 mutations in a subset of myeloid neoplasms, the authors acknowledged that subclinical T-LGL could not be excluded because further testing for detection of the subclinical T-LGL was not performed11.
According to our results, STAT5B mutations were detected in one patient with MDS and one patient with hypereosinophilia. Of note, a STAT5B N642H mutation was detected in the patient with hypereosinophilia, which was reported to show an association with myeloid neoplasm with eosinophilia49. Unlike STAT3, STAT5B mutations are not specific to T-LGL, and can be detected in other myeloid neoplasms30.
STAT3 mutation was not detected in a substantial fraction of cases of T-LGL. Considering that constitutive activation of STAT3 was observed even in STAT3 wild type, clonal expansion of T cells may be induced by other abnormalities such as a mechanism of dysregulation by activated interleukin (IL)-6 and a STAT3 loop in wild type8. Interestingly, STAT3 phosphorylation is enhanced by several inflammatory cytokines such as IL-6, IL-15 and MCP-150. Of note, overexpression of IL-15 could contribute to cell growth, chromosomal instability and leukemic transformation of T-LGL51.
This study has several limitations. First, evaluation of the characteristics of T-LGL subtypes according to cell phenotype could not be performed due to lack of access to flow cytometry and a relatively low number of patients, thus further study will be required. Second, matched germline samples could not be utilized due to the retrospective design of the study. However, we made a sincere effort to exclude germline variants during data processing. Third, because our data were acquired from one tertiary hospital, there is a possibility of ethnic differences and selection biases for T-LGL and PRCA.
To the best of our knowledge, this is the first study to report on T-LGL + PRCA showing unique features (low level of VAF in the STAT3 mutation, low level of ALC, and old age), reflecting late emergence of T-LGL in patients with already existing PRCA. In the T-LGL alone subgroup, a low level of ANC was detected in both the STAT3 mutant and wild type and lower level of hemoglobin was detected in the STAT3 mutant compared with wild type, while in the T-LGL + PRCA subgroup, low level of hemoglobin was detected regardless of STAT3 mutation and a low level of ANC was detected in the STAT3 mutant with a low level of VAF, suggesting that even a low mutational burden of STAT3 is sufficient to reduce the level of ANC. Beside mutation of STAT3, genes showing frequent mutation in T-LGL included KMT2D (17.1%), TERT (12.2%), SUZ12 (9.8%), BCOR (7.3%), DNMT3A (7.3%), and RUNX1 (7.3%). Concomitant MDS was detected in 7.3% (3/41) of cases of T-LGL through a high depth of NGS. Genes showing recurrent mutation (BCORL1, PIGA, and ASXL1) detected in aplastic anemia were not detected in patients with T-LGL. Of note, the results showed recurrent detection of mutations of the TERT promoter with good response to treatment. In addition, STAT3 mutations were not detected in other myeloid neoplasms, while STAT5B mutations were detected in 0.34% of our cohort of patients with hematologic diseases.
In conclusion, the findings of our study suggest that T-LGL+PRCA is a unique disease entity that can be classified as a subtype of T-LGL. Although mutation of STAT3 leads to a reduction in the levels of ANC and hemoglobin, the underlying severity of T-LGL or PRCA can obscure the reduction effects. Routine utilization of high depth NGS testing can provide sensitive detection of concomitant MDS in patients with T-LGL. STAT3 mutations suggest the presence of subclinical T-LGL in hematologic diseases. Mutation of the TERT promoter may indicate a good response to treatment of T-LGL, thus its addition to the NGS panel may be recommended.
Methods
Patient selection
Patients diagnosed with T-LGL (n = 41) or isolated PRCA (n = 3) were enrolled in the study. Patients with T-LGL were divided into two subgroups; T-LGL alone (n = 25) and T-LGL + PRCA (n = 16). T-LGL in our study was diagnosed when the following 3 criteria were met52. First, increased number of large granular lymphocytes (> 2 × 109/L) was identified in peripheral blood smear. Second, T cell expansion was confirmed by immunohistochemistry (CD3, CD4, CD8, and granzyme B) of BM biopsy. Third, TCR gene rearrangement was present. If the circulating large granular lymphocyte number was less than 2 × 109/L, both T cell expansion in immunohistochemistry of BM and presence of TCR gene rearrangement along with cytopenia were mandatory. In TCR gene rearrangement, 34 patients (77.3%) were positive for both TCR beta and gamma, 3 patients (6.8%) were positive for TCR beta alone, 4 patients (9.1%) were positive for TCR gamma alone. 3 PRCA patients (6.8%) were negative for both TCR gene rearrangement. Subclinical T-LGL was arbitrarily defined with clinically unsuspected but presence of clonal T cell expansion with STAT3 mutation12. A diagnosis of PRCA was made when anemia (hemoglobin < 10.0 g/dL) with absolute reticulocyte count < 10.0 × 109/L or BM proerythroblasts and/or basophilic erythroblasts < 5% of total nucleated cells4.
In addition, a review of 591 patients (173 with acute myeloid leukemia, 96 patients with MDS, 85 patients with myeloproliferative neoplasm (MPN), 77 patients with acute lymphoblastic leukemia, 35 patients with plasma cell myeloma, 28 patients with chronic lymphocytic leukemia, 20 patients with MDS/MPN, and 77 patients with cytopenia caused by other factors) who were requested for an NGS panel of hematologic malignancies at Seoul National University Hospital was conducted for identification of STAT3 and STAT5B mutation frequencies in hematologic diseases without T-LGL. These studies were approved by the institutional review board of Seoul National University Hospital (H-2106–128-1228) and were conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients.
Evaluation of bone marrow dysplasia and T cell clonality
An independent review of BM dysplasia was performed by two hematopathologists for detection of MDS. MDS based on criteria established by the WHO52 (≥ 10% dysplasia of ≥ 1 lineage). MDS was confirmed when both hematopathologists reached agreement. Anti-CD3 (DAKO, USA), CD20 (DAKO), CD4 (Leica biosystem, USA), CD8 (Roche, Switzerland), granzyme B (Roche), and CD56 antibodies (Roche), EBER in-situ hybridization (Ventana ISH iView Blue Detection Kit, Roche) were used with automatic staining (Ventana Benchmark Ultra, Roche) for exclusion of other mature T cell neoplasm and assessment of T cell expansion in BM. Most of T-LGL patients (36/41, 87.8%) expressed CD8, 2 patients (4.9%) expressed CD4, 1 patient (2.4%) were CD4/8 coexpressed and the remaining 1 patient (2.4%) showed undetermined phenotype due to poor stainability. Analysis of rearrangements of TCR gene beta and gamma chain was performed using the BIOMED-2 assay (Invivoscribe, USA) according to the manufacturer’s instructions.
Custom targeted NGS panels and data processing
Two custom targeted NGS panels were used. First, 84 genes including genes reported to show mutation in PRCA or aplastic anemia7,17,18,23,24,25, genes showing recurrent mutation in myeloid hematologic malignancy and STAT3 and STAT5B were used for T-LGL and/or PRCA patients (Supplementary Table 1). Sequencing was performed using NovaSeq6000 (Illumina, USA) by whole blood of BM (n = 22) or peripheral blood (n = 22) according to the manufacturer’s instructions. Ten unrelated healthy blood specimens without evidence of hematologic malignancy were used as controls. Analysis of data was performed using an in-house bioinformatics pipeline (Supplementary Method). The median depth of coverage was 1502 x (interquartile range, IQR; 1170–2204) and the lowest depth of coverage was 811 × for all samples. The cut-off for reporting variants was set as ≥ 2% VAF.
Second, a panel of 103 hematologic malignancy-related genes including STAT3 and STAT5B was used for hematologic diseases without T-LGL (Supplementary Table 1). Sequencing was performed using NextSeq550Dx (Illumina, USA) along with preparation of the DNA and RNA library using Archer VariantPlex Somatic Reagents and Archer FusionPlex Kits (ArcherDx Inc., USA). Analysis of sequence data was performed using Clinical Genomics Workspace (PierianDX Inc., USA). The average depth of coverage was > 200 × and the cut-off value was set as ≥ 2% VAF for all samples.
Treatment response
In our retrospective analysis for 44 patients, 31 patients who were symptomatic, transfusion-dependent, or had worsening of hematological parameters were treated with a various regimens including corticosteroid, methotrexate, cyclophosphamide, and/or cyclosporine (Supplementary Table 6). 13 patients were not treated based on asymptomatic, transfusion-independent, or clinical decision. Evaluation of treatment responses was performed according to the previous report with some modification53. The RBC transfusion dependency was defined as receiving more than three RBC transfusions within 16 weeks with at least two transfusion episodes. Complete response (CR) was defined as no need for RBC transfusion, ANC > 1.8 × 109/L, platelet > 100 × 109/L and lymphocytosis < 4.0 × 109/L during the treatment period of 16 to 24 weeks. Partial response (PR) was defined as a reduction of RBC transfusion by > 50%, ANC > 1.0 × 109/L, but < 1.8 × 109/L, platelet > 50 × 109/L, but < 100 × 109/L. Patients who did not meet these criteria were defined as no response (NR).
Statistical analysis
Chi-square test or Fisher's exact test and Wilcoxon rank sum test were performed for comparison of subgroups. Spearman correlation was performed to determine the association of the extent of STAT3 mutation with CBC parameters. P < 0.05 was considered statistically significant. All statistical analyses were performed using R version 4.2.1.
Data availability
The raw fastq files of this study have been submitted for the Sequence Read Archive (SRA) repository with the bioProject PRJNA919192.
References
Moignet, A. & Lamy, T. Latest advances in the diagnosis and treatment of large granular lymphocytic leukemia. Am. Soc. Clin. Oncol. Educ. Book 38, 616–625 (2018).
Kwong, Y. L. & Wong, K. F. Association of pure red cell aplasia with T large granular lymphocyte leukaemia. J. Clin. Pathol. 51, 672–675 (1998).
Kwong, Y. L., Au, W. Y., Leung, A. Y. & Tse, E. W. T-cell large granular lymphocyte leukemia: An Asian perspective. Ann. Hematol. 89, 331–339 (2010).
Means, R. T. Jr. Pure red cell aplasia. Blood 128, 2504–2509 (2016).
Oshimi, K. Clinical features, pathogenesis, and treatment of large granular lymphocyte leukemias. Intern. Med. 56, 1759–1769 (2017).
Fattizzo, B., Bellani, V., Pasquale, R., Giannotta, J. A. & Barcellini, W. Large granular lymphocyte expansion in myeloid diseases and bone marrow failure syndromes: Whoever seeks finds. Front. Oncol. 11, 748610 (2021).
Koskela, H. L. et al. Somatic STAT3 mutations in large granular lymphocytic leukemia. N. Engl. J. Med. 366, 1905–1913 (2012).
Teramo, A. et al. Intrinsic and extrinsic mechanisms contribute to maintain the JAK/STAT pathway aberrantly activated in T-type large granular lymphocyte leukemia. Blood 121, 3843–3854, s3841 (2013).
Lamy, T., Moignet, A. & Loughran, T. P. Jr. LGL leukemia: From pathogenesis to treatment. Blood 129, 1082–1094 (2017).
Fasan, A. et al. STAT3 mutations are highly specific for large granular lymphocytic leukemia. Leukemia 27, 1598–1600 (2013).
Kavesh, M. et al. Distinguishing STAT3/STAT5B-mutated large granular lymphocyte leukemia from myeloid neoplasms by genetic profiling. Blood Adv. 7, 40–45 (2023).
Jerez, A. et al. STAT3 mutations indicate the presence of subclinical T-cell clones in a subset of aplastic anemia and myelodysplastic syndrome patients. Blood 122, 2453–2459 (2013).
Rajala, H. L. et al. Discovery of somatic STAT5b mutations in large granular lymphocytic leukemia. Blood 121, 4541–4550 (2013).
Andersson, E. I. et al. High incidence of activating STAT5B mutations in CD4-positive T-cell large granular lymphocyte leukemia. Blood 128, 2465–2468 (2016).
Coppe, A. et al. Genomic landscape characterization of large granular lymphocyte leukemia with a systems genetics approach. Leukemia 31, 1243–1246 (2017).
Cheon, H. et al. Genomic landscape of TCRαβ and TCRγδ T-large granular lymphocyte leukemia. Blood 139, 3058–3072 (2022).
Yoshizato, T. et al. Somatic mutations and clonal hematopoiesis in aplastic anemia. N. Engl. J. Med. 373, 35–47 (2015).
Fujishima, N. et al. Clonal hematopoiesis in adult pure red cell aplasia. Sci. Rep. 11, 2253 (2021).
Durrani, J. et al. Large granular lymphocytic leukemia coexists with myeloid clones and myelodysplastic syndrome. Leukemia 34, 957–962 (2020).
Bravo-Pérez, C., Carrillo-Tornel, S., García-Torralba, E. & Jerez, A. Persistent large granular lymphocyte clonal expansions: “The Root of Many Evils”-and of some goodness. Cancers (Basel) 14, 1340 (2022).
Shi, M. et al. STAT3 mutation and its clinical and histopathologic correlation in T-cell large granular lymphocytic leukemia. Hum. Pathol. 73, 74–81 (2018).
Kawakami, F. et al. T cell clonal expansion and STAT3 mutations: A characteristic feature of acquired chronic T cell-mediated pure red cell aplasia. Int. J. Hematol. 115, 816–825 (2022).
Long, Z. et al. Gene mutation profile in patients with acquired pure red cell aplasia. Ann. Hematol. 99, 1749–1754 (2020).
Slavin, T. P. et al. Association between clonal hematopoiesis and late nonrelapse mortality after autologous hematopoietic cell transplantation. Biol. Blood. Marrow Transplant. 25, 2517–2521 (2019).
Takahashi, K. et al. Preleukaemic clonal haemopoiesis and risk of therapy-related myeloid neoplasms: A case-control study. Lancet Oncol. 18, 100–111 (2017).
Rajala, H. L. et al. The analysis of clonal diversity and therapy responses using STAT3 mutations as a molecular marker in large granular lymphocytic leukemia. Haematologica 100, 91–99 (2015).
Charles, R. J., Sabo, K. M., Kidd, P. G. & Abkowitz, J. L. The pathophysiology of pure red cell aplasia: Implications for therapy. Blood 87, 4831–4838 (1996).
Balasubramanian, S. K. et al. Rational management approach to pure red cell aplasia. Haematologica 103, 221–230 (2018).
Siegel, A. M. et al. A critical role for STAT3 transcription factor signaling in the development and maintenance of human T cell memory. Immunity 35, 806–818 (2011).
Qu, S. et al. STAT3 and STAT5B mutations have unique distribution in T-cell large granular lymphocyte proliferations and advanced myeloid neoplasms. Leuk. Lymphoma 62, 1506–1509 (2021).
Kawakami, T. et al. Frequent STAT3 mutations in CD8(+) T cells from patients with pure red cell aplasia. Blood Adv. 2, 2704–2712 (2018).
Patel, N. M. et al. Improved tumor purity metrics in next-generation sequencing for clinical practice: The integrated interpretation of neoplastic cellularity and sequencing results (IINCaSe) approach. Appl. Immunohistochem. Mol. Morphol. 27, 764–772 (2019).
Teramo, A. et al. STAT3 mutation impacts biological and clinical features of T-LGL leukemia. Oncotarget 8, 61876–61889 (2017).
Mariotti, B. et al. Identification of a miR-146b-Fas ligand axis in the development of neutropenia in T large granular lymphocyte leukemia. Haematologica 105, 1351–1360 (2020).
Mauracher, A. A. et al. Erythropoiesis defect observed in STAT3 GOF patients with severe anemia. J. Allergy. Clin. Immunol. 145, 1297–1301 (2020).
Savola, P., Bhattacharya, D. & Huuhtanen, J. The spectrum of somatic mutations in large granular lymphocyte leukemia, rheumatoid arthritis, and Felty’s syndrome. Semin. Hematol. 59, 123–130 (2022).
Alam, H. et al. KMT2D deficiency impairs super-enhancers to confer a glycolytic vulnerability in lung cancer. Cancer Cell 37, 599-617.e597 (2020).
Niroula, A. et al. Distinction of lymphoid and myeloid clonal hematopoiesis. Nat. Med. 27, 1921–1927 (2021).
Yamaguchi, H. et al. Mutations in TERT, the gene for telomerase reverse transcriptase. Aplastic Anemia. N. Engl. J. Med. 352, 1413–1424 (2005).
Killela, P. J. et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc. Natl. Acad. Sci. U.S.A. 110, 6021–6026 (2013).
Panero, J. et al. Acquired TERT promoter mutations stimulate TERT transcription in mantle cell lymphoma. Am. J. Hematol. 91, 481–485 (2016).
Huang, D. S. et al. Recurrent TERT promoter mutations identified in a large-scale study of multiple tumour types are associated with increased TERT expression and telomerase activation. Eur. J. Cancer 51, 969–976 (2015).
Dratwa, M., Wysoczańska, B., Łacina, P., Kubik, T. & Bogunia-Kubik, K. TERT-regulation and roles in cancer formation. Front. Immunol. 11, 589929 (2020).
Zanetti, M. A second chance for telomerase reverse transcriptase in anticancer immunotherapy. Nat. Rev. Clin. Oncol. 14, 115–128 (2017).
Johansson, P. et al. Recurrent alterations of TNFAIP3 (A20) in T-cell large granular lymphocytic leukemia. Int. J. Cancer 138, 121–124 (2016).
Ntziachristos, P. et al. Genetic inactivation of the polycomb repressive complex 2 in T cell acute lymphoblastic leukemia. Nat. Med. 18, 298–301 (2012).
Corcoran, R. B. et al. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Res. 71, 5020–5029 (2011).
Komrokji, R. S. et al. Characterization of myelodysplastic syndromes (MDS) with T-cell large granular lymphocyte proliferations (LGL). Leukemia 34, 3097–3099 (2020).
Cross, N. C. P. et al. Recurrent activating STAT5B N642H mutation in myeloid neoplasms with eosinophilia. Leukemia 33, 415–425 (2019).
Isabelle, C. et al. Cytokines in the pathogenesis of large granular lymphocytic leukemia. Front. Oncol. 12, 849917 (2022).
Mishra, A. et al. Aberrant overexpression of IL-15 initiates large granular lymphocyte leukemia through chromosomal instability and DNA hypermethylation. Cancer Cell 22, 645–655 (2012).
Swerdlow, S. H., Campo, E., Harris, N. L., Jaffe, E.S., Pileri, S.A., Stein, H., Thiele, J., & Vardiman, J.W. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Revised 4th Edition edn. Vol. 2 (IARC, 2017).
Platzbecker, U. et al. Proposals for revised IWG 2018 hematological response criteria in patients with MDS included in clinical trials. Blood 133, 1020–1030 (2019).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) Grant (2021R1A2C1006302) funded by the Korea Government (MSIT).
Author information
Authors and Affiliations
Contributions
S.Y.P. performed the research, analyzed data and wrote the paper; J.W.Y. performed the research and analyzed data; J.Y.G. performed the research; S.Y.C., D.J.J., J.S.L., M.W.S. and Y.H.C. critically reviewed the manuscript; H.S.Y. performed bioinformatics analysis and interpretation; H.K.K. designed the research, analyzed data and wrote the paper. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, S., Yun, J., Choi, S.Y. et al. Distinct mutational pattern of T-cell large granular lymphocyte leukemia combined with pure red cell aplasia: low mutational burden of STAT3. Sci Rep 13, 7280 (2023). https://doi.org/10.1038/s41598-023-33928-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33928-z
- Springer Nature Limited