Abstract
Patients undergoing total-knee arthroplasty (TKA) have transient increases in anterior knee skin temperature (ST) that subside as recovery progresses–except in cases of systemic or local prosthetic joint infections (PJI). This meta-analysis was designed to quantify the changes in knee ST following TKA in patients with uncomplicated recovery as a prerequisite for assessing the usefulness of thermal imaging for diagnosis of PJI. This meta-analysis (PROSPERO-CRD42021269864) was performed according to PRISMA guidelines. PUBMED and EMBASE were searched for studies reporting knee ST of patients that underwent unilateral TKA with uncomplicated recovery. The primary outcome was the weighted means of the differences in ST between the operated and the non-operated knees (ΔST) for each time point (before TKA, and 1 day; 1,2, and 6 weeks; and 3,6, and 12-months post-TKA). For this analysis, 318 patients were included from 10 studies. The elevation in ST was greatest during the first 2-weeks (ΔST = 2.8 °C) and remained higher than pre-surgery levels at 4–6 weeks. At 3-months, ΔST was 1.4 °C. It decreased to 0.9 °C and 0.6 °C at 6 and 12-months respectively. Establishing the baseline profile of knee ST following TKA provides the necessary first step for evaluating the usefulness of thermography for the diagnosis of post-procedural PJI.
Similar content being viewed by others
Introduction
The number of Total-knee arthroplasty (TKA) procedures in the US is projected to reach approximately 3.5 million by 20301. Prosthetic joint infection (PJI) occurs in up to 2% of primary arthroplasties leading to significant morbidity often requiring complex, multi-disciplinary treatments2. Nonetheless, uniform criteria have not been established for the diagnosis of TKA-associated PJI. The various guidelines emphasize that the diagnosis should be multi-disciplinary and include not only clinical examination and serum analysis, but also microbial culture, intraoperative findings, biochemical studies, and appropriate histopathological and immune-histochemical analyses3,4. While there is strong evidence for the usefulness of blood tests, including white cell counts and erythrocyte sedimentation rate, as well as C-reactive protein, and interleukin-6, imaging modalities localized to the knee region, such as PET-CT and nuclear scan, have been considered to provide only limited supporting evidence for the presence of PJI3.
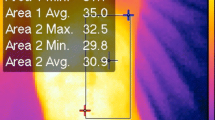
Infrared thermography is a noninvasive method that has been used in a variety of clinical entities to measure skin temperature distribution5. The latter is subtended by microcirculatory blood flow6 which is altered in inflammatory processes such as osteoarthritis7,8, infections9, or as a normal physiological response following surgical procedures. Incisions of the skin, muscle, and bone have been shown to be associated with an increase in C-reactive protein (CRP) and pro-inflammatory cytokines as well as local edema–all of which can contribute to increases in skin temperature (ST)10,11. Studies of patients undergoing TKA have shown a transient increase in knee ST that subsides as the recovery progresses (Fig. 1)10,12,13,14,15,16,17,18,19,20. However, this is not the case when there are systemic or prosthetic joint infections9,21,22.
Thermal Imaging Following Total Knee Arthroplasty (TKA). Left: operated right knee 2wks post TKA; Right: thermal image showing elliptical area of measurement around the patella of the operated (R) and unoperated (L) knees. See temperature scale in the margin. Note increased skin temperature (red and white) of the operated knee. These images were from a clinical study (#0251-20-HMO) the PI of which was LK. Informed consent was obtained from the patients as required.
The present study was designed, using a systematic-review and meta-analysis approach in order to establish the baseline, quantitative, temporal characteristics of knee skin-temperature, before and after TKA, in patients with uncomplicated recovery. This is a necessary prerequisite for assessing the usefulness of thermal imaging as an objective, non-invasive method for diagnosis of prosthetic joint infections.
Results
The results of the systematic literature search are presented in the PRISMA flow diagram (Fig. 2). We identified 349 potentially relevant articles by systematically searching EMBASE and PubMed, and an additional 12 were obtained from manual citation search. After removal of duplicates, 243 records were screened of which 230 were excluded according to the eligibility criteria. Full texts of the remaining articles, together with those identified by citation research (n = 25), were sought for more detailed evaluation of which 10 were included in the meta-analysis (Table 1). In the studies with non-standard treatment (peripheral nerve block13, titanium nitride prosthesis coating17, and celecoxib [NSAID]19), only the control data were included. The studies were performed in Europe (UK, France, Italy, the Netherlands) and Asia (China and Thailand) and included patients with uncomplicated recovery the majority of which were women. The age of the patients ranged from 58 to 72 years. Of the 318 patients included in the systematic review (from 10 studies), the majority had a background of primary knee osteoarthritis (KOA) with the minority (20 patients) having other conditions including post-traumatic KOA, rheumatoid arthritis, osteonecrosis, and osteochondritis dissecans. TKA was performed by the standard medial approach in all studies. Not all studies reported the details of the TKA procedure. Of those that reported, 5 used a tourniquet, and one did not; 4 used the patellar component in the prosthesis, while 2 did not. The skin temperature of the anterior knee region was measured before TKA and from the first day to 5 years after the procedure. Skin temperature was measured using a surface infrared thermometer or a thermal imaging system (Table 1). Average skin temperature over the knee region was reported as absolute temperature (°C) of operated and non-operated knees or as the difference between the knees. The position of the patients at the time of temperature measurement varied between studies. In some, the knee temperature was measured when the patients were sitting12,18, some supine13,15,17, and, in one study, while standing 16. The acclimatization time varied between 3 and 20 min with some studies not reporting this important feature10,13,14,19,23. Regarding the measurement area, two groups that used thermal imaging measured the average temperature of the knee area surrounding the surgical scar including the patella15,16; while groups that used a thermometer mostly did not include the patella as part of the measurement12. By overall appraisal, three studies were graded as having good thermal methodology12,16,18, while all others were graded as ‘Fair’ (Table 2).
Figures 3 and 4 present the results of the meta-analysis as 8 separate Forest Plots-one for each time point. These results are also summarized in Table 3 together with the statistics for heterogeneity and publication bias (‘file drawer bias’). In view of the high heterogeneity score in all variables (I2 > 75%, p < 0.001), we applied the random-effect model for the analysis. Publication bias was not detected in any of the time points (p > 0.05 by Egger’s test).
Meta-Analysis Forest Plots of ΔST Before TKA and at Early Follow Ups. This panel presents Forest plots of the mean temperature differences between the operated and non-operated knees (ΔST) before and up to 2 weeks post TKA using the random-effect model. Articles in each Forest plot are listed by year of publication. The mean, standard error and p-value of each study, and the pooled mean difference, are presented. Note that the difference in temperature between knees is significantly greater at all time points—even before the surgery.
Meta-Analysis Forest Plots of ΔST at Medium and Long-Term Follow Ups. This panel presents Forest plots of ΔST from 4 to 6 weeks to 1 year post TKA. See details in the previous figure. Here too note that the operated knee was significantly warmer than the non-operated knee at all time points—even 1 year post-TKA.
Figure 5 is an integrative bar graph of results from all time points with accompanying statistics. In uncomplicated knee recovery, ΔST was highest during the first 2-weeks post-surgery reaching a pooled mean of over 2.8 °C. The ΔST continued to be significantly higher than pre-TKA levels at 4–6 weeks (p < 0.0001). At 3-months post-TKA, ΔST was 1.4 °C and then gradually decreased to 0.9 °C and 0.6 °C at 6 and 12-months post-surgery respectively which were similar to pre-surgical levels (p > 0.95, pre-TKA vs. 6 and 12 months).
Knee Skin Temperature Before and After Total Knee Arthroplasty. Bar graph integrating meta-analysis results showing knee skin temperature differences in degrees Celsius before total knee arthroplasty (pre-TKA) and for each follow up time point (post-TKA) as well as the statistical results of the comparisons between these time-points. Bars = pooled weighted mean ± standard error of the mean by meta-analysis. Statistical results by 1-way ANOVA with Tukey as post-hoc test: *p < 0.005 vs Pre-TKA; #p = 0.015 vs 1 wk; TKA = total knee arthroplasty; n = number of studies included; d = day; w = week; m = months; y = year.
Discussion
We reviewed and analyzed the quantitative profile of temporal changes in skin temperature after TKA in patients with uncomplicated recovery. There is a prominent increase in ΔST in the first 2 weeks post-TKA that gradually resolves by 6 months reaching near pre-surgical values at 1-year post-surgery when clinical recovery was considered satisfactory and to occur without complication.
The average ΔST prior to surgery (0.4 ± 0.1 °C) was very close to the threshold of minimal clinical important difference in symmetrical limbs (0.5 °C 24). This initial significant ΔST can be explained by the underlying knee osteoarthritis characterizing the majority of patients that arrive for TKA. Previous studies report that osteoarthritis causes elevated ST compared to the unaffected knee (0.1–0.6 °C)8,25,26. However, patients with bilateral osteoarthritis, or other bilateral pathologies such as rheumatoid arthritis, may not show this difference27. The increased skin temperature in the early weeks following TKA was expected due to the acute inflammation that normally accompanies surgical procedures. However, at 6 months, clinically significant differences in skin temperature (≥ 0.5 °C24) were still present and lingered 1 year post surgery. This may reflect ongoing healing with changes in patellar blood flow and/or skin microvasculature28 in the area of the surgery.
Studies of patients with delayed PJI following TKA, including some after surgical revisions, showed elevated ST. Mumingjiang et al. reported that patients with PJI at 6 months post-TKA had differences in ST between the operated and non-operated knees of 4.2 ± 1.0 °C versus 1.0 ± 0.3 °C in patients without PJI16. Romano et al. reported that patients with PJI 8 months after TKA had differences in ST of 1.6 ± 0.6 °C versus 0 ± 0.4 °C in patients without PJI21. In a subsequent study, Romano et al. reported that at 1 year after TKA, patients with PJI had differences in ST of 2.2 ± 1.5 °C versus 0.6 ± 0.5 °C in those without PJI22. The patients from those 3 studies were diagnosed with PJI on the basis of elevated serum inflammatory markers as well as clinical signs of infection including local redness and swelling. However, cases of chronic low-grade infection after TKA are not commonly associated with these local characteristics of inflammation, and are therefore sometimes misdiagnosed as aseptic failures3,4. Further studies are warranted to determine if skin temperature measurements are useful for this particularly challenging condition.
According to this meta-analysis, the average normal ΔST at 6 months after TKA is 0.9 °C, and, at 1 year, it is 0.6 °C. Neither is significantly different from the pre-surgical levels, and both are clearly lower than that found in the studies of patients with PJI. As determined by this meta-analysis, it appears that, for each time point, the acceptable differentiation between conditions should be based on the 95%CI upper limit of the pooled weighted means of uncomplicated patients with an addition of 0.5 °C24. For example, at 12 months (95%CI upper limit = 1.0 °C), patients with a difference in ST of > 1.5 °C may be at risk for PJI. This hypothesis should be confirmed in further studies.
Skin temperature can be measured in sufficient resolution with infrared thermometers or thermal imaging cameras29. In 2 of the reviewed studies, thermal imaging was used to determine the average temperature over the entire region surrounding the surgical area15,16. Others used infrared thermometers to measure skin temperature at specific points, some of which did not include the patella. Since the contralateral knee was evaluated as part of the outcome, the difference in instrumentation should not influence the overall results30. Likewise, although the position of the patient is expected to influence the absolute measurement because of differences in blood flow between postures, here too these differences are expected to be of limited influence since both knees were measured under similar conditions31. The factor that is considered to have the greatest influence is the ambient temperature. This has 2 components—the room temperature and the exposure time for acclimatization. It is reasonable to assume that orthopedic clinics are climate controlled to 25 °C or less, and that patients do not experience extreme cold or heat during visits29. The optimal skin acclimatization time for whole body thermograms was determined to be 10 min, but it is shorter for the lower limbs32. Moreover, in the latter study, the changes in ST during the acclimatization time were found to be parallel in symmetrical limbs. Thus, it can be assumed that 5 min will be sufficient to determine a difference of 1 °C or more between knees, although the exact time threshold should be determined in subsequent clinical studies.
Applying a tourniquet during the TKA procedure modifies the blood flow and therefore may affect knee ST. Alisi et al.33 reported that ST of the ankle region decreased on application of a tourniquet during a TKA procedure. However, ST levels returned to pre-procedural levels 20 min after tourniquet release. We are not aware of studies that reported long-term effects of temporary tourniquet application on knee ST.
Monitoring clinical status by ST is not a new concept. For example, monitoring foot ST has been included in the evidenced-based guidelines for prevention of diabetic foot ulcers by the International Working Group on the Diabetic Foot34. More recently, Ghosh et al. reported that monthly monitoring of foot ST may predict recurrence of diabetic foot ulcers35. Other medical applications of ST include monitoring skin flap viability and depth of burn wounds36.
Smartphone-based applications for monitoring patient condition post-arthroplasties are already available, and information from biosensors including infrared thermometers or thermal imaging cameras can be integrated easily. Measuring ST at home on a regular basis can detect possible deviations or irregularities that may provide important information of relevance for early diagnosis of evolving pathologies such as PJI.
Finally, the usefulness of skin temperature measurements for diagnosis of PJI relies on its ability to differentiate between normal and abnormal levels. After careful consideration, and as recommended by the GRADE workgroup criteria for certainty of evidence37, we estimate that the accumulated body of evidence presented in this meta-analysis is of high quality and is sufficient to represent the normal, temporal changes in ST following TKA in patients without complications.
Limitations
In some studies, there were variations in patient posture, acclimatization, and region of interest (ROI). Nonetheless, they are of limited effect on outcomes since the operated and non-operated sides were subjected to similar conditions. Four studies included in this systematic-review did not report whether a tourniquet was used. Further studies are required to determine if peri-procedural tourniquet application has long-term effect on knee ST. Each study collected thermal information at different follow-up time-points which precluded a “paired” comparison. This required limiting the analysis to non-paired calculations which are more conservative.
Conclusions
This systematic review and meta-analysis has permitted characterization of the temporal changes in ST in patients with uncomplicated recovery following TKA. Further studies of changes in skin temparature in patients with PJI at different time points post-TKA, with correlative clinical and microbiological data, will provide important additional information related to the diagnostic usefulness of this objective, non-invasive thermal imaging modality.
Methods
Guidelines and Registration
This systematic-review and meta-analysis was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines23. The review question is stated according to PICO principles: Participants = patients with uncomplicated recovery following TKA; Intervention = thermography; Comparator = time points; Outcome = pooled weighted means of the difference between the operated and the non-operated knees (ΔST). The review protocol was registered prospectively in the international prospective register of systematic reviews, PROSPERO (CRD42021269864). The PRISMA-P checklist appears in the Supplementary file online.
Search strategy
The searches were conducted using PubMed and EMBASE. The search targeted studies reporting anterior knee skin temperature of patients before and after unilateral TKA, without date or language restrictions, up to May 24, 2021. The search protocol was defined using the following keywords: ‘total knee arthroplasty’ or ‘total knee replacement’ and ‘thermography’ or ‘infra-red thermometry’ or ‘infrared imaging’ or ‘thermal imaging’ or ‘thermogram’ or ‘thermographic imaging.’ The specific search protocol for each database is found in the Supplementary Table S1, online. Additional references were identified through manual search in the included manuscripts as well as in relevant reviews and websites.
Study eligibility
Inclusion Criteria: (1) adults before and after unilateral TKA; (2) uncomplicated recovery; (3) passive thermal measurements not following any physical activity or procedure other than TKA; (43) availability of data on the differences between operated and non-operated knee. Exclusion Criteria: (1) interventions other than TKA (i.e. injections, physical activity, other knee surgeries); (2) active thermal measurements (response to cryotherapy, exercise, heating) (3) patients not adults; (4) non-human studies; (5) language other than English; (6) groups treated with interventions that could affect inflammation; (7) studies with data of only the operated knee.
Screening, study selection, and data extraction
The screening was performed by two reviewers (LG and OH) independently using the blind screening mode of RYYAN-QCRI software38. Studies were screened initially by title and abstract. The full text of studies was screened again according to eligibility criteria. Disagreements were settled by discussion or in consultation with a third author (SDG). The list of excluded studies appears in Supplementary Table S2, online.
Data extraction included: Study Descriptors—First author, year of publication, country of origin, data collection period; Study Population—sample size, male:female counts, age; TKA Procedure—surgical approach, use of tourniquet, type of prosthesis, whether the patella was replaced (a metal replacement may affect skin temperature), dates of follow up visits; Skin Temperature Measurement- details of measuring device, method, location (ROI), imaging setup, acclimatization period. Missing methodological information was completed by contacting corresponding authors. A difference in skin temperature between the operated and non-operated knees of 0.5 °C is considered the minimum clinically important difference in ST for the anterior knee24.
Study appraisal was conducted according to the quality of measurement methodology26 and included equipment resolution, environmental conditions during data collection, and ROI. Accordingly, the quality of each study was scored as good, fair, or poor considering availability of information on patient position, skin exposure time, or ROI (Table 2). None of the articles included in this meta-analysis was graded as ‘poor’.
Data analysis and statistics
The primary study outcome for the quantitative analysis of ΔST was the pooled, weighted mean with 95% confidence intervals (CIs) as calculated by meta-analysis with a random-effect model. Meta-analyses were performed separately for each time point (i.e. pre-TKA and post-TKA at 1 day; 1,2, and 6 weeks; and at 3, 6, and 12 months). Heterogeneity between studies was assessed with I2 statistics (p < 0.1 and/or I2 > 50% indicated significant heterogeneity). Publication bias (‘file drawer bias’) was assessed by Begg’s Funnel-Plot and pseudo-95%-confidence limits. Egger’s test was used to determine bias. Comparisons between time points were performed using 1-way ANOVA with Tukey as the post-hoc test. Missing standard deviations were imputed by weighted average at each time point. When data were reported separately for the operated and non-operated knee, the average difference was calculated, and the SD was pooled. The Comprehensive Meta-Analysis (CMA) Version-3 software (Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. Biostat, Englewood, NJ 2013) and SYSTAT, version 13 (Systat Software, Chicago, USA) were used as appropriate for analyzing the data.
Data availability
All data can be found in the tables supplied as part of the manuscript.
References
Kurtz, S., Ong, K., Lau, E., Mowat, F. & Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am. 89, 780–785. https://doi.org/10.2106/JBJS.F.00222 (2007).
Izakovicova, P., Borens, O. & Trampuz, A. Periprosthetic joint infection: Current concepts and outlook. EFORT Open Rev. 4, 482–494 (2019).
Tubb, C. C., Polkowksi, G. G. & Krause, B. Diagnosis and prevention of periprosthetic joint infections. J. Am. Acad. Orthop. Surg. 28, e340–e348. https://doi.org/10.5435/JAAOS-D-19-00405 (2020).
McNally, M. et al. The EBJIS definition of periprosthetic joint infection. Bone Joint J. 103-B, 18–25. https://doi.org/10.1302/0301-620X.103B1.BJJ-2020-1381.R1 (2021).
Kumar, P. et al. Applications of thermal imaging with infrared thermography in orthopaedics. J. Clin. Orthop. Trauma 24, 101722. https://doi.org/10.1016/j.jcot.2021.101722 (2022).
Gavish, L. et al. Microcirculatory response to photobiomodulation-why some respond and others do not: A randomized controlled study. Lasers Surg. Med. 52, 863–872. https://doi.org/10.1002/lsm.23225 (2020).
Fokam, D. & Lehmann, C. Clinical assessment of arthritic knee pain by infrared thermography. J. Basic Clin. Physiol. Pharmacol. https://doi.org/10.1515/jbcpp-2017-0218 (2018).
Alfieri, F. M., Vargas, E. S. N. C. O., Dos Santos, A. C. A. & Battistella, L. R. Cutaneous temperature and pressure pain threshold in individuals with knee osteoarthritis. Reumatologia 58, 272–276. https://doi.org/10.5114/reum.2020.100195 (2020).
Scheidt, S. et al. A systematic review on the value of infrared thermography in the early detection of periprosthetic joint infections. Z. Orthop. Unfall. 158, 397–405. https://doi.org/10.1055/a-0969-8675 (2020).
Mehra, A., Langkamer, V. G., Day, A., Harris, S. & Spencer, R. F. C reactive protein and skin temperature post total knee replacement. Knee 12, 297–300. https://doi.org/10.1016/j.knee.2004.09.005 (2005).
Parvizi, J. et al. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J. Arthroplasty 33, 1309-1314 e1302. https://doi.org/10.1016/j.arth.2018.02.078 (2018).
Haidar, S. G., Charity, R. M., Bassi, R. S., Nicolai, P. & Singh, B. K. Knee skin temperature following uncomplicated total knee replacement. Knee 13, 422–426. https://doi.org/10.1016/j.knee.2006.08.003 (2006).
Martin, F. et al. Antiinflammatory effect of peripheral nerve blocks after knee surgery: Clinical and biologic evaluation. Anesthesiology 109, 484–490. https://doi.org/10.1097/ALN.0b013e318182c2a1 (2008).
Honsawek, S. et al. Relationship of serum IL-6, C-reactive protein, erythrocyte sedimentation rate, and knee skin temperature after total knee arthroplasty: a prospective study. Int. Orthop. 35, 31–35. https://doi.org/10.1007/s00264-010-0973-0 (2011).
Romanò, C. L., Romanò, D., Dell’Oro, F., Logoluso, N. & Drago, L. Healing of surgical site after total hip and knee replacements show similar telethermographic patterns. J. Orthop. Traumatol. 12, 81–86. https://doi.org/10.1007/s10195-011-0135-1 (2011).
Mumingjiang, Y., Zhou, X. D. & He, R. X. Value of knee skin temperature measured by infrared thermography and soluble intercellular adhesion molecule-1 in the diagnosis of peri-prosthetic knee infection in chinese individuals following total knee arthroplasty. Chin. Med. J. 127, 3105–3109. https://doi.org/10.3760/cma.j.issn.0366-6999.20140482 (2014).
van Hove, R. P., Brohet, R. M., van Royen, B. J. & Nolte, P. A. No clinical benefit of titanium nitride coating in cementless mobile-bearing total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 23, 1833–1840. https://doi.org/10.1007/s00167-014-3359-9 (2015).
Zeng, Y. et al. Differential knee skin temperature following total knee arthroplasty and its relationship with serum indices and outcome: A prospective study. J. Int. Med. Res. 44, 1023–1033. https://doi.org/10.1177/0300060516655237 (2016).
Xu, X. et al. Effect of celecoxib on surgical site inflammation after total knee arthroplasty: A randomized controlled study. Med. Princ. Pract. 27, 481–488. https://doi.org/10.1159/000492922 (2018).
Lin, S. J. et al. Temporal change of interleukin-6, C-reactive protein, and skin temperature after total knee arthroplasty using triclosan-coated sutures. Biomed. Res. Int. 2018, 9136208. https://doi.org/10.1155/2018/9136208 (2018).
Romanò, C. L., Logoluso, N., Dell’Oro, F., Elia, A. & Drago, L. Telethermographic findings after uncomplicated and septic total knee replacement. Knee 19, 193–197. https://doi.org/10.1016/j.knee.2011.02.012 (2012).
Romanò, C. L. et al. Value of digital telethermography for the diagnosis of septic knee prosthesis: A prospective cohort study. BMC Musculoskelet. Disord. 14, 7. https://doi.org/10.1186/1471-2474-14-7 (2013).
Martinez, V., Fletcher, D., Bouhassira, D., Sessler, D. I. & Chauvin, M. The evolution of primary hyperalgesia in orthopedic surgery: Quantitative sensory testing and clinical evaluation before and after total knee arthroplasty. Anesth. Analg. 105, 815–821. https://doi.org/10.1213/01.ane.0000278091.29062.63 (2007).
Selfe, J., Whitaker, J. & Hardaker, N. A narrative literature review identifying the minimum clinically important difference for skin temperature asymmetry at the knee. Thermol. Int. 18, 41–44 (2008).
Hendiani, J. A. et al. Mechanical sensation and pain thresholds in patients with chronic arthropathies. J. Pain 4, 203–211. https://doi.org/10.1016/s1526-5900(03)00557-1 (2003).
Ammer, K. Temperature of the human knee–a review. Thermol. Int. 22, 137–151 (2012).
Umapathy, S., Thulasi, R., Gupta, N. & Sivanadhan, S. Thermography and colour Doppler ultrasound: A potential complementary diagnostic tool in evaluation of rheumatoid arthritis in the knee region. Biomed. Tech. (Berl) 65, 289–299. https://doi.org/10.1515/bmt-2019-0051 (2020).
Hasegawa, M., Kawamura, G., Wakabayashi, H., Sudo, A. & Uchida, A. Changes to patellar blood flow after minimally invasive total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 17, 1195–1198. https://doi.org/10.1007/s00167-009-0834-9 (2009).
Lahiri, B. B., Bagavathiappan, S., Jayakumar, T. & Philip, J. Medical applications of infrared thermography: A review. Infrared Phys. Technol. 55, 221–235. https://doi.org/10.1016/j.infrared.2012.03.007 (2012).
Yang, H., Park, H., Lim, C., Park, S. & Lee, K. Infrared thermal imaging in patients with medial collateral ligament injury of the knee–a retrospective study. J. Pharm. 17, 50–54. https://doi.org/10.3831/KPI.2014.17.036 (2014).
Johnson, J. M. & Kellogg, D. L. Jr. Local thermal control of the human cutaneous circulation. J. Appl. Physiol. 1985(109), 1229–1238. https://doi.org/10.1152/japplphysiol.00407.2010 (2010).
Marins, J. C. B. et al. Time required to stabilize thermographic images at rest. Infrared Phys. Technol. 65, 30–35. https://doi.org/10.1016/j.infrared.2014.02.008 (2014).
Alisi, M. et al. Thermographic assessment of reperfusion profile following using a tourniquet in total knee arthroplasty: A prospective observational study. Med. Devices (Auckl) 14, 133–139. https://doi.org/10.2147/mder.S300726 (2021).
Bus, S. A. et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab. Res. Rev. 36(Suppl1), e3269. https://doi.org/10.1002/dmrr.3269 (2020).
Ghosh, A., Ray, S., Garg, M. K., Chowdhury, S. & Mukhopadhyay, S. The role of infrared dermal thermometry in the management of neuropathic diabetic foot ulcers. Diabet. Med. 38, e14368. https://doi.org/10.1111/dme.14368 (2021).
Ammer, K. Employment of FLIR ONE Infrared cameras in medicine–a literature overview. Thermol. Int. 30, 128–145 (2020).
Balshem, H. et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 64, 401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015 (2011).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5, 210. https://doi.org/10.1186/s13643-016-0384-4 (2016).
Acknowledgements
We thank Tomer Ben-Shushan, Reference Librarian, The Muriel and Philip Berman Medical Library, The Hebrew University of Jerusalem. These studies were supported in part by The Stuart Roden Family Research Fund, London, UK; The Saul and Joyce Brandman Fund for Cardiovascular Research, The Alexander Grass Family Research Fund, The Dr. Bruce and Baila Waldholtz Research Fund, and The Dr. Martin and Grace Rosman Research Fund, Faculty of Medicine, The Hebrew University of Jerusalem, Israel. This study was chosen for the EFORT Jacques Duparc poster award at the 23rd annual EFORT congress, June 22-24, 2022, Lisbon, Portugal.
Author information
Authors and Affiliations
Contributions
All authors critically reviewed the manuscript for important intellectual content, approved the final manuscript as submitted and agree to be accountable for all aspects of the work. Specifically: L.G. contributed to the conception and design of the study, collected the data, performed the screening and data-extraction, conducted the data analysis, was involved in the interpretation, and drafted the initial manuscript. L.K. contributed to the conception of the study, assisted in data extraction, and was involved in the interpretation of the clinical data. G.R. contributed to the conception of the study, assisted in data extraction, and was involved in the interpretation of the clinical data. S.D.G. contributed to the conception and design of the study, was part of the screening, involved in the data interpretation, and drafted the initial manuscript. O.H. contributed to the conception and design of the study, collected the data, performed the screening and data-extraction, and was involved in the interpretation of the thermal data.
Corresponding author
Ethics declarations
Competing interests
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gavish, L., Kandel, L., Rivkin, G. et al. Natural history of changes in knee skin temperature following total knee arthroplasty: a systematic review and meta-analysis. Sci Rep 13, 6810 (2023). https://doi.org/10.1038/s41598-023-33556-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-33556-7
- Springer Nature Limited