Abstract
This study comprehensively investigated clinical outcomes associated with renin angiotensin system inhibitor-based dual antihypertensive regimens in non-dialysis chronic kidney disease (CKD) patients. Keyword searches of databases were performed per PRISMA-NMA guidelines. Frequentist network meta-analysis were conducted with 16 head-to-head randomized controlled trials. The effect sizes of dichotomous and continuous variables were estimated with odds ratio (OR) and standard mean differences (SMD), respectively. The protocol is registered in PROSPERO (CRD42022365927). Dual antihypertensive regimens with combination of angiotensin receptor blockers (ARB) and calcium channel blockers (CCB) demonstrated substantially reduced odd of major cardiovascular disease (CVD) events over other regimens including angiotensin converting enzyme inhibitor (ACEI) monotherapy (OR 3.19) and ARB monotherapy (OR 2.64). Most significant reductions in systolic (SBP) and diastolic blood pressure (DBP) were observed with ARB-based CCB dual regimen over ACEI monotherapy (SMD 17.60 SBP and 9.40 for DBP), ACEI-based CCB regimen (SMD 12.90 for SBP and 9.90 for DBP), and ARB monotherapy (SMD 13.20 for SBP and 5.00 for DBP). However, insignificant differences were noticed for the odds of hyperkalemia, end stage renal disease progression, and all-cause mortality. ARB-based CCB regimen has the greatest benefits on BP reduction as well as major CVD risks in non-dialysis CKD patients.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a progressive disorder characterized by renal insufficiency with an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2 for more than 3 months, responsible for 1.2 million mortalities1,2,3. Among numerous comorbidities, hypertension is one of the most common etiologic factors for CKD, and the prevalence increases with declining renal function, accounting for 60 to 90% of CKD patients4. Hypertension is considered as a dominant attributed comorbidity for end stage renal disease (ESRD), defined as eGFR < 15 mL/min/1.73 m2 or renal failure, as blood pressure (BP) increases with worsening renal insufficiency, which subsequently accelerates the disease progression5. Moreover, uncontrolled hypertension increases the risks of significant adverse cardiovascular outcomes such as myocardial infarction (MI), stroke, or sudden cardiac death, and CVD is designated for the leading cause of mortality in CKD patients indeed6. Thus, maintaining target BP goals in CKD patients is critical to improve clinical prognoses.
The updated 2021 Kidney Disease Improving Global Outcomes (KDIGO) guideline for the management of blood pressure in CKD recommends renin-angiotensin system inhibitors (RASi), either angiotensin converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB), as the first-line antihypertensive agents for non-dialysis CKD patients with elevated BP to inhibit markedly increased renin angiotensin aldosterone system (RAAS) activity induced by renal insufficiency1,4,7. According to the previous studies, both ACEI and ARB not only delayed CKD progression but also reduced CVD events including heart failure and cardiac death in patients with renal insufficiency8. However, most CKD patients require additional antihypertensive agents to RASi to maintain optimal BP as the disease progresses. According to a nationwide population study9, more than 50% of CKD patients were prescribed with at least 2 antihypertensive agents to manage hypertension. Although the current guidelines suggest dual antihypertensive treatment with RASi, either ACEIs or ARBs, in CKD patients with uncontrolled BP by the primary antihypertensive agent, the valid evidences on the optimal selection of add-on agent for RASi-based dual hypertension treatment regimens in CKD patients are currently limited1,10, and considering increased risk of adverse events (AE) secondary to substantial changes in pharmacokinetic and pharmacodynamic characteristics, there is an urgent need for the establishment of evidence-based guidance on optimal pharmacotherapy in patients with renal insufficiency11. Nevertheless, as CKD patients are considered as vulnerable patient populations, the clinical studies to support the selection of optimal RASi-based dual antihypertensive regimens in patients with renal insufficiency are currently lacking, consequently making clinical decision more perplex12. Therefore, this study aims to comprehensively assess clinical outcomes of diverse RASi-based dual antihypertensive regimens in non-dialysis CKD patients by conducting pair-wise comparisons utilizing Frequentist network meta-analysis methods to evaluate clinical benefits of each RASi-based dual antihypertensive regimen, thereby providing supporting evidences on the optimal RASi-based dual antihypertensive regimens in non-dialysis CKD patients to enhance prognosis.
Results
Study selection and characteristics
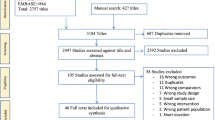
The primary database search and study selection process per PRISMA and PRISMA-NMA guidelines are described in Fig. 1. The primary database search yielded 2.751 studies, and 134 studies were eligible for full-text review after exclusion of duplicates, irrelevant studies, abstracts, non-human study, and studies published in languages other than English. After the full-text review, a total of 16 head-to-head randomized controlled trials were included for quantitative network meta-analysis. The lists and characteristics of the eligible studies for network meta-analysis are summarized in Table 1. Twelve types of antihypertensive therapy regimens in 4,677 patients were included in the analysis: ACEI monotherapy13,14,15,16,17,18,19,20,21, ARB monotherapy18,21,22,23,24,25, CCB monotherapy13,14, ARB and ACEI combination15,16,17,18,19,21, ARB and CCB combination24,26,27, ARB and thiazide combination (TZD)23,26, ARB and renin inhibitor (RI) combination22,25, ACEI-based CCB combination13,14,20,28, ACEI and SPR combination16,20, ACEI and TZD combination28, CCB and beta-blocker combination (BB)27, and CCB and TZD combination27. The network plot of eligible studies is described in Fig. 2. The most studied head-to-head trial pair comparison was ARB and ACEI combination therapy versus ACEI monotherapy (8 studies). The results of study quality assessment are organized in Supplementary Figure S1. Majority of included studies (13 studies) had low risk of bias, suggesting high quality of the evidence. The quality of generated evidences of each outcome based on GRADE approach is described in Fig. 3. The possibility of publication bias may present only in hyperkalemia risk based on the results of Egger’s test (P values < 0.05). All study outcomes had I2 index < 50% and P values > 0.05 for Cochran Q statistics, implying low risk of heterogeneity and inconsistency.
Study outcomes from network meta-analysis
The odd of major CVD events was significantly higher in ACEI monotherapy (OR 3.19; 95% CI 1.25–8.17, p = 0.0156), ACEI and SPR combination (OR 14.62; 95% CI 2.56- 83.49, P = 0.0026), ARB monotherapy (OR 2.64; 95% CI 1.18–5.87 P = 0.0177), and ARB and ACEI combination (OR 3.31; 95% CI 1.31–8.41, P = 0.0117) than ARB-based CCB combination therapy (Fig. 4a and Table 2). Similar odds of major CVD event were noticed in other RASi-based dual antihypertensive regimens including ACEI-based TZD combination and ACEI-based CCB combination when compared to ARB-based CCB combination. However, ACEI-based SPR combination therapy demonstrated markedly higher odds of major CVD events than ARB monotherapy, ARB-based CCB combination regimen, CCB monotherapy, CCB and BB combination and CCB and TZD combination (P < 0.05) (Table 2). ARB-based CCB combination therapy demonstrated substantially greater reduction in SBP than ACEI monotherapy (SMD 17.60; 95% CI 6.96–28.23; P = 0.0035), ACEI and CCB combination (SMD 12.90; 95% CI 1.44–24.35; P = 0.0499), ARB monotherapy (SMD 13.20; 95% CI 6.44–19.96; P = 0.0012), ARB and ACEI combination (SMD 15.79; 95% CI 5.22–26.36; P = 0.0086) and CCB monotherapy (SMD 18.40; 95% CI 7.40–29.39; P = 0.0039) (Fig. 4b and Table 3). Significantly lowered DBP was also observed in ARB-based CCB combination regimen when compared to ACEI monotherapy (SMD 9.40; 95% CI 2.95- 15.86; P = 0.0043), ACEI-based CCB combination regimen (SMD 9.90; 95% CI 2.59–17.22, P = 0.0080), ARB monotherapy (SMD 5.00; 95% CI 0.27–9.73; P = 0.0382), ARB and ACEI combination (SMD 8.30; 95% CI 1.91–14.69; P = 0.109) and CCB monotherapy (SMD 11.10; 95% CI 4.20–18.01; P = 0.0016) (Fig. 4c and Table 4). The BP control capacity was similar between ARB-based CCB combination and ARB-based TZD combination. The odd of hyperkalemia is statistically insignificant among diverse RASi-based antihypertensive treatment when referenced with ARB-based CCB combination therapy (Fig. 5a and Table 5). However, the indirect comparison analysis revealed substantially higher odd of hyperkalemia with ACEI-based SPR combination regimens than CCB monotherapy (p < 0.05) (Table 5). The odds of ESRD diagnosis and all-cause mortality were insignificant among antihypertensive treatment regimens (Fig. 5b,c and Tables 6, 7). The SUCRA analysis on ranking of antihypertensive treatment regimens for each outcome is summarized in Table 8. ARB-based CCB combination regimen demonstrated relatively better prognosis for major CVD events and BP controls among antihypertensive treatment regimens.
Discussion
Hypertension is the most prevalent comorbidity etiologic for CKD diagnosis and progression4. Uncontrolled hypertension not only increases the risk of major CVD events such as MI, stroke and cardiac death but also predisposes patients to the elevated risk of ESRD diagnosis, subsequently elevating the medication burdens associated with ESRD complications such as anemia, mineral bone disorder, electrolyte imbalance and uremia29. Nonetheless, implementation of optimal antihypertensive pharmacotherapy in CKD patients is still challenging due to limited number of evidences. Hence, this study evaluated the clinical outcomes associated with diverse RASi-based antihypertensive regimens in non-dialysis CKD patients to establish evidences on the optimal antihypertensive pharmacotherapy.
According to a previous network meta-analysis evaluating clinical outcomes of diverse antihypertensive monotherapy regimens, ACEI monotherapy has superior benefits on prevention of kidney disease and cardiovascular death over other regimens including ARB monotherapy, BB monotherapy and CCB monotherapy in non-dialysis CKD patients30. In this study, however, the risk of major CVD events was considerably elevated with RASi monotherapy, implying that either ACEI or ARB monotherapy may not be sufficient to control BP and major CVD risk in many CKD patients. The previous studies evaluating prescribing patterns of antihypertensive agents indeed revealed that more than 70% of CKD patients were prescribed at least 2 antihypertensives9,31. The types of dual antihypertensive regimens, however, were variable in these studies due to the obscurity on the optimal antihypertensive combination regimens in non-dialysis CKD patients9,31. Based on the treatment ranking results from SUCRA, ARB-based CCB combination had the lowest risk of major CVD events, followed by ACEI-based CCB combination and ACEI-based TZD combination (Table 3), and this may be correlated with the greatest BP reduction effects. Although this study demonstrated comparable reduction of major CVD risk and BP between RASi-based TZD combination and ARB-based CCB combination, the evidences suggest superior benefits of RASi-based CCB on prevention of cardiovascular death over RASi-based TZD in hypertensive patients with high risk for major CVD events, indicating potential advantage of ARB-based CCB combination regimen in non-dialysis CKD patients32. Moreover, considering that the diuretic efficacy of TZD worsens with decreased renal function33, RASi-based TZD combination may not be a promising choice for in patients with advanced CKD.
One of the concerns associated with RASi treatment is elevated risk of hyperkalemia1,10. Hyperkalemia induces cardiac arrhythmia, which consequently increases the risks of hospitalization and sudden cardiac death10. Both JNC8 and KDIGO guidelines restrict any combination of ACEI, ARB and direct RI in non-dialysis CKD patients based on the strong evidences of increased harm from hyperkalemia and acute kidney injury over cardiovascular and renal benefits1,10. Nonetheless, no significant difference in the risk of hyperkalemia was noticed among RASi-based antihypertensive treatment regimens, except RASi-based SPR combination treatment, when compared to the combination regimen of ARB with CCB. Interestingly, similar hyperkalemia risk was observed in concomitant administration of ACEI and ARB combination (OR 0.38; 95% CI 0.03–4.94) and non-RASi-based antihypertensive treatment including CCB monotherapy (OR 0.06; 95% CI 0.00–2.26), CCB and BB combination (OR 0.84; 95% CI 0.22–3.17) and CCB and TZD combination (OR 1.28; 95% CI 0.37- 4.42) in this study. Although the evident mechanism for similar hyperkalemia risks regardless of the diverse combination of antihypertensive agents is yet to be determined, disease-specific factor may have superior influences on hyperkalemia risk over RASi use in CKD patients34. Renal insufficiency itself is a compelling risk factor of hyperkalemia as the hyperkalemia incidence and severity increase with CKD progression, and a previous study revealed that the degree of renal insufficiency manifested by elevated serum creatinine level was the strongest positive correlation factor with serum potassium over other contributing factors such as diabetes, RASi use, and age35. However, the scarcity of evidences in CKD patients may hinder investigation of evident hyperkalemia risk from pharmacotherapy notwithstanding renal function. Hence, further studies investigating hyperkalemia risk associated with antihypertensive combination regimens including RASi-based dual antihypertensive treatment in CKD patients are warranted to improve patient prognosis.
The risk of ESRD diagnosis was statistically insignificant among antihypertensive treatment regimens. As CKD being a progressive chronic disorder, disease progression to ESRD may inevitable in many patients with the estimated probability of 52% in 10 years36. However, the time to ESRD diagnosis may be different as numerous patient- and disease-specific factors play crucial roles in ESRD progressions, and the studies suggest that those with younger age, female sex, diabetes, or dyslipidemia are more likely to have accelerated progression to ESRD37,38. Considering the substantial clinical adverse outcomes in ESRD patients, delaying ESRD progression itself may be acknowledged as valuable clinical benefits in CKD patients39. Thus, further studies investigating the impact of various antihypertensive treatment regimens on the time to ESRD diagnosis are warranted to ensure favorable prognoses in CKD patients.
Diabetes is also a major etiologic comorbidity for CKD diagnosis and progression, and BP management in CKD patients with diabetes is also pivotal as more than 80% of these patients are diagnosed with hypertension40. The guidelines recommend RASi-based antihypertensive treatment regimens regardless of diabetes status1,10. However, despite the significant influence of diabetes on accelerated disease progression in CKD patients, the studies investigating clinical outcomes of diverse antihypertensive treatment regimens are still limited38. Among 16 clinical trials included in this study, 9 clinical trials evaluated outcomes from 7 different antihypertensive regimen in CKD patients with diabetes: ACEI monotherapy, ARB monotherapy, ACEI-based spironolactone, ARB-based spironolactone, ARB and ACEI combination, and ARB-based renin inhibitor. The risk of major CVD events was substantially higher in ACEI + SPR (OR 5.53; 95% CI 1.05–29.19) when compared to ARB monotherapy (reference), the most prescribed antihypertensive regimen in Korea (Supplementary Figure S2)9,41. Meanwhile, the risk of hyperkalemia was similar among the treatment regimens when referenced with ARB monotherapy (Supplementary Figure S3). Nonetheless, considering that administration of RASi with spironolactone is rarely recommended in CKD patients, the only viable antihypertensive treatment regimens recommended by the current guidelines are ACEI monotherapy and ARB monotherapy in this analysis, implying the limited number of clinical trials in CKD patients with diabetes. Hence, further studies investigating clinical outcomes such as BP control and major CVD incidences associated different RASi-based antihypertensive treatment regimens in CKD patients with diabetes are required.
To the best of our knowledge, this is the first network meta-analysis investigating clinical outcomes of RASi-based dual antihypertensive regimens in non-dialysis CKD patients. We comprehensively compared cardiovascular outcomes including major CVD risks and BP controls as well as other clinical outcomes such as the risk of hyperkalemia, ESRD and all-cause mortality and demonstrated substantial clinical benefits from ARB-based CCB combination in non-dialysis CKD patients. However, considering more than 45% of advanced CKD patients discontinue RASi therapy within 1-year secondary to CKD progression, hospitalization for acute kidney injury, hyperkalemia, and the presence of multiple comorbidities, noticeably large number of CKD patients require antihypertensive agents other than RASi31,42. Thus, we additionally included 3 non-RASi-based antihypertensive regimens, CCB monotherapy, combination of CCB and BB, and combination of CCB and TZD, in the analysis based on prespecified PICOST-SD and demonstrated favorable effects of these regimens on major CVD risks. Nonetheless, the apparent benefits of non-RASi-based dual antihypertensive treatment should be thoroughly evaluated due to extremely limited evidences.
This study has several limitations. The included studies had differences in study designs, outcome measurements, and study follow-up durations, consequently increasing heterogeneity across the studies. Moreover, due to the vulnerability associated with CKD, small number of clinical trials as well as study participants may also play as limitation. However, considering that the majority of CKD patients are not eligible for the clinical trials, our study might contribute to the current body of literature on selection guidance on optimal hypertension pharmacotherapy in non-dialysis CKD patients to properly manage BP, thereby ameliorating the risk of major CVD events. Additionally, we included antihypertensive treatment regimens that are not currently recommended by the guidelines, combination of ACEI and ARB for example, to perform stepwise comparisons for network meta-analysis because more than half of the included studies had combination of ARB and ACEI regimen as study arm. Although exclusion of patients on impractical regimens may decrease the number of participants, this study manifested that combination of ARB and ACEI treatment attenuates the risk of major CVD despite comparable hyperkalemia risk with other antihypertensive regimens in non-dialysis CKD patients.
Conclusion
RASi-based dual antihypertensive regimen with ARB and CCB provided the most significant BP reduction as well as the lowest odds of major CVD events than other RASi-based antihypertensive regimens. However, the odds of hyperkalemia, ESRD progression, and all-cause mortality were statistically insignificant among various RASi-based antihypertensive regimens in CKD patients.
Methods
Data sources and search strategy
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 and PRISMA-Network Meta-Analyses (PRISMA-NMA) guidelines (Supplementary Table S1 and S243,44. Cochrane Library, MEDLINE (PubMed), and Scopus were searched from the inception to March 7 2023. The prespecified Medical Subject Headings (MeSH) and keywords were utilized for the initial database search: ‘angiotensin-converting enzyme inhibitors’, ‘angiotensin receptor antagonists’, ‘chronic kidney disease’, ‘hypertension’, and ‘renal insufficiency’. We also used ‘combin*’ as keyword to identify studies evaluating efficacy and safety of antihypertensive combination therapy containing either ACEI or ARB. The full database search terms and strategies are listed in Supplementary Table S3. The prespecified search filters were ‘clinical trials’, ‘humans’ and ‘English’. The manual search of the references from the eligible articles, otherwise referred to as snowball search, was performed to identify additional studies that meet eligible criteria. The protocol of this systematic review and network meta-analysis were registered in the International Prospective Register of Systematic Reviews (PROSPERO No. CRD42022365927).
Study selection and data extraction
The PICOST-SD (patient, intervention, control, outcomes, setting, time, and study design) is prespecified as follows: patients with HTN and non-dialysis CKD (stage 3 to 5), intervention with RASi-based (either ACEI or ARB) dual antihypertensive treatment, both inpatient and outpatients with treatment duration ≥ 24 weeks, and head-to-head RCT. Control was prespecified as any hypertensive treatment regimens including monotherapy and dual antihypertensive therapy that were directly compared with the intervention in the head-to-head RCT. Two reviewers independently screened titles/abstracts for eligibility of all identified studies from the initial database. The prespecified eligibility criteria of study inclusion included (1) head-to-head randomized controlled trials (RCT), (2) studies evaluating efficacy and safety of dual antihypertensive treatment regimens containing either ACEIs or ARBs as intervention in non-dialysis patients with CKD stage 3 to 5, (3) antihypertensive medications prescribed for ≥ 24 weeks, and (4) studies published in English. Duplicated studies, placebo-controlled RCTs, case reports, cross-over designed studies, observational studies, preclinical studies (in-vivo or in-vitro), abstracts including conference abstracts, study protocols, proceedings, reviews, and studies without available full-texts were excluded. Any disagreements on study eligibility were discussed until a consensus was reached. Cohen’s kappa statistic was calculated to determine interrater reliability for study selection and revealed kappa value of 0.88, implying strong level of agreement45.
The primary outcome of interest was major CVD events identified as MI, stroke, cardiovascular (CV) death, and CV-related hospitalization due to heart failure or angina as these have been identified as the most significant cause of mortality in CKD patient6. Moreover, other clinical outcomes including reduction in systolic blood pressure (SBP) and diastolic blood pressure (DBP), hyperkalemia, newly diagnosed ESRD (ESRD progression), and all-cause mortality, otherwise referred to as death of any cause were also investigated. Following information was extracted from the eligible study: study characteristics (author and year of publication), study population (number of patients and comorbidities), study intervention and comparators, and treatment duration. We extracted the number of patients experienced the outcomes of the study for dichotomous outcomes. For continuous outcomes such as SBP and DBP, we extracted the mean and standard deviation (SD) of each intervention.
Study quality assessments
Two reviewers assessed the quality of included studies, and any disagreements on study eligibility were resolved by the third reviewer (SJR). Risk of bias of included studies was assessed in accordance with Cochrane Risk of Bias version 2.0 (RoB 2) tool46, and each study were scored as low, some concerns (unclear), or high risk in the following domains: randomization process, deviations from the intended interventions, missing outcome data, measurements of the outcomes, and selection of the reported results. Any disagreements on the quality assessments were discussed until a consensus was reached. Studies were classified as low risk of bias if three or more domains were identified as low risk, whereas studies with at least two domains with high risk were classified as high-risk studies. The quality of evidences was assessed based on Cochrane GRADE guideline for each outcome47.
Statistical analysis and data synthesis
Pooled traditional pair-wise analyses on the outcomes were performed using ‘netmeta’ package in R (version 4.1.0.). Frequentist network meta-analyses were conducted to simultaneously compare the outcomes of interest by integrating direct and indirect effects of each RASi-based dual antihypertensive treatment regimen against a control group generated by the network meta-analysis in CKD patients48. ARB-based dual antihypertensive regimen with calcium channel blocker (CCB) was applied as the control antihypertensive treatment regimen for network analysis9,41. Dichotomous variables including major CVD events, ESRD diagnosis, all-cause mortality, and hyperkalemia were analyzed with a Mantel–Haenszel random effects model and odds ratio (OR) with 95% confidence intervals (CI) were calculated for each antihypertensive regimen. Changes in SBP and DBP were evaluated as weighted standard mean differences (SMD) with 95% CI. The heterogeneity and inconsistency of included studies were assessed with I2 index and Cochran’s Q, respectively. I2 index > 50% was considered as high heterogeneity and any P value < 0.05 was considered as significant inconsistency49. Egger’s test was performed to detect any publication of bias, and any P value > 0.05 implies a low risk of publication bias. The “netrank” function was utilized to assess the ranking of relative efficacy and safety of antihypertensive regimens in CKD patients, and the calculated P value was equivalent to the Surface Under the Cumulative Ranking (SCURA): the higher the P value, the better the rank of the antihypertensive treatment regimen50. The “netleague” function was utilized to create league tables for each outcome. All P values were calculated by two-sided tests, and statistical significance was determined by P values < 0.05.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Kidney Disease Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 Clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 99, S1–S87 (2021).
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733 (2020).
Meziri, F., Brahimi, F. Z. & Dorbane, C. Modulation of oxidative stress in chronic kidney disease patients with different physiopathological conditions. J. Complement. Med. Res. 13, 29–29 (2022).
Ku, E., Lee, B. J., Wei, J. & Weir, M. R. Hypertension in CKD: Core curriculum 2019. Am. J. Kidney Dis. 74, 120–131 (2019).
Judd, E. & Calhoun, D. A. Management of hypertension in CKD: beyond the guidelines. Adv. Chronic Kidney Dis. 22, 116–122 (2015).
Jankowski, J., Floege, J., Fliser, D., Böhm, M. & Marx, N. Cardiovascular disease in chronic kidney disease: Pathophysiological insights and therapeutic options. Circulation 143, 1157–1172 (2021).
Hameed, T. J., Ibraheem, M. M. & Mezher, M. A. Estimation of Renin enzyme activity and some biochemical parameters among chronic renal failure patients in Tikrit city. J. Popul. Ther. Clin. Pharmacol. 29, e134–e139 (2022).
Ku, E., McCulloch, C. E., Vittinghoff, E., Lin, F. & Johansen, K. L. Use of antihypertensive agents and association with risk of adverse outcomes in chronic kidney disease: Focus on angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. J. Am. Heart Assoc. 7, e009992 (2018).
Kim, H. C. et al. Korea hypertension fact sheet 2020: Analysis of nationwide population-based data. Clin. Hypertens. 27, 8 (2021).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311, 507–520. https://doi.org/10.1001/jama.2013.284427 (2014).
Lea-Henry, T. N., Carland, J. E., Stocker, S. L., Sevastos, J. & Roberts, D. M. Clinical pharmacokinetics in kidney disease: Fundamental principles. Clin. J. Am. Soc. Nephrol. 13, 1085–1095 (2018).
Pugh, D., Gallacher, P. J. & Dhaun, N. Management of hypertension in chronic kidney disease. Drugs 79, 365–379 (2019).
Herlitz, H. et al. The effects of an ACE inhibitor and a calcium antagonist on the progression of renal disease: The Nephros Study. Nephrol. Dial. Transplant. 16, 2158–2165 (2001).
MacGregor, M. S., Deighan, C. J., Rodger, R. S. & Boulton-Jones, J. M. A prospective open-label randomised trial of quinapril and/or amlodipine in progressive non-diabetic renal failure. Nephron. Clin. Pract. 101, c139-149 (2005).
Kanno, Y., Takenaka, T., Nakamura, T. & Suzuki, H. Add-on angiotensin receptor blocker in patients who have proteinuric chronic kidney diseases and are treated with angiotensin-converting enzyme inhibitors. Clin. J. Am. Soc. Nephrol. 1, 730–737 (2006).
Mehdi, U. F., Adams-Huet, B., Raskin, P., Vega, G. L. & Toto, R. D. Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy. J. Am. Soc. Nephrol. 20, 2641–2650 (2009).
Imai, E. et al. Effects of olmesartan on renal and cardiovascular outcomes in type 2 diabetes with overt nephropathy: a multicentre, randomised, placebo-controlled study. Diabetologia 54, 2978–2986 (2011).
Fernandez-Juarez, G. et al. Effect of dual blockade of the renin-angiotensin system on the progression of type 2 diabetic nephropathy: A randomized trial. Am. J. Kidney Dis. 61, 211–218 (2013).
Torres, V. E. et al. Angiotensin blockade in late autosomal dominant polycystic kidney disease. N. Engl. J. Med. 371, 2267–2276 (2014).
Van Buren, P. N., Adams-Huet, B., Nguyen, M., Molina, C. & Toto, R. D. Potassium handling with dual renin-angiotensin system inhibition in diabetic nephropathy. Clin. J. Am. Soc. Nephrol. 9, 295–301 (2014).
Saglimbene, V. et al. The long-term impact of renin-angiotensin system (RAS) inhibition on cardiorenal outcomes (LIRICO): A randomized, controlled trial. J. Am. Soc. Nephrol. 29, 2890–2899 (2018).
Parving, H. H., Persson, F., Lewis, J. B., Lewis, E. J. & Hollenberg, N. K. Aliskiren combined with losartan in type 2 diabetes and nephropathy. N. Engl. J. Med. 358, 2433–2446 (2008).
Abe, M., Okada, K., Maruyama, T. & Matsumoto, K. Antiproteinuric and blood pressure-lowering effects of a fixed-dose combination of losartan and hydrochlorothiazide in hypertensive patients with stage 3 chronic kidney disease. Pharmacotherapy 29, 1061–1072 (2009).
Kim-Mitsuyama, S. et al. Differential effectiveness of ARB plus CCB therapy and high-dose ARB therapy in high-risk elderly hypertensive patients: subanalysis of the OSCAR study. Hypertens. Res. 38, 199–207 (2015).
Soji, K. et al. Efficacy of add-on therapy of aliskiren to an angiotensin II receptor blocker on renal outcomes in advanced-stage chronic kidney disease: a prospective, randomized, open-label study. Clin. Exp. Nephrol. 19, 631–638 (2015).
Fogari, R. et al. Addition of manidipine improves the antiproteinuric effect of candesartan in hypertensive patients with type II diabetes and microalbuminuria. Am. J. Hypertens. 20, 1092–1096 (2007).
Rakugi, H. et al. Combination therapy for hypertension in patients with CKD: a subanalysis of the combination therapy of hypertension to prevent cardiovascular events trial. Hypertens. Res. 36, 947–958 (2013).
Bakris, G. L. et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): A prespecified secondary analysis of a randomised controlled trial. Lancet 375, 1173–1181 (2010).
Thomas, R., Kanso, A. & Sedor, J. R. Chronic kidney disease and its complications. Prim. Care 35, 329–344 (2008).
Zhang, Y. et al. ACE inhibitor benefit to kidney and cardiovascular outcomes for patients with non-dialysis chronic kidney disease stages 3–5: A network meta-analysis of randomised clinical trials. Drugs 80, 797–811 (2020).
Magvanjav, O. et al. Antihypertensive therapy prescribing patterns and correlates of blood pressure control among hypertensive patients with chronic kidney disease. J. Clin. Hypertens. (Greenwich) 21, 91–101 (2019).
Jamerson, K. et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N. Engl. J. Med. 359, 2417–2428 (2008).
Agarwal, R. & Sinha, A. D. Thiazide diuretics in advanced chronic kidney disease. J. Am. Soc. Hypertens. 6, 299–308 (2012).
Watanabe, R. Hyperkalemia in chronic kidney disease. Rev. Assoc. Med. Bras. (1992) 66Suppl 1, s31–s36 (2020).
Takaichi, K., Takemoto, F., Ubara, Y. & Mori, Y. Analysis of factors causing hyperkalemia. Intern. Med. 46, 823–829 (2007).
Cerqueira, D. C. et al. A predictive model of progression of CKD to ESRD in a predialysis pediatric interdisciplinary program. Clin. J. Am. Soc. Nephrol. 9, 728–735 (2014).
Hsu, C. Y., Iribarren, C., McCulloch, C. E., Darbinian, J. & Go, A. S. Risk factors for end-stage renal disease: 25-year follow-up. Arch. Intern Med. 169, 342–350 (2009).
Go, A. S. et al. Contemporary rates and predictors of fast progression of chronic kidney disease in adults with and without diabetes mellitus. BMC Nephrol. 19, 146 (2018).
Abbasi, M. A., Chertow, G. M. & Hall, Y. N. End-stage renal disease. BMJ Clin. Evid. 2010, 2002 (2010).
Ghaderian, S. B. & Beladi-Mousavi, S. S. The role of diabetes mellitus and hypertension in chronic kidney disease. J. Renal. Inj. Prev. 3, 109–110 (2014).
Park, S. & Shin, J. Asian management of hypertension: Current status, home blood pressure, and specific concerns in Korea. J. Clin. Hypertens. (Greenwich) 22, 493–496 (2020).
Burnier, M. Renin-angiotensin system blockade in advanced kidney disease: Stop or continue?. Kidney Med. 2, 231–234 (2020).
Hutton, B. et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern Med. 162, 777–784 (2015).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
McHugh, M. L. Interrater reliability: the kappa statistic. Biochem. Med. (Zagreb) 22, 276–282 (2012).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011).
Chapter 14: Completing 'Summary of findings' tables and grading the certainty of the evidence. Cochrane Training. https://training.cochrane.org/handbook/current/chapter-14#Figure15_1_b (2023).
Doing Meta-Analysis in R: A Hands on-Guide. Network Meta-Analysis. https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/netwma.html (2022).
Higgins, J. P. et al. Consistency and inconsistency in network meta-analysis: Concepts and models for multi-arm studies. Res. Synth. Methods 3, 98–110 (2012).
Rücker, G. & Schwarzer, G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med. Res. Methodol. 15, 58 (2015).
Funding
This research was supported by National Research Foundation (NRF) grant funded by Ministry of Science and ICT (No. 2020R1A2C1009224) and by Ministry of Education (NRF-2020R1A6A1A03043528 and NO. 2021R1I1A1A01044500) and was partially supported by a grant from Ministry of Food and Drug Safety (No. 21153MFDS601-1).
Author information
Authors and Affiliations
Contributions
Conceptualization: M.C., Y.J.C., S.J.R.; methodology: M.C., Y.J.C., S.J.R.; software; M.C., Y.J.C.; validation; C.Y.C., Y.J.C., S.J.R.: formal analysis; M.C., C.Y.C.: investigation; Y.J.C., S.J.R.; resources: Y.J.C., S.J.R.; data curation: M.C., C.Y.C., Y.J.C.; writing-original draft preparation; M.C., Y.J.C.; writing-review and editing; C.Y.C., S.J.R.; visualization: M.C., C.Y.C.; supervision Y.J.C., S.J.R.; project administration: S.J.R.; funding acquisition Y.J.C., S.J.R.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, M., Choi, CY., Choi, Y.J. et al. Clinical outcomes of renin angiotensin system inhibitor-based dual antihypertensive regimens in chronic kidney disease: a network meta-analysis. Sci Rep 13, 5727 (2023). https://doi.org/10.1038/s41598-023-32266-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32266-4
- Springer Nature Limited