Abstract
Despite standard treatment with systemic corticosteroids and/or antifungal triazoles, a substantial proportion of patients with allergic bronchopulmonary aspergillosis (ABPA) experience frequent relapses and require long-term treatment despite unfavorable adverse effects. We investigated the efficacy and safety of anti-interleukin (IL)-5/IL-5 receptor α chain (Rα) monoclonal antibodies (mAbs) in patients with ABPA complicated by asthma. ABPA cases treated with anti-IL-5/IL-5Rα mAbs were collected from 132 medical institutes in 2018 and published case reports in Japan. Clinical outcomes, laboratory and physiological data, and radiographic findings during 32 weeks before and after treatment were retrospectively evaluated. We analyzed 29 cases of ABPA: 20 treated with mepolizumab and nine with benralizumab. Treatment with anti-IL-5/IL-5Rα mAbs reduced the frequency of exacerbations (p = 0.03), decreased the dose of oral corticosteroids (p < 0.01), and improved pulmonary function (p = 0.01). Mucus plugs in the bronchi shrank or diminished in 18 patients (82%). Despite the clinical/radiographical improvement, serum levels of total IgE, the key biomarker for the pharmacological response in ABPA, were unchanged. Anti-IL-5/IL-5Rα mAbs that directly target eosinophils are promising candidates for the treatment of patients with ABPA, especially those with mucus plugs in the bronchi.
Similar content being viewed by others
Allergic bronchopulmonary aspergillosis (ABPA) is an allergic airway disease caused by Aspergillus fumigatus or other Aspergillus spp. that colonize the bronchi of patients with asthma or cystic fibrosis1,2. It is estimated that 2.5–5.0% of asthmatics worldwide develop ABPA3,4. It presents with various clinical symptoms, such as worsening asthmatic symptoms, cough, viscous sputum, and radiographic abnormalities in the chest, including pulmonary infiltrates and mucus plugs in the central bronchi. As the disease progresses, it is complicated by irreversible destruction of the airways, such as central bronchiectasis5, and secondary infection with Pseudomonas aeruginosa or non-tuberculous Mycobacterium6,7,8,9,10.
The standard treatment for ABPA is the administration of systemic corticosteroids and/or antifungal triazoles11. Medium-to-high doses of systemic corticosteroids can achieve disease remission in most cases; however, a substantial proportion of patients (13.5–45%) relapse and eventually become corticosteroid-dependent12,13. Long-term treatment with oral corticosteroids causes problems, especially in patients with comorbidities, such as diabetes mellitus or chronic infection in the lower airways. The use of triazole antifungal agents alone or in combination with systemic corticosteroids is another treatment option for ABPA14,15. However, post-treatment relapses are still common for this class of drugs, and long-term treatment may induce the emergence of drug-resistant fungi16. Therefore, the development of new treatment strategies with fewer adverse effects is warranted for ABPA. As ABPA is characterized by type 1 hypersensitivity to fungi and peripheral blood eosinophilia, biologics targeting type 2 inflammation, developed for the treatment of severe asthma, are expected to be potential therapeutic candidates for ABPA.
We and other researchers have previously reported the efficacy and safety of omalizumab for ABPA accompanied by asthma17,18,19,20. However, the effects of omalizumab on radiographic findings, such as mucus plugs in the bronchi, are marginal17. Furthermore, the dose of omalizumab is often suboptimal owing to markedly high levels of IgE in the serum, which is characteristic of ABPA17,20,21,22,23. However, a therapeutic strategy to suppress eosinophilic inflammation by targeting interleukin (IL)-5 or its receptor is not hindered by the magnitude of peripheral blood eosinophilia. Two types of antibodies target the IL-5/eosinophil pathway: anti-IL-5 monoclonal antibodies (mAbs), such as mepolizumab and reslizumab, and anti-IL-5 receptor-alpha chain (IL-5Rα) mAbs, such as benralizumab. Anti-IL-5/IL-5Rα mAbs has been shown to be effective against refractory eosinophilic lung diseases such as eosinophilic granulomatosis with polyangiitis, chronic eosinophilic pneumonia, and eosinophilic bronchiolitis24,25. Successful treatment outcomes in patients with ABPA have been demonstrated using these modalities10,26,27,28,29,30,31,32. Benralizumab exhibits more direct anti-eosinophilic effects via its antibody-dependent cell-mediated cytotoxicity on cells expressing IL-5Rα33, and some case reports have suggested better clinical outcomes in patients with asthma and ABPA treated with benralizumab than in those treated with mepolizumab34,35,36. However, most data on the efficacy and safety of anti-IL-5/IL-5Rα mAbs for patients with ABPA are based on case reports, except for one case series from Belgium26. Herein, we retrospectively analyzed the clinical outcomes, laboratory and physiological data, and radiographic findings of 29 Japanese patients with ABPA complicated by asthma who were treated with mepolizumab or benralizumab.
Results
Patient profiles
Twenty-nine patients with ABPM treated with anti-IL-5/IL-5Rα mAbs, including 22 (76%) women with a median age of 63 years, were registered from 15 clinical centers in Japan. All patients were positive for A. fumigatus-specific IgE and satisfied the diagnostic criteria for ABPA. The median score for the criteria was 8 (interquartile range [IQR], 5–10); all but one case had a score of 6 or higher, compatible with definite ABPA. The patient demographics and clinical characteristics are summarized in Table 1. All patients had a history of asthma, and there were no cases of cystic fibrosis. The median ages at the onset of ABPA and asthma were 56 and 36 years, respectively.
Twenty patients (69%) were treated with mepolizumab and nine with benralizumab. The age at asthma onset and peak peripheral eosinophil blood counts were higher in the mepolizumab group than in the benralizumab group; however, there were no apparent differences in other patient characteristics between the two treatment groups. The median duration of anti-IL-5/IL-5Rα mAb treatment was 76 weeks (81 and 55 weeks for mepolizumab and benralizumab, respectively). During the administration of anti-IL-5/IL-5Rα mAbs, 15 patients (52%) were on treatment with systemic corticosteroids and 10 (35%) with antifungal drugs. Seven patients had been previously treated with omalizumab, however, the control status of ABPA had worsened when treatment with anti-IL-5/IL-5Rα mAbs was introduced.
Clinical outcomes
There was a significant reduction in the exacerbation rate. During the first 32 weeks of anti-IL-5/IL-5Rα mAb treatment, there were 0.62 ± 0.78 exacerbations that required the administration or increase in the dose of systemic corticosteroids, which was 55% less frequent than the rate observed in the 32 weeks before treatment (1.38 ± 1.02, p = 0.03, Fig. 1A). Treatment with mepolizumab and benralizumab was similarly effective in decreasing the exacerbation rate (56 vs. 54%, respectively). The median percent forced expiratory volume in one second (FEV1) of predicted values increased from 87 to 92% with the anti-IL-5/IL-5Rα mAb treatment (p = 0.014, Fig. 1B). Of the 15 patients treated with oral corticosteroids, the maintenance dose was reduced in 11 patients (73%); the median dose of prednisolone (PSL) was reduced from 5 (IQR, 4–20) mg/day to 2 (IQR, 0–5) mg/day (p < 0.01, Fig. 1C). The median dose of PSL was reduced from 5 to 1 mg/day in the mepolizumab treatment group (p = 0.03) and from 15 to 2 mg/day in the benralizumab treatment group (p = 0.06).
Clinical outcomes of patients. Number of exacerbations within 32 weeks (A, n = 29), percent forced expiratory volume in one second (FEV1) of predicted values (B, n = 25), and dose of oral prednisolone (C, n = 15) before and after initiating treatment with mepolizumab or benralizumab in patients with allergic bronchopulmonary aspergillosis complicated by asthma. Treatment with mepolizumab or benralizumab significantly reduced exacerbation rate and oral corticosteroid dose, and improved pulmonary functions.
Biomarkers
The median peripheral eosinophil count at the start of mepolizumab treatment was 916 cells/µL, which decreased to 45 and 48 cells/µL at 16 and 32 weeks, respectively (p < 0.0001, Fig. 2A). The median peripheral eosinophil count at the start of benralizumab treatment was 245 cells/µL, which decreased to 0 cells/µL at 16 and 32 weeks (p < 0.004). Meanwhile, there was no significant change in the total IgE levels in the serum or fraction of exhaled nitric oxide (FENO) during the 32-week treatment period (Fig. 2B and C).
Biomarkers. Peripheral blood eosinophil counts (A, n = 29), serum IgE levels (B, n = 28), and fraction of exhaled nitric oxide (FENO) (C, n = 20) before and after initiating treatment with mepolizumab or benralizumab in patients with allergic bronchopulmonary aspergillosis complicated by asthma. Peripheral blood eosinophil counts were decreased significantly after treatment with mepolizumab or benralizumab, whereas there was no significant change in the serum IgE levels or FENO.
Radiographic findings
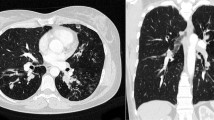
Mucus plugs were observed in the central bronchi on thoracic computed tomography (CT) in 22 patients (76%) treated with biologics: 17 of them were treated with mepolizumab and five with benralizumab. Improvement in mucus plugs after treatment was achieved in 18 (82%) patients, including 13 patients (76%) treated with mepolizumab and all patients (100%) treated with benralizumab. In the patients with an improvement of mucus plugs in the bronchi, there was a significantly larger reduction of peripheral blood eosinophil counts after anti-IL-5/IL-5Rα mAb treatment than in those without radiographical improvement (p < 0.001, Table 2), even when only the cases treated with mepolizumab were analyzed.
Switch treatment from mepolizumab to benralizumab
In this study, seven (35%) of the 20 patients originally treated with mepolizumab were switched at 40 weeks (median) to benralizumab treatment. The switch treatment was mostly performed to extend the intervals of treatment, but not for the failure to control respiratory symptoms due to ABPA and asthma with mepolizumab, except for one patient. However, residual mucus plugs in the bronchi were present in six patients despite mepolizumab treatment. After switching to benralizumab, symptoms further improved in two patients (29%); lung function improved in two patients (29%), and mucus plugs disappeared in four (67%) of six patients. No patient showed worsening ABPA or asthma control after switching to benralizumab.
Safety
There were no severe adverse events, including episodes of anaphylaxis, during treatment with anti-IL-5/IL-5Rα mAbs. One patient developed a temporary headache but continued to receive mepolizumab without recurrence of side effects.
Discussion
Mepolizumab and benralizumab were approved for the treatment of severe asthma in Japan in 2016 and 2018, respectively. In the present study, we retrospectively evaluated the efficacy and safety of these anti-IL-5/IL-5Rα mAbs in 29 Japanese patients with asthma-complicated ABPA. Mepolizumab, an anti-IL-5 mAb, and benralizumab, an anti-IL-5Rα mAb, were equally effective in reducing the exacerbation rates and doses of oral corticosteroids and improving lung function. Benralizumab may be more effective than mepolizumab in removing mucus plugs from the airways; residual mucus plugs during mepolizumab treatment disappeared in two-thirds of cases after switching to benralizumab. Among type 2 biomarkers, peripheral blood eosinophil counts decreased with these treatments, whereas serum IgE levels, a well-established biomarker for disease activity in ABPA, remained unchanged despite significant clinical improvements37,38. There was one case of a mild headache; however, no other serious adverse events, such as anaphylaxis, were observed.
Our data demonstrated that anti-IL-5/IL-5Rα mAbs not only improved clinical control but also radiographic abnormalities, such as mucus plugs in the bronchi. It is often difficult to evaluate whether biologics improve ABPA-specific pathology or underlying asthmatic condition. In contrast, mucus plugs in the central bronchi, often accompanied by central bronchiectasis and high-attenuation mucus, are specific for ABPA39,40. Although mucus plugs are also present in the bronchi of severe asthma, they are located in the distal airways and are not accompanied by bronchiectasis or high-attenuation mucus41. In the present study, mucus plugs reduced in size or disappeared after treatment with anti-IL-5/IL-5Rα mAbs in 82% of patients, suggesting that these biologics directly affect the pathophysiology of ABPA. Crosslinking of cysteine thiol groups in mucin partially mediated by eosinophil peroxidase has been demonstrated to be important for the formation of mucus plugs in the asthmatic airways41, and possibly in the airways of ABPA. In addition, we previously demonstrated that A. fumigatus can induce the release of extracellular traps from eosinophils, which are abundant in the mucus plugs of patients with ABPA42. Extracellular traps from activated eosinophils, composed of nuclear chromatin, form denser and more stable aggregates than neutrophil-derived extracellular traps and are also present in the mucus plugs of other eosinophilic diseases, such as chronic rhinosinusitis with nasal polyps and eosinophilic otitis media43. These data suggest that IL-5 and eosinophils are indispensable for the formation and maintenance of mucus plugs in patients with ABPA.
In the present study, 20 patients initially received mepolizumab, and nine received benralizumab. The clinical effects of mepolizumab and benralizumab on ABPA with respect to the control of daily symptoms or exacerbations were equivalent. However, we found a substantial difference between these biologics in their effects on mucus plugs. Although not statistically significant, benralizumab treatment resulted in a higher rate of disappearance of mucus plugs than mepolizumab treatment. Furthermore, the patients with radiographical improvement on mucus plugs demonstrated significantly larger reduction rate of peripheral blood eosinophil counts. In addition, a switch therapy from mepolizumab to benralizumab diminished the residual mucus plugs on treatment with mepolizumab in four patients, including the two patients we had previously reported34. The potent effect of benralizumab in suppressing mucus plug maintenance in the airways is likely related to its robust ability to deplete eosinophils in peripheral blood and tissues. In refractory eosinophilic asthma, bronchial subepithelial eosinophil counts after one year of treatment with mepolizumab were not statistically different from those in the placebo treatment group44. In contrast, subcutaneous benralizumab significantly reduced the airway mucosal eosinophil counts, with no eosinophils observed in the mucosal and submucosal tissues at day 84 in the benralizumab group45. These differences in the effects of mepolizumab and benralizumab in reducing the airway eosinophil numbers may have resulted in the difference in their effect on ABPA mucus plugs. Removal of eosinophilic mucus plugs by strict management of airway eosinophils with benralizumab prevents airway destruction and improves the long-term prognosis of patients with ABPA.
Various classes of biologics are effective in the treatment of ABPA. We and other researchers have demonstrated that omalizumab is effective in reducing exacerbations and the dose of oral corticosteroids17,20. Therefore, patients with ABPA refractory to standard treatment or those with comorbidities, such as diabetes mellitus and persistent airway infection, can benefit from omalizumab treatment. However, the dose of omalizumab needs to be adjusted based on the serum total IgE levels; therefore, sufficient neutralizing activity cannot be expected in cases with markedly high levels of serum IgE. In our previous study, 40% of patients with ABPA were treated with a suboptimal dose of omalizumab in Japan17. Seven patients who had been treated with omalizumab received anti-IL-5/IL-5Rα mAbs in this study, with some additional clinical benefits. Anti-IL-5/IL-5Rα mAbs may be more efficacious against mucus plugs than omalizumab. Radiographic improvement was observed in 50% of patients treated with omalizumab in our previous study17, whereas it was observed in 82% of patients treated with mepolizumab/benralizumab in this study. Interestingly, anti-IL-5/IL-5Rα mAb treatment was effective without a decrease in the total IgE levels in the serum, although serum IgE levels have been considered essential biomarkers reflecting the disease activity37,38. These findings suggest that both IgE and eosinophils are important therapeutic targets for ABPA, and eosinophil-targeted therapy may act directly on eosinophilic mucus plugs.
There have been case reports of ABPA treated with dupilumab, an anti-IL-4Rα mAb, which showed therapeutic effects on the symptoms and pulmonary function46,47,48. Some patients with ABPA refractory to treatment with omalizumab or mepolizumab responded to dupilumab treatment48,49,50; a clinical trial of dupilumab for ABPA is now underway. However, ABPA is often associated with marked eosinophilia, and there are concerns regarding the safety of dupilumab for ABPA treatment due to the systemic effects of eosinophilia. Post-treatment eosinophilia has been observed in clinical trials of dupilumab for atopic dermatitis51,52, and the development of symptomatic eosinophilia, such as eosinophilic pneumonia or eosinophilic granulomatosis with polyangiitis, after treatment with dupilumab has also been observed in patients with asthma or chronic rhinosinusitis with nasal polyps53,54,55,56,57. Therefore, appropriate biologics should be identified for each patient with ABPA in future studies.
Our study has some limitations. First, it was a retrospective study, which may have biased the patient selection criteria and overestimated the effects of anti-IL-5/IL-5Rα mAbs on ABPA. So far, no cases have been reported with premature discontinuation of anti-IL-5/IL-5Rα mAbs. Second, because anti-IL-5/IL-5Rα mAbs alone have not yet been approved for ABPA treatment, this study was limited to patients with comorbid asthma. A substantial proportion of the patients with ABPA lack specific predisposing factors, such as asthma or cystic fibrosis, and are termed as having ABPA sans asthma. ABPA sans asthma accounts for 7% of ABPA in India58 and 19% in Japan59. In addition, although efficacy and safety data were collected up to 32 weeks post-dose, long-term data are unknown, and there is a need for prospective long-term evaluation in the future.
Conclusion
In this study, anti-IL-5/IL-5Rα mAbs decreased the frequency of exacerbation, reduced the dose of oral corticosteroids, and improved lung function in patients with ABPA complicated by asthma, even in those refractory to omalizumab. There was no clear difference in the efficacy or safety between mepolizumab and benralizumab, although benralizumab may be more potent against mucus plugs. Therefore, anti-IL-5/IL-5Rα mAbs targeting eosinophils may be promising therapeutic candidates for patients with ABPA.
Methods
Subjects
In 2018, we sent questionnaires to 132 medical institutes that had participated in a nationwide survey on ABPM in 201359, asking about cases of ABPA with concomitant asthma treated with anti-IL-5/IL-5Rα mAbs. In addition, we asked the researchers in Japan who reported cases of ABPA treated with anti-IL-5/IL-5Rα mAbs to participate in this study27,28,29. Clinical data were retrospectively collected from medical records, additional questionnaires to physicians, and a case review meeting held in January 2019.
ABPA was diagnosed based on the modified Asano criteria39: (1) current or previous history of asthma or asthmatic symptoms, (2) peripheral blood eosinophilia (≥ 500 cells/mm3), (3) elevated total serum IgE levels (≥ 417 IU/mL), (4) immediate cutaneous hypersensitivity or specific IgE for A. fumigatus, (5) presence of precipitins or specific IgG for A. fumigatus, (6) growth of Aspergillus spp. in cultures of sputum or bronchial lavage fluid, (7) presence of fungal hyphae in bronchial mucus plugs, (8) central bronchiectasis on CT, (9) presence of mucus plugs in the central bronchi on CT/bronchoscopy or history of mucus plug expectoration, and (10) high attenuation mucus in the bronchi on CT. Patients who met six or more criteria were diagnosed with definite ABPA, and those who met five criteria were diagnosed as probable cases.
Ethics declarations
This study was approved by the Institutional Review Board for clinical research of the Tokai University Hospital (#18R-290 and #22R-161) and carried out according to the principles embodied in the Declaration of Helsinki of 1965, as revised in Brazil in 2013. The need for informed patient consent was waived by the Institutional Review Board in view of the anonymity of the data and the retrospective observational nature of the study.
Treatment effects and safety of anti-IL-5/IL-5Rα mAbs
Mepolizumab or benralizumab was administered subcutaneously at an approved dose for severe asthma. In seven cases in which anti-IL-5 and anti-IL-5Rα mAbs were sequentially administered to the same patient, the therapeutic effects were analyzed for the antibody administered first, whereas adverse effects were evaluated for each antibody. The effects of switching treatment from mepolizumab to benralizumab were analyzed as an additional analysis.
Clinical effects were evaluated with (1) exacerbation rates during 32 weeks prior to and after the initiation of treatment, and (2) dose of oral corticosteroids at baseline and 16 weeks after treatment. Exacerbation was defined as an event that required the administration of or an increase in the dose of systemic corticosteroids.
Functional evaluation was performed by comparing the FEV1 measured within 32 weeks before and after treatment with anti-IL-5/IL-5Rα mAb levels. Radiographic assessment of mucus plugs in the bronchi was performed using thoracic CT before and 16–52 weeks after treatment.
Statistical analysis
Numerical data are presented as the mean and standard deviation or median and IQR, and categorical data are presented as numbers and percentages. Categorical variables were compared using Fisher’s exact test, and continuous variables were compared using the Mann–Whitney U test or Wilcoxon signed-rank test and analysis of covariance. Statistical analyses were performed using GraphPad Prism (version 5.0; GraphPad Software, La Jolla, CA, USA) and IBM SPSS Statistics (version 26; IBM Corp., Armonk, NY, USA). Statistical significance was set at p < 0.05.
Data availability
The dataset used in this study is available from the corresponding author upon request.
References
Agarwal, R. et al. Allergic bronchopulmonary aspergillosis: Review of literature and proposal of new diagnostic and classification criteria. Clin. Exp. Allergy. 43, 850–873 (2013).
Asano, K., Kamei, K. & Hebisawa, A. Allergic bronchopulmonary mycosis—Pathophysiology, histology, diagnosis, and treatment. Asia Pac. Allergy. 8, e24 (2018).
Denning, D. W., Pleuvry, A. & Cole, D. C. Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med. Mycol. 51, 361–370 (2013).
Agarwal, R. Burden and distinctive character of allergic bronchopulmonary aspergillosis in India. Mycopathologia 178, 447–456 (2014).
Patterson, R., Greenberger, P. A., Radin, R. C. & Roberts, M. Allergic bronchopulmonary aspergillosis: Staging as an aid to management. Ann Intern Med. 96, 286–291 (1982).
Ionescu, M. D., Balgradean, M. & Marcu, V. Allergic bronchopulmonary aspergillosis in patient with cystic fibrosis—A case report. Maedica 9, 387–390 (2014).
Reece, E. et al. Co-colonisation with Aspergillus fumigatus and Pseudomonas aeruginosa is associated with poorer health in cystic fibrosis patients: An Irish registry analysis. BMC Pulm. Med. 17, 70 (2017).
Ishiguro, T. et al. Allergic bronchopulmonary aspergillosis with repeated isolation of nontuberculous mycobacteria. Intern. Med. 52, 1721–1726 (2013).
Ishiguro, T. et al. Pulmonary nontuberculous mycobacteriosis and chronic lower respiratory tract infections in patients with allergic bronchopulmonary mycosis without cystic fibrosis. Intern. Med. 55, 1067–1070 (2016).
Tsubouchi, H. et al. Successful treatment with mepolizumab in a case of allergic bronchopulmonary aspergillosis complicated with nontuberculous mycobacterial infection. Respir. Med. Case Rep. 28, 100875 (2019).
Agarwal, R. et al. Allergic bronchopulmonary aspergillosis. Indian J. Med. Res. 151, 529–549 (2020).
Patterson, R., Greenberger, P. A., Halwig, J. M., Liotta, J. L. & Roberts, M. Allergic bronchopulmonary aspergillosis. Natural history and classification of early disease by serologic and roentgenographic studies. Arch. Intern. Med. 146, 916–918 (1986).
Agarwal, R., Gupta, D., Aggarwal, A. N., Behera, D. & Jindal, S. K. Allergic bronchopulmonary aspergillosis: Lessons from 126 patients attending a chest clinic in north India. Chest 130, 442–448 (2006).
Agarwal, R. et al. A Randomized trial of itraconazole vs prednisolone in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Chest 153, 656–664 (2018).
Agarwal, R. et al. A randomised trial of prednisolone versus prednisolone and itraconazole in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Eur. Respir. J. 59, 2101787 (2022).
Hamprecht, A. et al. Azole resistance in Aspergillus fumigatus in patients with cystic fibrosis: A matter of concern?. Mycopathologia 183, 151–160 (2018).
Tomomatsu, K. et al. Effectiveness and safety of omalizumab in patients with allergic bronchopulmonary aspergillosis complicated by chronic bacterial infection in the airways. Int. Arch. Allergy Immunol. 181, 499–506 (2020).
Perez-de-Llano, L. A. et al. Effects of omalizumab in Aspergillus-associated airway disease. Thorax 66, 539–540 (2011).
Homma, T., Kurokawa, M., Matsukura, S., Yamaguchi, M. & Adachi, M. Anti-IgE therapy for allergic bronchopulmonary aspergillosis. J. Microbiol. Immunol. Infect. 49, 459–463 (2016).
Voskamp, A. L. et al. Clinical efficacy and immunologic effects of omalizumab in allergic bronchopulmonary aspergillosis. J. Allergy Clin. Immunol. Pract. 3, 192–199 (2015).
Randhawa, I., Chin, T. & Nussbaum, E. Resolution of corticosteroid-induced diabetes in allergic bronchopulmonary aspergillosis with omalizumab therapy: A novel approach. J. Asthma 46, 445–447 (2009).
Lin, R. Y., Sethi, S. & Bhargave, G. A. Measured immunoglobulin E in allergic bronchopulmonary aspergillosis treated with omalizumab. J. Asthma 47, 942–945 (2010).
Kelso, J. M. Following total IgE concentration in patients with allergic bronchopulmonary aspergillosis on omalizumab. J. Allergy Clin. Immunol. Pract. 4, 364–365 (2016).
Koike, H. et al. A review of Anti-IL-5 therapies for eosinophilic granulomatosis with polyangiitis. Adv Ther. 40, 25–40 (2023).
Asano, K., Suzuki, Y., Tanaka, J., Kobayashi, K. & Kamide, Y. Treatments of refractory eosinophilic lung diseases with biologics. Allergol Int. 72, 31–40 (2023).
Schleich, F. et al. Mepolizumab for allergic bronchopulmonary aspergillosis: Report of 20 cases from the Belgian Severe Asthma Registry and review of the literature. J. Allergy Clin. Immunol. Pract. 8, 2412–2413 (2020).
Terashima, T., Shinozaki, T., Iwami, E., Nakajima, T. & Matsuzaki, T. A case of allergic bronchopulmonary aspergillosis successfully treated with mepolizumab. BMC Pulm. Med. 18, 53 (2018).
Oda, N. et al. Severe asthma concomitant with allergic bronchopulmonary aspergillosis successfully treated with mepolizumab. Allergol. Int. 67, 521–523 (2018).
Soeda, S. et al. Case series of allergic bronchopulmonary aspergillosis treated successfully and safely with long-term mepolizumab. Allergol. Int. 68, 377–379 (2019).
Tsubouchi, K. et al. A case of allergic bronchopulmonary aspergillosis with marked peripheral blood eosinophilia successfully treated with benralizumab. Respir. Med. Case Rep. 32, 101339 (2021).
Matsuura, H. et al. Successful treatment with benralizumab for allergic bronchopulmonary aspergillosis that developed after disastrous heavy rainfall in Western Japan. Intern. Med. 60, 1443–1450 (2021).
O’Reilly, A. & Dunican, E. The use of targeted monoclonal antibodies in the treatment of ABPA-A case series. Medicina 58, 53 (2021).
Kolbeck, R. et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J. Allergy Clin. Immunol. 125, 1344–1353 (2010).
Tomomatsu, K. et al. Rapid clearance of mepolizumab-resistant bronchial mucus plugs in allergic bronchopulmonary aspergillosis with benralizumab treatment. Allergol. Int. 69, 636–638 (2020).
Drick, N. et al. Switch from IL-5 to IL-5-receptor alpha antibody treatment in severe eosinophilic asthma. J. Asthma Allergy. 13, 605–614 (2020).
Kavanagh, J. E. et al. Benralizumab after sub-optimal response to mepolizumab in severe eosinophilic asthma. Allergy 76, 1890–1893 (2020).
Agarwal, R. et al. Clinical significance of decline in serum IgE levels in allergic bronchopulmonary aspergillosis. Respir. Med. 104, 204–210 (2010).
Agarwal, R. et al. Utility of IgE (total and Aspergillus fumigatus-specific) in monitoring for response and exacerbations in allergic bronchopulmonary aspergillosis. Mycoses 59, 1–6 (2016).
Asano, K. et al. New clinical diagnostic criteria for allergic bronchopulmonary aspergillosis/mycosis and its validation. J. Allergy Clin. Immunol. 147, 1261–1268 (2021).
Agarwal, R. et al. Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: An analysis of 155 patients. Chest 132, 1183–1190 (2007).
Dunican, E. M. et al. Mucus plugs in patients with asthma linked to eosinophilia and airflow obstruction. J. Clin. Invest. 128, 997–1009 (2018).
Ueki, S., Hebisawa, A., Kitani, M., Asano, K. & Neves, J. S. Allergic bronchopulmonary aspergillosis—A luminal hypereosinophilic disease with extracellular trap cell death. Front. Immunol. 9, 2346 (2018).
Ueki, S. et al. Eosinophil extracellular trap cell death-derived DNA traps: Their presence in secretions and functional attributes. J. Allergy Clin. Immunol. 137, 258–267 (2016).
Haldar, P. et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N. Engl. J. Med. 360, 973–984 (2009).
Laviolette, M. et al. Effects of benralizumab on airway eosinophils in asthmatic patients with sputum eosinophilia. J. Allergy Clin. Immunol. 132, 1086–1096 (2013).
van der Veer, T. et al. Reduced exacerbation frequency and prednisone dose in patients with ABPA and asthma treated with dupilumab. Clin. Transl. Allergy 11, e12081 (2021).
Nishimura, T. et al. Complete withdrawal of glucocorticoids after dupilumab therapy in allergic bronchopulmonary aspergillosis: A case report. World J. Clin. Cases 9, 6922–6928 (2021).
Mikura, S. et al. Successful treatment of mepolizumab- and prednisolone-resistant allergic bronchopulmonary aspergillosis with dupilumab. Intern. Med. 60, 2839–2842 (2021).
Ramonell, R. P., Lee, F. E., Swenson, C. & Kuruvilla, M. Dupilumab treatment for allergic bronchopulmonary aspergillosis: A case series. J. Allergy Clin. Immunol. Pract. 8, 742–743 (2020).
Kai, Y. et al. Successful management of recurrent allergic bronchopulmonary aspergillosis after changing from mepolizumab to dupilumab: A case report. Respir. Med. Case Rep. 39, 101723 (2022).
Simpson, E. L. et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N. Engl. J. Med. 375, 2335–2348 (2016).
Wollenberg, A. et al. Laboratory safety of dupilumab in moderate-to-severe atopic dermatitis: Results from three phase III trials (LIBERTY AD SOLO 1, LIBERTY AD SOLO 2, LIBERTY AD CHRONOS). Br. J. Dermatol. 182, 1120–1135 (2020).
Castro, M. et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N. Engl. J. Med. 378, 2486–2496 (2018).
Wechsler, M. E. et al. Long-term safety and efficacy of dupilumab in patients with moderate-to-severe asthma (TRAVERSE): An open-label extension study. Lancet Respir. Med. 10, 11–25 (2022).
Bachert, C. et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): Results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 394, 1638–1650 (2019).
Frohlich, M., Olivenstein, R. & Cormier, M. Eosinophilic pulmonary complications of dupilumab in 2 patients with asthma and chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. Pract. 10, 617–619 (2022).
Yamazaki, K. et al. Eosinophilic granulomatosis with polyangiitis after treatment with dupilumab. J. Allergy Clin. Immunol. Glob. 1, 180–182 (2022).
Muthu, V. et al. Allergic bronchopulmonary aspergillosis (ABPA) sans asthma: A distinct subset of ABPA with a lesser risk of exacerbation. Med. Mycol. 58, 260–263 (2020).
Oguma, T. et al. Allergic bronchopulmonary aspergillosis in Japan: A nationwide survey. Allergol. Int. 67, 79–84 (2018).
Acknowledgements
This work was supported by a Research Grant on Allergic Disease and Immunology from the Japan Agency for Medical Research and Development under grant numbers JP18ek0410026 and JP 22ek0410098.
Author information
Authors and Affiliations
Contributions
K.T. and K.A. contributed to the conception and design of the study and analysis and interpretation of the data. H.Y., T.I., S.I., J.H., S.S., N.H., N.T., N.O., S.K., T.N., Y.S., M.Y., M.K., T.T., N.O., J.T., and T.O. helped in study conduct and data collection. K.T. wrote the manuscript. All authors have agreed to be accountable for all aspects of the study and have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
KA received lecture fees from GlaxoSmithKline plc and AstraZeneca K.K., Novartis, Sanofi. KT received lecture fees from AstraZeneca K.K. NH received personal fees from AstraZeneca K.K, GlaxoSmithKline plc, Novartis, Sanofi and grants from AstraZeneca K.K. JT received a research grant from GlaxoSmithKline plc. Other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tomomatsu, K., Yasuba, H., Ishiguro, T. et al. Real-world efficacy of anti-IL-5 treatment in patients with allergic bronchopulmonary aspergillosis. Sci Rep 13, 5468 (2023). https://doi.org/10.1038/s41598-023-32246-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-32246-8
- Springer Nature Limited