Abstract
In the absence of real-time surveillance data, it is difficult to derive an early warning system and potential outbreak locations with the existing epidemiological models, especially in resource-constrained countries. We proposed a contagion risk index (CR-Index)—based on publicly available national statistics—founded on communicable disease spreadability vectors. Utilizing the daily COVID-19 data (positive cases and deaths) from 2020 to 2022, we developed country-specific and sub-national CR-Index for South Asia (India, Pakistan, and Bangladesh) and identified potential infection hotspots—aiding policymakers with efficient mitigation planning. Across the study period, the week-by-week and fixed-effects regression estimates demonstrate a strong correlation between the proposed CR-Index and sub-national (district-level) COVID-19 statistics. We validated the CR-Index using machine learning methods by evaluating the out-of-sample predictive performance. Machine learning driven validation showed that the CR-Index can correctly predict districts with high incidents of COVID-19 cases and deaths more than 85% of the time. This proposed CR-Index is a simple, replicable, and easily interpretable tool that can help low-income countries prioritize resource mobilization to contain the disease spread and associated crisis management with global relevance and applicability. This index can also help to contain future pandemics (and epidemics) and manage their far-reaching adverse consequences.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Coronavirus Disease 2019 (COVID-19), a highly contagious respiratory borne infection, and its variants are still spreading rapidly and have caused more than 6.4 million global deaths. Although scientists have developed pharmaceutical treatments (medicine, therapeutics) and vaccines, it is still uncertain how effective these pharmaceutical measures are against the future variants of COVID-19, as evident from the recent astounding surge in global caseloads with the latest variant of concern—Omicron. The series of COVID-19 waves in the last two years have generated tremendous stress on the health care systems, prompting public health professionals to recommend universal vaccination and boosting.
This situation is more acute in Low and Middle-Income Countries (LMICs), where a major share of the unvaccinated population resides (about 19.87% of the low-income country population received only one dose of vaccine compared to the global full vaccination rate of 62%)1. In the face of widespread poverty, deficient safety-net measures, high self-employment, and a sizable informal economy, LMICs remained vulnerable imposing mobility restrictions that showed adverse consequences—leading to unemployment, poverty, and starvation2. Moreover, limited data capacity, insufficient health infrastructure, resource limitations, and inadequate COVID-19 testing ability made it further difficult for the LMIC governments to mitigate and manage the COVID-19 spread (for example, facilitating widespread testing and vaccinations), which demonstrate that conventional crisis management policies by LMICs are not equipped to tackle a pandemic of such scale.
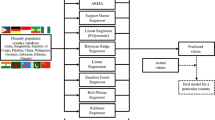
Efforts to contain future pandemics (and epidemics) and manage their far-reaching adverse consequences require smart crisis management—employing early warning systems, efficient planning, and targeted interventions. To this end, we proposed a data-driven strategy to prioritize the allocation of limited resources of LMICs for gaining efficiency in managing current COVID-19 response by (1) deriving a composite index of contagion risk (CR) index, grounded on infectious disease spreadability vectors of COVID-19 suggested by epidemiologists and public health experts; (2) validating the proposed CR-Index with publicly available sub-national (district) level COVID-19 data for South Asia (Bangladesh, India, and Pakistan), employing regression and machine learning (ML) methods; and (3) identifying high and low-risk zones to prioritize resource mobilization (such as vaccination roll-out) to contain the disease spread and associated crisis management, with global relevance and applicability.
There have been limited country-specific studies generating composite indices to rank areas in terms of health vulnerabilities, but none focused on a contagion risk-based index, especially for a large region containing multiple low-income countries, such as South Asia, home to one-fifth of global population. In disaster management, risk is defined as the ability of the population to absorb and ultimately recover from the effects of being exposed to a hazardous event, given the level of vulnerability of the population and the resources they have to mitigate its effects. Therefore, our first main contribution is proposing a contagion risk index to aid policymakers in low-income countries to prioritize resource allocation, and devise effective mitigation and reconstruction strategies for affected populations. Our second contribution relates to examining the predictive accuracy and generalization capability of our proposed risk index, CR-Index, using tools of machine learning and cross-validation based on time-series data. Thus, our study relates to a small but burgeoning literature that uses machine learning and artificial intelligence to predict COVID-19 outbreak3,4,5,6.
Methods
Data
The data employed in this study are collected from institutions and national statistics departments of respective countries. For Pakistan, we only use Sindh province in our estimations, due to the lack of district-level daily COVID-19 data. Similarly, for Bangladesh, we could not use COVID-19 mortality estimates. For each of the countries, we use different time-spans due to data availability issues. For Bangladesh, we use data from April 13, 2020, to February 28, 2022, for India, from January 30, 2020, to October 31, 2021, and for Pakistan (Sindh) from September 12, 2020, to November 22, 2021. Detailed data sources are provided in Table 1. Further details on the data collection approach and summary statistics are available in the supplementary file.
Domain and variable choice for CR-index
To derive the sub-national CR-Index, we broadly defined the following four domains founded on infectious disease spreadability vectors: urbanization, informality, migration, and health infrastructure.
Under the urbanization domain, we use district-wise percentage of the urban population variable for all the three countries7,8,9,10,11,12. This degree of urbanization variable (share of the urban population) captures a particular district's overall economic-demographic condition, demonstrating more vibrant economic interactions in the region. It also suggests a higher level of industrialization, trade, and travel connectivity resulting in a higher probability of social interactions and a greater possibility of spreading the virus.
The informal employment or “informality” at the sub-national level also plays a role in COVID-19 transmission, especially in LMICs. Informal employment does not follow conventional labor rights and policy. Moreover, employees hired informally are low-income daily wage earners who do not have job security, do not get paid or seek leaves, and often do not have the luxury to work from home, resulting in more exposure to contagion spread. Developing countries, such as Bangladesh, India, and Pakistan have a considerably large informal sector (both in rural and urban areas), hired in construction, transportation, manufacturing, and service sectors, where the continuous search for new income opportunities is a harsh reality. Approximately 71% of the sectoral composition of employment in developing countries are self-employed compared to 13% in developed countries13,14. We obtained data on informal employment share for Bangladesh and Pakistan (Sindh), but such data with high accuracy was not available for India, where we used the share of non-farm employment in India, which is a reasonable proxy for informal employment15,16,17.
Developing countries are also known to have a large share of the mobile population—classified as domestic and international migrants. For example, Bangladesh is the sixth leading country of origin for international migrants18. Due to the COVID-19 pandemic and resulting global economic shutdown, a large percentage of international migrants went back to their home countries—carrying the disease with them and contributing to the virus spread. Similarly, domestic migrants face similar consequences and lost urban sources of income due to the lockdown that forced them to go back to their villages of origin. Both these channels of reverse migration also contributed to virus transmission, as documented in recent studies19,20. To capture this important vector of virus diffusion, we include district level international and domestic migrants as a variable in the CR-Index construction19,20,21. For Bangladesh and India, we obtained data on the share of migrants in the district that includes both domestic and international migrants. For Pakistan, only the data on domestic migration at the district level was available.
Finally, sub-national health infrastructure, measured as the number of beds and health facilities per million of population, have been utilized as candidate variables representing the health infrastructure domain22,23,24. For Bangladesh and India, we used hospital beds per million in a district. For Pakistan, we took health facilities per million as data were more reliable for health facilities than the total number of beds.
We tried to be consistent about the choice of variables for the four domains across the three countries. However, due to administrative and institutional differences (along with data availability), a few variables are not the same. Sources for data for each of the domain specific variables for each of the countries are provided in Table 1.
The CR-Index variable is a composite of these four domains, whereby greater its value, greater the risk a district faces in terms of spread of COVID-19 infections to its population. Further details on the data used for the CR-Index, its construction, rationale, and descriptive statistics are given in subsections A1, A2, and A3 in the supplementary file.
CR-index construction
Using each of the domain specific variables, we first created sub-indices j {j = 1, 2, 3, 4} using the following formula for each district d in country c {c = Bangladesh, India, Pakistan}:
\({X}_{c,d,j}\) is the sub-national domain specific value, while \(\mathrm{min}\left({X}_{c,d,j}\right)\) and \(\mathrm{max}\left({X}_{c,d,j}\right)\) are the country-domain specific minimum and maximum values of the variable at the district (sub-national) level. After generating sub-indices for each domain-district-country, we use simple arithmetic mean to generate the composite CR-Index for each district in each country, following the human development index (HDI) construction method of the UNDP for wide acceptability25. Formally,
Here n is the number of domains. We used arithmetic mean, given some sub-indexes generated zero value (for example, some districts did not have any reported international migration, resulting in a score of zero for that sub-index). The process of CR-Index construction normalizes the variables based on the minimum and maximum variation of each variable across sub-nations for each country.
Measures for CR-index validation
Correlation test
We run an Ordinary Least Squares (OLS) regressions to examine whether the statistical validity of the correlation between the CR-Index and COVID-19 epidemiologic data remains consistent across the time-horizon after controlling for district-specific variables. We run the following regressions:
Here, t represents a specific time horizon (week) where \(t=\mathrm{1,2},\dots , n\) and \(IHST[{y}_{c,d,t}]\) is the Inverse Hyperbolic Sine Transformation (IHST) of the reported COVID-19 epidemiologic data (positive cases or death) for each district. IHST is appropriate when a variable contains a significant number of 0’s. The equation for IHST for a variable y is, log(yi + (yi2 + 1)0.5) where, \(y_{i} \ge 0\). The IHS ensures that zero COVID-19 cases or deaths are not dropped during the process of normalization. \({Z}_{c,d}\) is the district-specific control, which is the district level population. \(\epsilon_{c,d,t}\) is a time and district specific unobservable term.
Regression test
Utilizing the time-series pattern of the daily data, we estimate regressions in Eqs. (4) and (6), where daily reported COVID-19 cases and deaths are regressed against the CR-Index using OLS. In Eqs. (5) and (7), the daily reported COVID-19 cases and deaths are regressed against the CR-Index, with day fixed effects (FE) and district controls. Under this setting, Eqs. (5) and (7) are the most conservative specifications, taking care of the time dimension and regional control, while Eqs. (4) and (6) control for the time trend, \(\gamma \left(t\right)\).
In Eqs. (4) and (6), the time trend, \(\gamma \left(t\right)\), controls for the rise of district specific COVID-19 cases throughout the study period. The parameter \(\gamma \) in Eqs. (5) and (7) is the time FE, which controls for any time related variation across days within the study period for all the districts. \(\epsilon_{c,d,t}\), is the time and district specific unobservable term.
Risk zoning and predictive accuracy using machine learning
To cross-validate the predictive accuracy of the CR-Index for any future event, we use the Random Forests (RF) process in machine learning26,27. RF belongs to a class of supervised algorithms and has been used widely in public health and epidemiology28,29. In contrast to non-parametric approaches, RF allows for flexible functional forms leading to better predictions and has been proven to effectively manage the bias-variance trade-off27.
Based on CR-Index score, we classified districts into three risk zones: ‘Red’ if the percentage of COVID-19 cases (or deaths) exceeds the 90th percentile relative to all other districts for a given country; ‘Orange’ if the percentage of cases/deaths is between 90 and 25th percentiles; and ‘Green’ if below the 25th percentile. Using the RF algorithm, the multiclass classification response is modeled as a function of CR-Index, where, for a given country, the predicted risk zone of each district is compared with their actual risk in the test data. We use the early/late split method30, where the early data is utilized to train, and the later data is used as a test31. The results of the random forests and predictive accuracy are determined by two key parameters also known as tuning parameters: the number of trees to grow and the number of random features for the splitting process32. The number of trees is set to 500, and the number of random features is one, since our primary variable of interest is the CR-Index. Smaller the number of features, greater the parsimony of the model, therefore, greater the predictive accuracy27,32. Moreover, to reduce the bias and variance of the estimations, we fit RF using fivefold cross validation repeated for 50 times32.
Finally, the classification prediction of the CR-Index is assessed by the AUC (Area Under the Curve) and ROC (Receiver Operating Characteristics) curves. ROC is a probability curve, whereas AUC measures the degree of separability33. The ROC curve plots the true positive rate (TPR) against the false positive rate (FPR). TPR, also known as “Sensitivity”, is the ratio of districts that are correctly categorized as high-risk (true positive) to the total number of positives. Whereas FPR, is “1—Specificity)”, where “Specificity” is the true negative rate, and it is the ratio of the number of low-risk districts incorrectly categorized as high-risk to the total number of actual negatives. In general, an AUC value between 0.70 and 0.80 is considered acceptable; 0.80–0.90 is considered excellent, and more than 0.90 is considered outstanding33. The values of AUC-ROC are obtained using the “mLeval’’ and “pROC” packages of statistical software “R”34,35.
Ethics approval
Prior ethical approval is not required as the study uses publicly available data.
Results
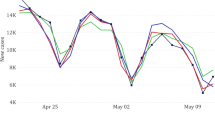
Correlation estimates
Based on Eq. (3), Panel A of Fig. 1, produced the weekly regression estimates for the CR-Index for district-wise COVID-19 cases for Bangladesh, India, and Pakistan (Sindh). During the initial stages of the pandemic, few of the estimates came out statistically insignificant due to insufficient data-points across all the districts. However, after COVID-19 cases were reported from almost all the districts, estimates remained robust and statistically significant. Panel B presents the weekly regression estimates using COVID-19 deaths. Both the figures show that CR-Index is statistically significant and maintains a close range of coefficient values within the period of our analysis.
Panel regression estimations
Columns (1) and (3) in Table 2 report the regression results based on Eqs. (4) and (6) for COVID-19 cases using OLS and time FE. Whereas columns (2) and (4) report the regression results based on Eqs. (5) and (6) for COVID-19 deaths. In summary, the OLS and FE regression results show that the CR-Index is positive and significantly associated with COVID-19 spread and mortality, demonstrating strong predictive power of the CR-Index. In Column (2), 1 percent increase in the value of CR-Index is associated with an approximate 1.88 percent increase in the number of positive COVID-19 cases for Bangladesh, 5.39 percent for India, and 4.6 percent for Pakistan (Sindh), after controlling for time fixed effect and district specific control. In Column (4), a 1 percent increase in CR-Index is associated with an approximate 1.65 and 1.06 percent increase in COVID-19 deaths for India and Pakistan (Sindh). Columns (2) and (4) offer the most conservative specification, and with regular assumptions on FE identification. The p values for these coefficients are close to zero, showing a strong predictive power of the CR-Index in case of COVID-19 related deaths as well.
Contagion zoning
Using the score of the CR-Index, we divided districts for each of the countries into three zones (Red/Orange/Green) based on the CR-Index distribution described before. In Fig. 2, Panel A, sub-panels (A1), (B1), and (C1) show these three zones’ spatial distribution for each of the countries. Sub-panels (A2), (B2), and (C2) superimpose the latest available aggregated district-wise COVID-19 positive cases. The map shows that the proposed index and zoning classification can identify vulnerable districts/regions robustly. Sub-panels (A3), (B3) and (C3) show the CR-Index histogram and kernel-density plot of the distribution. Panel B of Fig. 2 superimposes the aggregate COVID-19 deaths for India and Pakistan (Sindh) on their respective maps and shows that the CR-Index is robustly identifying vulnerable regions with high COVID-19 death rates. All the maps in Fig. 2 were generated using the statistical software, STATA BE 17 (https://www.stata.com/). Section C (supplementary file) reports the basic summary statistics, and the distribution of district-specific CR-Index scores COVID-19 cases and deaths (as a % of total reported cases for the latest available date) based on these proposed zones.
Machine learning results
Table 3 reports the AUC values from the machine learning exercise for the three South Asian countries. Columns (1)–(5) of Table 3 report estimates using the entire 2020 as the training data and 2021 as the testing data—using the early-late split method of cross validation—our preferred model for the validation exercise. Using the same training data we also predicted the month-by-month results, where each month in 2021 was used as the test, and reported the average of these in columns (6)–(10). Time series plots of COVID-19 cases and deaths for the three South Asian countries are provided in Section B of the supplementary file. The complete month-by-month results are given in Section D in the supplementary file.
From columns (1)–(5) in Table 3, the mean values of AUCs range from 0.84 to 0.97, therefore, suggesting excellent to outstanding out-of-sample predictive accuracy for the CR-Index. This implies that for a given random data, the CR-Index can distinguish districts with high-risk COVID-19 cases/deaths for more than 91% of the time, on average. These findings are further supported by results in columns (6)–(10) of Table 3 using month-by-month out-of-sample prediction tests, where the average value of AUC is about 0.80. In addition to AUC-ROC, Table 3 also reports the values of other commonly used metrics for predictive performance, namely, sensitivity, specificity, and balanced accuracy.
To check the robustness of the multiclass classification based estimates, we additionally conduct binary risk-zoning classification (high-risk vs. low-risk districts using 75th percentile cut-off) and district-monthly data. These estimates are strongly similar with Table 3 estimates and are reported in the supplementary file (section D2 and D3). The ROC curves corresponding to binary classification are also reported in Fig. D1 (supplementary file).
Discussion
Data-driven mitigation planning, and management are crucial for resource-constrained countries—ensuring the best use of their limited resources. In the absence of adequate, regular and reliable epidemiologic data, it is difficult for the policy makers from low-income countries to derive advance planning and timely response to contain and manage the spread of an epidemic or pandemic; and formulate a targeted resource distribution plan for mass testing, therapeutics and vaccination.
To this end, this paper created a sub-national level contagion-risk index in South Asia, developed using four important socio-economic and health domains (urbanization, informality, migration and health infrastructure) on disease spreadability vectors. The dataset employed for CR-Index utilized readily available statistics at the sub-national level, which has wide applicability for global adoption, particularly for LMICs. Our proposed CR-Index shows strong statistical properties in explaining the variabilities of COVID-19 cases and deaths for all the three countries, across different timeframes. We have provided a simple flowchart, Fig. A5.1, Section A5, in the supplementary file to explain the step-by-step process to develop the CR-Index for any LMICs where such data are available.
Built on the CR-Index, we propose zone-specific contagion management measures as a potential solution for precautionary advance planning and to prioritize the efficient allocation of limited resources. Classifying districts into high, moderate and low-risk, based on the 75th and 25th percentile distribution thresholds, we validate the CR-Index accuracy using machine learning based on test/train cycle method26. As suggested in the existing literature to use a nonlinear curve fitting strategy36, we utilize random forest as our machine learning algorithm, which allows us to explore non-linearities in our proposed CR-Index variable. We applied 2020 COVID-19 data to train the CR-Index, and then examine its out-of-sample predictive performance using the data in 2021—the test sample. The resultant values of AUC-ROC in our preferred model are generally well-above 0.80 and statistically significant at a 5% significance-level, thus, suggesting superior predictive performance of the CR-Index. The predictive performance of the index is more accurate during periods of exceptionally high COVID-19 cases and deaths. For example, the values of AUC-ROC using the data for COVID-19 cases in India for the months of April and May 2021 (when delta was the dominant variant in India) as test samples are the highest amongst all the months in 2021 (supplementary Table D1.1).
The findings of this study relate to recent studies that have computed composite indices to rank districts in terms of COVID-19 vulnerabilities using various information on socio-economic, demographic, and infrastructure characteristics7,10,11,37,38,39. However, our study differs from those studies in some important ways. First, instead of creating COVID-19 vulnerability indices, our study focuses on computing contagion risk indexes at sub-national level. Second, while these studies focus on a single country, for example, India3, our study, in contrast, computes contagion risk indices for a region, using data from major three countries in South Asia with a combined population of more than 1.5 billion (about one-fifth of global population). Third, there exists paucity of studies that examine the validity of the relevant vulnerability indices for COVID-19 at sub-national level. Our study aims to fill this void by using machine learning where the performance of the contagion risk index is validated using various hold-out data.
Despite the strong empirical and predictive support of the CR-Index, there are some important limitations. First, it would have been ideal to construct a measure of the index at a lower administrative level, such as at the level of a sub-district. Second, our measure of CR-Index is static, and the data utilized to construct the index is not the most recent, therefore, it may not accurately capture riskiness in districts in which rapid changes have transpired lately. Future research can employ more recent and real-time data that are collected from disparate sources, such as, phone-tracking data to capture mobility and migration. Third, the rationale for choosing variables under each domain is country-specific, and this choice could be arbitrary. However, the focus should not be on selecting variables but on the domains, which are known to affect the contagion spread during this pandemic. Fourth, we have constructed the CR-Index using variables for each country and normalized the variables based on the minimum and maximum variation of each variable across districts. However, relative values of the variables can also be utilized to develop the index. Fifth, our index assigns equal weights to each variable and sub-domain. The domains may not be equally important; thus, different weights could be assigned to the variables. Alternatives, such as, factor weights are, however, problematic as they are sensitive to data and lack interpretability. Sixth, due to inaccuracy and non-availability of data on COVID-19 induced deaths at the district-level of Bangladesh, we could not use it for the CR index construction for Bangladesh. Finally, our proposed CR-Index is simple and additive, and, therefore, unable to account for the multiplicative and non-linear nature of the variables and sub-domains. This requires the use of methodological advancements using non-linear/non-parametric methods that can create a more robust measure of the contagion risk index.
Despite reduction in COVID-19 case trends and ever-increasing vaccination rate, epidemiologists and virologists expressed vigilance and have not completely ruled out future variants that can evade vaccine immunity40. The proposed contagion risk index aims to help policymakers in LMICs to effectively prioritize resource allocation and adopt risk mitigation strategies for better responses to future COVID-19 waves and pandemics. The analysis in this paper offers initial guidelines for developing a comprehensive contagion risk index, which can be modified further with additional data and methodological enhancements.
Conclusion
In conclusion, in the absence of real time surveillance data, our study proposes a system for early warning and potential contagion hotspots—based on communicable disease spreadability vectors—for better disease management, planning and targeted intervention. To facilitate this recommendation, we have developed, validated, and illustrated the use of an easily interpretable data-driven Contagion Risk Index, as a toolkit, in the case of COVID-19 pandemic in South Asia. This simple, low-cost, flexible toolkit could be readily adapted for low and middle-income countries and could be utilized as a decision support guide for an efficient use of their limited resources, while reducing the likelihood of a rapid resurgence of the communicable diseases which would be useful for future epidemics and pandemics.
Data availability
Data and codes to reproduce the analysis and graphs associated with this study are available from https://github.com/ma0511/COVID-19-South-Asia-Project.
References
Ritchie, H., Mathieu, E., Rodés-Guirao, L., Appel, C., Giattino, C. & Ortiz-Ospina, E. et al. Coronavirus (COVID-19) vaccinations (2022). https://ourworldindata.org/covid-vaccinations. Accessed 20 June 2022.
Egger, D. et al. Falling living standards during the COVID-19 crisis: Quantitative evidence from nine developing countries. Sci. Adv. 7(6), eabe0997 (2021).
Elsheikh, A. H. et al. Artificial intelligence for forecasting the prevalence of COVID-19 pandemic: An overview. Healthcare 9(12), 1614 (2021).
Saba, A. I. & Elsheikh, A. H. Forecasting the prevalence of COVID-19 outbreak in Egypt using nonlinear autoregressive artificial neural networks. Process Saf. Environ. Prot. 141, 1–8 (2020).
Al Qaness, M. A. et al. Efficient artificial intelligence forecasting models for COVID-19 outbreak in Russia and Brazil. Process Saf. Environ. Prot. 149(1), 399–409 (2021).
Elsheikh, A. H. et al. Deep learning-based forecasting model for COVID-19 outbreak in Saudi Arabia. Process Saf. Environ. Prot. 149(1), 223–233 (2021).
Acharya, R. & Porwal, A. A vulnerability index for the management of and response to the covid-19 epidemic in India: An ecological study. Lancet Glob. Health 8(9), e1142–e1151 (2020).
Qiu, Y., Chen, X. & Shi, W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (covid-19) in China. J. Popul. Econ. 33(4), 1127–1172 (2020).
Khalatbari-Soltani, S., Cumming, R. C., Delpierre, C. & Kelly-Irving, M. Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J. Epidemiol. Community Health 74(8), 620–623 (2020).
Sarkar, A. & Chouhan, P. COVID-19: District level vulnerability assessment in India. Clin. Epidemiol. Glob. Health 9, 204–215 (2021).
Jha, S., Goyal, M. K., Gupta, B. & Gupta, A. K. A novel analysis of COVID 19 risk in India incorporating climatic and socioeconomic Factors. Technol. Forecast. Soc. Change 167, 120679 (2021).
Ahmed, F., Ahmed, N. E., Pissarides, C. & Stiglitz, J. Why inequality could spread COVID-19. Lancet Public Health 5(5), e240 (2020).
Stebbins, S. Unemployment rate remains historically high: These US cities are among those with highest jobless rates. USA Today (2020). https://www.usatoday.com/story/money/2020/08/08/cities-with-the-worstunemployment-since-the-pandemic-started/42. Accessed 29 June 2022.
Iqbal, K., Toufique, K. A., Ahmed, N., Pabon, N. F. & Ibon, W. F. Dynamics of rural nonfarm sector: 2000–2016. Paper Presented at 2019 BIDS Research ALMANAC (2019). Available from: https://bids.org.bd/uploads/events/ALMANAC2019/S1_P1.pdf
Romanello, M. Covid-19 and the informal sector. In Covid-19 and International Development (ed. Papyrakis, J.) 89–102 (Springer, 2022).
Paremoer, L., Nandi, S., Serag, H. & Baum, F. Covid-19 pandemic and the social determinants of health. BMJ 372, 100. https://doi.org/10.1136/bmj.n129 (2021).
Megersa, K. The informal sector and covid-19. Institute of Development Studies (2020).
The number of international migrants reaches 272 million, continuing an upward trend in all world regions, says UN (2019). https://www.un.org/development/desa/en/news/population/international-migrant-stock-2019.html. Accessed 29 June 2022.
Ahsan, R., Iqbal, K., Khan, M., Mobarak, A. M. & Shonchoy, A. Using migration patterns to predict Covid-19 risk exposure in developing countries. Policy Brief. Yale School of Management (2020).
Lee, J. N., Mahmud, M., Morduch, J., Ravindran, S. & Shonchoy, A. S. Migration, externalities, and the diffusion of covid-19 in South Asia. J. Public Econ. 193, 104312 (2021).
Cowley, L. A. et al. Genomics, social media and mobile phone data enable mapping of sars-cov-2 lineages to inform health policy in Bangladesh. Nat. Microbiol. 6(10), 1271–1278 (2021).
Maani, N. & Galea, S. Covid-19 and underinvestment in the public health infrastructure of the United States. Milbank Q. 98(2), 250 (2020).
Banik, R., Rahman, M., Sikder, T. & Gozal, D. COVID-19 in Bangladesh: Public awareness and insufficient health facilities remain key challenges. Public Health 183, 50 (2020).
Kumar, A., Nayar, K. R. & Koya, S. F. COVID-19: Challenges and its consequences for rural health care in India. Public Health Pract. 1, 100009 (2020).
Anand, S. & Sen, A. Human development Index: Methodology and Measurement. Human Development Report Office (HDRO). United Nations Development Programme (UNDP) (1994).
Hofman, J. M. et al. Integrating explanation and prediction in computational social science. Nature 595(7866), 181–188 (2021).
Breiman, L. Random forests. Mach. Learn. 45(1), 5–32 (2001).
Lin, S. H. & Ikram, M. A. On the relationship of machine learning with causal inference. Eur. J. Epidemiol. 35(2), 183–185 (2020).
Wiemken, T. L. & Kelley, R. R. Machine learning in epidemiology and health outcomes research. Annu. Rev. Public Health 41, 21–36 (2019).
Efron, B. Prediction, estimation, and attribution. Int. Stat. Rev. 88, S28–S59 (2020).
Cochrane, C. Time series nested cross-validation. Towards Data Science (2018). https://towardsdatascience.com/time-series-nested-cross-validation76adba623eb9
Kuhn, M. & Johnson, K. Applied Predictive Modeling (Springer, USA, 2013).
Mandrekar, J. N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 5(9), 1315–1316 (2010).
John, C. R. MLeval: Machine learning model evaluation. R package version 03 (2020).
Robin, X. et al. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 12(1), 1–8 (2022).
Peter, O. J., Qureshi, S., Yusuf, A., Al-Shomrani, M. & Idowu, A. A. A new mathematical model of COVID-19 using real data from Pakistan. Result Phys. 24, 104098 (2021).
Tiwari, A., Dadhania, A. V., Ragunathrao, V. A. & Oliveira, E. R. Using machine learning to develop a novel covid-19 vulnerability index (c19vi). Sci. Total Environ. 773, 145650 (2021).
Welsh, C. E., Sinclair, D. R. & Matthews, F. E. Static socio-ecological COVID-19 vulnerability index and vaccine hesitancy index for England. Lancet Reg. Health Eur. 14, 100296 (2022).
Li, T., Luo, J. & Huang, C. Understanding small Chinese cities as COVID-19 hotspots with an urban epidemic hazard index. Sci. Rep. 11(1), 1 (2021).
Biswas, S. Covid-19: Should India be bracing for a fourth wave? BBC News (2022). https://www.bbc.co.uk/news/world-asia-india-60832236. Accessed June 2022.
Acknowledgements
We are thankful to Maha Rahman to guide us with the data of Sindh, Pakistan. We are also grateful to Sam Asher and Paul Novosad and their team at Development Data Lab for making the Indian data available at their website.
Author information
Authors and Affiliations
Contributions
A.S.: conceptualization, methodology, validation, writing—original draft preparation; writing—reviewing and editing; M.M.: conceptualization, methodology, validation, writing—original draft preparation, data collection and analysis, writing—reviewing and editing; T.M.: validation, writing—original draft preparation, data collection and analysis, writing—reviewing and editing; M.A.: validation, data collection and analysis, writing—reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shonchoy, A.S., Mahzab, M.M., Mahmood, T.I. et al. Data driven contagion risk management in low-income countries using machine learning applications with COVID-19 in South Asia. Sci Rep 13, 3732 (2023). https://doi.org/10.1038/s41598-023-30348-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-30348-x
- Springer Nature Limited
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.