Abstract
The earlier the diagnosis of multiple sclerosis (MS), the sooner disease-modifying treatments can be initiated. However, significant delays still occur in developing countries. We aimed to identify factors leading to delayed diagnosis of MS in Upper Egypt. One hundred forty-two patients with remitting relapsing MS (RRMS) were recruited from 3 MS units in Upper Egypt. Detailed demographic and clinical data were collected. Neurological examination and assessment of the Disability Status Scale (EDSS) were performed. The mean age was 33.52 ± 8.96 years with 72.5% of patients were females. The mean time from symptom onset to diagnosis was 18.63 ± 27.87 months and the median was 3 months. Seventy-two patients (50.7%) achieved diagnosis within three months after the first presenting symptom (early diagnosis), while seventy patients (49.3%) had more than three months delay in diagnosis (delayed diagnosis). Patients with a delayed diagnosis frequently presented in the period before 2019 and had a significantly higher rate of initial non-motor presentation, initial non-neurological consultations, prior misdiagnoses, and a higher relapse rate. Another possible factor was delayed MRI acquisition following the initial presentation in sixty-six (46.5%) patients. Multivariable logistic regression analysis demonstrated that earlier presentation, initial non-neurological consultation, and prior misdiagnosis were independent predictors of diagnostic delay. Despite advances in MS management in Egypt, initial non-neurological consultation and previous misdiagnoses are significant factors responsible for delayed diagnosis in Upper Egypt.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a chronic central nervous system autoimmune disorder mainly affecting productive young and middle-aged adults1. The personal, social and economic sequels are directly related to the consequent inflammation and progressive degeneration along the disease course. Even though no curative treatment for MS has been discovered yet, a breakthrough has been made in the disease-modifying treatments (DMT) industry to alter the disease course2. Through an expanding landscape of drugs with different mechanisms of action, the aim of treatment has shifted from merely controlling the disease activity to the prevention of any progression3,4. Therefore, the earlier the diagnosis of MS can be made, the sooner the DMTs can be initiated to achieve the treatment goals of timely prevention of disability progression with reduced burdens imposed by the disease nature5. However, significant delays are still being noticed before reaching MS diagnosis that could withhold timely DMTs administration6. A varied number of factors might cause such delays; this may be disease-related due to the variability of clinical and imaging manifestations, physician-related due to insufficient knowledge of the primary care physicians, or system-related due to the unavailability of diagnostic facilities and specialized centers7,8. Since the prevalence of MS is rising in Egypt (25/100,000 was recorded from different centers)9, and patients can typically live with MS for almost 40 years10, this could be a considerable burden in such a developing country like Egypt particularly the South of it, affecting the quality of life of patients and their families alongside the significant economic consequences on the society11. Therefore, a strategy that targets factors causing such delays might have the same importance as developing treatment12. Therefore, the current study aimed to identify the factors that play a role in delayed diagnosis of multiple sclerosis in a large sample of patients with multiple sclerosis from Upper Egypt.
Results
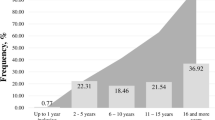
The study included 142 patients with MS with a mean age of 33.52 ± 8.96 years. One hundred and three patients (72.5%) were females, while 39 (27.5%) were males. The mean age at onset was 28.37 ± 8.506 (13–50) years (27.52 ± 8.25 years in females while in males, 30.60 ± 8.88 years). The mean age at diagnosis was 30.12 ± 8.627 (16–50) years. The duration of illness in the studied patients ranged from 3 months up to 20 years, with a mean duration of 5.55 ± 4.08 years and a median of 5 years. Patients had 3 relapses as a median number of relapses during their illness. The most prevalent primary symptoms were motor symptoms in 49 patients (34.5%), followed by sensory symptoms and optic neuritis in 28 patients (19.7%) and 27 patients (19%), respectively.
At the onset of symptoms, 55.6% of the patients initially visited a neurologist, while the remaining initially consulted other specialties like orthopedics and ophthalmologists. Eighty patients (56.3%) were initially misdiagnosed at the first medical consultation, with a median delay from the onset of clinical symptoms to MS diagnosis of three months. The current mean EDSS score was 2.93 ± 1.86 SD with a range of 0.50 to 6.50). When females were compared against males, no statistically significant differences could be found regarding age at onset, age at diagnosis, or time to reach MS diagnosis (U = 0.415). There were also no differences between groups regarding the first specialty sought, previous misdiagnosis, frequency of relapses or the current EDSS scores. Other demographic and clinical features were summarized in Table 1).
The overall median diagnostic delay was three months. About seventy-two patients (50.7%) achieved diagnosis within three months after the first presenting symptom, while seventy patients (49.3%) had more than three months delay in diagnosis and treatment initiation. Consequently, patients were divided into two groups; patients who received an early diagnosis of MS (during three months of onset) and those who had delayed diagnosis (after three months of onset).
We found no statistically significant difference between the two groups of patients regarding the different demographic data. However, there was a statistically significant difference between the two groups regarding the age at onset, the initial presentation of whether it’s motor or non-motor, the first specialty sought, previous misdiagnoses, relapse frequency and the year of the first presentation. Patients diagnosed earlier were slightly older than patients with delayed diagnosis (p = 0.041). Also, Patients with initial motor presentation were diagnosed earlier than patients with non-motor presentation (2 months versus 6 months, p = 0.030). The direct presentation to neurologists in 73.5% of patients who had motor symptoms at onset could explain why those patients acquired MS diagnosis earlier without prior misdiagnosis in 55.1%. Other differences between the two groups of patients with motor and non-motor onset were illustrated in Table 2. Early diagnosis of MS within the first 3 months was achieved in 81.9% of patients who presented initially to a neurologist compared to only 18.1% of patients who presented to other medical specialties (ophthalmologists followed by orthopedics were the most common non-neurological specialists visited by 17.6% and 16.9% of patients respectively). At least one prior misdiagnosis was given in about 97.1% of patients with a delayed diagnosis, which could be explained by the low index of suspicion for MS with consequently delayed referral to an MS specialist. The significant differences in the frequency of relapses could be explained as a factor or a consequence of delayed diagnosis. Delayed diagnosis will lead to delayed DMT initiation and therefore increase relapse frequency. Also, misdiagnosing a prior symptom may shift attention from MS suspicion. Although reluctance in seeking medical advice is a well-known factor in developing countries like Egypt; it was found to be independent from socioeconomic or educational level. Also, differences in the distribution of specialized neurology services and imaging facilities between urban and rural areas couldn’t explain such delays. However, the notable improvement found in MS diagnosis over the years, especially from 2019 to date, might reflect the increased awareness among laypersons with improved recognition of the possible neurological symptoms and improved healthcare-seeking behavior. Alongside the improved awareness of MS among healthcare providers and the healthcare system, this could be a possible explanation of the trend towards the shorter time to diagnose MS in more recent years. The multivariable logistic regression analysis model demonstrated in SD: Standard deviation Table 3 confirmed that seeking the advice of a non- neurologist, receiving a prior misdiagnosis, and the earlier year period of presentation were the three independent predictors of MS diagnostic delay.
When radiological data were reviewed for possible factors contributing to the diagnostic delay, sixty-six (46.5%) patients had no MRI exams at their initial presentation for different reasons; mainly because their physicians didn’t ask for or they just had a CT scan instead (in 63 patient), while only 3 patients reported a delay in acquiring MRI for their unaffordable price. For those who had an MRI scan immediately after presentation, 17 (12%) of patients showed atypical or incomplete data to fulfil MS diagnostic criteria and were given an alternative initial diagnosis. The radiological data analysis was not incorporated as a possible factor for the diagnostic delay in the logistic regression model as the initial MRI exams of 45 (31.8%) patients were not available and only follow-up images at later stages of the disease were reviewed. Also, different MRI machines with different resolutions and different protocols used to acquire these images have complicated data analysis and comparison. A summary of the radiological data was provided in Table 4.
Discussion
This research was conducted to investigate the diagnostic delay in MS and the contributing factors in the upper Egyptian population. Given the rising prevalence and incidence of MS in recent years, as well as the importance of early diagnosis and treatment to reduce patients' disabilities and the imposed economic burden, investigating these factors is critical.
In the present study, the mean age at the onset of MS was 28.37 ± 8.506 years, which is somewhat considered younger compared with most studies from other geographical locations. The age at onset of MS symptoms was reported to be 29.35 and 28.2 years in two different studies from Iran4,13 and 33.7 years in Canada14. In another study from Spain, the mean age of patients at the onset of the disease was 31.2 years15. In Colombia, the mean age at the time of the first symptom was 32.4 ± 10.6 years, and at the time of diagnosis was 34.5 ± 10.5 years16. On the other hand, women had a typical representation in our cohort (72.5%), following the known global epidemiology of MS and the MENA area, with a female–to–male ratio of 2.6:14.
The most common initial presenting symptoms were motor symptoms related to the pyramidal system involvement, followed by sensory symptoms and optic nerve involvement. This is also similar to the data obtained from the large registry of the MENACTRIMS (Middle East North Africa Committee for Treatment and Research in Multiple Sclerosis)9. In the present study, the mean duration of illness was 5.55 ± 4.04 years, the annual frequency of relapses was 3.35 ± 1.7 and the mean EDSS scores of 2.9 ± 1.86. These results were concordant with the conclusion of the MENACTRIMS study reporting that except for an earlier age at onset and a more aggressive clinical course leading to earlier disability, the clinical phenotype of MS in the MENA region was similar to the Western phenotype9.
According to the National Institute of Clinical Excellence (NICE), a timeline of no longer than three months is recommended to diagnose MS (< 6 weeks between onset symptoms and the first neurological consultation and < 6 weeks between the neurological consultation and MS diagnosis)17. In this study, the median delay between the onset of symptoms and MS diagnosis was three months. This was a month longer than the median delay of two months reported in a study from Iran by Ghiasian et al.18. In Portuguese, the median time between the first presentation and diagnosis was 9 months19. In the study by Fernandez et al.15, the delay was 24.9 months. In Colombia, the overall mean diagnostic delay was 3.07 years (SD 3.83), and about 45.7% of the patients had a delayed diagnosis16. The possible reasons for the observed variations between countries are the different levels of health literacy among different populations, different ways the referral processes work, the strength and accessibility to specialized health care facilities and the use of different diagnostic criteria. Table 5 shows the differences in the time to diagnosis between different studies from different populations.
Regarding age, in the current study, we found a statistically significant difference between the two groups regarding the age at onset (p = 0.041), where the diagnostic delay was more common at a younger age of onset. This was consistent with a previous Egyptian study from Ain Shams University, which found that those younger at the onset of MS experienced diagnostic delays, and denial of symptoms was a leading cause of delayed time to first medical consultation23. Furthermore, studies from Canada, Denmark, and the United States of America found that younger onset patients had significantly longer delays, which could be explained by the fact that younger people seek care less frequently, contributing to the longer time to diagnosis14,24,25. In contrast, In Portuguese, older age at onset was associated with a longer time to diagnosis, which was primarily explained by a broader age-related differential diagnosis of MS12. In Colombia, no link was found between age at onset and delayed diagnosis16. These differences between studies could be also attributed to differences in MS prevalence, differences in MS risk factors leading to the variability of the age at onset in different countries, or even different paths of access to the diagnostic facilities18.
When patients were compared based on their gender, no statistically significant difference between males and females regarding the time to reach MS diagnosis (U = 0.415). There were no differences between both groups regarding the first speciality sought, previous misdiagnosis, frequency of relapses or the current EDSS scores. These findings regarding the difference between gender were in line with the previous reports6,14,16,19,26. In contrast to the study from Iran, patient delay in seeking medical advice was noted in men compared to women18. This was explained by the men’s delayed help-seeking behavior, thus potentially hindering diagnostic processes27.
Although it was theoretically hypothesized that the presence of a spouse might shorten the time needed to diagnose by the earlier discerning of symptoms and encouraging early medical consultation, we could not find a statistically significant difference between the mean diagnostic delay and marital status. Not many studies specifically looked at how marital status affects the time to MS diagnosis. Still, one Iranian study found that married patients experienced shorter diagnostic delays than single patients18.
Regarding education, no statistically significant difference was found between patients with a low educational level compared to those with higher levels in the mean diagnostic delay, contrasting some other reports from the literature18.
From a clinical perspective, the initial symptoms could affect the time to diagnosis, where syndromes typical for MS prompt immediate diagnosis while other symptoms might be vague and lead to various differential diagnoses. In the current study, patients with motor versus non-motor onset had a statistically significant difference in the median diagnostic delay. While In Portuguese, the motor deficits were associated with a long diagnostic delay, as the minority first examined by a neurologist explaining part of this delay19. Although most studies reported that onset symptoms were independently associated with diagnostic delay, the exact onset symptom associated with such delays was contrasted in different studies from different countries. For example, optic neuritis was associated with a shorter diagnostic delay in Spain15 and Iran18, owing to an earlier presentation to neurologists. In contrast to the Canadian and Danish cohorts, optic neuritis was associated with lengthier time to MS diagnosis, which was explained by the rapidly resolving nature of the symptom14,24. Contrasting reports on the sensory symptoms at the debut of illness also exist, where in the Canadian cohort28 was associated with a shorter time to diagnosis, in contrast to the previous study from Egypt as well as the Iranian cohorts where it was associated with a longer delay explained by being a non-specific presentation that can be linked to several etiologies13,23.
Patients can present to doctors of different specialties depending on the nature of their symptoms (e.g., general practitioners, ophthalmologists, orthopedics, or neurosurgeons), and if MS is suspected, a consultation of a neurologist or even MS specialist is needed29. Almost half of the patients in the current study were first examined by a non-neurological specialty, a factor that independently predicted the diagnostic delay when compared to patients seen by neurologists (p < 0.001). On examining the literature, considerable delays result from delayed contact with an MS expert, which impact treatment options and the chance for early intervention14. This finding was supported by an international multicentric study that assessed neurologist's knowledge of MS diagnosis and treatment and found that 27% of neurologists had no or only basic awareness of the 2017 McDonald criteria, and more than one-third of neurologists had no or only basic understanding of atypical MS presentations30. Although ophthalmology and orthopedic services were the first specialties consulted in the previous Egyptian study (as in the current study), the most prevalent referral source to a neurologist was family and media recommendations23. So, increasing the awareness of MS symptoms among laypeople, primary care practitioners, and general neurologists might reduce the time to MS diagnosis.
In the current study, 56.3% of the patients received a previous misdiagnosis leading to a statistically significant delay in the mean diagnostic time (p < 0.001) and was an independent predictor of the diagnostic delay. Almost half of the patients in the Portuguese cohort have also received an incorrect prior diagnosis, which led to a longer delay in MS diagnosis19.
As was evident in the current study, the number of patients with a delayed diagnosis has decreased over time, and the time to diagnosis has shortened significantly. Also, presentation in earlier periods was an independent predictor for the diagnostic delay, in concordance with previous findings13,14,15,16. A possible explanation might be the increased awareness of the neurological symptoms among the public, alongside the updated MS diagnostic criteria over the years, making it easier to confirm the diagnosis earlier. More importantly, the approval and availability of several treatment options supported by either insurance or government funding have increased awareness of MS among neurologists13.
Despite the latest advances in MS management and increasing availability of DMTs in Egypt's healthcare insurance and governmental funding systems in the last few years, seeking a non-neurologist at initial presentation and previous misdiagnoses are significant factors to the delayed diagnosis in Upper Egypt.
The most important barrier was the lack of an appropriate case registry, with many patients not remembering important data and dates regarding their disease course. Also missing radiological data at the initial presentation together with the use of different MRI machines without a standard MS protocol have limited further analysis of these data as possible factors for the diagnostic delay. Other factors could be evaluated in further studies, like the costs of the specialist visits, the investigatory tools like MRI, CSF Oligoclonal bands, and electrophysiological studies alongside their availability. Moreover, large-scale nationwide studies are recommended.
Methods
Participants
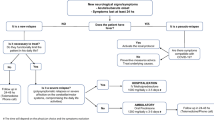
One hundred ninety patients diagnosed with RRMS on DMTs were recruited from three MS centers. Patients were adults of both sexes diagnosed with RRMS according to the 2017 McDonald’s criteria31. After excluding patients with any clinical or radiological finding suggestive of demyelinating diseases other than MS, patients with systemic disease or on long-term treatments, patients with incomplete clinical or radiological data, or patients who declined to provide written informed consent, 142 patients were included in the study (Fig. 1).
Study procedures
This cross-sectional, multicenter, hospital-based observational study included three MS units from three governorates in Upper Egypt (Assiut, Qena, and Luxor). After meeting the inclusion and exclusion criteria, all eligible cases with MS were interviewed and examined by specialized neurologists. Different demographic data, complete clinical data, a complete neurological examination, including the Expanded Disability Status Scale (EDSS) application, and revision of various radiological, electrophysiological, and CSF examinations were collected.
Ethics
This study was approved by the Local Ethics Committee of Faculty Medicine, South Valley University (IRB no: SUV MED NAP020220756) and was conducted in accordance with the provisions of the Declaration of Helsinki. Also, written informed consent from all participants was obtained after the description of the aim of the study and methods before participation in the study.
Statistical analysis of data
The IBM Statistical Package for Social Sciences version 20.0 was used for data analysis (Armonk, NY: IBM Corp). The qualitative variables were described using ratios and percentages. The Shapiro–Wilk test was used to confirm the normality of the distribution. Quantitative variables with normal distributions were reported using mean and SD, while those without normal distributions were described using median and mid-quartiles. The level of statistical significance was set at p 0.05. Diagnostic delay was analysed as a dichotomous variable and classified as an early diagnosis (diagnosed within the first three months) or a delayed diagnosis (diagnosed beyond three months). We chose three months as the time frame suggested by NICE guidelines17, after which diagnosis is considered delayed. The delayed diagnosis was the considered outcome variable, and multivariate logistic regression analysis was employed to identify variables that can be regarded as independent predictors of diagnosis delay.
Data availability
Data can be made available to qualified investigators upon reasonable request to the corresponding author.
References
Stenager, E. A global perspective on the burden of multiple sclerosis. Lancet Neurol. 18(3), 227–228. https://doi.org/10.1016/S1474-4422(18)30498-8 (2019).
Stahnke, A. M. & Holt, K. M. Ocrelizumab: A new B-cell therapy for relapsing remitting and primary progressive multiple sclerosis. Ann. Pharmacother. 52(5), 473–483. https://doi.org/10.1177/1060028017747635 (2018).
Derfuss, T. et al. Advances in oral immunomodulating therapies in relapsing multiple sclerosis. Lancet Neurol. 19(4), 336–347. https://doi.org/10.1016/S1474-4422(19)30391-6 (2020).
Moradi, N. et al. Utilization of multiple sclerosis therapies in the middle east over a decade: 2009–2018. CNS Drugs 35(10), 1097–1106. https://doi.org/10.1007/s40263-021-00833-w (2021).
Damal, K., Stoker, E. & Foley, J. F. Optimizing therapeutics in the management of patients with multiple sclerosis: A review of drug efficacy, dosing, and mechanisms of action. Biologics Targets Ther. 2013(7), 247–258. https://doi.org/10.2147/BTT.S53007 (2013).
Giovannoni, G. et al. Brain health: Time matters in multiple sclerosis. Multiple Sclerosis Relat. Disord. 9, S5–S48. https://doi.org/10.1016/j.msard.2016.07.003 (2016).
Gaitán, M. I. & Correale, J. Multiple sclerosis misdiagnosis: A persistent problem to solve. Front. Neurol. 10(MAY), 466. https://doi.org/10.3389/fneur.2019.00466 (2019).
Kelly, S. B. et al. Multiple sclerosis, from referral to confirmed diagnosis: An audit of clinical practice. Mult. Scler. J. 17(8), 1017–1021. https://doi.org/10.1177/1352458511403643 (2011).
Yamout, B. I., Assaad, W., Tamim, H., Mrabet, S. & Goueider, R. Epidemiology and phenotypes of multiple sclerosis in the Middle East North Africa (MENA) region. Multiple Sclerosis J. Exp. Transl. Clin. 6(1), 4–9. https://doi.org/10.1177/2055217319841881 (2020).
Scalfari, A. et al. Mortality in patients with multiple sclerosis. Neurology 81(2), 184. https://doi.org/10.1212/WNL.0B013E31829A3388 (2013).
Ziemssen, T. et al. Optimizing treatment success in multiple sclerosis. J. Neurol. 263(6), 1053–1065. https://doi.org/10.1007/s00415-015-7986-y (2016).
Waubant, E. Improving outcomes in multiple sclerosis through early diagnosis and effective management. Prim. Care Companion CNS Disord. 14(5), 11016. https://doi.org/10.4088/PCC.11016co2cc (2012).
Mobasheri, F., Jaberi, A. R., Hasanzadeh, J. & Fararouei, M. Multiple sclerosis diagnosis delay and its associated factors among Iranian patients. Clin. Neurol. Neurosurg. 1(199), 106278 (2020).
Kingwell, E. et al. Factors associated with delay to medical recognition in two Canadian multiple sclerosis cohorts. J. Neurol. Sci. 292(1), 57–62 (2010).
Fernández, O. et al. Characteristics of multiple sclerosis at onset and delay of diagnosis and treatment in Spain (The Novo Study). J. Neurol. 257(9), 1500–1507. https://doi.org/10.1007/s00415-010-5560-1 (2022).
Cárdenas-Robledo, S., Lopez-Reyes, L., Arenas-Vargas, L. E., Carvajal-Parra, M. S. & Guío-Sánchez, C. Delayed diagnosis of multiple sclerosis in a low prevalence country. Neurol. Res. 43(7), 521–527. https://doi.org/10.1080/01616412.2020.1866374 (2021).
National Institute for Health and Clinical Excellence Guidelines, 2004. http://www.nice.org.uk/nicemedia/live/10930/46699/46699.pdf
Ghiasian, M., Faryadras, M., Mansour, M., Khanlarzadeh, E. & Mazaheri, S. Assessment of delayed diagnosis and treatment in multiple sclerosis patients during 1990–2016. Acta Neurol. Belg. 121(1), 199–204. https://doi.org/10.1007/s13760-020-01528-7 (2021).
Aires, A. et al. Diagnostic delay of multiple sclerosis in a portuguese population. Acta Med. Port. 32(4), 289–294. https://doi.org/10.20344/amp.11187 (2019).
Adamec, I., Barun, B., Gabelić, T., Zadro, I. & Habek, M. Delay in the diagnosis of multiple sclerosis in Croatia. Clin. Neurol. Neurosurg. 115(1), S70–S72. https://doi.org/10.1016/j.clineuro.2013.09.025 (2013).
Thormann, A. et al. Comorbidity in multiple sclerosis is associated with diagnostic delays and increased mortality. Neurology 89(16), 1668–1675. https://doi.org/10.1212/WNL.0000000000004508 (2017).
Marrie, R. A. A. et al. Comorbidity delays diagnosis and increases disability at diagnosis in MS. Neurology 72(2), 117–124. https://doi.org/10.1212/01.WNL.0000333252.78173.5F (2009).
Tohamy, A. A., Swelam, M. S., Abdelgawad, D. M. & Aref, H. A. Causes of delayed diagnosis of multiple sclerosis in egypt. QJM Int. J. Med. https://doi.org/10.1093/QJMED/HCAA054.011 (2020).
Esbjerg, S., Keiding, N. & Koch-Henriksen, N. Reporting delay and corrected incidence of multiple sclerosis. Stat. Med. 18(13), 1691–1706. https://doi.org/10.1002/(sici)1097-0258(19990715)18:13%3c1691::aid-sim160%3e3.0.co (1999).
Marrie, R. A. et al. Changes in the ascertainment of multiple sclerosis. Neurology 65(7), 1066–1070. https://doi.org/10.1212/01.WNL.0000178891.20579.64 (2005).
Kaufmann, M. et al. Factors associated with time from first-symptoms to diagnosis and treatment initiation of multiple sclerosis in Switzerland. Mult. Scler. J. Exp. Transl. Clin. 4(4), 205521731881456 (2018).
Eccles, A. Debate and analysis delayed diagnosis of multiple sclerosis in males: may account for and dispel common understandings of different MS “types”. Br. J. Gen. Pract. 69(680), 148–149 (2019).
Kaisey, M., Solomon, A. J., Luu, M., Giesser, B. S. & Sicotte, N. L. Incidence of multiple sclerosis misdiagnosis in referrals to two academic centers. Mult. Scler. Relat. Disord. 30, 51–56. https://doi.org/10.1016/j.msard.2019.01.048 (2019).
Brownlee, W. J., Hardy, T. A., Fazekas, F. & Miller, D. H. Diagnosis of multiple sclerosis: progress and challenges. Lancet 389(10076), 1336–1346. https://doi.org/10.1016/S0140-6736(16)30959-X (2017).
Péloquin, S. et al. Challenges in multiple sclerosis care: Results from an international mixed-methods study. Mult. Scler. Relat. Disord. 50, 102854 (2021).
McNicholas, N., Hutchinson, M., McGuigan, C. & Chataway, J. 2017 McDonald diagnostic criteria: A review of the evidence. Multiple Sclerosis Relat. Disord. 24, 48–54. https://doi.org/10.1016/j.msard.2018.05.011 (2018).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
E.M.K., A.G., I.E.M., H.B.H., D.M.M., contributed to study concept and design, acquisition of data, draft and revision of the report, statistical analyses, and interpretation of data. H.B.H., D.M.M., contributed to case recruitments, acquisition of data and statistical analyses. E.M.K., D.M.M. contributed to editing of this report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khedr, E.M., El Malky, I., Hussein, H.B. et al. Multiple sclerosis diagnostic delay and its associated factors in Upper Egyptian patients. Sci Rep 13, 2249 (2023). https://doi.org/10.1038/s41598-023-28864-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28864-x
- Springer Nature Limited
This article is cited by
-
EDSS and infratentorial white matter lesion volume are considered predictors of fatigue severity in RRMS
Scientific Reports (2023)