Abstract
Hemoglobin variability is known to increase cardiovascular mortality in chronic kidney disease, but the association of hemoglobin variability with the risk of cardiovascular disease (CVD) in the general population is yet unclear. This retrospective cohort study based on ‘the South Korean National Health Insurance Service database’ consisted of 198,347 adults who went through all three health examinations. Hemoglobin variability is defined as the average successive variability of three separate hemoglobin values from each health screening period. Participants were followed up for 6 years to determine the risk of coronary heart disease and stroke. We used multivariate Cox proportional hazards regression to examine the adjusted hazard ratios for CVD according to hemoglobin variability. Per 1 unit increase of hemoglobin variability, the risk for CVD (aHR 1.06, 95% CI 1.02–1.09) and stroke (aHR 1.08, 95% CI 1.03–1.13) increased significantly. The risk-increasing trend was preserved in the low-to-moderate risk group of CVDs (aHR 1.07, 95% CI 1.02–1.11). This result suggests that subjects with high hemoglobin variability who would otherwise be categorized as having low-to-moderate CVD risk may have higher risk of CVD than those with low hemoglobin variability.
Similar content being viewed by others
Introduction
The Global Burden of Disease study reported that cardiovascular diseases (CVDs) are one of the primary causes of death worldwide1. Although the CVD mortality in high-income countries has been decreased for the past half-century, the decline rate has slowed down2. In addition, those who survived from cardiovascular event will still experience serious sequela such as arrhythmias or physical disability. Thus, it is important to prevent CVD by identifying and managing CVD risk factors prior to cardiovascular event development. Metabolic parameters such as cholesterol level3, glucose level4, blood pressure5, and body weight6 are well-known risk factors of CVD. Moreover, the variability of such parameters over time, which reflects the dysregulation of homeostasis, has also previously been shown to be associated with the increased risk of CVD7,8,9,10,11. The variability of hemoglobin levels has been demonstrated to be associated with the increased cardiovascular mortality, only in patients with chronic kidney disease (CKD)12. However, hemoglobin variability in the general population is not fully studied as a potential risk factor of CVD, while low hemoglobin concentration and change in hemoglobin levels were shown to be risk factors for CVD13,14.
In the general population, high hemoglobin variability is related to the increased all-cause mortality15. Another study examined that high hemoglobin variability is associated with higher risk of hypertension in the general population16. Since the leading cause of mortality is CVD globally1, and that hypertension is one of the main risk factors of CVD5, it is reasonable to assume that the risk of CVD also may be elevated with high hemoglobin variability. In fact, hemoglobin variability reflects the inflammatory state and repeated anemic stimuli which are considered to increase the risk of CVDs by triggering atherosclerosis and ventricular hypertrophy, respectively17,18. Thus, there is a need for more studies about the impact of hemoglobin variability on subsequent CVD outcomes.
We, therefore, aimed to determine the association between hemoglobin variability and the risk of CVD using the National Health Insurance Service (NHIS) database from South Korea.
Methods
Study design
This retrospective cohort study is based on the National Health Insurance Service—National Health Screening Cohort (NHIS-HEALS) database during 2002–2013. The national health screening for South Korean aged 40 years or more is performed biannually by the National Health Insurance which covers 97% of all citizens of South Korea19. The health examination includes basic physical examinations assessing the body mass index (BMI) and blood pressure, blood test detecting biochemical indicators such as total cholesterol, fasting serum glucose (FSG), and hemoglobin concentration, and self-reported questionnaires consisted of multiple-choice questions regarding health behavior and medical history. To construct the NHIS-HEALS database, the NHIS used the simple random sampling method and combined health examination information with clinical information such as hospital use, diagnoses, and death. Numerous epidemiological studies have used this database previously, and its applicability has been demonstrated elsewhere20.
Study population
Among 264,480 subjects over 40 years old who went through all three health examinations in the first (2002–2003), second (2004–2005), and third (2006–2007) periods, 47,248 individuals who were already diagnosed with CVD or died before the index date of 1 January 2008 were excluded (Fig. 1). In addition, we excluded 369 participants who did not have values for hemoglobin levels, and 18,516 participants who lacked information on other covariates. A total of 198,347 participants were included in this study.
Ethical approval
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. This study was approved by the Seoul National University Hospital Institutional Review Board (IRB number: 1703-039-836). The requirement for informed consent was waived as the NHIS database was anonymized according to strict confidentiality guidelines prior to distribution.
Data use
The data from this study is directly available via the NHIS database registration system and thus cannot be allowed for other researchers to access when they are intended to replicate the procedures.
Exposure: hemoglobin variability
We calculated hemoglobin variability using the average successive variability (ASV) method21,22. Firstly, we took hemoglobin values from three health examinations. Then we subtracted the values from second to first examination, and third to second examination to get the differences. We calculated the average of those two differences of hemoglobin values.
Outcome: cardiovascular disease
The primary outcome of this study is CVDs which is divided into coronary heart diseases (CHDs) and strokes according to the American Heart Association (AHA) guidelines23. We defined CVD events as hospitalization for 2 days or more with CHDs or strokes from January 1, 2008 to December 31, 2013 to minimize the possibility of misdiagnoses. We used the International Classification of Diseases, Tenth Revision (ICD-10) codes to identify CHDs (I20–I25) and strokes (I60–I69). Previous studies suggest that it is accurate to define CVD based on the ICD-10 code24.
Covariates
We included sex, age, household income (first, second, third, or fourth quartiles), initial hemoglobin concentration, change in hemoglobin levels, smoking state (never, pass, or current smoker), alcohol consumption (0, 1–2, 3–4, 5–6, or 7 times per week), Charlson comorbidity index (CCI), systolic blood pressure, total cholesterol, and BMI as possible confounding covariates. The initial hemoglobin concentration is the hemoglobin value from the first examination, and the change in hemoglobin levels was calculated by subtracting hemoglobin levels of the first examination from those of the third examination. We divided body weight by height squared to calculate BMI, and household income was categorized by insurance premium. CCI is the most extensively used comorbidity index25, which includes the risk of various comorbidities such as kidney disease, chronic lung disease, liver disease, dementia, and malignant tumors26. We also used the European Society of Cardiology (ESC) Systemic Coronary Risk Estimation (SCORE) for a subgroup analysis. It is a reasonable tool recommended by the ESC to estimate an individual’s 10-year risk of future fatal CVD using age, sex, systolic blood pressure, smoking state, and total cholesterol level29. We used the low-risk SCORE chart which is established for the European countries of which 2016 CVD mortality rate was under 150 per 100,000, based on the 2016 age-adjusted CVD mortality in WHO data from the Global Burden of Disease Study29,30.
Statistical analysis
We used Multivariate cox proportional hazards regression to examine the adjusted hazard ratios (aHRs) and confidence intervals (CIs) of 95% for CVDs, CHDs and strokes. We considered the p value under 0.05 as statistically significant. We also used restricted cubic spline regression model to present the continuous relationship between hemoglobin variability and the aHRs of CVD risk27. Referring to previous studies, we placed 4 knots at the 5th, 35th, 65th, 95th percentiles of hemoglobin variability15,28. Considering potential bias due to other causes before the follow-up investigation, 1- and 2-year of latent periods were washed out for sensitivity analyses. In addition, we performed stratified analyses according to several confounding factors: age, physical activity, smoking state, alcohol consumption, CCI, hemoglobin concentration, and change in hemoglobin levels. We also performed subgroup analyses according to the ESC SCORE. Individuals who got ESC SCORE lower than 5% are considered as low-to-moderate risk groups for future fatal CVD, according to the European Atherosclerosis Society (EAS) and ESC guidelines29. Data collection was performed by SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA), and conducted all statistical analyses by STATA version 13 (StataCorp, College Station, Texas, USA).
Results
Among the total cohort of 198,347, the number (%) of men and women were 116,016 (58.5) and 82,331 (41.5). The average follow-up duration of total cohort is 5.8 years. Baseline characteristics of total cohort, men and women are demonstrated in Table 1. The mean age [standard deviation (SD)] of total cohort is 55.3 (8.5) years. The mean value (SD) of hemoglobin variability (ASV), initial hemoglobin concentration, and change of hemoglobin levels of total cohort were 0.9 (0.6) g/dL, 14.0 (1.5) g/dL, and 0.2 (1.2) g/dL, respectively. The mean (SD) BMI was 23.9 (2.8) kg/m2; systolic blood pressure, 125.1 (15.9) mmHg; FSG, 97.6 (24.8) mg/dL; and total cholesterol, 198.9 (36.2) mg/dL. Among total participants, 39% were categorized as the highest quartile of household income, 47% reported that they do not exercised, and 68.7% had 1 or lower CCI scores. More than half of the participants were reported as non-alcohol consumers (56.9%) and never smokers (70.6%).
During follow-up duration, CVD, CHD, stroke events each occurred 8687 (4.4%), 4001 (2.0%), and 4744 (2.4%) in the total cohort. The numbers of CVD, CHD, stroke events per each year in the follow-up duration are shown in the Supplementary Table S1. The association between hemoglobin variability and the risk of CVD, CHD and stroke is shown in Table 2. The risk of CVD was elevated per 1 unit increase of hemoglobin variability for the total cohort (aHR 1.06, 95% CI 1.02–1.09) as well as for men (aHR 1.06, 95% CI 1.02–1.11) and women (aHR 1.06, 95% CI 1.00–1.12). The risk of stroke also increased in total cohort (aHR 1.08, 95% CI 1.03–1.13), men (aHR 1.07, 95% CI 1.01–1.14) and women (aHR 1.08, 95% CI 1.01–1.16) per 1 unit increase of hemoglobin variability. The risk-increasing trends of CVD and stroke were preserved in sensitivity analyses after washing out 1-year latent period (see Supplementary Table S2). However, the risk-increasing trend of CHD was not statistically significant.
The aHRs of the covariates for CVD are provided in Supplementary Table S3. Among various confounders, age, initial hemoglobin level, income, smoking state, BMI and CCI showed relatively strong contribution to CVD risk.
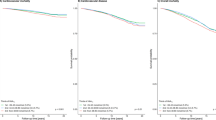
The association of hemoglobin variability with the risk of CVD is plotted by restricted cubic spline regression in Fig. 2. The higher hemoglobin variability was related to the increased risk of CVD in a dose-responsive manner for total cohort as well as in both men and women. We also plotted Restricted cubic spline graph to show the result of subgroup analyses by ESC SCORE in Fig. 3. Higher hemoglobin variability was significantly associated with the elevated risk of CVD for the low-to-moderate risk group (aHR 1.07, 95% CI 1.02–1.11).
Restricted cubic spline graph of hazard ratio for cardiovascular disease in total cohort (a), men (b) and women (c). Hazard ratio is calculated by Cox proportional hazards regression analysis after adjustments for age, sex, initial hemoglobin level, change in hemoglobin level, household income, smoking, alcohol consumption, physical activity, systolic blood pressure, fasting serum glucose, total cholesterol, and Charlson comorbidity index. CI confidence interval.
Restricted cubic spline graph of hazard ratio for cardiovascular disease in the subgroups of ESC SCORE : Low-to-moderate risk group (a) and High risk group (b). Hazard ratio is calculated by Cox proportional hazards regression analysis after adjustments for age, sex, initial hemoglobin level, change in hemoglobin level, household income, smoking, alcohol consumption, physical activity, systolic blood pressure, fasting serum glucose, total cholesterol, and Charlson comorbidity index. P value for interaction between the subgroups is 0. 434. ESC SCORE European Society of Cardiology Systemic Coronary Risk Estimation, aHR adjusted hazard ratio, CI confidence interval.
Results from stratified analyses according to the age, physical activity, smoking state, alcohol consumption, CCI, hemoglobin concentration, and change direction in hemoglobin levels are demonstrated in Table 3. As the hemoglobin variability increases, the risk of CVD elevated in both 60 years or older (aHR 1.07, 95% CI 1.02–1.12) and younger than 60 years old (aHR 1.05, 95% CI 1.00–1.10). When stratified by physical activity, smoking state, and alcohol consumption, one unit increase of hemoglobin variability was associated with the elevated risk of CVD in all subgroups: never smokers (aHR 1.06, 95% CI 1.02–1.11), ever smokers (aHR 1.06, 95% CI 1.00–1.12), non-alcohol consumers (aHR 1.06, 95% CI 1.02–1.11), and alcohol consumers (aHR 1.05, 95% CI 1.00–1.11). Both participants who got CCI scores of 0–1 (aHR 1.07, 95% CI 1.03–1.12) and those with CCI scores ≥ 2 (aHR 1.05, 95% CI 1.00–1.11) showed increased risk of CVD in the total cohort. When divided by whether participants had the hemoglobin concentration of anemia at least once among three health examinations or not, only those without anemia at all showed significantly higher risk of CVD (aHR 1.07, 95% CI 1.02–1.11). When stratified by the direction of change between hemoglobin levels, only those who had increased hemoglobin concentration in the third examination compared to the first examination showed significantly elevated risk of CVD (aHR 1.07, 95% CI 1.02–1.12). However, all of the p-values for interaction between subgroups of each confounder were not statistically significant.
Discussion
In this retrospective cohort study, we observed that high hemoglobin variability was significantly associated with increased risk of CVD. To our knowledge, this was the first large population-based study on the association of hemoglobin variability with the risk of CVD in the general population.
Most previous studies regarding hemoglobin variability focused on patients with CKD12,31. One study examined that 1 SD increase of hemoglobin variability in hemodialysis patients was associated with a 10% increase in cardiovascular death rate12. With regard to the general population, there is a study which determined that 5% SD elevation of hemoglobin variability was related to 8% increase in all-cause mortality15. In another study using the general population, the highest hemoglobin variability group had 9% higher hazard ratio of hypertension than the lowest group16. In this study, we observed that 1 unit elevation of hemoglobin variability was related to the higher risk of CVDs in the general population.
Hemoglobin concentration or its variability may be affected by various factors including demographic characteristics, such as gender, age32, behavioral factors, such as exercise33, and, smoking34, biochemical indicators, such as plasma volume35, medications, such as iron preparations36, and erythropoiesis-stimulating agents37,38, and clinical state, such as inflammation, infection39, and malignancies40. Among those factors, there are several possible mechanisms to explain how high hemoglobin variability could increase the risk of CVD. First, high hemoglobin variability can cause left ventricular hypertrophy (LVH)15,41. In chronic anemia, the growth of myocardial cell is stimulated and cardiac output increases as compensation for the decreased number of red blood cells41. When there is high variability in hemoglobin levels, anemic stimuli would be repeated, which can eventually cause enlargement of ventricles15. LVH is proved to be an accurate marker of CVD42, and also has been examined to be a prognostic factor independent of hypertension43. Second, hemoglobin variability may be a marker of underlying active inflammatory response, which is related to an elevated risk of CVD. Inflammatory cytokines like Tumor Necrosis Factor-alpha (TNF-α) and Interferon-γ (IFN-γ) can cause high hemoglobin variability by interfering the differentiation of erythroid progenitor cells and the production of erythropoietin in the kidneys, and limiting iron availability for erythrocytes18. Inflammation plays an important role throughout all stages of atherosclerosis which is in turn closely related with cardiovascular risks17.
To assess the possible confounding effect of behavioral factors, including alcohol consumption, physical activity, and smoking state, age, and comorbidities, we performed stratified analyses according to the subgroups of those factors. Previous studies found that CKD patients with higher hemoglobin concentration were more likely to be physically active than those with lower concentration44. Physical activity is associated with the decreased risk of CHD45 and stroke46, which decreases the risk of CVD by lowering other risk factors like inflammation and blood pressure47. Additionally, smoking state can also alter the hemoglobin concentration34. In all subgroups of the total cohort, higher hemoglobin variability was related to the increased risk of CVD regardless of such confounding factors. Age is also considered to be a major risk factor of CVD48, and hemoglobin level tends to decrease as age increases, especially in men49. When stratified by age, the risk-increasing trend was also preserved in all subgroups of total cohort. Comorbidities such as chronic renal disease is also a well-known risk factor of CVD events50. To take this into account, we used Charlson comorbidity index (CCI) which is a measure of overall comorbidity status25. We also found that the risk-increasing association was preserved despite the subgroups of CCI in total cohort.
In previous studies, the risk of CVD can be elevated by the underlying anemia and the change of hemoglobin levels13,14. Thus, we conducted stratified analysis by whether participants had hemoglobin concentration of anemia at least once among three health examinations or not, and by the change direction in hemoglobin levels. Although only subgroups of anemia and increasing hemoglobin group showed significantly increasing hazard ratios, we can expect that hemoglobin variability could have an independent effect on CVD excluding the effect of anemia and hemoglobin change since p-values for interaction between subgroups were not statistically significant. These results of subgroup analyses suggest that hemoglobin variability could be a meaningful risk factor of CVD regardless of other confounders.
To further investigate the clinical implications of hemoglobin variability among generally healthy populations, we conducted a subgroup analysis of those who were low-to-moderate risk according to the ESC SCORE which predicts 10-year risk of future fatal CVD29. High hemoglobin variability was significantly associated with increased risk of CVD even in the low-to-moderate risk group of ESC SCORE. Compared to the high risk population who have many other screening clinical indicators like high blood pressure or serum lipid level, there is a relative lack of effective predictors of the CVD risk for low-to-moderate risk population. On the basis of this subgroup analysis, we can consider hemoglobin variability as a useful biomarker for stratifying the risk of CVD among the low-to-moderate risk group classified by a well-established risk score.
There are several limitations in this study. First, the risk of CVD could be underestimated due to the operational definition of CVD events. We defined the incidence of CVD as hospitalization for 2 days or more with coronary heart diseases or strokes to minimize the possibility of misdiagnosis with reference to previous studies regarding CVD events51,52,53. Although this definition is still missing the sudden death from cardiovascular diseases which imply fatal CVD cases, the risk-increasing trend was significant despite the possibility of underestimation. Second, this study has the probability of selection bias by limiting the study population to those who took all three health examinations in the given period. To quantify the effect of selection bias, we compared descriptive characteristics such as age, sex, income and CCI between the study population and the others who did not take all three health examinations (see Supplementary Table S4). P-values show that those descriptive characteristics are significantly different between those two groups, and this result implies the possibility of selection bias. Therefore, we need further studies to find out the association of hemoglobin variability and CVD in the excluded group. Third, the database we used was missing several confounders of which the association with hemoglobin concentration or the risk of CVD is proved by previous studies. It is well known that inflammation can alter hemoglobin levels, but we could not detect inflammatory markers such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR)18. Hemoglobin concentration can be also affected by various coexisting diseases, including CKD54 and chronic obstructive pulmonary disease55. Although we could not adjust all of the comorbidities separately, we used CCI in which the risk of chronic pulmonary disease, renal disease, and other various comorbidities are considered26. In fact, we found that high hemoglobin variability is associated with increased risk of CVD even in the subgroup of CCI values of 2 or less, in which most chronic diseases were excluded. Further studies adjusting these missing covariates are necessary to prove the independent effect of hemoglobin variability on the risk of CVD. Fourth, since the study design is retrospective cohort, additional studies are needed to prove the exact causal relationship between hemoglobin variability and CVD. Finally, since the study population is 40 years or older South Korean adults, this study may not be enough for generalization to other countries.
In conclusion, individuals with high hemoglobin variability are more likely to suffer from CVD in the future, compared to those with low variability. Hemoglobin variability may be a meaningful risk factor of CVD in the general population. Specifically, when individuals who were categorized as the low-to-moderate CVD risk group by well-established CVD risk assessment scores show high hemoglobin variability, it may be beneficial to closely follow-up these subjects for early signs and symptoms of CVD.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Collaborators, G. B. D. C. O. D. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1736–1788. https://doi.org/10.1016/S0140-6736(18)32203-7 (2018).
Lopez, A. D. & Adair, T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int. J. Epidemiol. 48, 1815–1823. https://doi.org/10.1093/ije/dyz143 (2019).
Anderson, K. M., Castelli, W. P. & Levy, D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA 257, 2176–2180. https://doi.org/10.1001/jama.257.16.2176 (1987).
Park, C. et al. Fasting glucose level and the risk of incident atherosclerotic cardiovascular diseases. Diabetes Care 36, 1988–1993. https://doi.org/10.2337/dc12-1577 (2013).
Kannel, W. B., Dawber, T. R. & McGee, D. L. Perspectives on systolic hypertension. The Framingham study. Circulation 61, 1179–1182. https://doi.org/10.1161/01.cir.61.6.1179 (1980).
Wilson, P. W., D’Agostino, R. B., Sullivan, L., Parise, H. & Kannel, W. B. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch. Intern. Med. 162, 1867–1872. https://doi.org/10.1001/archinte.162.16.1867 (2002).
Kim, M. K. et al. Associations of variability in blood pressure, glucose and cholesterol concentrations, and body mass index with mortality and cardiovascular outcomes in the general population. Circulation 138, 2627–2637. https://doi.org/10.1161/CIRCULATIONAHA.118.034978 (2018).
Kim, M. K. et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: A nationwide population-based study. Eur. Heart J. 38, 3560–3566. https://doi.org/10.1093/eurheartj/ehx585 (2017).
Gosmanova, E. O. et al. Association of systolic blood pressure variability with mortality, coronary heart disease, stroke, and renal disease. J. Am. Coll. Cardiol. 68, 1375–1386. https://doi.org/10.1016/j.jacc.2016.06.054 (2016).
Choi, S. et al. Impact of visit-to-visit variability in systolic blood pressure on cardiovascular outcomes in Korean national health insurance service-national sample cohort. Am. J. Hypertens. 30, 577–586. https://doi.org/10.1093/ajh/hpw157 (2017).
Xu, D. et al. Fasting plasma glucose variability and all-cause mortality among type 2 diabetes patients: A dynamic cohort study in Shanghai, China. Sci. Rep. 6, 39633. https://doi.org/10.1038/srep39633 (2016).
Lin, F. J. et al. Impact of hemoglobin variability on cardiovascular mortality in maintenance hemodialysis patients. Int. Urol. Nephrol. 50, 1703–1712. https://doi.org/10.1007/s11255-018-1919-5 (2018).
Lee, G. et al. Association of hemoglobin concentration and its change with cardiovascular and all-cause mortality. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.117.007723 (2018).
Lee, G. et al. Association between changes in hemoglobin concentration and cardiovascular risks and all-cause mortality among young women. J. Am. Heart Assoc. 7, e008147. https://doi.org/10.1161/JAHA.117.008147 (2018).
Son, M. & Yang, S. Association between long-term hemoglobin variability and mortality in Korean adults: A nationwide population-based cohort study. Sci. Rep. 9, 17285. https://doi.org/10.1038/s41598-019-53709-x (2019).
Son, M., Park, J., Park, K. & Yang, S. Association between hemoglobin variability and incidence of hypertension over 40 years: A Korean national cohort study. Sci. Rep. 10, 12061. https://doi.org/10.1038/s41598-020-69022-x (2020).
Libby, P. Inflammation and cardiovascular disease mechanisms. Am. J. Clin. Nutr. 83, 456S-460S. https://doi.org/10.1093/ajcn/83.2.456S (2006).
Weiss, G. & Goodnough, L. T. Anemia of chronic disease. N. Engl. J. Med. 352, 1011–1023. https://doi.org/10.1056/NEJMra041809 (2005).
Cheol Seong, S. et al. Data resource profile: The national health information database of the national health insurance service in South Korea. Int. J. Epidemiol. 46, 799–800. https://doi.org/10.1093/ije/dyw253 (2017).
Lee, J., Lee, J. S., Park, S. H., Shin, S. A. & Kim, K. Cohort profile: The national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46, e15. https://doi.org/10.1093/ije/dyv319 (2017).
Bangalore, S. et al. Body-weight fluctuations and outcomes in coronary disease. N. Engl. J. Med. 376, 1332–1340. https://doi.org/10.1056/NEJMoa1606148 (2017).
Choi, D., Choi, S. & Park, S. M. Impact of weight variability on mortality among Korean men and women: A population based study. Sci. Rep. 9, 9543. https://doi.org/10.1038/s41598-019-46037-7 (2019).
Writing Group, M. et al. Executive summary: Heart disease and stroke statistics–2016 update: A report from the American Heart Association. Circulation 133, 447–454. https://doi.org/10.1161/CIR.0000000000000366 (2016).
Park, J. K. et al. The accuracy of ICD codes for cerebrovascular diseases in medical insurance claims. Korean J. Prev. Med. 33, 76–82 (2000).
de Groot, V., Beckerman, H., Lankhorst, G. J. & Bouter, L. M. How to measure comorbidity. A critical review of available methods. J. Clin. Epidemiol. 56, 221–229. https://doi.org/10.1016/s0895-4356(02)00585-1 (2003).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40, 373–383. https://doi.org/10.1016/0021-9681(87)90171-8 (1987).
Durrleman, S. & Simon, R. Flexible regression models with cubic splines. Stat. Med. 8, 551–561. https://doi.org/10.1002/sim.4780080504 (1989).
Harrell, F. E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis (Springer, 2001).
Mach, F. et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 41, 111–188. https://doi.org/10.1093/eurheartj/ehz455 (2020).
Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016 (World Health Organization, 2018).
Kuragano, T. et al. Association between hemoglobin variability, serum ferritin levels, and adverse events/mortality in maintenance hemodialysis patients. Kidney Int. 86, 845–854. https://doi.org/10.1038/ki.2014.114 (2014).
Hawkins, W. W., Speck, E. & Leonard, V. G. Variation of the hemoglobin level with age and sex. Blood 9, 999–1007 (1954).
Eichner, E. R. Sports anemia, iron supplements, and blood doping. Med. Sci. Sports Exerc. 24, S315-318 (1992).
Nordenberg, D., Yip, R. & Binkin, N. J. The effect of cigarette smoking on hemoglobin levels and anemia screening. JAMA 264, 1556–1559 (1990).
Otto, J. M. et al. Hemoglobin concentration, total hemoglobin mass and plasma volume in patients: Implications for anemia. Haematologica 102, 1477–1485. https://doi.org/10.3324/haematol.2017.169680 (2017).
Aronoff, G. R. Safety of intravenous iron in clinical practice: Implications for anemia management protocols. J. Am. Soc. Nephrol. 15(Suppl 2), S99-106. https://doi.org/10.1097/01.ASN.0000143815.15433.87 (2004).
Macdougall, I. C. et al. Pharmacokinetics and pharmacodynamics of intravenous and subcutaneous continuous erythropoietin receptor activator (C.E.R.A.) in patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 1, 1211–1215. https://doi.org/10.2215/CJN.00730306 (2006).
Fishbane, S. & Berns, J. S. Hemoglobin cycling in hemodialysis patients treated with recombinant human erythropoietin. Kidney Int. 68, 1337–1343. https://doi.org/10.1111/j.1523-1755.2005.00532.x (2005).
Priyadarshi, A. & Shapiro, J. I. Erythropoietin resistance in the treatment of the anemia of chronic renal failure. Semin. Dial. 19, 273–278. https://doi.org/10.1111/j.1525-139X.2006.00172.x (2006).
Gaspar, B. L., Sharma, P. & Das, R. Anemia in malignancies: Pathogenetic and diagnostic considerations. Hematology 20, 18–25. https://doi.org/10.1179/1607845414Y.0000000161 (2015).
Georgieva, Z. & Georgieva, M. Compensatory and adaptive changes in microcirculation and left ventricular function of patients with chronic iron-deficiency anaemia. Clin. Hemorheol. Microcirc. 17, 21–30 (1997).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 71, e13–e115. https://doi.org/10.1161/HYP.0000000000000065 (2018).
Devereux, R. B. et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA 292, 2350–2356. https://doi.org/10.1001/jama.292.19.2350 (2004).
Hoshino, J. et al. Associations of hemoglobin levels with health-related quality of life, physical activity, and clinical outcomes in persons with stage 3–5 nondialysis CKD. J. Ren. Nutr. 30, 404–414. https://doi.org/10.1053/j.jrn.2019.11.003 (2020).
Berlin, J. A. & Colditz, G. A. A meta-analysis of physical activity in the prevention of coronary heart disease. Am. J. Epidemiol. 132, 612–628. https://doi.org/10.1093/oxfordjournals.aje.a115704 (1990).
Wannamethee, S. G. & Shaper, A. G. Physical activity and the prevention of stroke. J. Cardiovasc. Risk 6, 213–216. https://doi.org/10.1177/204748739900600404 (1999).
Mora, S., Cook, N., Buring, J. E., Ridker, P. M. & Lee, I. M. Physical activity and reduced risk of cardiovascular events: Potential mediating mechanisms. Circulation 116, 2110–2118. https://doi.org/10.1161/CIRCULATIONAHA.107.729939 (2007).
Lakatta, E. G. Age-associated cardiovascular changes in health: Impact on cardiovascular disease in older persons. Heart Fail. Rev. 7, 29–49. https://doi.org/10.1023/a:1013797722156 (2002).
Salive, M. E. et al. Anemia and hemoglobin levels in older persons: Relationship with age, gender, and health status. J. Am. Geriatr. Soc. 40, 489–496. https://doi.org/10.1111/j.1532-5415.1992.tb02017.x (1992).
Parikh, N. I., Hwang, S. J., Larson, M. G., Levy, D. & Fox, C. S. Chronic kidney disease as a predictor of cardiovascular disease (from the Framingham Heart Study). Am. J. Cardiol. 102, 47–53. https://doi.org/10.1016/j.amjcard.2008.02.095 (2008).
Kim, K., Park, S. M. & Lee, K. Weight gain after smoking cessation does not modify its protective effect on myocardial infarction and stroke: Evidence from a cohort study of men. Eur. Heart J. 39, 1523–1531. https://doi.org/10.1093/eurheartj/ehx761 (2018).
Choi, S. et al. Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern. Med. 178, 1060–1068. https://doi.org/10.1001/jamainternmed.2018.2310 (2018).
Son, J. S. et al. Association of blood pressure classification in korean young adults according to the 2017 American College of Cardiology/American Heart Association Guidelines With Subsequent Cardiovascular Disease Events. JAMA 320, 1783–1792. https://doi.org/10.1001/jama.2018.16501 (2018).
Babitt, J. L. & Lin, H. Y. Mechanisms of anemia in CKD. J. Am. Soc. Nephrol. 23, 1631–1634. https://doi.org/10.1681/ASN.2011111078 (2012).
John, M., Lange, A., Hoernig, S., Witt, C. & Anker, S. D. Prevalence of anemia in chronic obstructive pulmonary disease: Comparison to other chronic diseases. Int. J. Cardiol. 111, 365–370. https://doi.org/10.1016/j.ijcard.2005.07.043 (2006).
Author information
Authors and Affiliations
Contributions
W.J.L. and S.C. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. W.J.L., S.C. contributed to the study concept and design. S.C., S.M.P. contributed to the acquisition of data, and W.J.L., S.C., S.M.P., G.L., J.C., J.S.S., K.H.K. contributed to the analysis or interpretation of data. W.J.L. drafted the manuscript and S.C., S.M.P., G.L., J.C., Y.H.O., J.S.S., K.H.K., S.J.C. critically revised the manuscript. Statistical analysis was run by W.J.L., and S.C. provided administrative, technical, or material support.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, W.J., Choi, S., Park, S.M. et al. Association of hemoglobin variability with the risk of cardiovascular disease: a nationally representative retrospective cohort study from South Korea. Sci Rep 13, 2148 (2023). https://doi.org/10.1038/s41598-023-28029-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-28029-w
- Springer Nature Limited