Abstract
Intensive care units (ICU) are often overflooded with alarms from monitoring devices which constitutes a hazard to both staff and patients. To date, the suggested solutions to excessive monitoring alarms have remained on a research level. We aimed to identify patient characteristics that affect the ICU alarm rate with the goal of proposing a straightforward solution that can easily be implemented in ICUs. Alarm logs from eight adult ICUs of a tertiary care university-hospital in Berlin, Germany were retrospectively collected between September 2019 and March 2021. Adult patients admitted to the ICU with at least 24 h of continuous alarm logs were included in the study. The sum of alarms per patient per day was calculated. The median was 119. A total of 26,890 observations from 3205 patients were included. 23 variables were extracted from patients' electronic health records (EHR) and a multivariable logistic regression was performed to evaluate the association of patient characteristics and alarm rates. Invasive blood pressure monitoring (adjusted odds ratio (aOR) 4.68, 95%CI 4.15–5.29, p < 0.001), invasive mechanical ventilation (aOR 1.24, 95%CI 1.16–1.32, p < 0.001), heart failure (aOR 1.26, 95%CI 1.19–1.35, p < 0.001), chronic renal failure (aOR 1.18, 95%CI 1.10–1.27, p < 0.001), hypertension (aOR 1.19, 95%CI 1.13–1.26, p < 0.001), high RASS (aOR 1.22, 95%CI 1.18–1.25, p < 0.001) and scheduled surgical admission (aOR 1.22, 95%CI 1.13–1.32, p < 0.001) were significantly associated with a high alarm rate. Our study suggests that patient-specific alarm management should be integrated in the clinical routine of ICUs. To reduce the overall alarm load, particular attention regarding alarm management should be paid to patients with invasive blood pressure monitoring, invasive mechanical ventilation, heart failure, chronic renal failure, hypertension, high RASS or scheduled surgical admission since they are more likely to have a high contribution to noise pollution, alarm fatigue and hence compromised patient safety in ICUs.
Similar content being viewed by others
Introduction
Staff and patients in intensive care units (ICU) are confronted with an excessive amount of monitoring alarms on a daily basis1,2. Although alarming ICU staff of a deviation of a vital parameter is necessary in the context of delivering intensive care3,4, the majority of the alarms in the ICU are reported as false positive, caused by patient movement or poor skin contact of electrodes for example, and are often clinically non-actionable5,6,7,8,9,10. Most of these false alarms require no clinical intervention but cause disruption in the healthcare providers’ workflow2,11. This can lead to alarm fatigue, defined by Sendelbach and Funk12 as a sensory overload resulting from of the large number of particularly false alarms, and can have severe adverse effects on both the ICU staff and patients. For healthcare providers, these include decreased work satisfaction, reduced concentration, high stress levels and burnout13. For patients, it can lead to sleep disturbance14,15,16, higher rate of delirium17,18, and delayed recovery13,14. Alarm fatigue can even lead to life-threatening events and death. In fact, 98 alarm-related incidents between 2009 and 2012 were reported by the Joint Commission, an organization that evaluates and accredits healthcare institutions, 80 of which resulted in patient death19. Consequently, the ECRI Institute listed alarm-related hazards among their Top 10 Health Technology Hazards for the year 202020.
In the literature, approaches to reduce the high rate of alarms in the ICU are being discussed. These include the implementation of nurse workshops21 to raise nurses’ awareness and offer solutions for better ‘alarm hygiene’, the development of algorithms22 and machine learning models, as well as the combination of different sensor waves23. However, to our knowledge, these approaches have not yet been integrated into the clinical routine, most likely to prevent suppression of crucial life-saving alarms, which might entail legal ramifications.
So far, research has not involved patient-specific features in the study of alarms and mostly relied on descriptive analysis or the suggestion of potential solutions to combat alarm fatigue. The aim of this study is to identify patient characteristics that influence the alarm rate in the ICU, particularly characteristics significantly associated with a high alarm rate.
Methods
All collected data were stored on servers within the hospital’s network. Data extraction, data processing and statistical analysis were conducted using RStudio version 1.3.1093 and R version 4.0.3.
Alarm logs
Every patient in the ICU is connected to a standard monitoring device that monitors their vital parameters; heart rate, blood pressure, SpO2 for instance. The alarms issued from these monitoring devices are mostly related to the patient's vital parameters (deviance from a predefined limit; for example, if a patient's SpO2 were below the predefined limit of 90%, an alarm would sound).
We extracted the alarm logs from monitoring devices of eight ICUs (on three different campuses) of a German tertiary care university hospital in Berlin (discontinuously) from September 2019 until March 2021. At the time of the study, the monitors in use in the included ICUs were part of the Philips IntelliVue patient monitoring system. Three of these ICUs are surgical, three are internal, and two are neurological/neurosurgical. The raw alarm logs consist of entries with information on the respective bed the alarm was issued from, the reason (value higher or lower than a threshold, pauses, technical alarms) and date/time of the alarm. Technical alarms are not related to the patient's clinical condition and were not included in this study. Similar data was published by Poncette et al.24.
Alarms issued from other devices such as infusion pumps, other medical devices, or refrigerators are mostly technical alarms, and concern battery level, obstruction of flow, device temperature, or drug levels (syringe empty etc.) for instance and were not part of this study.
Patient inclusion criteria
Patients identified through the alarm logs were included if they were 18 years of age or older and if a minimum of 24 h of alarm data was available. During the study period, the hospital was gradually updating the electronic health records to a newer software and database, only patients from the new database (COPRA System GmbH) were included.
Variable selection
The patient characteristics included in the analysis are demographic data (age, body mass index (BMI), sex), clinical scores to represent the clinical condition and severity of illness of the patients (Sequential Organ Failure Assessment (SOFA) score, Glasgow Coma Scale (GCS), Simplified Acute Physiology Score (SAPS) II, Confusion Assessment Method for the ICU (CAM-ICU), Richmond Agitation Sedation Scale (RASS), admission type and pre-existing conditions (Charlson Comorbidity Index (CCI), and presence of coronary heart disease, hypertension, asthma, chronic obstructive pulmonary disease, diabetes, heart failure, chronic kidney failure) as well as characteristics regarding ICU healthcare utilization (if mechanical ventilation, extracorporeal membrane oxygenation (ECMO), dialysis were received, if the patient was isolated, and if the patient had a central venous catheter in place).
Extraction of patient characteristics
The above-mentioned patient characteristics were extracted from patients’ electronic health records. For data on ICU healthcare utilization, we extracted the associated timestamps (e.g., for the central line: the dates of placement and removal of the central line). If no data was available for a certain day, we considered that the patient did not receive the corresponding intervention. The BMI was calculated from the height and weight of a patient. The pre-existing conditions and each subscore of the CCI were extracted using ICD-10 GM codes. The CCI was then calculated for each patient. For mechanical ventilation, we extracted the intervals in which each patient received an airway device (Magill tube, face mask etc.). The airway devices were then categorized as invasive or non-invasive.
Data engineering
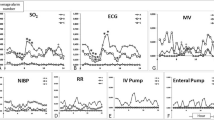
The alarm logs were cleaned; only entries describing alarm start were selected, the alarms were categorized in groups depending on the origin of the alarm (electrocardiogram (ECG), ventilator etc.), as previously described25. Only alarms regarding ECG, invasive and non-invasive blood pressure (IBP and NIBP), SpO2, ventilator and temperature were selected since these constitute the basic monitoring requirements for a patient in the ICU. Alarms from other devices (e.g., intracranial pressure and pulse contour cardiac output (PiCCO) monitor) were discarded. This assures that the alarms are issued from the same number of devices for all included patients. Technical alarms (battery levels, disconnections) were discarded as well. Alarms from devices such as syringe or infusion pumps are not saved in these alarm logs. The alarms were then linked to the respective patients (through the bed name where the alarm was generated and the bed name each patient occupied) and the rate of alarms per 24 h for each patient was calculated. To have uniform data for all patients, each 24-h block started at 6 a.m. (start of the morning shift in these ICUs). An above-median and below-median alarm rate were defined as “high” and “low”, respectively. Alarm rates that were equal to the median were randomly categorized as “high” or “low”.
The variables described above were extracted for patients identified through the alarm logs after inclusion criteria were filtered. The data were grouped into 24-h blocks, all starting at 6 a.m. Continuous variables (such as numerical scores—GCS, RASS, SAPS II—that are measured multiple times per day) were summarized using the median for each patient and day. The CAM-ICU test is generally performed several times per day: The variable ‘CAM-ICU positive’ indicates whether one of the tests during a certain day was positive for the patient. Binary data were summarized to indicate whether a patient received the intervention on a certain day (e.g., was the patient invasively ventilated on this day? YES/NO). The type of mechanical ventilation was categorized as invasive or non-invasive depending on the airway device the patient received.
Statistical analysis
A univariate analysis was performed using a t-test for continuous variables and a chi-square test for categorical variables. A multivariable logistic regression analysis including the aforementioned covariates was performed. Patient cases with missing values were excluded and the complete-case method was adopted. To test for collinearity between covariates, the variance inflation factor was computed (VIF). The VIF is a metric calculated for each variable in the model. It represents the ratio of the variance of the complete model to the variance of a model containing only that variable. Since all variables had a VIF lower than 5.3, no variables were excluded from the logistic regression model. The significance level was set at α = 0.05.
Ethics approval and consent to participate
The ethical approval was granted by the Ethics Commission of the Charité-Universitätsmedizin Berlin (Chairman: Prof. Morgenstern, ethics vote number: EA1/127/18, ethics vote date: 10/27/2021). All procedures were followed in accordance with the Ethics Committee of the Charité-Universitätsmedizin Berlin and with the Helsinki Declaration of 1975. Due to the retrospective nature of the study, informed consent was waived by the data protection department of the Charité-Universitätsmedizin Berlin based on the Berlin State Hospital Act.
Results
Dataset
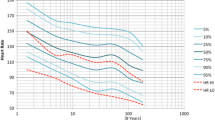
The extracted raw alarm logs contained 9,748,329 alarm start entries. After summarizing the entries per day and filtering the patient inclusion criteria, the final number of observations included in the analysis was 26,890, from 3205 different patients. Some of these patients were re-admitted to the ICU, the total number of cases is 3334. The median (interquartile range) alarm rate was 119(169) per patient per day, with a range of 1–9438.
Group comparison
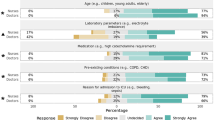
Table 1 shows the summary and differences between patients in the high- and low-alarm-rate groups. A higher percentage of patients in the high alarm rate group were males and they were on average older than the patients in the low alarm rate group (p < 0.001 for age and sex). There was no difference between the average BMIs of both groups (median 27 for both). Almost half of the patients were admitted as medical, slightly more than a third were surgical emergencies and the rest (14.1% and 15.2% for the low and high alarm rate group respectively) were planned surgical cases. The average patient in the high and low alarm rate groups had severe comorbidities with a CCI mean of 5.8 in the high alarm rate group and a slightly lower mean of 5.4 in the low-alarm rate group (p < 0.001). Patients with a higher alarm rate had more invasive interventions (invasive mechanical ventilation and invasive blood pressure monitoring) and were more likely to have a central venous catheter (p < 0.001). More patients with pre-existing cardiovascular diseases (coronary heart disease, heart failure, hypertension) and chronic kidney failure are in the high-alarm group. The percentage of patients with diabetes is comparable in both groups. There are more patients with asthma (p = 0.005) in the low alarm group, and more patients with chronic obstructive pulmonary disease (p < 0.001) in the high alarm group. Patients with a higher alarm rate had on average a higher SAPS II score (40 vs. 36, p < 0.001) and higher SOFA scores (5.3 vs 6.2, p < 0.001) indicating a higher risk of mortality. They also had a slightly higher yet significant RASS (-1.1 vs -1.2, p < 0.001). There is a higher rate of positive CAM-ICU outcomes (16% vs 18%, p < 0.001) and a slightly lower GCS in the high alarm rate group (11 vs 10 p < 0.001). There was no difference between the rate of dialysis (p = 0.12) or isolation status (p = 0.24), however more patients received ECMO in the low-alarm group (9.2% vs. 6%, p < 0.001).
Variables associated with a high alarm rate
We fitted a multivariable logistic regression model with these characteristics to assess the independent effect of each characteristic on the alarm rate while controlling for the other variables. The results of the model are presented in Table 2. They show that patients who received invasive blood pressure monitoring (OR 4.68, 95%CI 4.15–5.29, p < 0.001) or invasive mechanical ventilation (OR 1.24, 95%CI 1.16–1.32, p < 0.001), and patients who were previously diagnosed with chronic kidney failure (OR 1.18, 95%CI 1.1–1.27, p < 0.001), heart failure (OR 1.26, 95%CI 1.19–1.35, p < 0.001) or hypertension (OR 1.19, 95%CI 1.13–1.32, p < 0.001) were more likely to have high alarm rates. RASS was significantly associated with a higher alarm rate (OR 1.22, 95%CI 1.18–1.25, p < 0.001). Patients admitted to the ICU due to a planned surgical procedure were more likely to trigger more alarms than patients admitted to the ICU due to non-surgical reasons (OR 1.22, 95%CI 1.13–1.32, p < 0.001), although there was no difference between patients admitted to the ICU due to a surgical emergency and patients admitted in medicine (p = 0.8).
Variables associated with a low alarm rate
Patients who received dialysis or ECMO had higher odds of a low alarm rate (OR 0.67, 95%CI 0.62–0.72, p < 0.001 and OR 0.51, 95%CI 0.46–0.57, p < 0.001 respectively, Table 2).
Discussion
Our aim was to identify patient characteristics associated with a high alarm rate in order to emphasize ICU alarm management on patients more likely to have a high alarm rate.
We included only alarms that are associated with the patient's health status; all technical alarms were discarded. To reflect the patient’s health status, we included several variables from different categories (i.e., patient demographics, hospital stay characteristics, clinical scores), and found that invasive blood pressure monitoring, invasive mechanical ventilation, heart failure, chronic renal failure, hypertension, high RASS and scheduled surgical admission were significantly associated with a high alarm rate.
Patients with pre-existing conditions of chronic kidney failure, hypertension and heart failure are usually more unstable and challenging to care for, especially in an acute situation, which would explain the higher rate of alarms compared to patients without these conditions. The same is true for patients who received invasive blood pressure monitoring and invasive ventilation. However, we did not find a significant association of the other diagnoses (i.e., coronary heart disease, asthma) and the clinical scores (i.e., GCS, SAPS II) with a higher alarm rate. This may be explained by a tendency of undercoding diagnoses in EHRs26,27,28. As for patients with a high RASS, the higher number of alarms may be due to artifacts caused by movement or agitation, for example.
Dialysis and ECMO were significantly associated with a low alarm rate. A possible explanation for this counterintuitive finding could be that these patients are usually sedated and intubated, resulting in less alarms related to movement. However, invasive ventilation was associated with a higher alarm rate. As stated above, the alarms of the ECMO and dialysis devices were not included in the alarm rate calculated for the patients in this study.
From these findings, we can suggest that ICU staff should pay closer attention to the alarm management and alarm hygiene of patients with characteristics associated with a high alarm rate. Many solutions to reduce the high rate of alarms have been proposed in the literature, e.g., machine learning algorithms22 and sensor fusion methods23. However, most of these suggestions have not found their way into clinical routine yet. Nevertheless, we believe that there are many steps that can be taken in order to alleviate the alarm burden in ICUs. Individualizing alarm thresholds for example is an important first step29. Although this suggestion might seem trivial, there is a significant number of staff members that adhere to the default thresholds of the monitoring devices and do not adjust the thresholds according to an individual patient’s need30,31. This might be either due to lack of time/will or of know-how. Therefore implementing workshops as suggested by Brantley et al.21 and Bi et al.32, and assigning monitor superusers (staff members that undergo training in and become experts in setting up monitoring devices) as described by Sowan et al.33, are also concrete steps that ICU staff can undergo to reduce the high rate of alarms. Another solution is to implement the use of the pause function while examining or performing interventions on patients34, or to implement a delay between the deviation of the vital parameter and the sounding of the alarm35.
We hope that this study encourages further research directed towards patient-specific effects on monitoring alarms. We believe that developing individualized alarm management for patient monitoring systems will strongly alleviate alarm fatigue and even reduce the rate of false alarms.
This study has several limitations. Although multiple ICUs were included in this study, it remains a single-center retrospective study, utilizing EHRs which are prone to be biased, especially regarding diagnosis26,27,28. Due to the retrospective nature of the study, differentiating between false and true alarms is extremely complex and was not performed. However, only patient-related monitoring alarms were included; technical alarms (from monitoring or other medical devices) were excluded. Furthermore, there is no absolute threshold defining a high alarm rate36. We therefore set the threshold as the median alarm rate of our dataset. Future studies should investigate the criticality of alarms on patient level (i.e., yellow, red alarms) as well as other metrics of ICU alarm load such as alarm floods as previously described37.
Conclusion
The high rate of alarms in ICUs is an issue that impairs the quality of patient care, increases the staff’s stress levels, and can even cause sentinel events. This study is the first to analyze the effect of patient characteristics on ICU alarm rates. We showed that invasive blood pressure monitoring, invasive mechanical ventilation, preexisting chronic kidney failure, hypertension, and heart failure, a high RASS as well as scheduled surgical admission can significantly increase the ICU’s alarm rate. ICU staff should pay close attention to alarm management, especially with patients that have these characteristics. Our findings are an important step towards developing novel alarm management strategies incorporating patient-specific characteristics. Future studies with other ICUs should be performed to confirm our findings and examine whether interventions on alarm management targeted at these patients result in a significant reduction of the alarm rate in the ICUs.
Data availability
The datasets used during the current study are located in the internal network of the Charité-Universitätsmedizin Berlin and are not publicly available due to the current data privacy policy, but are available from the corresponding author on reasonable request.
References
Drew, B. J. et al. Insights into the problem of alarm fatigue with physiologic monitor devices: A comprehensive observational study of consecutive intensive care unit patients. PLoS ONE 9(10), e110274 (2014).
Ruskin, K. J. & Hueske-Kraus, D. Alarm fatigue: Impacts on patient safety. Curr. Opin. Anaesthesiol. 28(6), 685–690 (2015).
Stewart, J. S. S. The aim and philosophy of patient monitoring. Postgrad. Med. J. 46(536), 339–343 (1970).
Kipnis, E. et al. Monitoring in the intensive care. Crit. Care Res. Pract. 2012, 473507 (2012).
Schmid, F., Goepfert, M. S. & Reuter, D. A. Patient monitoring alarms in the ICU and in the operating room. Crit. Care 17(2), 216 (2013).
Imhoff, M. & Kuhls, S. Alarm algorithms in critical care monitoring. Anesth. Analg. 102(5), 1525–1537 (2006).
Görges, M., Markewitz, B. A. & Westenskow, D. R. Improving alarm performance in the medical intensive care unit using delays and clinical context. Anesth. Analg. 108(5), 1546–1552 (2009).
Tsien, C. L. & Fackler, J. C. Poor prognosis for existing monitors in the intensive care unit. Crit. Care Med. 25(4), 614–619 (1997).
Chambrin, M. C. et al. Multicentric study of monitoring alarms in the adult intensive care unit (ICU): A descriptive analysis. Intensive Care Med. 25(12), 1360–1366 (1999).
Siebig, S. et al. Intensive care unit alarms–how many do we need?. Crit. Care Med. 38(2), 451–456 (2010).
Poncette, A.-S. et al. Improvements in patient monitoring in the intensive care unit: Survey study. J. Med. Internet Res. 22(6), e19091 (2020).
Sendelbach, S. & Funk, M. Alarm fatigue: A patient safety concern. AACN Adv. Crit. Care 24(4), 378–386 (2013).
AAMI Foundation. Clinical Alarm Management Compendium (Accessed 29 September 2021); www.aami.org/alarmcompendium.
Xie, H., Kang, J. & Mills, G. H. Clinical review: The impact of noise on patients’ sleep and the effectiveness of noise reduction strategies in intensive care units. Crit. Care 13(2), 208 (2009).
Simons, K. S. et al. Noise in the intensive care unit and its influence on sleep quality: A multicenter observational study in Dutch intensive care units. Crit. Care Lond. Engl. 22(1), 250 (2018).
Aaron, J. N. et al. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep 19(9), 707–710 (1996).
Van Rompaey, B., Elseviers, M. M., Van Drom, W., Fromont, V. & Jorens, P. G. The effect of earplugs during the night on the onset of delirium and sleep perception: A randomized controlled trial in intensive care patients. Crit. Care Lond. Engl. 16(3), R73 (2012).
Pugh, R. J., Jones, C. & Griffiths, R. D. The impact of noise in the intensive care unit. In Intensive Care Medicine (ed. Vincent, J. L.) 942–949 (Springer, 2007).
The Joint Commission Sentinel Event Alert (accessed 1 November 2021); https://www.jointcommission.org/-/media.
ECRI Institute: Top 10 Health Technology Hazards for 2020 (accessed 30 September 2021); http://www.ecri.org.
Brantley, A. et al. Clinical trial of an educational program to decrease monitor alarms in a medical intensive care unit. AACN Adv. Crit. Care 27(3), 283–289 (2016).
Clifford, G. D. et al. False alarm reduction in critical care. Physiol. Meas. 37(8), E5-23 (2016).
Borges, G. & Brusamarello, V. Sensor fusion methods for reducing false alarms in heart rate monitoring. J. Clin. Monit. Comput. 30(6), 859–867 (2016).
Poncette, A.-S., et al. Resources for a “Do-it-Yourself Analysis” of the patient monitoring alarm data from intensive care units (Accessed 1 December 2021); 10.5281/zenodo.4560041.
Poncette, A.-S. et al. Patient monitoring alarms in an intensive care unit: Observational study with do-it-yourself instructions. J. Med. Internet Res. 23(5), e26494 (2021).
Johnson, N., Mant, D., Jones, L. & Randall, T. Use of computerised general practice data for population surveillance: Comparative study of influenza data. BMJ 302(6779), 763–765 (1991).
Myers, L. & Stevens, J. Using EHR to conduct outcome and health services research. In Secondary Analysis of Electronic Health Records 61–70 (Cham, Springer, 2016).
Corser, W. et al. Concordance between comorbidity data from patient self-report interviews and medical record documentation. BMC Health Serv. Res. 8, 85 (2008).
Graham, K. C. & Cvach, M. Monitor alarm fatigue: Standardizing use of physiological monitors and decreasing nuisance alarms. Am. J. Crit. Care Off. Publ. Am. Assoc. Crit.-Care Nurses 19(1), 28–34 (2010).
Fidler, R. L. et al. Understanding heart rate alarm adjustment in the intensive care units through an analytical approach. PLoS ONE 12(11), e0187855 (2017).
Ruppel, H. et al. Challenges of customizing electrocardiography alarms in intensive care units: A mixed methods study. Heart Lung J. Crit. Care 47(5), 502–508 (2018).
Bi, J. et al. Effects of monitor alarm management training on nurses’ alarm fatigue: A randomised controlled trial. J. Clin. Nurs. 29(21–22), 4203–4216 (2020).
Sowan, A. K., Gomez, T. M., Tarriela, A. F., Reed, C. C. & Paper, B. M. Changes in default alarm settings and standard in-service are insufficient to improve alarm fatigue in an intensive care unit: A Pilot project. JMIR Hum. Factors 3(1), e1 (2016).
Li, A. & Gretzinger, D. Applying an evidence-based approach to managing alarm safety: A university health network case study. In (ed Jaffray, D. A.) World Congress on Medical Physics and Biomedical Engineering 1538–1541 (Springer International Publishing, 2015).
Welch, J. et al. Framework for alarm management process maturity. Biomed. Instrum. Technol. 50(3), 165–179 (2016).
Wilken, M., Hüske-Kraus, D. & Röhrig, R. Alarm fatigue: Using alarm data from a patient data monitoring system on an intensive care unit to improve the alarm management. Stud. Health Technol. Inform 267, 273–281 (2019).
Hüske-Kraus, D., Wilken, M. & Röhrig, R. Measuring Alarm system quality in intensive care units. Zukunft der Pflege Tagungsband der 1. Clusterkonferenz 2018, 89–93 (2018).
Acknowledgements
This work was performed at the Institute of Medical Informatics, Charité-Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was funded by the German Federal Ministry of Education and Research (BMBF), grant number: 16SV8559, INALO. AP is a participant in the Charité Digital Clinician Scientist Program funded by the Charité-Universitätsmedizin Berlin and the Berlin Institute of Health.
Author information
Authors and Affiliations
Contributions
ZS extracted the data from the alarms logs, performed the formal analysis and was responsible for writing the first draft. DS contributed to the conceptualization, methodology, analysis and validation of the study, as well as editing the final manuscript. JK assisted in the methodology, statistical analysis and validation of the study. NG, SK, AF, PH assisted in the conceptualization, data curation, statistical analysis and review and editing of the manuscript. FS, CS, CH, AW provided the resources, supervised, reviewed and edited the manuscript from a clinical viewpoint. FB and AP were responsible for the conceptualization, funding acquisition, project administration, supervision of all parts of the study as well as reviewing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sinno, ZC., Shay, D., Kruppa, J. et al. The influence of patient characteristics on the alarm rate in intensive care units: a retrospective cohort study. Sci Rep 12, 21801 (2022). https://doi.org/10.1038/s41598-022-26261-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-26261-4
- Springer Nature Limited