Abstract
Exposure to trauma, high-stress situations, and disrupted sleep are well known risk factors affecting firefighters’ mental health. Little is known about the association between firefighters’ exposure to fire contaminants and mental health disorders. The UK Firefighter Contamination Survey assessed firefighters’ health and capacity for occupational exposure to contaminants. Participants were invited to anonymously complete its 64 questions online. Logistic regression analyses assessed the associations between self-reported mental health disorders and proxies of contaminant exposure. Results found that firefighters who notice soot in their nose/throat for more than a day after attending fires (Odds Ratio (OR) = 1.8, 1.4–2.4), and those who remain in their personal protective equipment (PPE) for over 4 h after fires (OR = 1.9, 1.2–3.1), were nearly twice as likely to report mental health disorders. Significantly increased odds ratios for all three outcomes of interest (anxiety, depression and/or any mental health disorders) were also found among firefighters who take PPE home to clean. Sleeping problems were reported by 61% of firefighters. These firefighters were 4.2 times more likely to report any mental health disorder (OR = 4.2, 3.7–4.9), 2.9 times more likely to report anxiety (OR = 2.9, 2.4–3.5) and 2.3 times more likely to report depression (OR = 2.3, 1.9–2.8) when compared to firefighters who did not report sleep issues. Effective decontamination measures within UK Fire and Rescue Services, together with firefighters’ wellness, may play a crucial role in protecting firefighters’ mental health.
Similar content being viewed by others
Introduction
Mental health disorders can be caused by a combination of psychological, environmental, biological, and chemical factors. To date, research on firefighters’ mental health has mainly focused on psychological factors such as direct exposure to trauma1 or occupational stress2, finding firefighters to have an increased risk of suicide3, depression1,2, and post-traumatic stress disorder (PTSD)4. Studies have also investigated the effects of other occupational exposures, e.g. abrupt fire incident call-outs, disrupted sleep5, as well as physical and/or emotional fatigue on firefighters’ mental health. However, little is known about the relationship between firefighters’ exposure to fire effluent and mental health.
Fire smoke is a heterogenous cocktail of chemicals with varying toxicities and modes of action6. A growing body of research has identified a number of different fire effluents contaminating fire stations and firefighters’ PPE. Elevated levels of polybrominated diphenyl ethers (PBDEs)7,8, polychlorinated and polybrominated dibenzo-p-dioxins and dibenzofurans (PCDD/Fs and PBDD/Fs)9 or halogenated gas phase flame retardants7 have also been reported in firefighters’ blood and urine10– suggesting several routes for chronic exposure11,12,13,14,15,16.
Several components of fire smoke have also been associated with mental health disorders. For example, the U.S. Environmental Protection Agency and the Agency for Toxic Substances and Disease Registry, found exposure to neurotoxic chemicals such as mercury and lead, or endocrine disruptors such as polychlorinated biphenyls, PBDEs or poly- and perfluoroalkyl substances (PFAS), can lead to hormone imbalances and/or neuroendocrine dysfunction, leading to conditions such as depression and anxiety17. Additionally, suffering life-altering, painful and/or chronic physical health conditions (e.g. cancer or other long-term diseases) from exposures to contaminants may also negatively impact firefighters' mental health.
The UK Firefighter Contamination Survey has uncovered several practices which would increase firefighters’ risk of contaminant exposure and/or promote travel of contaminants back to workplaces/homes18. This manuscript explores one of potentially many health implications of such increased exposure, associating proxies of contamination with self-reported mental health disorders among UK firefighters (see also Wolffe et al.18). By assessing mental health risks for a broad range of contaminant control practices the survey provides an interim means of quickly identifying areas in which UK Fire and Rescue Services can optimally target resources for improving firefighters’ occupational health.
Methods
Survey design
The methods used to conduct the survey and analyse its results are detailed in Wolffe et al.18 and are summarised again in Supplemental File S2. Ethical approval for the survey was granted by the University of Central Lancashire Ethics Committee and all analyses were conducted in accordance with relevant guidelines and regulations.
Briefly, all currently serving (i.e. excluding retired) UK firefighters were eligible to take part in the survey and were recruited to participate via email through the Fire Brigades Union (whose members make up approximately 75% of the UK’s total firefighting workforce18,19). Firefighters were invited to anonymously complete the survey online. Informed consent was obtained from all participants.
The survey, which took approximately 20 min to complete, consisted of 64 questions covering six key topics (Tables S1, S2, S3, S4, S5 and S6): demographics, PPE, workplace contamination, personal contamination, attitudes/awareness and training, and health (Supplemental File S1). Branching logic was used to route participants through the survey based on answers to previous questions.
Mental health conditions
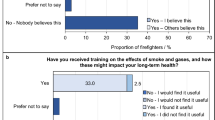
Firefighters were able to choose multiple specific conditions from a list, as presented in Fig. 1 and Supplemental File S1. Analyses conducted in this manuscript specifically assess any mental health condition (i.e. those reporting at least one of the listed mental health conditions), anxiety, or depression.
Firefighters’ Mental Health Conditions. The proportion of total surveyed firefighters with any, or specific, mental health disorders (blue). The prevalence of mental health disorders in the general English population39 is displayed for comparison (orange). “Any mental health condition”, “anxiety” and “depression” among surveyed firefighters is compared to “any common mental disorder”, “generalised anxiety disorder” and “depressive episode” in the general English population, respectively. * indicates a p-value of < 0.05 for differences in proportions between firefighters and English population.
Analysis
A complete case analysis was conducted for all firefighters who answered the questions about mental health and potential contaminant exposure.
Multiple logistic regression analyses were used to assess the association between mental health conditions and potential for exposure to fire contaminants, adjusting for plausible non-contaminant risk factors and confounders assessed in the survey (see Supplemental File S2) i.e. age, length of service, sleeping problems20, excessive drinking21,22, smoking23, infrequently exercising24, having a managerial role (as a measure of work-related stress25), attending fires on a more frequent basis (regular exposure to trauma26), having another physical health condition (i.e. diabetes27,28, blood pressure problems29,30, cancer31,32, or fertility issues33,34,35), and having another mental health condition36 (for analyses of depression and anxiety).
Analyses were conducted using the statsmodels module for Python 337, and Statistical Package for Social Sciences (SPSS) version 28.0.1.1. Note that firefighters reporting only attention deficit hyperactivity disorder (ADHD) or only autism spectrum disorder (ASD) were excluded from logistic regression analyses as these conditions represent developmental disorders, first appearing in childhood, and most commonly researched with regard to early life exposures to contaminants, rather than the later life exposures firefighters receive as adults during their careers.
Odds ratios (OR) with 95% confidence intervals are presented as a means of assessing the statistical significance of differences in the prevalence of mental health conditions between various demographic groups, or between groups at (potentially) greater versus lower risk of contaminant exposure.
Results and analysis
A total of 10, 649 firefighters responded to the questionnaire, representing approximately 24% of the UK’s total firefighter workforce (Wolffe et al.18). Participant demographics were analysed in Wolffe et al. 18, and were not found to significantly differ from the English firefighter population38 with respect to sex (p > 0.05), but appeared to under-represent younger age categories, retained firefighters, and those belonging to an ethnic minority (p < 0.05)18.
Around 19% (n = 2019) of firefighters self-reported at least one mental health condition. Figure 1 displays the range and frequency of mental health disorders selected by firefighters, which is then compared to the prevalence of those conditions in the general English population (where possible3). Note that firefighters were able to select more than one mental health condition.
Self-reports of anxiety were most prevalent among surveyed firefighters (approximately 12%), followed by depression (around 10%) and post-traumatic stress disorder (PTSD) (around 5%), as presented in Fig. 1. The prevalence of self-reported anxiety and depression among surveyed firefighters was also significantly higher than that of the English population (Fig. 1, difference in proportions test p < 0.05).
Less than 2% of surveyed firefighters reported obsessive compulsive disorder (OCD) (1.6%), attention deficit hyperactivity disorder (ADHD) (0.6%), eating disorders (0.4%), bipolar disorder (0.3%), autism spectrum disorder (ASD) (0.2%), or schizophrenia (0.04%). The majority of firefighters who selected “other” (0.4%) listed “stress” associated with their work (40% of firefighters answering “other”, or 0.2% of total surveyed firefighters).
Out of the 19% of surveyed firefighters suffering any mental health condition (n = 2019), around 44% reported having more than one condition (n = 878). The frequency with which mental health conditions co-occurred is displayed in Fig. 2. Anxiety and depression co-occurred most frequently.
From the logistic regression models (Supplemental File S2), having a co-occurring mental health condition had the most sizeable impact on reporting depression or anxiety. Firefighters with at least one co-occurring condition were nearly 16 times more likely to suffer depression (OR = 15.6, 13.3–18.4) and around 13 times more likely to suffer anxiety (OR = 13.3, 11.5–15.5) when compared to firefighters with no co-occurring mental health conditions (i.e. who only had depression, or only anxiety).
Demographics
Similar proportions of firefighters in each role, except for the most senior roles (such as area or principal manager), were found to suffer from any mental health condition, anxiety, or depression, Fig. 3. The proportion of surveyed firefighters with any mental health condition, anxiety, or depression generally increased with length of service, Fig. 3. Firefighters who had served longer (i.e. ≥ 15 years) were slightly more likely to report suffering any mental health condition compared to firefighters who had served less time (OR = 1.1, 1.0–1.3), although no significant differences were observed for anxiety (OR = 1.0, 0.9–1.2) or depression (OR = 1.0, 0.9–1.2).
Firefighters’ Mental Health Conditions by Demographics. (a) The proportion of firefighters with any mental health condition, anxiety, or depression in each demographic category. (b) Odds ratios (with 95% confidence intervals) for specific demographic groups having any mental health condition, anxiety, or depression. Note that the proportions of surveyed firefighters in each demographic category are presented in Wolffe et al., 18. The results of underpowered demographic groups (e.g. sex = “Other” for which there was a total of 4 firefighters) should be interpreted cautiously. Odds ratios were adjusted for various mental health risk factors (Supplementary File S2).
Only wholetime firefighters, when compared to firefighters on all other contract types combined, were more (but not significantly more) likely to report any mental health condition (OR = 1.1, 1.0–1.3), and anxiety (OR = 1.2, 1.0–1.4).
Firefighters who attended fires on at least a weekly basis were more likely to report depression compared to firefighters who attended fires less frequently (OR = 1.2, 1.0–1.4). However, no significant differences between these groups were noted for any mental health condition (OR = 1.0, 0.9–1.1), or anxiety (OR = 1.0, 0.9–1.2).
Health and lifestyle
Firefighters were also asked questions related to their health and lifestyle, which could possibly be linked with mental health conditions such as anxiety, or depression (Supplemental File S1, Wolffe et al.18). These questions were subsequently included in logistic regression models (Supplemental File S2) and are explored further below.
Sleeping problems
Around 61% of all surveyed firefighters (n = 6490) said that they have sleeping problems, Fig. 4a. Those who reported sleeping problems were 4.2 times more likely to report any mental health condition (OR = 4.2, 3.7–4.9), 2.9 times more likely to report anxiety (OR = 2.9, 2.4–3.5) and 2.3 times more likely to report depression (OR = 2.3, 1.9–2.8) compared to firefighters who did not report it, Fig. 4c.
Firefighters’ Sleeping Problems. (a) The proportion of total surveyed firefighters who indicated whether they had sleeping problems. (b) The proportion of firefighters with sleeping problems listing the reasons for their sleep disturbances. Note that firefighters were able to select more than one reason. (c) Adjusted odds ratios (with 95% confidence intervals) for firefighters’ mental health conditions due to sleeping problems. (d) Adjusted odds ratios (with 95% confidence intervals) for firefighters sleeping problems due to demographic variables. Note that odds ratios presented in (c) and (d) were adjusted for a variety of disturbed sleep risk factors (Supplementary File S2).
Firefighters were also asked to provide more details about their sleeping problems. They were able to select multiple answers, listed in Supplemental File S1. Over 65% of firefighters (out of 6490, n = 4228) indicated that shift work was a major sleep disturbance (Fig. 4b). Mental health (46%, n = 3010) and workload (36%, n = 2313) were also frequently selected. Home, personal or family-life related reasons (e.g. disturbed by children or split/divorce etc.) were the most common disturbances listed by firefighters selecting “other”.
Multiple logistic regression analyses (Supplemental File S2) revealed a slightly increased likelihood of reporting sleeping problems for managerial firefighters (OR = 1.1, 1.0–1.2), wholetime firefighters (OR = 1.1, 1.0–1.2), firefighters attending fires on at least a weekly basis (OR = 1.2, 1.1–1.3), and firefighters with 15 + years of service (OR = 1.1, 0.9–1.2), Fig. 4d. However, this increase was only significant for firefighters attending incidents on a weekly basis. Retained firefighters were slightly, but significantly, less likely to report sleeping problems when compared to firefighters employed on all other contract types combined (OR = 0.9, 0.7–1.0).
Other health and lifestyle variables
Several other health and lifestyle variables were also found to be significantly associated with firefighters’ mental health, and are presented in Table 1.
Firefighters with a cancer diagnosis were significantly more likely to report any mental health condition (OR = 1.5, 1.1–1.9), but were not found to be significantly more likely to report anxiety (OR = 1.2, 0.9–1.7), depression (OR = 0.9, 0.6–1.3) or sleeping problems (OR = 1.0, 0.8–1.3).
Aside from problems sleeping and having a co-occurring mental health condition, the only health/lifestyle variables found to be significantly associated with depression was infrequent exercising (OR = 1.4, 1.2–1.7). Excessive drinking, smoking, and problems with blood pressure were found to be significantly associated with both any mental health condition and sleeping problems (Table 1).
Fertility problems were significantly associated with any mental health condition (OR = 1.4, 1.1–1.9), anxiety (OR = 1.3, 1.0–1.7) and sleeping problems (OR = 1.3, 1.1–1.5).
Exposure to fire contaminants during/after fire incidents
Significantly increased odds ratios for any mental health condition were found for firefighters who noticed soot in their nose/throat for more than a day after attending a fire (OR = 1.8, 1.4–2.4), and for those that remained in PPE for more than 4 h after a fire (OR = 1.9, 1.2–3.1). Results are shown in Fig. 5. Firefighters were also significantly more likely to report any mental health condition if they reported still noticing the smell of fire smoke on the body after washing (OR = 1.3, 1.1–1.5), or eating with sooty hands (OR = 1.3, 1.1–1.4).
Firefighters’ Exposure to Contaminants During/After Fires and Mental Health Odds Ratios. Odds ratios (with 95% Confidence Intervals) were adjusted for various mental health risk factors (Supplementary File S2).
Similar results were found for anxiety. Significantly increased odds ratios were found for firefighters who eat with sooty hands (OR = 1.2, 1.1–1.4 for anxiety), and who noticed soot in the nose/throat for up to a day after washing (OR = 1.4, 1.0–1.8 for anxiety).
Those noticing the smell of fire smoke on the body after washing were significantly more likely to report depression (OR = 1.3, 1.0–1.5).
Fire contaminants on firefighters’ PPE and at their workplace
Firefighters with ill-fitting PPE were significantly more likely to report any mental health disorder (OR = 1.4, 1.2–1.7), and anxiety (OR = 1.4, 1.1–1.7), presented in Fig. 6. Significantly increased odds ratios were also found for firefighters taking PPE home (OR = 1.4, 1.2–1.6 for any mental health condition, OR = 1.3, 1.1–1.6 for anxiety, and OR = 1.3, 1.0–1.6 for depression).
Firefighters’ PPE/Workplace Contamination and Mental Health Odds Ratios. Odds ratios (with 95% confidence intervals) were adjusted for various mental health risk factors (Supplementary File S2).
Additionally, significantly increased odds ratios were found, for those firefighters failing to store clean and dirty PPE separately (OR = 1.1, 1.0–1.3 for any mental health condition (Fig. 6)).
Infrequently sending fire gloves for professional decontamination was also associated with an increased anxiety odds ratio (OR = 1.5, 1.0–2.3).
Firefighters who worked in stations with no designated clean and dirty areas were also more likely to report any mental health condition (OR = 1.2, 1.1–0.4), and anxiety (OR = 1.2, 1.0–1.4), as were firefighters working in stations which smell of fire (OR = 1.2, 1.1–1.4 for any mental health condition and OR = 1.2, 1.0–1.4 for anxiety), Fig. 6.
Culture, fire contaminant awareness and training and culture
Firefighters who personally believe that contaminated PPE should be celebrated as a “badge of honour” (explained in Wolffe et al.18) were significantly more likely to report any mental health condition (OR = 1.5, 1.2–1.7), or anxiety (OR = 1.2, 1.0–1.5) (Fig. 7). Feeling that colleagues uphold this belief was also associated with a slightly increased odds ratio for any mental health condition (OR = 1.2, 1.0–1.3).
Firefighters Training/Culture and Mental Health Odds Ratios. Odds ratios (with 95% confidence intervals) were adjusted for various mental health risk factors (Supplementary File S2).
The other variables significantly associated with any mental health disorder and anxiety were feeling that cleaning was not taken seriously at the workplace (OR = 1.4, 1.3–1.6 for any mental health condition, and OR = 1.2, 1.0–1.4 for anxiety). In addition, firefighters who had not received training on the health effects of fire contaminants were only slightly (but not significantly) more likely to indicate having any mental health condition (OR = 1.1, 1.0–1.2).
Discussion
Occupational exposure to contaminants and mental health disorders in firefighters
UK firefighters were found to have significantly higher rates of (any) self-reported mental health conditions when compared to the general UK population (who were more reliably diagnosed against the UK revised Clinical Interview Schedule (CIS-R)). In particular, the rates of self-reported anxiety and depression in firefighters far exceeded those diagnosed in the general population. The rate of anxiety among surveyed firefighters was twice that of the general population, while the rate of depression was nearly three times that of the general population.
Several measures of potential contaminant exposure were associated with a significantly increased odds ratios for any mental health condition, anxiety, or depression. For example, firefighters noticing soot in the nose/throat for a day or more after washing, were nearly twice as likely to suffer any mental health condition.
Of the potential sources of contaminant exposure assessed in the survey, eating with sooty hands, taking PPE home to clean, wearing poorly fitting PPE, and noticing soot in the nose/throat were most consistently associated with increased odds ratios for mental health disorders, significantly increasing the likelihood of firefighters reporting any mental health condition, anxiety, and (in the case of taking PPE home) depression.
There is very little known about the association between firefighters’ exposures to different contaminants and mental health disorders. Given that firefighters spend prolonged amounts of time attending fire incidents, their capacity for exposure is far greater when compared to the general population and other occupational groups. For example, exposure studies record concentrations of particulate matter (PM) orders of magnitude greater at fire incidents (e.g. wildfires40) when compared to ambient concentrations measured in studies of mental health in general populations41. This comparison is particularly concerning, given that 84% of surveyed firefighters often/sometimes attend fires without respiratory protective equipment (Wolffe et al.18).
Furthermore, recent biomonitoring data has revealed positive associations between urinary concentrations of several polycyclic aromatic hydrocarbons42 (a class of chemicals commonly released in fires and found on firefighters’ PPE, workplaces etc.) and mental health disorders (such as depression)43,44,45.
However, most research on the association between mental health disorders and chemicals, particulates etc. found in fire smoke comes from studies focused on identifying genetic risk factors for mental health disorders46,47 and exposure to chemicals in early-life (including pre-natal) leading to impeded neurodevelopment48,49. There are also epidemiological studies examining the occurrence of mental health disorders in general populations, e.g. associations between common air pollutants (PM10 and PM2.5, benzene, nitrogen oxides, ozone etc.) and common mental health disorders41,50, depression41,51,52,53, and/or anxiety52 have been documented41.
Further, it is widely recognised that social (e.g. socioeconomic status), psychological (e.g. exposure to trauma), biological (e.g. enduring painful illness), and environmental (e.g. interactions with the physical environment) factors not only vary, but may also have synergistic effects on mental health outcomes. Thus, it is possible that the impact on firefighters may be amplified as firefighters are already occupationally predisposed to several other mental health risk factors (e.g. exposure to trauma/stress etc.).
Mental health disorders in firefighters and sleeping problems
As well as mental health conditions, poor sleep is known to impact performance, e.g. compromising firefighters’ safety by reducing reaction times54. In addition, chronic sleeping problems may also lead to poor immune, cardiovascular, and gastrointestinal health55.
Over 60% of surveyed firefighters reported sleeping problems (with shift work pattern being the major reason). By contrast, an estimated 36% of UK adults have sleeping problems56. A strong link between sleeping problems and mental health was found among surveyed firefighters (Fig. 4), with firefighters reporting sleeping problems being at least twice as likely to suffer anxiety or depression compared to firefighters without sleeping issues, and over 4 times as likely to report any mental health condition (Fig. 4).
Research suggests that increasing awareness and screening firefighters for sleep disorders as well as revising their shift schedules (in order to minimise disruption to circadian rhythms) may help to maintain healthy sleep schedules57.
Other occupational risk factors for mental health disorders in firefighters
Although the survey did not account for all mental health risk factors, the rate of self-reported PTSD (a condition associated with exposure to trauma) among surveyed firefighters was comparable to that of the UK population (p > 0.05). However, as explained earlier, caution needs to be taken when comparing self-reported cases with CIS-R diagnosed cases.
Scientific literature on firefighters’ risk of PTSD is variable in terms of its findings and measures. Some authors have identified being younger, or beginning a career in the Fire and Rescue Service at a young age, as risk factors for developing PTSD58. Others have documented a higher prevalence of PTSD among retired when compared to serving firefighters59. Thus, given the relatively older modal age of surveyed firefighters (between 45 and 54 years old, Wolffe et al.18), and the exclusion of retired/ex-firefighters, it is possible that the prevalence of PTSD in UK firefighters is under-represented in the survey. Similarly, firefighters suffering from PTSD may have been less inclined to participate in the survey.
Other occupational risk factors for mental health disorders among firefighters may include cultural aspects of firefighting, and/or awareness of contaminant exposure and its health effects. Studies in populations who are knowingly exposed to contaminants (e.g. contaminated drinking water etc.) document increased rates of mental health conditions such as anxiety, as a result of concern over the effects of this exposure60. Similarly, if firefighters’ awareness of the health effects of contaminant exposure outpaces decontamination policy changes/enforcement, this may cause anxiety among firefighters who feel that their health is not being prioritised.
Similarly, cultural aspects of firefighting (e.g. workplace bravado or the need to remain stoic in high stress or traumatic situations), may negatively impact firefighters’ mental health e.g. by supressing trauma.
Limitations
Previous parts of the UK Firefighter Contamination Survey analysis already discussed some of the limitations of this survey (Wolffe et al.18) such as participation bias. Additionally, the self-reported mental health conditions, studied in this manuscript, were not verified against an official clinical diagnosis.
As the primary focus of the survey was on contaminant control measures, several confounders of mental health were also not accounted for e.g. family history and/or co-occurring diseases which may contribute to the development of mental health disorders61.
Quantitation of contaminants in firefighters and/or PPE and workplaces, and how these may change with regards to the contaminant control practices assessed in this survey, would further strengthen suggested relationships between fire contaminant exposure and mental health outcomes.
The analyses conducted in this manuscript found several significant associations between potential contaminant exposure and mental health disorders. However, the manuscript does not assess interaction between these exposure variables. For example, eating while wearing PPE may be associated with eating with sooty hands. Refining a final logistic regression model, in which all relevant exposure variables assessed in the survey are included and interaction accounted for, represents an area for future work. Additionally, a complete case analysis is presented in this manuscript (whereby firefighters who did not answer the question about mental health were excluded from subsequent analyses). Thus, further model development will require imputation methods to account for missing data and reduce potential bias.
It should also be noted that mental health is a topic which continues to be associated with stigma, especially in males62. Thus, it is possible that the prevalence of mental health conditions in the survey has been under-represented.
Furthermore, sleeping problems and mental health conditions share mutual causality, whereby mental health conditions can arise from poor sleep, and vice versa. In fact, 46% of firefighters reporting sleeping problems indicated that mental health was the cause. As logistic regression analyses did not distinguish between firefighters who did and did not report mental health as a cause of their sleeping problems, further refinement of logistic regression models should be performed.
Finally, the survey did not ask firefighters about their access to mental health services/support within their workplaces, (a variable known to influence mental health outcomes in firefighters63), so cannot give a complete account of issues concerning mental health within the UK Fire and Rescue Service.
Conclusion
The rate of depression among UK firefighters is nearly three times that of the general population. Additionally, firefighters suffer anxiety at a rate over twice that of the general population, with a slightly higher proportion of firefighters reporting any mental health condition compared to the general population (20% versus 17%). Given the high rates of depression and anxiety, further support for mental health, and focus on mental health interventions, may be required in UK Fire and Rescue Services.
Several health and lifestyle factors were found to be significantly associated with mental health disorders among surveyed firefighters. The most significant among these was sleeping problems. However, adjusting for such risk factors through logistic regression analyses revealed significantly increased anxiety and any mental health condition odds ratios for several measures of contaminant exposure, including noticing soot in the nose/throat, taking PPE home to clean, wearing poorly fitting PPE, and eating with sooty hands. Further analysis on firefighters’ capacity for exposure to fire contaminants is covered in Wolffe et al.18.
Analyses conducted in this manuscript can be used to inform more comprehensive predictive models of mental health in the UK FRSs, outlining several contaminant control measures which should be considered in such modelling.
Further research is required in order to better understand the complex relationship between potential contaminant exposure and firefighters’ mental health, including the potentially modifying effects of other risk factors such as psychological, biological, environmental, and genetic factors.
However, given the potentially synergistic effects of these risk factors, it is important to consider interventions which address not only contaminant exposure, but also firefighters’ physical and mental well-being in order to improve the mental health of firefighters in the UK Fire and Rescue Service.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Regehr, C., Hill, J., Knott, T. & Sault, B. Social support, self-efficacy and trauma in new recruits and experienced firefighters. Stress Health 19, 189–193 (2003).
Paulus, D. J., Vujanovic, A. A., Schuhmann, B. B., Smith, L. J. & Tran, J. Main and interactive effects of depression and posttraumatic stress in relation to alcohol dependence among urban male firefighters. Psychiatry Res. 251, 69–75 (2017).
Stanley, I. H., Hom, M. A., Hagan, C. R. & Joiner, T. E. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J. Affect. Disord. 187, 163–171 (2015).
Boffa, J. W. et al. Posttraumatic stress disorder symptoms and suicide risk in male firefighters. J. Nerv. Ment. Dis. 206, 179–186 (2018).
Hom, M. A. et al. The association between sleep disturbances and depression among firefighters: Emotion dysregulation as an explanatory factor. J. Clin. Sleep Med. 12, 235–245 (2016).
Stec, A. A. & Hull, T. R. Fire Toxicity (Woodhead Publishing, 2016).
Mayer, A. C. et al. Characterizing exposures to flame retardants, dioxins, and furans among firefighters responding to controlled residential fires. Int. J. Hyg. Environ. Health 236, 113782 (2021).
Park, J.-S. et al. High exposure of california firefighters to polybrominated diphenyl ethers. Environ. Sci. Technol. 49, 2948–2958 (2015).
Shaw, S. D. et al. Persistent organic pollutants including polychlorinated and polybrominated dibenzo-p-dioxins and dibenzofurans in firefighters from Northern California. Chemosphere 91, 1386–1394 (2013).
Engelsman, M., Toms, L.-M.L., Banks, A. P. W., Wang, X. & Mueller, J. F. Biomonitoring in firefighters for volatile organic compounds, semivolatile organic compounds, persistent organic pollutants, and metals: A systematic review. Environ. Res. 188, 109562 (2020).
Fent, K. W. et al. Flame retardants, dioxins, and furans in air and on firefighters’ protective ensembles during controlled residential firefighting. Environ. Int. 140, 105756 (2020).
Banks, A. P. W., Engelsman, M., He, C., Wang, X. & Mueller, J. F. The occurrence of PAHs and flame-retardants in air and dust from Australian fire stations. J. Occup. Environ. Hyg. 17, 73–84 (2020).
Gill, R. et al. Polybrominated diphenyl ether and organophosphate flame retardants in canadian fire station dust. Chemosphere 253, 126669 (2020).
Hall, S. M. et al. Per- and polyfluoroalkyl substances in dust collected from residential homes and fire stations in North America. Environ. Sci. Technol. 54, 14558–14567 (2020).
Young, A. S. et al. Per- and polyfluoroalkyl substances (PFAS) and total fluorine in fire station dust. J. Expo. Sci. Environ. Epidemiol. 31, 930–942 (2021).
Peaslee, G. F. et al. Another pathway for firefighter exposure to per- and polyfluoroalkyl substances: Firefighter textiles. Environ. Sci. Technol. Lett. 7, 594–599 (2020).
Vuong, A. M. et al. Polybrominated diphenyl ether (PBDE) and poly- and perfluoroalkyl substance (PFAS) exposures during pregnancy and maternal depression. Environ. Int. 139, 105694 (2020).
Wolffe, T. A. M., Clinton, A., Robinson, A., Turrell, L. & Stec, A. A. Contamination of UK firefighters personal protective equipment and workplaces. Sci Rep, (2023).
Fire Brigades Union. Form AR21 Trade Union and Labour Relations (Consolidation) Act 1992: Annual Return for a Trade Union (The Fire Brigades Union). (2019).
Freeman, D., Sheaves, B., Waite, F., Harvey, A. G. & Harrison, P. J. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 7, 628–637 (2020).
Merikangas, K. R. & Gelernter, C. S. Comorbidity for alcoholism and depression. Psychiatr. Clin. North Am. 13, 613–632 (1990).
Boden, J. M. & Fergusson, D. M. Alcohol and depression. Addiction 106, 906–914 (2011).
Morrell, H. E. R. & Cohen, L. M. Cigarette smoking, anxiety, and depression. J. Psychopathol. Behav. Assess 28, 281–295 (2006).
Mikkelsen, K., Stojanovska, L., Polenakovic, M., Bosevski, M. & Apostolopoulos, V. Exercise and mental health. Maturitas 106, 48–56 (2017).
Garbarino, S., Cuomo, G., Chiorri, C. & Magnavita, N. Association of work-related stress with mental health problems in a special police force unit. BMJ Open 3, e002791 (2013).
Jahnke, S. A., Poston, W. S. C., Haddock, C. K. & Murphy, B. Firefighting and mental health: Experiences of repeated exposure to trauma. Work 53, 737–744 (2016).
Robinson, D. J., Coons, M., Haensel, H., Vallis, M. & Yale, J.-F. Diabetes and mental health. Can. J. Diabetes 42, S130–S141 (2018).
Ducat, L., Philipson, L. H. & Anderson, B. J. The mental health comorbidities of diabetes. JAMA 312, 691 (2014).
Licht, C. M. M. et al. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension 53, 631–638 (2009).
Johnson, H. M. Anxiety and hypertension: Is there a link? A literature review of the comorbidity relationship between anxiety and hypertension. Curr. Hypertens. Rep. 21, 66 (2019).
Hewitt, M. & Rowland, J. H. Mental health service use among adult cancer survivors: Analyses of the national health interview survey. J. Clin. Oncol. 20, 4581–4590 (2002).
Massie, M. J. Prevalence of depression in patients with cancer. J. Natl. Cancer Inst. Monogr. 2004, 57–71 (2004).
Peterson, B. et al. An introduction to infertility counseling: A guide for mental health and medical professionals. J. Assist. Reprod. Genet. 29, 243–248 (2012).
Ramezanzadeh, F. et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health 4, 9 (2004).
el Kissi, Y. et al. General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: A comparative study between men and women. Eur. J. Obstet. Gynecol. Reprod. Biol. 167, 185–189 (2013).
Lamers, F. et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study. J. Clin. Psychiatry 72, 341–348 (2011).
Seabold, S. & Perktold, J. Statsmodels: Econometric and statistical modeling with Python. Proc. of the 9th python in science conf http://statsmodels.sourceforge.net/ (2010).
Home Office. Fire Statistics Data Tables - Workforce and Workforce Diversity. https://www.gov.uk/government/statistical-data-sets/fire-statistics-data-tables#workforce-and-workforce-diversity.
NHS Digital. Adult psychiatric morbidity survey: Survey of mental health and wellbeing, England, 2014. https://digital.nhs.uk/data-and-information/publications/statistical/adult-psychiatric-morbidity-survey/adult-psychiatric-morbidity-survey-survey-of-mental-health-and-wellbeing-england-2014.
Navarro, K. Working in smoke: Wildfire impacts on the health of firefighters and outdoor workers and mitigation strategies. Clin. Chest Med. 41, 763–769. https://doi.org/10.1016/j.ccm.2020.08.017 (2020).
Buoli, M. et al. Is there a link between air pollution and mental disorders?. Environ. Int. 118, 154–168. https://doi.org/10.1016/j.envint.2018.05.044 (2018).
Rahman, H. H., Niemann, D. & Munson-Mcgee, S. H. Association among urinary polycyclic aromatic hydrocarbons and depression: A cross-sectional study from NHANES 2015–2016. Environ. Sci. Pollut. Res. https://doi.org/10.1007/s11356-021-16692-3/Published (2022).
Stec, A. A. et al. Occupational exposure to polycyclic aromatic hydrocarbons and elevated cancer incidence in firefighters. Sci. Rep. 8, 1–8 (2018).
Cherry, N. et al. Exposure and absorption of PAHs in wildland firefighters: A field study with pilot interventions. Ann. Work Expo. Health 65, 148–161 (2021).
Gill, B. & Britz-McKibbin, P. Biomonitoring of smoke exposure in firefighters: A review. Curr. Opin. Environ. Sci. Health 15, 57–65. https://doi.org/10.1016/j.coesh.2020.04.002 (2020).
Hollander, J. A. et al. Beyond the looking glass: recent advances in understanding the impact of environmental exposures on neuropsychiatric disease. Neuropsychopharmacology 45, 1086–1096. https://doi.org/10.1038/s41386-020-0648-5 (2020).
Khan, A. et al. Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLoS Biol. 17, e3000353 (2019).
Herbstman, J. B. et al. Prenatal exposure to PBDEs and neurodevelopment. Environ. Health Perspect. 118, 712–719 (2010).
Dórea, J. G. Exposure to environmental neurotoxic substances and neurodevelopment in children from Latin America and the Caribbean. Environ. Res. https://doi.org/10.1016/j.envres.2020.110199 (2021).
Bakolis, I. et al. Mental health consequences of urban air pollution: Prospective population-based longitudinal survey. Soc. Psychiatry Psychiatr. Epidemiol. 56, 1587–1599 (2021).
Calderón-Garcidueñas, L. et al. Air pollution and your brain: What do you need to know right now. Prim. Health Care Res. Dev. 16, 329–345. https://doi.org/10.1017/S146342361400036X (2015).
Pun, V. C., Manjourides, J. & Suh, H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: Results from the NSHAP study. Environ. Health Perspect. 125, 342–348 (2017).
Gładka, A., Rymaszewska, J. & Zatoński, T. Impact of air pollution on depression and suicide. Int. J. Occup. Med. Environ. Health 31, 711–721. https://doi.org/10.13075/ijomeh.1896.01277 (2018).
Stout, J. W., Beidel, D. C., Brush, D. & Bowers, C. Sleep disturbance and cognitive functioning among firefighters. J. Health Psychol. 26, 2248–2259 (2021).
Billings, J. & Focht, W. Firefighter shift schedules affect sleep quality. J. Occup. Environ. Med. 58, 294–298 (2016).
Morphy, H., Dunn, L., Lewis, M., Boardman, H. & Croft, P. Epidemiology of Insomnia: A longitudinal study in a UK population. Sleep 30, 274–280 (2007).
Sullivan, J. P. et al. Randomized, prospective study of the impact of a sleep health program on firefighter injury and disability. Sleep https://doi.org/10.1093/sleep/zsw001 (2017).
Skeffington, P. M., Rees, C. S. & Mazzucchelli, T. Trauma exposure and post-traumatic stress disorder within fire and emergency services in Western Australia. Aust. J. Psychol. 69, 20–28 (2017).
Harvey, S. B. et al. The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. Aust. N. Z. J. Psychiatry 50, 649–658 (2016).
Schmitt, H. J. et al. Chronic environmental contamination: A systematic review of psychological health consequences. Sci. Total Environ. 772, 145025 (2021).
Cherry, N., Galarneau, J.-M., Melnyk, A. & Patten, S. Childhood care and abuse in firefighters assessed for mental ill-health following the Fort McMurray fire of May 2016. J. Affect Disord. Rep. 4, 100090 (2021).
Chatmon, B. N. Males and mental health stigma. Am. J. Mens. Health 14, 155798832094932 (2020).
Cherry, N., Galarneau, J., Haynes, W. & Sluggett, B. The role of organizational supports in mitigating mental ill health in firefighters: A cohort study in Alberta, Canada. Am. J. Ind. Med. 64, 593–601 (2021).
Acknowledgements
We would like to sincerely thank all the firefighters who took part in the survey for their time and service. Gratitude is also extended to the Fire Brigades Union, for their invaluable input and support of the survey, and for distributing the survey to participants. We would also like to acknowledge Lancashire Fire and Rescue Service for their participation in pilot versions of the survey.
Funding
The UK Firefighter Contamination Survey was funded by the Fire Brigades Union and the University of Central Lancashire.
Author information
Authors and Affiliations
Contributions
A.C. and A.S. devised the survey and distributed it to firefighters with the assistance of the Fire Brigades Union. T.W. calculated logistic regression analyses, with input from L.T. and A.R. T.W. drafted the first iteration of the manuscript. A.S. and T.W. reviewed and edited the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no known competing interests. AC and LT are PhD Researchers, who were affiliated with UCLan at the time the survey was conducted.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wolffe, T.A.M., Robinson, A., Clinton, A. et al. Mental health of UK firefighters. Sci Rep 13, 62 (2023). https://doi.org/10.1038/s41598-022-24834-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-24834-x
- Springer Nature Limited
This article is cited by
-
Culture and awareness of occupational health risks amongst UK firefighters
Scientific Reports (2023)
-
Contamination of UK firefighters personal protective equipment and workplaces
Scientific Reports (2023)