Abstract
We aimed to identify the association between Hounsfield Unit(HU)-related variables and percutaneous nephrolithotomy (PCNL) outcomes. We enrolled patients with single renal stones (1–3 cm) who underwent single-tract PCNL between January 2014 and October 2019. Demographics and stone characteristics were retrospectively reviewed. Preoperative computerized tomography (CT) and follow-up CT within at least 3 months after PCNL were included in this analysis. Stone-free status was defined as residual stone measuring ≤ 2 mm within 3 months postoperatively. HU and cross-sectional area (CSA) were measured using the free-draw technique. We analyzed HU-related variables using logistic regression model for outcomes. Altogether, 188 out of 683 patients met the inclusion criteria. The stone-free rate (SFR) was 79.2%. There were no significant differences in age, sex, BMI, ASA class, laterality, pre-op shockwave lithotripsy, stone size, stone burden, skin-to-stone distance, and HU between the stone-free and remnant groups. CSA and HU/CSA in the stone-free and remnant groups were 94.5 ± 46.1 and 128.3 ± 98.5 (p = 0.043) and 10.1 ± 5.6 and 7.3 ± 3.4 (p = 0.001), respectively. Multivariate logistic regression analysis revealed that pelvis, ureteropelvic junction stones, and HU/CSA were independent predictors of SFR. HU did not affect PCNL outcomes. We believe that HU/CSA could be used for determining stone treatment plans and predicting outcomes.
Similar content being viewed by others
Introduction
Noncontrast computed tomography (NCCT) is widely accepted for diagnosing urolithiasis. It has higher sensitivity (> 94%) and specificity (> 95%) than plain radiography ultrasonography and intravenous pyelography1. The information obtained from NCCT to determine treatment modality includes stone size, multiplicity, location, anatomic anomaly, skin-to-stone distance, stone density (Hounsfield unit [HU]), and fragility (stone heterogeneity index [SHI] and variation coefficient [VCSD])2,3,4,5. The size of the stone is important in predicting the possibility of spontaneous passage. HU, SHI, and VCSD are related to stone composition and fragility, and they determine the success of shock wave lithotripsy (SWL). However, there are few studies in the literature regarding the predictive role of HU in the outcomes of percutaneous nephrolithotomy (PCNL)6,7,8,9.
The stone scoring systems used to predict the outcome of PCNL are the STONE, CROES nephrolithometric nomogram, and Guy’s stone score10,11,12. These scoring systems were suggested based on the stone number, HU, burden, location, anatomical abnormality, and the surgeon’s experience. Of these scoring systems, only the STONE scoring system includes HU; however, in this scoring system, the clinical evidence for setting HU (950) as the cut-off value is insufficient.
This study aimed to identify the association between the HU-related variables and outcome of PCNL. We introduced the concept of stone density based on HU and cross-sectional area (CSA) as a possible predictor of PCNL outcome.
Materials and methods
Ethics approval
This study was approved by the Institutional Review Board of The Catholic University of Korea (approval number KC18RESI0836). All procedures performed in study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All information used for statistical analysis was anonymized, and the requirement for obtaining informed consent was waived by the Institutional Review Board of The Catholic University of Korea.
Patient selection and study design
We retrospectively reviewed data of 683 consecutive patients who underwent PCNL at a single tertiary institution between January 2014 and October 2019. Overall, 188 patients with single-tract PCNL and a maximal stone diameter of 10–30 mm were included and evaluated with pre- and postoperative CT scans. Our study analyzed the impact of HU-related variables on PNL, Therefore, the stone size, which is generally known to have a significant impact on success rates, was limited to single stones with 10–30-mm size. The 10–20-mm sized stones in the lower calyx were included according to the stone management guidelines13. We retrospectively evaluated the patients’ characteristics, stone-related variables measured by NCCT, and operation parameters (operative (OP) time, stone-free rate, hemoglobin, hematocrit, creatinine, hospital stay, and complications). The stone-related variables were stone diameter, stone location [ureteropelvic junction (UPJ), renal pelvis, lower/mid/upper calyx], stone maximal CSA, skin-to-stone distance, HU value using the free-draw method at the maximal CSA, and the SHI (Standard deviation of HU). Among the axial and coronal views, the larger CSA was set as the reference value at the bone setting view. The free-draw method is done easily using the PACS program by utilizing digital free-hand calipers (Fig. 1). Moreover, it was measured by directly laying it out using a free hand along the inner layer of the stone shape in maximal CSA. Two urologists, including a urologic resident, evaluated the stone status and performed stone measurement and calculation.
Free draw measurement technique of renal stone. Axial vs. coronal view, and soft tissue setting vs. bone setting view. In soft tissue and bone setting views, the stone has almost similar Hounsfield unit and stone heterogeneity index values. In the axial and coronal views, the value of the maximal stone diameter is equal to 29 mm; however, the cross-sectional areas are 153 and 235 mm2, respectively.
We defined stone-free status (SFS) as the absence of residual fragments or presence of a clinically insignificant remnant stone (≤ 2 mm). OP time was defined as the time from percutaneous access puncture to the final dressing at the incision site.
Post-PCNL outcome data were retrospectively collected from electronic medical records. Pre- and postoperative radiologic evaluation of the kidneys, ureter, and bladder (KUB) and NCCT examinations were performed in all patients. All patients who underwent PCNL were evaluated by plain KUB radiography and NCCT within 3 months postoperatively. All cases were analyzed at 1 week, 4–8 weeks, and 3–6 months postoperatively. Patients with remnant stone fragments were followed up every 6 months after routine follow-up.
All procedures were performed by experienced endourologist who performed more than 150 cases of PCNL in a year. The exclusion criteria for this study were simultaneous bilateral PCNL and multiple approaches requiring more than two nephroscopic tracts. Perioperative variables and baseline demographics were compared between patients with SFS and remnant status. The preoperative data included body mass index, American Society of Anesthesiology classification, and preoperative SWL (Table 1). The operative data and complication data were also reviewed. Complications were recorded according to the modified Clavien system for reporting complications14. The primary endpoint was to calculate the correlations between HU-related variables and PCNL outcomes.
Surgical technique
Urinalyses and cultures were obtained preoperatively for all patients, and prophylactic antibiotics were administered according to the results.
The procedures were performed with the patients in prone position after undergoing cystoscopic ureteral catheter insertion, which was carried out under general anesthesia. The Foley catheter is inserted after ureteral catheterization. It is then placed in a sterile bag with a ureteral catheter to prevent dislocation and contamination before prone position. Foley catheter is removed on postoperative day 1. Percutaneous access was achieved using fluoroscopic guided puncture, with balloon dilatation up to 24 Fr. A 20-Fr nephroscope was used for the procedure. The stone was fragmented using pneumatic and ultrasonic devices (Swiss Lithoclast, EMS Electro Medical System, Switzerland). Once PCNL was completed, the collecting system was carefully inspected, and a nephrostogram was performed to exclude remnant stones. The procedure was terminated without nephrostomy tube insertion, unless there were any intraoperative events or suspected residual stones. D–J insertion was not performed routinely unless there was an edematous UPJ, suspected remnant stones, or significant bleeding during the procedure15.
Statistical analyses
Continuous variables are reported as mean ± SD or range and were compared using independent sample Student’s t-test or Mann–Whitney U test as appropriate. Categorical variables were analyzed for statistical significance using Chi-square or the linear-by-linear association test. We calculated using the G*Power 3.1 Window program, required number of samples for logistic regression was at least 158 (α error 0.05, power 1 − β = 0.80, Odds Ratio (OR) = 0.6, and Pr(Y = 1 | X = 1)H0 = 0.3), making the number of subjects in this study sufficient to obtain power. We used a logistic regression model to perform univariate and multivariate assessments to determine the predictors of SFS and OP time. p-values < 0.05 were considered statistically significant. Inter observer reliability was assessed with the intraclass correlation coefficient (ICC)16. Statistical analysis was performed using R software (version 3.3.2, R Foundation for Statistical Computing, Vienna, Austria; http://r-project.org). G power 3.1 for window.
Results
Patient demographics, stone characteristics, and perioperative data
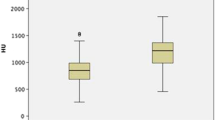
From January 2014 to October 2019, 683 patients underwent PCNL. Subsequently, 495 were excluded due to stone number, size, and tract number. Finally, 188 patients met the inclusion criteria. After PCNL, the SFS rate was 79.2% (149/188) and the remnant rate was 20.8% (39/188). Demographics, operative factors, and stone characteristics were compared between the stone-free and remnant groups (Tables 1, 2); significant differences were found in lower calyx stone (25.5% vs. 48.7%, p = 0.009), pelvis and UPJ stone (62.4% vs. 33.3%, p = 0.002), stone CSA (94.5 ± 46.1 vs. 128.3 ± 98.5, p = 0.043), HU/CSA (10.1 ± 5.6 vs. 7.3 ± 3.4, p = 0.001), and OP time (56.4 ± 22.6 vs. 6.55 ± 22.9, p = 0.027). The modified Clavien–Dindo classification was used for complication categorization (Table 3). In total, 31 complications occurred in 25 (13.3%) patients.
Multivariate logistic regression of SFR
In the univariate analysis, the following factors were significantly related to remnant status: lower calyx stone (p = 0.006, Odds ratio = 2.77), pelvis or UPJ stone (p = 0.002, Odds ratio = 0.30), stone CSA (p = 0.013, Odds ratio = 2.77), and HU/CSA (p = 0.00, Odds ratio = 0.87). In a final model of the multivariate logistic regression analysis, pelvis and UPJ stone (p = 0.003, Odds ratio = 0.65) and HU/CSA (p = 0.027, Odds ratio = 0.90) were independent significant predictors of SFS in overall patients (Table 4). Lower calyx stone, SSD, HU, SHI, Radio-opacity did not affect the SFS. The stone status prediction logistic regression model was shown to be significant (× 2 = 22.497, p = 0.001), and the Nagelkerke coefficient of determination (R2) of the model showed a 48.7% explanatory power.
Discussion
In this study, we focused on the association between HU-related variables and PCNL outcome measured by CT using the free-draw stone measurement method. The main study findings were as follows: factors that affect single-stone PCNL SFR are stone location and HU/CSA; and the factor that affects OP time is the CSA.
For the association between HU and the outcome of PCNL, Gucuk et al.6,9 reported that the cut-off value of HU should be 677.5, and the success rate decreases if the HU value is low. Meanwhile, Alper et al.7 suggested that there is no correlation between HU, success rates, and OP time, and that fluoroscopy time is prolonged when the HU value is high. The only large-scale study was conducted by CROES Group in 2013 using a multicenter design; the authors reported that the success rate decreased for very low- and high-density stones, and longer OP times were required8. As such, there is no consensus regarding the effects of HU on PCNL outcomes. The major reason for inconsistency is the lack of inter-observer reliability and reproducibility because of different methods for measuring HU.
In the present study, the location that affected stone-free rate was the renal pelvis; these stones are graded I in the Guy's stone scoring system. Using HU/CSA as the predictor of PCNL outcome, we demonstrated a tendency toward a high stone-free rate for stones that have high HU/CSA values. This can be explained by the fact that SFR would be high as HU increases in the same CSA and that SFR would be high as CSA decreases in the same HU.
In the CROES study8, PCNL success probability was low for very low- and high-density stones. First, that study did not employ a consistent measurement methodology across a large number of centers. Second, there was a heterogeneity in terms of stone assessment due to the differences in CT slice thickness and energy protocols. Third, HU tends to increase in proportion to the size of the stone17 and the proportion of radio-opacity increases as HU increases. Considering all of these points, it would be insufficient to believe that the effect of HU itself on OP time is significant. In our study, there were no significant differences in terms of analysis of OP time based on HU, radio-opacity, and stone heterogeneity index. Furthermore, there was no significant correlation between OP time and HU as a continuous variable.
Considering stone size measurement, Patel et al. raised issues regarding limits because of high inter-observer variability from the existing manual measurement and the proposed effectiveness of stone measurement methods using commercialized computer programs18,19. Nevertheless, there is insufficient clinical or cost-related evidence to start using it in clinical practice. On the other hand, regarding the free-draw measurement we used, Tanaka et al.20 suggested the efficiency of the measurement using stone CSA and using it to predict the SWL outcome.
In terms of standardization of HU measurement, Narayan et al.21 compared region-of-interest measurement techniques. There appears to be no consensus regarding which measurement technique is effective. Motley et al.22 and Nakada et al.23 reported that HU and stone diameter ratio were important factors for predicting calcium stone and uric acid stone outcomes. To the best of our knowledge, the present study is the first to report the ratio of HU and CSA and its effect on PCNL outcomes.
Understanding that there is no standard measurement method, our free-draw technique can be used as a single measurement in almost all PACS programs. Moreover, we limited our study population to a single stone that is larger than the size of CT thickness and minimized the partial volume effect. The homogeneity of this dataset represents an advantage of the present study.
Despite these advantages, our study has several limitations. First, it has a retrospective design with a small number of patients. Although, the stone range (1.0–3.0 cm) makes the group heterogeneous, it can be considered that bias was minimized because it was targeted for single-stone and single-tract PCNL patients. Recently, along with a growing trend of offering patients with ‘decided choice’ of surgery, it is important to note that there is a possibility of offering flexible ureteroscopy in patients with stones with < 2 cm in size or even a ‘combo approach’ with SWL and flexible ureteroscopy24. Second, there is a possibility that the CSA/HU ratio as the predictor could be a confounding variable. Because HUs tend to increase with increasing stone size25, CSA alone may be the factor for determining SFR. Moreover, it possible that a measurement bias exists between the physicians using the free-draw stone measurement method. However, in measuring the Hounsfield unit, it is known that inter/intra observer variability shows a high probability of agreement regardless of the measurement method26, and our data also showed agreement in intraclass correlation coefficient analysis. Nevertheless, maximal stone diameter, CSA, and HU were not significant predictive factors for SFR, and we minimized the possibility of confounding variables using multivariate logistic regression. There are many variables that affect PCNL outcome, our study group contains only single stone and single tract PCNL patients. Finally, we did not include the analysis of stone composition. For these reasons, a prospective study on larger numbers is required, with the analysis of stone composition included.
In conclusion, there was no effect of HU itself on PCNL outcome. However, a HU-related variable, HU/mm2, was predictive of SFR. We believe that HU/CSA could be used to design stone treatment plans and to predict PCNL outcomes. With future research, HU/CSA could be used as an effective variable in determining ureteroscopic surgery and SWL outcome.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Smith, R. C., Verga, M., McCarthy, S. & Rosenfield, A. T. Diagnosis of acute flank pain: Value of unenhanced helical CT. AJR Am. J. Roentgenol. 166, 97–101 (1996).
Gucuk, A. & Uyeturk, U. Usefulness of hounsfield unit and density in the assessment and treatment of urinary stones. World J. Nephrol. 3, 282–286 (2014).
Lee, J. Y. et al. Stone heterogeneity index as the standard deviation of Hounsfield units: A novel predictor for shock-wave lithotripsy outcomes in ureter calculi. Sci. Rep. 6, 23988. https://doi.org/10.1038/srep23988 (2016).
Yamashita, S. et al. Variation coefficient of stone density: A novel predictor of the outcome of extracorporeal shockwave lithotripsy. J. Endourol. 31, 384–390 (2017).
Waqas, M., Saqib, I. U., Jamil, M. I., Khan, M. A. & Akhter, S. Evaluating the importance of different computed tomography scan-based factors in predicting the outcome of extracorporeal shock wave lithotripsy for renal stones. Investig. Clin. Urol. 59, 25–31 (2018).
Gucuk, A. et al. Does the Hounsfield unit value determined by computed tomography predict the outcome of percutaneous nephrolithotomy?. J. Endourol. 26, 792–796 (2012).
Gok, A. et al. The hounsfield unit value calculated with the aid of non-contrast computed tomography and its effect on the outcome of percutaneous nephrolithotomy. Urolithiasis. 43, 277–281 (2015).
Anastasiadis, A. et al. Impact of stone density on outcomes in percutaneous nephrolithotomy (PCNL): An analysis of the clinical research office of the endourological society (CROES) PCNL global study database. Scand. J. Urol. 47, 509–514 (2013).
Gucuk, A., Yilmaz, B., Gucuk, S. & Uyeturk, U. Are stone density and location useful parameters that can determine the endourological surgical technique for kidney stones that are smaller than 2 cm? A prospective randomized controlled trial. Urol. J. 16, 236–241 (2019).
Okhunov, Z. et al. S.T.O.N.E. nephrolithometry: Novel surgical classification system for kidney calculi. Urology 81, 1154–1159 (2013).
Smith, A. et al. A nephrolithometric nomogram to predict treatment success of percutaneous nephrolithotomy. J. Urol. 190, 149–156 (2013).
Thomas, K., Smith, N. C., Hegarty, N. & Glass, J. M. The Guy’s stone score—grading the complexity of percutaneous nephrolithotomy procedures. Urology 78, 277–281 (2011).
Türk, C. et al. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur. Urol. 69, 468–474 (2016).
de la Rosette, J. J. et al. Categorisation of complications and validation of the Clavien score for percutaneous nephrolithotomy. Eur. Urol. 62(2), 246–255 (2012).
Choi, S. W. et al. Totally tubeless versus standard percutaneous nephrolithotomy for renal stones: Analysis of clinical outcomes and cost. J. Endourol. 28, 1487–1494 (2014).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163 (2016).
Stewart, G. et al. Stone size limits the use of Hounsfield units for prediction of calcium oxalate stone composition. Urology 85, 92–95 (2015).
Patel, S. R. et al. Automated renal stone volume measurement by noncontrast computerized tomography is more reproducible than manual linear size measurement. J. Urol. 186, 2275–2279 (2011).
Yamashita, S. et al. Three-dimensional mean stone density measurement is superior for predicting extracorporeal shock wave lithotripsy success. Int. J. Urol. 26, 185–191 (2019).
Tanaka, M. et al. Stone attenuation value and cross-sectional area on computed tomography predict the success of shock wave lithotripsy. Korean J. Urol. 54, 454–459 (2013).
Narayan, V. M. et al. Evaluating region of interest measurement strategies to characterize upper urinary tract stones on computerized tomography. J. Urol. 197, 715–722 (2017).
Motley, G., Dalrymple, N., Keesling, C., Fischer, J. & Harmon, W. Hounsfield unit density in the determination of urinary stone composition. Urology 58, 170–173 (2001).
Nakada, S. Y. et al. Determination of stone composition by noncontrast spiral computed tomography in the clinical setting. Urology 55, 816–819 (2000).
Inoue, T., Okada, S., Hamamoto, S. & Fujisawa, M. Retrograde intrarenal surgery: Past, present, and future. Investig. Clin. Urol. 62, 121–135 (2021).
Williams, J. C. Jr. et al. Correction of helical CT attenuation values with wide beam collimation: In vitro test with urinary calculi. Acad. Radiol. 8, 478–483 (2001).
Disselhorst, G. W. et al. Inter- and intraobserver agreement in measuring urolithiasis density on nonenhanced computed tomography. J. Endourol. 34, 417–422 (2020).
Funding
This study was supported by Research Fund of Seoul St. Mary’s Hospital, The Catholic University of Korea.
Author information
Authors and Affiliations
Contributions
H.W.M.: manuscript writing, statistics, and project development; M.T.: manuscript editing; Y.H.P.: project development, manuscript editing, and data collection; W.J.B.: manuscript editing and project development; U-S.H.: manuscript editing and project development; S-H.H.: project development; J.Y.L.: project development; S.W.K.: project development; H.J.C.: project development, data collection, and statistics. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moon, H.W., Taeyb, M., Park, Y.H. et al. The impact of Hounsfield unit-related variables on percutaneous nephrolithotomy outcomes. Sci Rep 12, 18451 (2022). https://doi.org/10.1038/s41598-022-23383-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23383-7
- Springer Nature Limited