Abstract
Smoking is a trigger for asthma, which has led to an increase in asthma incidence in China. In smokers, asthma management starts with smoking cessation. Data on predictors of smoking cessation in Chinese patients with asthma are scarce. The objective of this study was to find the differences in clinical characteristics between current smokers and former smokers with asthma in order to identify factors associated with smoking cessation. Eligible adults with diagnosed asthma and smoking from the hospital outpatient clinics (n = 2312) were enrolled and underwent a clinical evaluation, asthma control test (ACT), and pulmonary function test. Information on demographic and sociological data, lung function, laboratory tests, ACT and asthma control questionnaire (ACQ) scores was recorded. Patients were divided into a current smokers group and a former smokers group based on whether they had quit smoking. Logistic regression analysis was used to analyze the factors associated with smoking cessation. Of all patients with asthma, 34.6% were smokers and 65.4% were former smokers, and the mean age was 54.5 ± 11.5 years. Compared with current smokers, the former smokers were older, had longer duration of asthma, had higher ICS dose, had more partially controlled and uncontrolled asthma, had more pack-years, had smoked for longer, and had worse asthma control. The logistic regression model showed that smoking cessation was positively correlated with age, female sex, pack-years, years of smoking, partially controlled asthma, uncontrolled asthma, and body mass index (BMI), but was negatively correlated with ACT, FEV1, FEV1%predicted, and widowed status. More than 30% of asthma patients in the study were still smoking. Among those who quit smoking, many quit late, often not realizing they need to quit until they have significant breathing difficulties. The related factors of smoking cessation identified in this study indicate that there are still differences between continuing smokers and former smokers, and these factors should be focused on in asthma smoking cessation interventions to improve the prognosis of patients with asthma.
Similar content being viewed by others
Introduction
Asthma is a prevalent and highly heterogeneous chronic respiratory inflammatory disease that affects about 300 million people worldwide1. Cigarette smoking is one of the preventable triggers of asthma and many previous studies have assessed the relationship between smoking and asthma2. Kim et al. found that the incidence of wheezing and exercise-induced wheezing increased with the increase of total pack-years of smoking among current smokers and former smokers3. In addition, long-term smoking significantly reduced the sensitivity of asthma patients to inhaled corticosteroids (ICS) and caused a significant decrease in forced expiratory volume in 1 s (FEV1)4,5.
Recent studies have shown that quitting smoking improves asthma control in smokers with asthma, while airway hyperresponsiveness, neutrophils and fractionated exhaled nitric oxide (FeNO) are reduced, leading to reduced chronic inflammation of the airways6,7. Mathias et al. found that smoking cessation was related to the number of years of smoking and the level of education received, and the quit rate of middle-aged smokers was significantly higher8. In addition, a new diagnosis of asthma was associated with an increased rate of quitting smoking in a Norwegian study of general trends in smoking cessation9. These factors may be related to smoking cessation. However, there is currently little data on smoking cessation among Chinese asthma patients. In this study, we aim to understand the characteristics of asthma in current smokers and former smokers in order to identify the key factors driving smoking cessation.
Patients and methods
Study participants and definitions
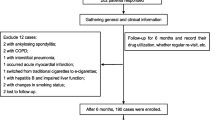
This study was approved by the Ethics Review Committee of the Second Xiangya Hospital of Central South University (Ethical Code: LYF2021159), all participants signed an informed consent form and all experiments were performed in accordance with the Declaration of Helsinki. Initially, we included 3816 patients with asthma registered in the outpatient department of the Second Xiangya Hospital of Central South University (Hunan, China) between January 2017 and June 2021. Asthma was diagnosed according to the Global Initiative for Asthma (GINA)10, with bronchodilation FEV1 change > 200 ml and 12%; Bronchial stimulation test was positive; Symptoms of asthma (including wheezing, difficulty breathing, chest tightness or coughing) occur. All patients were treated with a combination of ICS and long-acting β2 agonist (ICS/LABA). The non-smokers were defined as participants who had never smoked or had smoked fewer than 100 cigarettes in their lifetime. Smokers were defined as having smoked continuously for more than 10 pack-years. The former smokers were defined as participants who had quit smoking for at least 6 months prior to the study. Patients who had never smoked, had no registered smoking history, had less than 10 pack-years, and were younger than 18 years old were excluded. A detailed description of the flow diagram for recruiting voluntary patients can be found in Fig. 1.
Data collection
After the collection of written informed consent, participants’ age, sex, duration of asthma, drug treatment, exacerbation, asthma and chronic obstructive pulmonary disease overlap (ACO) occurrence, education level, marital status and smoking status were documented. Height and weight were measured, and body mass index (BMI) was calculated. Meanwhile, laboratory tests [e.g., immunoglobulin E (IgE), blood eosinophils, blood neutrophils, FeNO], asthma control test (ACT), asthma control questionnaire (ACQ), asthma control, and pulmonary function test (PFT) results were recorded. This included FEV1 and forced vital capacity (FVC), and the values of FEV1/FVC and FEV1%predicted were calculated. ACT scores range from 0 to 25, with a score of 20–25 indicating good asthma control and a score below 20 indicating poor asthma control11. ACQ consists of seven items, each of which ranges from 0 (fully controlled) to 6 (severely uncontrolled). ACQ scores are the average of the seven items and current studies have established the cut-off values for controlled asthma (ACQ ≤ 0.75 points) and poorly controlled asthma (ACQ ≥ 1.5 points)12.
Patient selection
A total of 2312 patients (including 1511 former smokers and 801 current smokers) were included in this study, excluding 1504 patients (859 patients with no smoking history, 130 patients with no record of weight or height, 95 patients who refused to participate, 180 patients who smoked less than 10 pack-years, and 240 never-smokers).
Statistical analysis
SPSS 26.0 software (IBM Corp.) was used to perform all statistical analyses, and GraphPad Prism 8.0.1 software (GraphPad Software Inc) was used to generate the graphs. Continuous variables were described as the mean and standard deviation (SD) or median (interquartile range, IQR), and categorical variables were expressed as the number (percentage). Differences between the two groups were determined using Student’s t test, and the Mann–Whitney U test. Multivariate logistic regression was used to calculate the odds ratio (ORs) of various adjustments. A P-value < 0.05 indicated a statistically significant difference.
Statement of ethics
This study was approved by the Ethics Review Committee of the Second Xiangya Hospital of Central South University (Ethical Code: LYF2021159), all participants signed an informed consent form and all experiments were performed in accordance with the Declaration of Helsinki.
Results
Demographic characteristics
Table 1 shows the demographic and sociological characteristics, lung function indexes and biochemical indexes of the 2312 participants, including 801 current smokers and 1511 former smokers. The mean age was 52.4 ± 11.2 years for current smokers and 55.5 ± 11.1 years for former smokers (Table 1). There were significant differences in age, sex, asthma duration, marital status, education and BMI between the current smokers and former smokers. Compared with the current smokers, the former smokers were older, had longer duration of asthma, had higher ICS dose, had more partially controlled and uncontrolled asthma, had lower ACT scores, FEV1, FEV1/FVC, and FEV1%predicted, as well as more pack-years and longer duration of smoking. Interestingly, the current smokers had higher IgE, FeNO, blood eosinophils, and blood neutrophils, but lower mean ACQ scores compared to the former smokers. Detailed information regarding participant characteristics is shown in Table 1.
Multivariate logistic regression analysis of factors associated with smoking cessation based on clinical parameters and sociodemographic characteristics
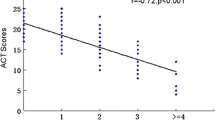
Multivariate logistic regression was used to analyze the factors significantly associated with smoking cessation based on clinical parameters and sociodemographic characteristics. According to the clinical parameters, ACT was negatively associated with smoking cessation, with an OR of 0.907 (95% CI = 0.862–0.956), while partially controlled and uncontrolled asthma were positively correlated with smoking cessation, with an OR of 2.733 and 1.801 (95% CI = 2.084–3.583, 1.045–3.103), respectively. Patients were more likely to quit smoking if they had poor pulmonary function, with an OR of 0.722 (95% CI = 0.629–0.828) for FEV1 and 0.991 for FEV1%predicted (95% CI = 0.986–0.996) (Table 2). According to the sociodemographic characteristics, patients who were widowed were less likely to quit, with an OR of 0.059 (95% CI = 0.025–0.142). BMI was positively correlated with smoking cessation, with an OR of 1.156 (95% CI = 1.114–1.199). Patients who were older and had more pack-years were more likely to quit smoking, with an OR of 2.789 and 1.063 (95% CI = 1.008–7.716, 1.039–1.088), respectively. Patients who had longer asthma duration and higher ICS dose were more likely to quit smoking, with an OR of 1.023 and 1.441 (95% CI = 1.013–1.033, 1.053–1.972), respectively. Patients who had more years of smoking were more likely to quit smoking, with an OR of 1.033 (95% CI = 1.002–1.064). Meanwhile, females were also more likely to quit smoking compared to males, with an OR of 3.694 (95% CI = 2.770–4.926) (Table 3).
Discussion
Asthma, characterized by chronic airway inflammation, is a highly heterogeneous disease. This cross-sectional descriptive study including outpatients with asthma compares the different characteristics of current smokers and former smokers. Previous studies have not found any relationship between smoking and asthma control13. However, in this study, we found that compared with the current smokers, the former smokers were older, had longer duration of asthma, had higher ICS dose, had lower ACT scores, FEV1, FEV1/FVC, FEV1%predicted and more pronounced asthma symptoms. These findings suggest that most asthma patients continue to smoke until they experience significant symptoms of wheezing, discomfort and shortness of breath. Several studies have found that smoking contributes to increased morbidity and mortality, exacerbation of symptoms and frequent hospitalizations in asthmatic patients14,15,16. At the same time, asthmatics in the smoking group had more frequent asthma attacks, an increased number of life-threatening asthma attacks, and a higher mortality rate among heavy smokers compared to asthmatic non-smokers17,18,19. Polosa et al. found that duration of smoking and smoking status were significantly associated with asthma severity in a dose-dependent manner, with the most significant association with disease severity observed among smokers who smoked for more than 20 pack-years20. Evidence of causality is supported by a significant association between asthma severity and active smoking and a clear dose–response relationship. Smoking can cause acute constriction of the bronchi in patients with asthma, resulting in reduced lung function, and the effect of smoking on reduced lung function in patients with chronic obstructive lung disease has been proven21. In addition, long-term exposure to cigarette smoke can promote proliferation and activation of bronchial epithelial cells, goblet cells, smooth muscle cells and fibroblasts, leading to excessive secretion of mucus, fibrosis, extracellular matrix deposition and airway remodeling, leading to accelerated decline of FEV1 and increased severity of airflow obstruction21,22.
Studies have shown that asthmatic smokers who quit smoking have significantly improved quality of life, and reduced nighttime and daytime rescue β2-agonist use, ICS use, daytime asthma symptoms and airway hyperreactivity. They also show increased sensitivity to ICS, and improved asthma management21,23. Therefore, the daily management of asthma patients should strengthen the propaganda and education of smoking cessation, in order to improve symptoms and prevent the deterioration of the condition. The current study found some factors associated with smoking cessation. We observed a significant negative association between ACT and smoking cessation. Patients with well-controlled asthma are less likely to quit smoking. We found that FEV1 and FEV1%predicted were negatively associated with smoking cessation, and patients were more likely to quit smoking when they had dyspnea and worsening symptoms. Our results are consistent with the findings of Godtfredsen et al. that smoking cessation is promoted when lung function is impaired24. We found that duration of asthma and ICS dose were positively associated with smoking cessation. Studies have shown that long-term smoking can promote the occurrence of fixed airflow obstruction and induce ICS resistance to increase ICS dose25,26,27. We observed a positive correlation between age and smoking cessation, with smokers becoming more aware of the need to quit as they get older, consistent with previous studies18. A study has found that quitting behavior varies by age group, with those over 50 more likely to quit28. We found that widowed patients were less likely to quit smoking than married patients, probably because they lived alone. Studies have shown that people who live with a partner or who are married are more likely to quit, those who live alone are less likely to quit, and quitting is more likely to fail if their partner is also a smoker29,30,31. We observed that females are more likely to quit smoking than males, consistent with previous research32. In this study, we found that compared with the current smokers, the former smokers had higher BMI, which is consistent with previous findings and may be related to increased appetite after quitting33,34. We also found a positive association between BMI and smoking cessation. Studies have shown that BMI has been identified as a risk factor for the development of asthma, the incidence of asthma increases with obesity, and obese individuals are more difficult to control, which is more likely to promote smoking cessation35,36,37. However, it may reduce the likelihood of quitting, which can be accompanied by weight gain33. We discovered that patients who had consumed more pack-years and had more years of smoking were more likely to quit smoking. Studies have shown that health scares can influence the smoking behavior of smokers, including those of family or friends. Wang et al. found that health scares reduced the likelihood of heavy smoking (> 20 cigarettes/day) by 41.6% compared with moderate and light smoking, and increased the likelihood of ever smokers to quit by 85.3%38. The duration and total pack-years of smoking were positively correlated with wheezing and exercise wheezing3. Meanwhile, studies showed that the amount of smoking is an important factor in successful quitting, and smokers who consumed more cigarettes were more likely to quit32,39.
There were some limitations of this study: (a) This is a cross-sectional descriptive study; therefore, we cannot draw conclusions about the direction of causation, and the results of this study can only provide data related to smoking cessation, but not on predictive factors. (b) Since we relied on self-reports to determine smoking status, patients’ desire to respond to social expectations might lead to underestimation of smoking status, as well as recall bias. (d) The mechanisms of the factors associated with smoking cessation are unexplained and need to be further explored.
Conclusions
In conclusion, more than 30% of asthma patients in the study were still smoking. Among those who quit smoking, many quit late, often not realizing they need to quit until they have significant breathing difficulties. The related factors of smoking cessation identified in this study indicate that there are still differences between continuing smokers and former smokers, and these factors should be focused on in asthma smoking cessation interventions to improve the prognosis of patients with asthma (Supplementary information).
Data availability
The data used and analyzed in this study are available from the corresponding author on reasonable request; E-mail: xudongxiang@csu.edu.cn.
Abbreviations
- ACQ:
-
Asthma control questionnaire
- ACT:
-
Asthma control test
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FeNO:
-
Fractionated exhaled nitric oxide
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HAT:
-
Histone acetylases
- HDAC:
-
Histone deacetylases
- ICS:
-
Inhaled corticosteroids
- IgE:
-
Immunoglobulin E
- IL-4:
-
Interleukin-4
- IQR:
-
Interquartile range
- OR:
-
Odd ratio
- PFT:
-
Pulmonary function test
- Ppb:
-
Parts per billion
- M ± SD:
-
Mean ± standard deviation
- T2:
-
Type 2
- Th2:
-
T-helper cell type 2
References
Zhang, F., Hang, J., Zheng, B., Su, L. & Christiani, D. C. The changing epidemiology of asthma in Shanghai, China. J. Asthma 52, 465–470. https://doi.org/10.3109/02770903.2014.982762 (2015).
Beasley, R., Semprini, A. & Mitchell, E. A. Risk factors for asthma: is prevention possible?. Lancet 386, 1075–1085. https://doi.org/10.1016/s0140-6736(15)00156-7 (2015).
Kim, S. Y., Sim, S. & Choi, H. G. Active and passive smoking impacts on asthma with quantitative and temporal relations: A Korean Community Health Survey. Sci. Rep. 8, 8614. https://doi.org/10.1038/s41598-018-26895-3 (2018).
Thomson, N. C. & Chaudhuri, R. Asthma in smokers: Challenges and opportunities. Curr. Opin. Pulm. Med. 15, 39–45. https://doi.org/10.1097/MCP.0b013e32831da894 (2009).
Shimoda, T., Obase, Y., Kishikawa, R. & Iwanaga, T. Influence of cigarette smoking on airway inflammation and inhaled corticosteroid treatment in patients with asthma. Allergy Asthma Proc. 37, 50–58. https://doi.org/10.2500/aap.2016.37.3944 (2016).
Westergaard, C. G., Porsbjerg, C. & Backer, V. The effect of smoking cessation on airway inflammation in young asthma patients. Clin. Exp. Allergy 44, 353–361. https://doi.org/10.1111/cea.12243 (2014).
Piccillo, G. et al. Changes in airway hyperresponsiveness following smoking cessation: Comparisons between Mch and AMP. Respir. Med. 102, 256–265. https://doi.org/10.1016/j.rmed.2007.09.004 (2008).
Holm, M. et al. Predictors of smoking cessation: A longitudinal study in a large cohort of smokers. Respir. Med. 132, 164–169. https://doi.org/10.1016/j.rmed.2017.10.013 (2017).
Danielsen, S. E., Løchen, M. L., Medbø, A., Vold, M. L. & Melbye, H. A new diagnosis of asthma or COPD is linked to smoking cessation—The Tromsø study. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 1453–1458. https://doi.org/10.2147/copd.S108046 (2016).
Boulet, L. P. et al. The Global Initiative for Asthma (GINA): 25 years later. Eur. Respir. J. https://doi.org/10.1183/13993003.00598-2019 (2019).
Nathan, R. A. et al. Development of the asthma control test: A survey for assessing asthma control. J. Allergy Clin. Immunol. 113, 59–65. https://doi.org/10.1016/j.jaci.2003.09.008 (2004).
Jia, C. E. et al. The asthma control test and asthma control questionnaire for assessing asthma control: Systematic review and meta-analysis. J. Allergy Clin. Immunol. 131, 695–703. https://doi.org/10.1016/j.jaci.2012.08.023 (2013).
González Barcala, F. J. et al. Factors associated with asthma control in primary care patients: The CHAS study. Arch. Bronconeumol. 46, 358–363. https://doi.org/10.1016/j.arbres.2010.01.007 (2010).
Santos, V. et al. Association of quality of life and disease control with cigarette smoking in patients with severe asthma. Braz. J. Med. Biol. Res. 55, e11149. https://doi.org/10.1590/1414-431X2021e11149 (2022).
Hough, K. P. et al. Airway remodeling in asthma. Front. Med. (Lausanne) 7, 191. https://doi.org/10.3389/fmed.2020.00191 (2020).
Shavit, O. et al. Impact of smoking on asthma symptoms, healthcare resource use, and quality of life outcomes in adults with persistent asthma. Qual. Life Res. 16, 1555–1565. https://doi.org/10.1007/s11136-007-9267-4 (2007).
Gonzalez-Barcala, F. J. et al. Asthma exacerbations: Risk factors for hospital readmissions. Ir. J. Med. Sci. 187, 155–161. https://doi.org/10.1007/s11845-017-1633-9 (2018).
Blakey, J. D. et al. Identifying risk of future asthma attacks using UK medical record data: A respiratory effectiveness group initiative. J. Allergy Clin. Immunol. Pract. 5, 1015-1024.e1018. https://doi.org/10.1016/j.jaip.2016.11.007 (2017).
Patel, S. N. et al. Multicenter study of cigarette smoking among patients presenting to the emergency department with acute asthma. Ann. Allergy Asthma Immunol. 103, 121–127. https://doi.org/10.1016/s1081-1206(10)60164-0 (2009).
Polosa, R. et al. Greater severity of new onset asthma in allergic subjects who smoke: A 10-year longitudinal study. Respir. Res. 12, 16. https://doi.org/10.1186/1465-9921-12-16 (2011).
Polosa, R. & Thomson, N. C. Smoking and asthma: Dangerous liaisons. Eur. Respir. J. 41, 716–726. https://doi.org/10.1183/09031936.00073312 (2013).
Wilson, S. J. et al. Airway elastin is increased in severe asthma and relates to proximal wall area: Histological and computed tomography findings from the U-BIOPRED severe asthma study. Clin. Exp. Allergy 51, 296–304. https://doi.org/10.1111/cea.13813 (2021).
Tønnesen, P. et al. Effects of smoking cessation and reduction in asthmatics. Nicotine Tob. Res. 7, 139–148. https://doi.org/10.1080/14622200412331328411 (2005).
Huang, K. et al. Prevalence, risk factors, and management of asthma in China: A national cross-sectional study. Lancet 394, 407–418. https://doi.org/10.1016/s0140-6736(19)31147-x (2019).
Bennett, G. H. et al. Risk factors and clinical outcomes associated with fixed airflow obstruction in older adults with asthma. Ann. Allergy Asthma Immunol. 120, 164-168.e161. https://doi.org/10.1016/j.anai.2017.10.004 (2018).
Jabbal, S., Kuo, C. R. & Lipworth, B. Randomized controlled trial of triple versus dual inhaler therapy on small airways in smoking asthmatics. Clin. Exp. Allergy 50, 1140–1147. https://doi.org/10.1111/cea.13702 (2020).
Graff, S. et al. Clinical and biological factors associated with irreversible airway obstruction in adult asthma. Respir. Med. 175, 106202. https://doi.org/10.1016/j.rmed.2020.106202 (2020).
Chen, D. & Wu, L. T. Smoking cessation interventions for adults aged 50 or older: A systematic review and meta-analysis. Drug Alcohol Depend. 154, 14–24. https://doi.org/10.1016/j.drugalcdep.2015.06.004 (2015).
Tøttenborg, S. S., Thomsen, R. W., Johnsen, S. P., Nielsen, H. & Lange, P. Determinants of smoking cessation in patients with COPD treated in the outpatient setting. Chest 150, 554–562. https://doi.org/10.1016/j.chest.2016.05.020 (2016).
Lee, C. W. & Kahende, J. Factors associated with successful smoking cessation in the United States, 2000. Am. J. Public Health 97, 1503–1509. https://doi.org/10.2105/ajph.2005.083527 (2007).
Lou, P. et al. Supporting smoking cessation in chronic obstructive pulmonary disease with behavioral intervention: A randomized controlled trial. BMC Fam. Pract. 14, 91. https://doi.org/10.1186/1471-2296-14-91 (2013).
Kim, Y. J. Predictors for successful smoking cessation in Korean adults. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 8, 1–7. https://doi.org/10.1016/j.anr.2013.09.004 (2014).
Ben Taleb, Z. et al. Smoking cessation and changes in body mass index: Findings from the first randomized cessation trial in a low-income country setting. Nicotine Tob. Res. 19, 351–356. https://doi.org/10.1093/ntr/ntw223 (2017).
Tian, J., Venn, A., Otahal, P. & Gall, S. The association between quitting smoking and weight gain: A systematic review and meta-analysis of prospective cohort studies. Obes. Rev. 16, 883–901. https://doi.org/10.1111/obr.12304 (2015).
Brumpton, B., Langhammer, A., Romundstad, P., Chen, Y. & Mai, X. M. General and abdominal obesity and incident asthma in adults: The HUNT study. Eur. Respir. J. 41, 323–329. https://doi.org/10.1183/09031936.00012112 (2013).
Boudreau, M., Bacon, S. L., Ouellet, K., Jacob, A. & Lavoie, K. L. Mediator effect of depressive symptoms on the association between BMI and asthma control in adults. Chest 146, 348–354. https://doi.org/10.1378/chest.13-1796 (2014).
van Zelst, C. M. et al. Association between elevated serum triglycerides and asthma in patients with obesity: An explorative study. Allergy Asthma Proc. 42, e71–e76. https://doi.org/10.2500/aap.2021.42.210020 (2021).
Wang, Q., Rizzo, J. A. & Fang, H. Changes in Smoking Behaviors following Exposure to Health Shocks in China. Int. J. Environ. Res. Public Health. https://doi.org/10.3390/ijerph15122905 (2018).
Godtfredsen, N. S., Prescott, E., Osler, M. & Vestbo, J. Predictors of smoking reduction and cessation in a cohort of danish moderate and heavy smokers. Prev. Med. 33, 46–52. https://doi.org/10.1006/pmed.2001.0852 (2001).
Acknowledgements
We thank all the voluntary patients involved in the study.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81760009, No. 82170039, No. 82160009), the Natural Science Foundation of Hunan Province (No. 2020JJ4815), Qian Ke He foundation-ZK [2022] General 425, and Guilin talent mini-highland scientific research project (Municipal Committee Talent Office of Guilin City [2020] No.3-05).
Author information
Authors and Affiliations
Contributions
Conceptualization and design: Z.C., L.M., P.C., X.X.; Methodology: Z.C., Y.S., B.X., Q.Z., S.L., X.Z., L.M., P.C., X.X.; Data management: Z.C., R.O., Y.Y., Y.H., W.D., X.J., L.M., P.C., X.X.; Statistical analysis and interpretation: Z.C., B.W., J.J., Q.S., Y.Z., D.Z., L.M., P.C., X.X.; All authors contributed to drafting the original manuscript of important intellectual content and final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Z., Wasti, B., Shang, Y. et al. Different clinical characteristics of current smokers and former smokers with asthma: a cross-sectional study of adult asthma patients in China. Sci Rep 13, 1035 (2023). https://doi.org/10.1038/s41598-022-22953-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22953-z
- Springer Nature Limited