Abstract
Instable ventilatory control is an endotypic trait of obstructive sleep apnea syndrome (OSAS). This study aimed to evaluate the relationships between the anatomical compromise of the upper (oro- and naso-pharynx) and lower airways and ventilatory control (measured by chemical loop gain) in otherwise healthy children suffering from moderate to severe OSAS (apnea hypopnea index ≥ 5/hour). The children underwent ear, nose and throat examination, measurement of impedance of the respiratory system that allowed characterizing peripheral lung mechanics using the extended Resistance-Inertance-Compliance model. Physiologically constrained analytical model based on tidal breathing analysis allowed for the computation of steady-state plant gain, steady-state controller gain (CG0) and steady-state loop gain (LG0). Medium-frequency components of the feedback control system were then deduced. Fifty children (median age 11.2 years) were enrolled. Oropharyngeal obstruction was associated with decreased CG0 (0.6 [0.2; 1.0] vs 1.5 [0.5; 6.6] L.s− 1.mmHg− 1, p = 0.038) and LG0 (0.4 [0.2; 1.1] vs 1.2 [0.4; 9.3], p = 0.027), while nasal obstruction did not modify ventilatory control parameters. In a multivariate analysis Medium-Frequency PG was negatively related to minute ventilation and respiratory system compliance. Both upper (tonsil hypertrophy) and lower (compliance of respiratory system) airways are linked to ventilatory control in children with moderate to severe OSAS.
Similar content being viewed by others
Introduction
Obstructive sleep apnea syndrome (OSAS) affects 1–4% of children1 and is associated with significant cardiovascular, behavioral and neurocognitive morbidity. Instability of the control of ventilation is now increasingly recognized as a pathophysiological factor of OSAS, along with factors as anatomically compromised airways, low respiratory threshold and insufficient neuromuscular activation of pharyngeal dilators2. Nevertheless, the degree of contribution of ventilatory control abnormalities to the pathogenesis of OSAS in children remains debated3. Loop gain (LG), controller gain (CG), and plant gain (PG), which reflect the stability of ventilatory control, chemoreceptor sensitivity and the pulmonary control of blood gas in response to a change in ventilation, respectively, have been evaluated in children with OSAS. While some investigators demonstrated an increase in LG in some adult patients suffering from OSAS4, two independent groups demonstrated an increase in PG in children with OSAS while their LG was not different from that of non-OSAS children due to a reduction of CG5,6. These two groups established a positive correlation between PG and OSAS severity assessed by the apnea–hypopnea index (AHI), which suggests that high PG may play a more important role in pediatric OSAS. The mechanisms explaining this increase in PG deserve to be studied since it could lead to therapeutic approaches.
PG is related to lung function as by definition it depicts the modification of alveolar CO2 after a variation of ventilation. An abnormally elevated PG may result from reduced lung volumes, a reduced ability to eliminate CO2 adequately such as in ventilation/perfusion mismatch and decreased pulmonary blood flow7. Pulmonary function abnormalities have been associated with OSAS. In obese children, van Eyck and colleagues showed that correlations between sleep-related respiratory parameters (respiratory disturbance index, mean SaO2, SaO2 nadir) and FEV1 remained significant after correction for BMI z-score, demonstrating an independent relationship between OSAS and airflow limitation8. In the study of Zerah and colleagues9, specific respiratory conductance was linked to OSAS severity and variables that influenced this conductance were distal airway obstruction, morphological upper airway abnormalities and the AHI, highlighting the contribution of both upper and lower airways to adult OSAS. Among upper airways, both nasal and oropharyngeal obstruction can contribute to OSAS10,11.
There are also arguments for the contribution of lower and upper airway obstruction to altered ventilatory control. In children with persistent asthma with and without OSAS, the OSAS group was found to have higher PG than the non-OSAS group12. As well, the subjects with more severe OSAS and abnormal lung function had higher PG and lower CG relative to the rest of the population studied. The link between upper airway compromise and ventilatory control is important to confirm since Armoni Domany and colleagues demonstrated that six months following adenotonsillectomy, there was a significant decrease in the elevated PG in the OSAS group, while no change observed in the control group6. Thus, this study suggested that the mechanisms leading to increased PG are also secondary to upper airway abnormalities.
The objective of our study in otherwise healthy children suffering from moderate to severe OSAS was to assess the relationships between their degree of anatomical compromise of the upper (oro- and naso-pharynx) and lower airways and ventilatory control. A two-compartment lung model allowed assessing the respective contributions of central and peripheral respiratory system. We focused on this group of OSAS since there is a therapeutic indication10 and delineation of underlying endotypes deserves to be done.
Methods
Participants
Patients were included prospectively as part of our day hospital evaluation for moderate to severe OSAS. The evaluations performed during the hospitalization were: clinical examination with collection of height, weight, neck circumference, oral examination, lung function tests, ear, nose and throat (ENT) examination by an otolaryngologist (IB) together with a measurement of nasal obstruction (acoustic rhinometry) and study of ventilatory control using a recording of tidal ventilation.
The inclusion criteria were symptoms suggestive of OSAS (snoring, apnea, restless sleep, oral breathing) and an AHI ≥ 5/h in otherwise healthy children 3–18 years of age (asthma included) with or without obesity. Non-inclusion criteria were midface deficiency, marked mandibular hypoplasia, prematurity (based on a report of birth at least four weeks earlier), genetic disorders and ongoing treatment for OSAS. This study conformed to the standards set by the latest revision of the Declaration of Helsinki and was approved by the Ethics Committee of Robert Debré University Hospital (study registration identity PHENOSAS: N° 2018–416), and the database of collected data was declared to the French regulatory agency (CNIL). Informed consent was obtained from all subjects and their legal guardian(s).
All recordings were performed on the day of the ENT examination during an in-hospital stay, in the morning before the ENT examination. Recordings of tidal breathing were performed as previously described13, lasting 20 min, with the first 5 min being discarded. During the recordings, subjects were awake and sitting in a calm and non-stimulating atmosphere. Flow rate, end-tidal PO2 (PETO2) and end-tidal PCO2 (PETCO2) were continuously monitored, and signals were digitized using the MP-100 system (Biopac System Inc., Santa Barbara, CA) at a rate of 50 Hz; the data were stored for further analysis.
End-expiratory CO2 slope
The quality of the end-tidal CO2 slope is important to take into account when considering its ability to reflect alveolar CO214. We proposed a method for the calculation of a corrected expiratory slope (see Supplementary Information). This procedure permitted us to search for outliers corresponding to subjects that could have poorly performed during the tidal breathing recording.
Loop gain model
We used a constrained bivariate (minute ventilation (\({\dot{\mathrm{V}}}_{\mathrm{e}}\)) and PETCO2) analytical model that allowed us to calculate the components of CG and PG (steady-state gains, time constants of the gains and circulatory delays)13.
Briefly, the plant that describes the relationship between ventilation and alveolar PCO2 (PACO2) is modelled as a first order time delay system with a gain (called steady-state plant gain PG0) and a time constant (τp, which represents the time it takes for a PACO2 to reach 63% of its final value after a step change in ventilation).
where s denotes the frequency.
The “controller” describes the relationship between PaCO2 and ventilatory drive that equals ventilation in awake subjects. In this model, the controller is modelled using a static gain (CG0, or steady-state controller gain) and a time constant (τc). Changes in PACO2 are delayed by approximately 6 s before reaching the peripheral chemoreceptors. Delays in the time domain are modelled as exponentials in the frequency domain, hence:
where PaCO2 is the arterial PCO2 in the vicinity of the chemoreceptors and D is the delay.
Thus, this model contained only five parameters (PG0, CG0, τp, τc, and D).
By definition, PG0 should be negative and CG0 should be positive; hence, a condition of model fit failure was the observation of non-physiological gain values.
The model was fitted on the changes from baseline (mean) levels of the ventilatory parameters (\({\dot{\mathrm{V}}}_{\mathrm{e}}\) and PETCO2) that were obtained from tidal breathing measurements while awake, and thus, the analyses were specifically related to chemosensitivity. Since the medium frequency band (corresponding to oscillations of 5–15 breaths/cycle) spans the range of cycle durations of periodic breathing observed experimentally, we focused on this frequency range as was previously done13.
In-laboratory polysomnography
Polysomnography studies were performed overnight. An Alice 6 LDx polysomnography system (Philips, Murrysville, PA) recorded the following parameters: chest and abdominal wall motion using respiratory inductance plethysmography, heart rate by electrocardiogram, arterial oxygen saturation by pulse oximetry, airflow using a 3-pronged thermistor, nasal pressure by a pressure transducer, electroencephalographic leads (C3/A2, C4/A1, F3/A2, F4/A1, O1/A2, O2/A1), left and right electrooculograms, submental electromyogram, and tibial electromyogram. Study participants were also recorded with an infrared video camera. Experienced pediatric sleep physicians scored patients using standard pediatric sleep scoring criteria15. The definition of moderate to severe OSAS was sleep disorder breathing symptoms and an apnea hypopnea index (AHI) ≥ 5 episode/h10.
Pulmonary function tests
Impedance of the respiratory system was measured using an impulse oscillatory system (IOS: Master Scope Body, Carefusion Technologies, Yorba Linda, California, USA), as previously described16. We used the following IOS variables: resistance and reactance at 5, 10, 15, 20, 25, 30 and 35 Hz. Since OSAS may be an independent risk factor for small airway disease9, we used an additional lung model to characterize this small airway disease.
We used the extended Resistance-Inertance-Compliance model (eRIC) capable of accounting for significant frequency dependence of the respiratory impedance, which has previously been described16,17. In eRIC (Fig. 1A), R is partitioned into central (Rc) and peripheral (Rp) resistance of the respiratory system, while CRS is the compliance of the respiratory system (including parenchymal and conducting airways compliances). The model was fitted to the impedance data (5–35 Hz) and the minimization of a performance index allowed the calculation of model parameters, as previously done17. We used the corrected Akaike information criterion to evaluate the goodness of fit of the eRIC model on this particular data set16.
The eRIC model (A) and the impedance spectra obtained by fitting the model. Respiratory system resistance (B) and reactance (C) obtained by fitting the model (thick solid lines) to the data of the experimental measurements represented by the median values and the 25th and 75th percentiles for each frequency.
In all subjects we measured functional residual capacity (FRC) by gas dilution according to American Thoracic Society guidelines18. Z scores for FRC were computed with Cook and Herman reference equations for children19. Z-scores of IOS variables were calculated according to Gochicoa-Rangel et al.20.
ENT examination
All patients were assessed by an otolaryngologist with endoscopic nasal examination as standard care for moderate to severe OSAS clinical evaluation. Fiber endoscopy was performed with a flexible endoscope after local anesthesia using lidocaine hydrochloride 10%. Nasal obstruction was defined as obstruction from large adenoids (grade 3 or 4 according to Cassano et al.21) or turbinate hypertrophy. Oropharyngeal obstruction was defined as presence of obstructive tonsils (grade 3 or 4 according to Brodsky et al.22). The ENT specialist was blinded for the results of rhinometry.
Acoustic rhinometry
The measurements were conducted with the EccoVision Acoustic Rhinometer (E. Benson Hood Laboratories, Pembroke, MA) in the supine position after the subjects were in this position for 5 min, as previously described23. The volume of the nasopharynx was recorded and was corrected for height to obtain a normalized parameter. The calculated nasal resistance given by the apparatus (from nostril to nasopharynx) was also recorded. Nasal airway resistance was determined for each side of the nose and the total resistance was calculated using Ohm’s law equation for parallel resistors: 1/RT = 1/Rr + 1/Rl, where RT is the total nasal resistance, Rr = nasal resistance on the right side, and Rl = nasal resistance on the left side.
Statistical analysis
We decided to conduct a multivariate analysis with at most five factors, one factor per dimension explored. These factors included two anthropometric factors, namely height and the body mass index (BMI) z-score; one factor from the ENT examination; one factor from the lung function tests; and one factor from the polysomnography data. To perform a multivariate analysis with at most five factors, the sample size of OSAS cases would have to be approximately 50 subjects (10 subjects per factor).
Results were expressed as medians [25–75th percentiles]. Comparisons of continuous variables between groups were performed using the Wilcoxon test or the Kruskal–Wallis test when appropriate. Subsequent intergroup comparisons were performed using the Dunn test for multiple comparisons and p-values adjusted with the Benjamini–Hochberg method. Categorical variables were compared using the chi-square test or the Fisher exact test when appropriate. Correlations were evaluated using Pearson's correlation coefficient. Additional statistical analyses are described in the text. A P value of less than 0.05 was deemed significant. No correction for multiple testing was done due to the pathophysiological design of the study24. All statistical analyses were performed with R software version 4.1.025.
Results
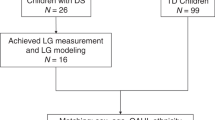
Sixty-nine children were included in this study all having an AHI ≥ 5/h. From them, 12 children did not produce exploitable tidal breathing recordings because of either insufficient cooperation or leaks/irregular breathing pattern during the recording. The population of excluded children was not different from the remaining population (Supplementary Table S1 online). Two additional children were excluded because of poor quality of the end-tidal CO2 record (Supplementary Results online).
Five additional children were removed from the data set because the analytical model of plant/controller gain produced non-physiological (negative) values for the CG0, their clinical characteristics were similar to the characteristics of the children included in the final analysis (Supplementary Table S2 online). The flow chart of the included children is summarized in Fig. 2. Thus, 50 children were included in the final analysis; their description is given in Table 1. Tables S3 and S4 in Supplementary Results (available online) show the measurements obtained from the tidal breathing analysis and the results of the pulmonary function tests and eRIC modeling respectively. Eleven had physician-diagnosed asthma and their lung function did not differ from non-asthmatic subjects (Table S4 in SupplementaryResults online). The ENT examination found nasal obstruction in 20 children, which was related to the presence of obstructive adenoids (n = 12) and/or to turbinate hypertrophy (n = 10). Twenty-two children had oropharyngeal obstruction corresponding to Brodsky grade 3 or 4. Respiratory system resistance and reactance obtained by fitting the eRIC model to the data of the experimental measurements are shown in Figs. 1B,C. The performance index and the corrected Akaike information criterion were 1.7 [0.9; 2.4] and -78 [− 86; − 73] respectively.
Effect of nasal obstruction on ventilatory control
Clinical, lung function and ventilatory control parameters of the children presenting nasal obstruction and those without are given in Table 1. As age and height were significantly different between the two groups (children with nasal obstruction were younger), we performed statistical analysis adjusted for age as an independent variable. No significant differences in ventilator control parameters were observed between the two groups (Table 1).
Effect of oropharyngeal obstruction on ventilatory control
Clinical, lung function and ventilatory control parameters of the children presenting oropharyngeal obstruction and those without are given in Table 2. We found that steady-state CG, controller characteristic time constant and stead-state LG were significantly lower in OSAS children with oropharyngeal obstruction (Table 2 and Fig. 3). Increased central resistance (Rc) was evidenced in children with oropharyngeal obstruction (p = 0.028). The analysis of the entire sample of children that had successful ENT examinations and IOS measurements (67 children) further showed that Rc in children with oropharyngeal obstruction was increased compared to those without: 0.56 kPa.s.L− 1 [0.49; 0.72] vs 0.48 [0.41; 0.61], respectively; p = 0.014. This difference remained significant after adjustment for height (padj = 0.045).
Relationship between plant gain and lung function
The correlations found between PG and lung function described by the eRIC model are given in Table 3. We found that steady-state PG decreased with increasing minute ventilation (\({\dot{\mathrm{V}}}_{\mathrm{e}}\)) and BMI z-score in both univariate (r = − 0.55, p < 0.001 and r = − 0.54, p < 0.001 respectively) and multivariate analyses (adjusted r2 = 0.36, p < 0.001).
Univariate analyses demonstrated that the plant characteristic time constant (τp) was related to FRC (r = 0.44, p = 0.001) and to the compliance of the respiratory system, CRS (r = 0.50, p < 10–3). African ethnicity was associated with faster plant time constants 3.6 s [2.7; 6.1] vs 7.5 s [4.4; 11.9] than in Caucasians, p = 0.04 (Kurskal-Wallis test), padj = 0.03. A multiple regression analysis with τp as the dependent variable and FRC, CRS and ethnicity as independent variables showed that only CRS (p = 0.026) and African ethnicity (p = 0.033) remained independent predictors of the plant characteristic time constant (adjusted r2 = 0.33, p < 0.001) in Table 3.
Medium-Frequency (MF)-PG correlated to minute ventilation (\({\dot{\mathrm{V}}}_{\mathrm{e}}\), r = − 0.67, p < 0.001), to CRS (r = − 0.41, p = 0.004) and BMI z-score (r = − 0.47, p < 0.001) but not to AHI. A multiple regression analysis with MF-PG as the dependent variable and \({\dot{\mathrm{V}}}_{\mathrm{e}}\), CRS, BMI z-score and ethnicity showed that only \({\dot{\mathrm{V}}}_{\mathrm{e}}\) (p = 0.001) and CRS (p = 0.038) remained independent predictors of MF-PG (adjusted r2 = 0.50, p < 0.001) in Table 3.
Asthma related plant gain modifications
Eleven subjects had physician-diagnosed asthma. It has been shown that in asthmatic subjects PG is related to percent predicted forced expiratory volume in first second (FEV1%) and to the FEV1/FVC ratio12. In asthmatic subjects, respiratory system compliance will be mainly influenced by bronchial muscle tone, and hence, the relationship between PG and CRS may be less significant.
We found that, MF-PG was no longer related to CRS in asthmatic subjects (Fig. 4B), while the relation between MF-PG and \({\dot{\mathrm{V}}}_{\mathrm{e}}\) remained significant (Fig. 4A). In non-asthmatic subjects, we found that MF-PG correlated to obstructive AHI (r = 0.36, p = 0.023) and to all previously described parameters (\({\dot{\mathrm{V}}}_{\mathrm{e}}\), r = − 0.66, p < 0.001, BMI z-score r = − 0.42, p = 0.008, CRS r = − 0.48, p = 0.002) in univariate analysis.
A multiple regression analysis in the subgroup of non-asthmatic subjects with MF-PG as the dependent variable and \({\dot{\mathrm{V}}}_{\mathrm{e}}\), CRS, BMI z-score and obstructive AHI showed that only \({\dot{\mathrm{V}}}_{\mathrm{e}}\) (p = 0.001) and CRS (p = 0.024) remained independent predictors of MF-PG in this subgroup (adjusted r2 = 0.52, p < 0.001).
Discussion
The most significant results of this pathophysiological study in children suffering from moderate to severe OSAS is the observation that oropharyngeal obstruction is associated with decreased steady-state CG and LG and that PG is related to pulmonary function (negative correlation with ventilation and compliance of the respiratory system).
The relationship between oropharyngeal obstruction and ventilatory control is corroborated by previous studies in children with sleep disordered breathing that reported a decrease in LG in children presenting oropharyngeal obstruction26. Here, we advance one step further in explaining this decrease by the decrease in CG. One may hypothesize that the decrease in CG is an adaptive response to the increase in the resistance of proximal airways. We evidenced an increase in Rc, corresponding to the resistance of the central airways in the eRIC model of the respiratory system in the group of children with oropharyngeal obstruction. Steady-state CG is the ratio of the increase in ventilatory drive to the increase in arterial CO2, thus a reduced controller gain would be more advantageous from a work of breathing perspective. The decrease in controller characteristic time constant is less intuitive to explain, but τc corresponds to the time during which an increase in PaCO2 will stimulate the ventilatory drive. Its modification observed in children with OSAS and with oropharyngeal obstruction could also be interpreted as an adaptive response to the increased proximal airway resistance. The fact that the steady-state CG and LG, and not only the MF-CG or MF-LG, are decreased by oropharyngeal obstruction means that the amplitude of the response of the ventilator drive after a stepwise increase in CO2 (or decrease in ventilation for loop gain) would be reduced. We did not evidence any relationship between ventilatory stability parameters and nasal obstruction. This could be explained by the obligatory mouth breathing route during sleep in subjects with nasal obstruction, shunting the nasopharynx. Thus, one may hypothesize that children with nasal obstruction may have similar modifications of ventilatory control than children with pharyngeal obstruction if these modifications are related to the route of breathing. We show that these modifications are related to the presence of oropharyngeal obstruction (Table 2), whatever the presence of nasal obstruction. Nasal obstruction inducing mouth breathing is known to increase the work of breathing in healthy subjects27. One may hypothesize that oropharyngeal obstruction will induce more work of breathing than nasal obstruction without oropharyngeal obstruction, leading to the adaptive response of ventilatory control.
We also evidenced that MF-PG decreased with increased minute ventilation and compliance of the respiratory system. The relationship with minute ventilation may seem trivial as ventilation is linked to alveolar PCO2 by the equation of alveolar ventilation28, but here we found a relationship that applies to different subjects and not to the variations of ventilation for a given subject.
Moreover, it is expected from the model of Khoo and colleagues29 (eq. S1 in Supplementary Information online) that steady-state PG (PG0) decreases with increasing alveolar ventilation and shunt fraction. We found that the two independent predictors (negatively related) of PG0 were minute ventilation (\({\dot{\mathrm{V}}}_{\mathrm{e}})\) and BMI z-score. The decrease in PG0 with BMI is surprising as some authors have suggested that the reduction of lung volumes due to obesity would produce an increase in PG7. In a previous study from our group, we found that MF-PG was decreased in obese control women compared to lean controls although this difference was not significant (0.042 mmHg.min.L− 1 [0.022; 0.070] in obese controls vs 0.076 mmHg.min.L− 1 [0.031; 0.107] in lean controls)30. On the other hand, it is well-known that obesity is associated with increased shunt fraction31 that would reduce PG. Our data suggests that obesity decreases PG by two mechanisms: via the increase in both \({\dot{\mathrm{V}}}_{\mathrm{e}}\) 32 and pulmonary shunt.
Concerning the plant characteristic time constant (τP), it is expected from eq. S2 (in Supplementary Information online) that τP scales as alveolar volume and is decreased by ventilation inhomogeneity. We found that τP increased with lung volume (FRC) and decreased with decreasing CRS, which was expected as CRS decreases with increasing ventilation inhomogeneities33. We also found that African ethnicity was associated with decreased τP, which could be explained by reduced pulmonary volume compared to Caucasian ethnicity34.
When investigating factors related to MF-PG, we found that only minute ventilation and respiratory system compliance remained independent predictors of MF-PG. Thus, the positive correlation between PG and AHI reported by two groups5,6 is possibly explained by the up-regulation of inflammatory pathways known to contribute to airway inflammation in patients with OSAS35,36. OSAS is a disorder associated with oxidative stress, up-regulation of redox-sensitive genes and inflammatory cascade35. OSAS is associated with increased prevalence of neutrophilic pattern in the sputum, thus modifying airway inflammation37. These well described pathways support the hypothesis that the inflammatory response associated with OSAS could lead to small airway inflammation and remodeling, which would reduce the compliance of the respiratory system. This relationship is lost in asthmatic patients with OSAS whose bronchial inflammation relies on other inflammatory pathways, which is associated with changes in airway remodelling38, while CRS reflects mainly the stiffness of the conducting airways and the elastance of the alveolar tissue explained by the negligible contribution of the chest wall to total respiratory system impedance in children and in the frequency range of IOS, i.e. 5-35Hz39. Thus, the normalization of plant gain after adenotonsillectomy observed by Armoni Domany and colleagues6 could be explained by the resolution of OSAS and consequent down-regulation of inflammatory pathways leading to improved peripheral lung function.
Our findings also havepotential clinical implications. We confirmed the decrease in LG in children with oropharyngeal obstruction and moderate to severe OSAS. Thus, a more stable chemical control of ventilation is expected in these children arguing against the participation of this endotypic trait in OSAS severity. Therefore, they would be less likely to respond to treatments as oxygen that reduces AHI in adult patients treated for OSAS presenting elevated LG40. LG has been identified as a predictor of treatment success of oral appliance therapy along with upper airway collapsibility in adults with OSAS41. Namely, a greater response to therapy occurred in those patients with a mild anatomic compromise and a lower LG. Oral appliances are also used to treat OSAS in children, and it has been shown to reduce the AHI by 60% in a small randomized controlled study42. Lower LG is expected in children with OSAS and oropharyngeal obstruction, increasing the chances of success of oral appliances. In this case, oral appliances could be used as a treatment option for those children not eligible for adenotonsillectomy, because of surgical contraindication or refusal of the procedure, which remains a first line therapy in children with OSAS and adenotonsillar hypertrophy10. PG was increased in children with impaired lower airway mechanics but not specifically in asthmatics, advocating in favor of an effect of OSAS per se on lung mechanics. Thus, the decrease in PG observed after adenotonsillectomy is probably secondary to the improvement of OSAS rather than a proper PG-related effect. The identification of children with residual OSAS and increased PG after adenotonsillectomy should permit clinicians to spot an endotype that could respond to targeted treatment as acetazolamide. Acetazolamide is a carbonic anhydrase inhibitor that produces metabolic acidosis, yielding an increase in baseline ventilation and hence reduces PG. Edwards et al.43 observed a 50% reduction in AHI after treatment with acetazolamide in adults with moderate to severe OSAS while the PG was reduced by 40%.
Our study has strengths. First, we used tidal breathing records during wakefulness to evaluate ventilatory control, which is the recommended technique to measure chemical loop gain44. Indeed, to evaluate chemical LG in OSAS patients, it is necessary to measure it when the upper airway is stable, for example by measuring ventilatory responses during wakefulness or while the patient is asleep on continuous positive airway pressure (CPAP). When patients with OSAS sleep, there is prevalent snoring and flow limitation that usually continue during the open phase, following an apnea, thus loop gain measurements from polysomnography-driven signals are possibly hampered by the upper airway muscles responsiveness. In snoring children, the upper airway is more stable than in snoring adults45 thus, loop gain measurements made during sleep (off CPAP) are still probably acceptable and could be compared to our results. Second, we present a unique dataset from children suffering from moderate to severe OSAS combining upper airway and lower airway assessments.
Our cross-sectional study has limitations. Only children suffering from moderate to severe OSAS were included. First, it was related to the observational design of our study; since in our center, the extensive medical check-up including nasal endoscopy is only carried out in children with a formal therapeutic indication (AHI ≥ 5/hour, moderate to severe OSAS) in accordance with European recommendations10. Second, we previously showed that PG explained only 10% of AHI variance; thus in children suffering from moderate to severe OSAS, both normal and elevated values of PG would be observed, allowing the examination of correlations with lung function indices.
In conclusion, we showed that controller and loop gains are reduced in children evaluated for moderate to severe OSAS and presenting oropharyngeal obstruction while nasal obstruction was not associated with a modification of ventilatory control parameters. Controller and loop gains are probably reduced in this population in response to the increased resistance of proximal/central airways. Impairment of lower airways by reducing the compliance of the respiratory system was associated with increased plant gain. This study provides a better understanding of the changes in ventilatory control associated with OSAS in children.
Data availability
The data that support the findings of this study are available from the corresponding author upon request. The data are not publicly available because they contain information that may compromise the privacy of the research participants.
References
Lumeng, J. C. & Chervin, R. D. Epidemiology of pediatric obstructive sleep apnea. Proc. Am. Thorac. Soc. 5, 242–252 (2008).
Eckert, D. J., White, D. P., Jordan, A. S., Malhotra, A. & Wellman, A. Defining phenotypic causes of obstructive sleep apnea identification of novel therapeutic targets. Am. J. Respir. Crit. Care Med. 188, 996–1004 (2013).
Amin, R. & Khoo, M. Loop gain in paediatric sleep-disordered breathing: A different story from adults. Respirology 25, 1119–1120 (2020).
Eckert, D. J. Phenotypic approaches to obstructive sleep apnoea—New pathways for targeted therapy. Sleep Med. Rev. 37, 45–59 (2018).
Bokov, P. et al. Cross-sectional study of loop gain abnormalities in childhood obstructive sleep apnea syndrome. Sleep Med. 69, 172–178 (2020).
Armoni Domany, K. et al. The effect of adenotonsillectomy on ventilatory control in children with obstructive sleep apnea. Sleep 42(5), zsz045 (2019).
Deacon-Diaz, N. & Malhotra, A. Inherent vs induced loop gain abnormalities in obstructive sleep apnea. Front. Neurol. 9, 896 (2018).
Van Eyck, A. et al. Sleep-disordered breathing and pulmonary function in obese children and adolescents. Sleep Med. 15, 929–933 (2014).
Zerah-Lancner, F. et al. Pulmonary function in obese snorers with or without sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 156, 522–527 (1997).
Kaditis, A. G. et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: Diagnosis and management. Eur. Respir. J. 47, 69–94 (2016).
Lofaso, F. et al. Nasal obstruction as a risk factor for sleep apnoea syndrome. Eur. Respir. J. 16, 639–643 (2000).
He, Z. et al. Phenotype of ventilatory control in children with moderate to severe persistent asthma and obstructive sleep apnea. Sleep 42(9), 130 (2019).
Bokov, P., Matrot, B., Gallego, J. & Delclaux, C. Comparison of methods of chemical loop gain measurement during tidal ventilation in awake healthy subjects. J. Appl. Physiol. 125, 1681–1692 (2018).
Gederi, E. et al. Model-based estimation of loop gain using spontaneous breathing: A validation study. Respir. Physiol. Neurobiol. 201, 84–92 (2014).
Berry, R. B. et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. J. Clin. Sleep Med. JCSM Off Publ. Am. Acad. Sleep Med. 8, 597–619 (2012).
Bokov, P. et al. Cross-sectional phenotyping of small airway dysfunction in preschool asthma using the impulse oscillometry system. J. Asthma 58, 573–585 (2021).
Bokov, P., Jallouli-Masmoudi, D., Amat, F., Houdouin, V. & Delclaux, C. Small airway dysfunction is an independent dimension of wheezing disease in preschool children. Pediatr. Allergy Immunol. 33, e13647 (2022).
Wanger, J. et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 26, 511–522 (2005).
Cook, C. D. & Hamann, J. F. Relation of lung volumes to height in healthy persons between the ages of 5 and 38 years. J. Pediatr. 59, 710–714 (1961).
Gochicoa-Rangel, L. et al. Values of Impulse oscillometry in healthy mexican children and adolescents. Respir. Care 60, 119–127 (2015).
Cassano, P., Gelardi, M., Cassano, M., Fiorella, M. L. & Fiorella, R. Adenoid tissue rhinopharyngeal obstruction grading based on fiberendoscopic findings: A novel approach to therapeutic management. Int. J. Pediatr. Otorhinolaryngol. 67, 1303–1309 (2003).
Brodsky, L. Modern assessment of tonsils and adenoids. Pediatr. Clin. North Am. 36, 1551–1569 (1989).
Bokov, P. et al. The utility of acoustic pharyngometry and rhinometry in pediatric obstructive sleep apnea syndrome. Sleep Med. 58, 75–81 (2019).
Rothman, K. J. No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46 (1990).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2021).
Siriwardhana, L. S. et al. Role of ventilatory control instability in children with sleep-disordered breathing. Respirol. Carlton Vic. 25, 1174–1182 (2020).
Fitzpatrick, M. F. et al. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur. Respir. J. 22, 827–832 (2003).
West, J. B. & Luks, A. M. West’s Respiratory Physiology: The Essentials, 11e. (2021).
Khoo, M. C. K., Hu, W.-H. & Amin, R. Effects of Ventilation-Perfusion Mismatch on Severity of Obstructive Sleep Apnea: A Modeling Study. In 2020 42nd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) 2792–2795 (2020). doi:https://doi.org/10.1109/EMBC44109.2020.9175297.
Bokov, P., Essalhi, M. & Delclaux, C. Loop gain in severely obese women with obstructive sleep apnoea. Respir. Physiol. Neurobiol. 221, 49–53 (2016).
Hedenstierna, G. et al. Oxygenation impairment during anesthesiainfluence of age and body weight. Anesthesiology 131, 46–57 (2019).
Chlif, M., Keochkerian, D., Choquet, D., Vaidie, A. & Ahmaidi, S. Effects of obesity on breathing pattern, ventilatory neural drive and mechanics. Respir. Physiol. Neurobiol. 168, 198–202 (2009).
Lutchen, K. R., Greenstein, J. L. & Suki, B. How inhomogeneities and airway walls affect frequency dependence and separation of airway and tissue properties. J. Appl. Physiol. 80, 1696–1707 (1996).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 40, 1324–1343 (2012).
Ryan, S., Taylor, C. T. & McNicholas, W. T. Predictors of elevated Nuclear Factor-κB–dependent genes in obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 174, 824–830 (2006).
Israel, L. P., Benharoch, D., Gopas, J. & Goldbart, A. D. A pro-inflammatory role for nuclear factor kappa B in childhood obstructive sleep apnea syndrome. Sleep 36, 1947–1955 (2013).
Teodorescu, M. et al. Obstructive sleep apnea risk, asthma burden, and lower airway inflammation in adults in the severe asthma research program (SARP) II. J. Allergy Clin. Immunol. Pract. 3, 566-575.e1 (2015).
Taillé, C. et al. Obstructive sleep apnoea modulates airway inflammation and remodelling in severe asthma. PLoS ONE 11, e0150042 (2016).
King, G. G. et al. Technical standards for respiratory oscillometry. Eur. Respir. J. 55, (2020).
Wellman, A. et al. Effect of oxygen in obstructive sleep apnea: Role of loop gain. Respir. Physiol. Neurobiol. 162, 144–151 (2008).
Edwards, B. A. et al. Upper-airway collapsibility and loop gain predict the response to oral appliance therapy in patients with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 194, 1413–1422 (2016).
Villa, M. P. et al. Randomized controlled study of an oral jaw-positioning appliance for the treatment of obstructive sleep apnea in children with malocclusion. Am. J. Respir. Crit. Care Med. 165, 123–127 (2002).
Edwards, B. A. et al. Acetazolamide improves loop gain but not the other physiological traits causing obstructive sleep apnoea. J. Physiol. 590, 1199–1211 (2012).
Younes, M. CrossTalk proposal: Elevated loop gain is a consequence of obstructive sleep apnoea. J. Physiol. 592, 2899–2901 (2014).
Marcus, C. L. et al. Upper airway collapsibility in children with obstructive sleep apnea syndrome. J. Appl. Physiol. 77, 918–924 (1994).
Author information
Authors and Affiliations
Contributions
P.B. conceived and designed the research; P.B., I.B. and C.D2. performed measurements; P.B. and C.D2. analyzed data; all authors interpreted results of the experiments; P.B. prepared the figures; P.B. and C.D2. drafted the manuscript; all authors edited and revised the manuscript; all authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bokov, P., Boujemla, I., Matrot, B. et al. Oropharyngeal obstruction and respiratory system compliance are linked to ventilatory control parameters in pediatric obstructive sleep apnea syndrome. Sci Rep 12, 17340 (2022). https://doi.org/10.1038/s41598-022-22236-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22236-7
- Springer Nature Limited