Abstract
To investigate the effect of both prostate volume and serum testosterone changes on lower urinary tract symptoms in patients with prostate cancer undergoing androgen deprivation therapy. A total of 167 patients who received androgen deprivation therapy for prostate cancer treatment from January 2010 to August 2020 were enrolled in this retrospective study. Changes in the International Prostate Symptom Score (IPSS) in the patient groups stratified by prostate volume and the amount of testosterone reduction were assessed every 4 weeks until 12 weeks after androgen deprivation therapy initiation. Longitudinal mixed models were used to assess the adjusted effects of prostate volume and testosterone reduction on IPSS change. All mean values of IPSS-total score (IPSS-total), voiding subscore (IPSS-vs), and storage subscore (IPSS-ss) significantly decreased from baseline to week 12 in both patients with small (< 33 mL) and large (≥ 33 mL) prostates. The mean values of IPSS-total, IPSS-vs, and IPSS-ss similarly decreased in patients with large prostate with a baseline IPSS-total of ≥ 13. However, in those with small prostate, IPSS-ss specifically remained unchanged, while IPSS-total and IPSS-vs significantly decreased. In addition, only in patients with small prostate (< 33 mL), patients with lesser testosterone reduction (< Δ400 ng/dL) showed greater improvement in IPSS-ss by 7.5% compared with those with greater testosterone reduction (≥ Δ400 ng/dL). In conclusion, although androgen deprivation therapy generally improves lower urinary tract symptoms, it may worsen specifically storage symptoms in patients with relatively small prostate and greater testosterone reduction. Our finding suggests that testosterone may influence lower urinary tract symptoms in these patients.
Similar content being viewed by others
Introduction
Lower urinary tract symptoms (LUTS) usually do not appear until the tumor has grown to compress or invade adjacent structures (e.g., the prostatic urethra, urinary bladder, or neurovascular bundles) because the majority of prostate cancer (PCa) arises in the peripheral zone of the prostate1,2. However, patients with early PCa may also develop LUTS, as the prevalence of benign prostatic hyperplasia increases with age, as does those of PCa. Overall, almost 45% of patients with PCa suffer from moderate to severe LUTS3,4,5.
In recent years, there have been reports that ADT performed as neoadjuvant therapy before radiation therapy or brachytherapy may significantly reduce prostate volume (PV)6,7. Thus, the relationship between ADT and LUTS relief has been extensively studied because ADT reduces prostate size. Reports exist on cases in which patients with PCa who experienced acute urinary retention were able to regain the ability to void after ADT8. On the other hand, the association between ADT and LUTS may be due not only to ADT reducing the PV but also due to changes in circulating testosterone. A previous study found that low testosterone levels in patients with bladder outlet obstruction negatively correlated with detrusor pressure while enhancing detrusor overactivity9. Thus, sex steroids in the genitourinary tract not only regulate the development and function of sex organs but may also influence lower urinary tract function10. Both epidemiological and experimental studies have revealed a link may exist between testosterone and volume threshold for inducing micturition11,12. However, previous and current studies have solely focused on the correlation between PV reduction and LUTS improvement in patients with PCa undergoing ADT, although testosterone may affect micturition.
Therefore, in this study evaluated the combined effect of PV and testosterone reduction on LUTS in patients with PCa undergoing ADT by analyzing the International Prostate Symptom Score (IPSS) changes stratified by the amount of both PV and serum testosterone reduction.
Results
Baseline characteristics
Patient baseline characteristics were generally similar between the groups stratified by PV. However, patients with large prostate (≥ 33 mL) demonstrated a higher mean IPSS-total score (IPSS-total) and IPSS voiding subscore (IPSS-vs) (all p < 0.050) compared with those with a relatively small prostate (< 33 mL), whereas the difference was not significant regarding IPSS storage subscore (IPSS-ss) (p = 0.078). Smaller FBC and lower Qmax were also noted in patients with large prostate when compared with those of small prostate (182.35 ± 74.31 vs 303.46 ± 122.78, p = 0.023 and 8.98 ± 2.88 vs. 17.92 ± 6.11, p < 0.001, respectively). Patient characteristics according to PV are shown in Table 1.
IPSS changes according to PV
A significantly higher proportion of patients showing clinically meaningful LUTS relief (responders) were noted in patients with large prostate compared with small prostate after 8 weeks. This trend continued until week 12 (40.7% vs. 30.9%, p = 0.021 and 43.0% vs. 34.6%, p = 0.036, respectively, Fig. 1).
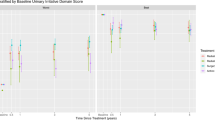
All mean values of IPSS-total, IPSS-vs, and IPSS-ss significantly decreased from baseline to week 12 in both patients with small (r = − 0.563, − 0.485, and − 0.232, all p < 0.050, respectively) and large (r = − 0.759, − 0.626, and − 0.357, all p < 0.050, respectively) prostates. Focusing on patients with a baseline IPSS-total of ≥ 13 (a commonly used threshold in studies on the management of LUTS), IPSS-total, IPSS-vs, and IPSS-ss similarly significantly decreased in patients with large prostate (r = − 0.861, − 0.724, and − 0.398, all p < 0.050, respectively, Fig. 2A–C). However, although the decreasing trend of IPSS-total and IPSS-vs (r = − 0.684 and − 0.537, all p < 0.050, respectively, Fig. 2A,B) was similar with those in patients with large prostate, IPSS-ss remained virtually unchanged from baseline to week 12 (r = − 0.190, p = 0.179, Fig. 2C) in patients with small prostate. No significant change was noted in the quality of life (QoL) score throughout the 12-week period both in patients with large and small prostate (Fig. 2D).
Mean (± standard error) changes in the International Prostate Symptom Score (IPSS) from baseline to 12 weeks after androgen deprivation therapy in patients with baseline IPSS of ≥ 13, stratified by prostate volume (mL). (A) IPSS total score; (B) IPSS voiding score; (C) IPSS storage score; (D) IPSS quality of life score.
Significance of testosterone reduction on IPSS change
Focusing on the patients with a baseline IPSS-total of ≥ 13, no difference exists in the total patients and those with large prostate in the magnitude of changes in all four IPSS categories after 12 weeks of ADT (IPSS-total, IPSS-vs, IPSS-ss, and QoL score; all p > 0.050) between patient groups stratified by the amount of serum testosterone reduction from baseline to week 12 (Δ serum testosterone, < Δ400 vs. ≥ Δ400 ng/dL, Table 2). However, no significant differences exist in changes in IPSS-total, IPSS-vs, and QoL score in patients with small prostate, whereas a greater decrease was noted in IPSS-ss in the group with smaller testosterone reduction (p = 0.037, Table 2). In patients with serum testosterone reduction of ≥ Δ400 ng/dL, a 0.08 ± 0.46 increase was noted in the mean IPSS-ss value in 12 weeks after ADT.
Adjusted effect of PV and serum testosterone on IPSS
Adjusted and unadjusted longitudinal models demonstrated modest, positive effects of PV on LUTS improvement with a 9.5% greater IPSS-total and 12.5% greater IPSS-vs decrease (p = 0.026 and p = 0.003, respectively) in patients with large (≥ 33 mL) prostates compared with those with small (< 33 mL) prostates over time (Table 3). No significant effects of PV on IPSS-ss and QoL score improvement were noted (all p > 0.050, Table 3). In longitudinal mixed models specifically performed in patients with PV of < 33 mL (n = 81), patients with lesser serum testosterone reduction (< Δ400 ng/dL) showed 7.5% greater IPSS-ss improvement (p = 0.038, Table 3) compared with those with greater serum testosterone reduction (≥ 400 ng/dL) over time. However, there is no significant effect of serum testosterone reduction on IPSS-total, IPSS-vs, and QoL score (all p > 0.050, Table 3).
Discussion
The data in this study demonstrated that more patients showed clinically meaningful LUTS relief after 12 weeks of ADT in patients with large prostate (PV ≥ 33 mL) compared with small (PV < 33 mL) prostate (40.7% vs. 30.9%, respectively). Moreover, the improvement of IPSS-total and IPSS-vs was more prominent in patients with large prostate compared with those with small prostate (r = − 0.861 vs. − 0.684 and r = − 0.724 vs. − 0.537, respectively) after excluding patients with mild LUTS (IPSS 0–7) who were not candidates for medical intervention. Previous studies have also shown the consisting findings that PV decreased from 18 to 41% when ADT was administered for 3–8 months, theoretically suggesting that ADT can improve LUTS13. Moreover, baseline PV before ADT initiation positively correlated with percent volume reduction during ADT14, suggesting that patients with larger prostate may experience more PV reduction and thus improved LUTS.
In the previous studies, the relationship between testosterone and LUTS often disappeared after statistical adjustment for age15, indicating that testosterone may not be the primary cause of the anatomical and functional change in the urinary tract. Nevertheless, numerous studies focused on the interrelation between circulating testosterone levels and LUTS at the molecular level by discovering a large extent of androgen receptors at the urethra and bladder16. The role of testosterone and its metabolites on neuromuscular transmission was also noted in rat isolated urinary bladder17. In addition, testosterone exerts its ability by manipulating nitric oxide, which acts as a nonadrenergic-noncholinergic neurotransmitter in the urogenital tract18. The positive effects of testosterone, i.e., increased bladder capacity and compliance and decreased detrusor pressure, on urinary symptoms were observed in a clinical study19,20. The higher serum levels of testosterone generated by testosterone supplementation were associated with reduced IPSS, probably indicating a correlation between serum testosterone level and their effects on LUTS21. Especially, lower IPSS-ss were reported in patients with testosterone supplementation than control by a more recent study based on a large registry data22,23. In the same context, an Asian study that investigated the relationship between male overactive bladder (OAB) symptoms and androgen deprivation revealed that ADT in patients with PCa was associated with an increased risk of OAB that was ADT duration-dependent23. Taken together, considering that the changes in both PV and testosterone during ADT can affect LUTS, analyzing that the combined effect of the two may provide relevant suggestions to enlighten the actual cause of changes in LUTS in patients with PCa undergoing ADT.
Unlike previous studies that solely focused on the association between prostate size and LUTS improvement in patients with PCa undergoing ADT, the present study primarily aims to determine the effect of both baseline PV and serum testosterone reduction after ADT on LUTS changes over 12 weeks. Consistent with previous reports, more significantly reduced scores were observed in IPSS-total and IPSS-vs in patients with large prostate compared with those with small prostate. However, as for IPSS-ss, the score reduction was not significant specifically in patients with small prostate suggesting that storage symptom during ADT does not share the mechanism of voiding symptom improvement, which is due to the PV reduction. This point focused on the role of testosterone on LUTS, particularly storage symptoms. Thus, these results that analyzed the effect of testosterone on IPSS changes revealed that the decreased amount of testosterone and those of IPSS-ss were inversely correlated. In patients with baseline IPSS ≥ 13, PV < 33 mL, and a decrease in testosterone above 400 ng/dL after 12 weeks of ADT, IPSS-ss was rather increased by 0.08 ± 0.46 (Table 2), indicating that patients with small prostate and greater testosterone reduction are likely to experience storage symptoms to be not improved during ADT, compare to those with small prostate and lesser testosterone reduction. Although voiding symptoms are expected to be improved during ADT due to PV reduction effect, storage symptoms are reckoned to be the opposite due to the reduction effect of testosterone. Furthermore, serum testosterone reduction by ADT maintained its effect on storage symptoms after adjusting PV along with other covariates (e.g., age at ADT initiation, BMI, tumor characteristics, and LHRH agonist type). In this study, the relationship between testosterone and LUTS, which was not clearly shown in previous studies, was observed probably due to the methodology of subclassifying patients more specifically (e.g., prostate size, baseline IPSS, and amount of testosterone reduction after ADT).
This study should mention the following limitation. Although IPSS reduction was noted, the concomitant PV reduction was not confirmed as follow up PV measurement was not performed in this study. Therefore, the proportion of the improvement of symptoms was not confirmed as the size decreases. In addition, urodynamic parameters corresponding to IPSS measurements were not repeatedly checked, which may have made it possible to more specifically analyze the pattern of IPSS changes. Additionally, the results of serum testosterone levels measurement may not be consistent from patient to patient because it can vary depending on the time of measurement during a day. However, this study tried to keep the measurement time as constant as possible by limiting the time from 9:00 am and noon. The absence of a control group is another drawback in this analysis.
In conclusions, LUTS generally improves in patients with PCa undergoing ADT. However, in patients with clinically meaningful symptoms (IPSS-total ≥ 13), storage symptom did not improve significantly in those with small prostate (< 33 mL). Storage symptoms even worsened in patients with both small prostate and greatest testosterone reduction (> 470 ng/dL). Taken together, both PV and testosterone change during ADT can influence LUTS. In particular, changes in testosterone can specifically affect the storage symptoms.
Methods
Study overview and inclusion/exclusion criteria
The present study protocol was reviewed and approved by the Institutional Review Board of Hallym University Sacred Heart Hospital (approval No. 2020-12-012). All research was performed in accordance with relevant guidelines and regulations, including the Declaration of Helsinki. A waiver of informed consent was granted due to the retrospective nature of this study. A total of 167 patients with locally advanced or metastatic PCa, with an estimated life expectancy of at least 12 months, and undergoing ADT for > 3 months from January 2010 to August 2020 were included for evaluation. All patients received one of three luteinizing hormone-releasing hormone (LHRH) agonists (goserelin acetate, 11.34 mg; triptorelin acetate, 11.25 mg; or leuprolide acetate, 11.25 mg) subcutaneously injected into the abdominal wall, and oral bicalutamide (50 mg) was administered daily. None of the included patients underwent bilateral orchiectomy as a form of ADT. The exclusion criteria were shown in Table 4. Especially, those with inappropriate data (those with missing IPSS records at 4, 8, 12 weeks, serum testosterone values at 4, 12 weeks) and significant pyuria suggesting recent urinary tract infection were excluded.
Baseline parameters
The baseline parameters of patients, including age at ADT initiation, body mass index (BMI), prostate-specific antigen, cancer characteristics (Gleason score and TNM stage), pre-ADT IPSS, functional bladder capacity (FBC), maximal uroflow rate (Qmax), and postvoid residual urine volume (measured by diagnostic ultrasound), were evaluated. Serum testosterone was measured between 9:00 am and noon. PV was measured by transrectal ultrasonography, following the previously mentioned protocol24.
Outcome measurements
The IPSS questionnaire was obtained from the patients before ADT at baseline and at 4, 8, and 12 weeks after ADT initiation to assess the severity of LUTS and its changes during ADT. Serum testosterone was also rechecked at 12 weeks after ADT start. The number and proportion (in percentage) of patients showing clinically meaningful LUTS relief (responder), which was defined as an IPSS-total score reduction of at least three points were evaluated according to PV13. IPSS was classified into four categories and analyzed respectively: IPSS-total, IPSS-vs, IPSS-ss, and QoL score. IPSS change was especially examined for patients with a baseline IPSS-total of ≥ 13. In addition, outcome measurements stratified by the amount of testosterone reduction from baseline and baseline PV were performed to specifically investigate the impact of testosterone and PV on LUTS relief in patients undergoing ADT. The median value of 33 mL for PV was used to categorize the patients for the comparison. Testosterone reduction value of Δ400 ng/dL for patient categorization was also used for the same reason.
Statistical analysis
The differences in continuous and categorical variables between the groups stratified by PV were analyzed using the independent t-test and chi-square test, respectively. The significance of changing trends of IPSS values was confirmed by calculating the Pearson’s correlation coefficient and using ordered logistic regression. IPSS changes from baseline were also analyzed by analysis of covariance. IPSS parameter changes during ADT by PV and serum testosterone accounting for repeated, correlated observations in the same patient throughout the study period were evaluated using longitudinal mixed-model analyses. The recorded IPSS values were log-transformed for comparison. Multivariable modeling was utilized using recorded baseline covariates to control for potential confounders. All covariates were inserted into single multivariable models, which predict each outcome, and those with a p ≤ 0.2 in each model were included as final covariates for the full-adjusted model. All statistical analyses were performed using the SAS® Software 9.3 (SAS Institute, Cary, NC, USA), and a p-value of < 0.050 was considered to indicate statistical significance.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Hamilton, W. & Sharp, D. Symptomatic diagnosis of prostate cancer in primary care: A structured review. Br. J. Gen. Pract. 54, 617–621 (2004).
Guess, H. A. Benign prostatic hyperplasia and prostate cancer. Epidemiol. Rev. 23, 152–158 (2001).
Lehrer, S., Stone, N. N., Droller, M. J. & Stock, R. G. Association between American Urologic Association (AUA) urinary symptom score and disease stage in men with localized prostate cancer. Urol. Oncol. 7, 73–76 (2002).
Andersson, S. O., Rashidkhani, B., Karlberg, L., Wolk, A. & Johansson, J. E. Prevalence of lower urinary tract symptoms in men aged 45–79 years: A population-based study of 40 000 Swedish men. BJU Int. 94, 327–331 (2004).
Royce, P. L., Ooi, J. J. Y., Sothilingam, S. & Yao, H. H. Survival and quality of life ourcomes of high-intensity focused ultrasound treatment of localized prostate cancer. Prostate Int. 8, 85–90 (2020).
Kucway, R. et al. Prostate volume reduction with androgen deprivation therapy before interstitial brachytherapy. J. Urol. 167, 2443–2447 (2002).
Langenhuijsen, J. F. et al. Neoadjuvant androgen deprivation for prostate volume reduction: The optimal duration in prostate cancer radiotherapy. Urol. Oncol. 29, 52–57 (2011).
Mommsen, S. & Petersen, L. Transurethral catheter removal after bilateral orchiectomy for prostatic carcinoma associated with acute urinary retention. Scand. J. Urol. Nephrol. 28, 401–404 (1994).
Koritsiadis, G. et al. Androgens and bladder outlet obstruction: A correlation with pressure-flow variables in a preliminary study. BJU Int. 101, 1542–1546 (2008).
Badawi, J. K., Bosch, R., Djurhuus, J. C. & Hanna-Mitchell, A. T. Is testosterone important in LUT function in men and women? ICI-RS 2015. Neurourol. Urodyn. 36, 859–862 (2017).
Coyne, K. S. et al. The prevalence of lower urinary tract symptoms (LUTS) and overactive bladder (OAB) by racial/ethnic group and age: Results from OAB-POLL. Neurourol. Urodyn. 32, 230–237 (2013).
Cheng, C. L. & de Groat, W. C. Effect of orchiectomy and testosterone replacement on lower urinary tract function in anesthetized rats. Am. J. Physiol. Renal Physiol. 311, F864–F870 (2016).
Barry, M. J. et al. Benign prostatic hyperplasia specific health status measures in clinical research: How much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J. Urol. 154, 1770–1774 (1995).
Whittington, R. et al. The effect of androgen deprivation on the early changes in prostate volume following transperineal ultrasound guided interstitial therapy for localized carcinoma of the prostate. Int. J. Radiat. Oncol. Biol. Phys. 44, 1107–1110 (1999).
Litman, H. J., Bhasin, S., O’Leary, M. P., Link, C. L. & McKinlay, J. B. An investigation of the relationship between sex-steroid levels and urological symptoms: Results from the Boston Area Community Health survey. BJU Int. 100, 321–326 (2007).
Rosenzweig, B. A. et al. Location and concentration of estrogen, progesterone, and androgen receptors in the bladder and urethra of the rabbit. Neurourol. Urodyn. 14, 87–96 (1995).
Hall, R., Andrews, P. L. & Hoyle, C. H. Effects of testosterone on neuromuscular transmission in rat isolated urinary bladder. Eur. J. Pharmacol. 449, 301–309 (2002).
Filippi, S. et al. Characterization and functional role of androgen-dependent PDE5 activity in the bladder. Endocrinology 148, 1019–1029 (2007).
Yassin, A. A., El-Sakka, A. I., Saad, F. & Gooren, L. J. Lower urinary-tract symptoms and testosterone in elderly men. World J. Urol. 26, 359–364 (2008).
Shigehara, K., Izumi, K., Mizokami, A. & Namiki, M. Testosterone deficiency and nocturia: A reviw. World J. Mens Health 35, 14–21 (2017).
Saad, F., Gooren, L. J., Haider, A. & Yassin, A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J. Androl. 29, 102–105 (2008).
Debruyne, F. M. et al. Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: Prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int. 119, 216–224 (2017).
Li, J. R., Wang, S. S., Lin, C. H., De Groat, W. C. & Cheng, C. L. Positive association of male overactive bladder symptoms and androgen deprivation: A Nationwide Population-based Cohort Study. Anticancer Res. 39, 305–311 (2019).
Choi, H. et al. Analysis of initial baseline clinical parameters and treatment strategy associated with medication failure in the treatment of benign prostatic hyperplasia in Korea. Int. Neurourol. J. 14, 261–266 (2010).
Funding
This research was supported by Hallym University Research Fund 2020 (HURF-2020-10).
Author information
Authors and Affiliations
Contributions
W.J.B., acquisition, analysis, or interpretation of data, manuscript draft; H.K., acquisition of data; C.Y.O., acquisition of data; J.K.J., acquisition of data; J.S.C., acquisition of data; M.S., conception or design of the work, acquisition, analysis, or interpretation of data, revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bang, W.J., Kim, H., Oh, C.Y. et al. Clinical significance of prostate volume and testosterone reduction on lower urinary tract symptoms in patients with prostate cancer undergoing androgen deprivation therapy. Sci Rep 12, 18535 (2022). https://doi.org/10.1038/s41598-022-21963-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21963-1
- Springer Nature Limited