Abstract
Higher plasma leucine, isoleucine and valine (BCAA) concentrations are associated with diabetes, obesity and insulin resistance (IR). Here, we evaluated the effects of 6-weeks very-low calorie diet (VLCD) upon fasting BCAA in overweight (OW) non-diabetic men, to explore associations between circulating BCAA and IR, before and after a weight loss intervention. Fasting plasma BCAAs were quantified in an OW (n = 26; BMI 32.4 ± 3 kg/m2; mean age 44 ± 9 y) and a normal-weight (NW) group (n = 26; BMI 24 ± 3.1 kg/m2; mean age 32 ± 12.3 y). Ten of the OW group (BMI 32.2 ± 4 kg/m2; 46 ± 8 y) then underwent 6-weeks of VLCD (600–800 kcal/day). Fasting plasma BCAA (gas chromatography-mass spectrometry), insulin sensitivity (HOMA-IR) and body-composition (DXA) were assessed before and after VLCD. Total BCAA were higher in OW individuals (sum leucine/isoleucine/valine: 457 ± 85 µM) compared to NW control individuals (365 ± 78 µM, p < 0.001). Despite significant weight loss (baseline 103.9 ± 12.3 to 93 ± 9.6 kg and BMI 32.2 ± 4 to 28.9 ± 3.6 kg/m2), no changes were observed in BCAAs after 6-weeks of VLCD. Moreover, although VLCD resulted in a significant reduction in HOMA-IR (baseline 1.19 ± 0.62 to 0.51 ± 0.21 post-VLCD; p < 0.001), Pearson’s r revealed no relationships between BCAA and HOMA-IR, either before (leucine R2: 2.49e−005, p = 0.98; isoleucine R2: 1.211−e006, p = 0.9; valine R2: 0.004, p = 0.85) or after VLCD (leucine R2: 0.003, p = 0.86; isoleucine R2: 0.006, p = 0.82; valine R2: 0.002, p = 0.65). Plasma BCAA are higher in OW compared to NW individuals. However, while 6-weeks VLCD reduced body weight and IR in OW individuals, this was not associated with reductions in BCAA. This suggests that studies demonstrating links between BCAA and insulin resistance in OW individuals, are complex and are not normalised by simply losing weight.
Similar content being viewed by others
Introduction
The global prevalence of obesity (BMI of ≥ 30 kg/m2) has reached epidemic proportions and is predicted to rise from 33% in 2005 to ~ 58% by 20301. Obesity is a central feature of insulin resistance (IR), a major risk factor for developing type 2 diabetes (T2DM;2,3), whilst also being associated with adverse outcomes to multiple co-morbidities, including COVID-193. Thus, novel insights into the pathophysiology of IR, and effective treatments are needed.
Branched-chain amino acids (BCAA) are diet-derived nutrients, which are established regulators of skeletal muscle proteostasis that act as critical anabolic signals [and substrates] positively regulating muscle and whole-body protein synthesis4,5. Yet, excess circulating BCAA, and their keto-acid by-products6,7, have been associated with adverse metabolic health; for example several studies have shown that dietary BCAA restriction8 and pharmacological reduction of plasma BCAAs9 can improve insulin sensitivity (IS). Over decades, studies have consistently shown that higher blood concentrations of BCAAs are common diagnostic and prognostic features for IR and risks of T2DM, with historical10, and more recent data11,12, proposing BCAA to be a root-cause of IR and dysglycaemia across liver, skeletal muscle and adipose tissue sites indepedent of BMI13,14. The proposed mechanisms by which BCAAs induce insulin resistance centre upon two themes: (1) that excess dietary BCAAs lead to sustained activation of mTORC1 (of which, leucine is a trigger15) via serine phosphorylation of insulin receptor substrate (IRS-1) and IRS-2, and that (2) impaired BCAA metabolism results in accumulation of BCAA-metabolic intermediates which suppress insulin action resulting in lipid accumulation11. Some studies have also shown reduced skeletal muscle expression of genes involved in BCAA metabolism in those with T2DM16, whilst others have shown that insulin-resistant rats demonstrate reduced capacity for BCAA catabolism17. Finally, work from our lab18 has shown that treating murine C2C12 myoblasts with sodium phenylbutyrate (PB), which induces BCAA catabolism, reduces BCAA and branched-chain keto-acid (BCKA) concentrations, impaires IRS-1 signaling with concomitant increases in phosphorylation of protein kinase B (AKT). In sum, multiple lines of evidence point to dysregulated BCAA metabolism in insulin resistant states.
However, a general limitation of this research area is a lack of “cause-effect” relationships between higher BCAA and IR in overweight humans (OW)—an aspect which could be addressed in longitudinal weight loss studies tracking BCAA abundance. Of all means to induce weight loss, non-pharmaceutical approaches remain an important first step in the management of obesity and diabetes. Specifically, very low-calorie diets (VLCD) represent a safe and effective means to reduce IR with short-term (~ 8 week) VLCD being sufficient to normalise hepatic IR, improve β-cell function in individuals with T2DM19 and induce remission of T2DM20, whilst also proving efficacious in obese21 and adolescent populations22. The aim of this study was to investigate relationships between fasting plasma BCAA/BCKA and insulin sensitivity (IS) following 6-weeks of VLCD in OW men. We hypothesised that BCAA would be higher in our obese volunteers, and that ensuing weight loss and reductions in IR would be associated with a normalisation of BCAA, that would further be associated with improved IS.
Research design and methods
Ethical approval
This study was approved by the University of Nottingham Faculty of Medicine Ethics Committee (D/2/2006-B12092016) and complied with the 2013 Declaration of Helsinki. Informed consent was obtained from all participants prior to enrolment onto the study.
Participant characteristics
To confirm that OW individuals have increased fasting plasma BCAA concentrations, we undertook baseline measurements of OW men (n = 26, 44 ± 9 y, BMI 32.4 ± 3 kg/m2) and NW individuals (n = 26 {8 female: 18 male} , 32 ± 12.3 y, BMI 24 ± 3.1 kg/m2). The samples from the latter cohort were obtained from participants in a previously published study from our laboratory23. Of the twenty-six OW individuals, n = 10, middle-aged men (45.9 ± 8.3 y, BMI 32.2 ± 4 kg/m2) of mixed ethnic backgrounds underwent 6-weeks VLCD. Volunteers with diabetes, hypertension, respiratory or cardiovascular disorders were excluded. Individuals were not taking any prescribed medications. Before enrolment, participants were screened by a medical questionnaire and physical examination (resting 12-lead ECG, clinical blood chemistry).
Study procedures
On study days, volunteers reported to our laboratory at ~ 09:00 h fasted (except water) from midnight. Body composition was determined by dual-energy X-ray absorptiometry (DXA; Lunar Prodigy II, GE Medical Systems) with body regions auto-processed (Encore software, GE Healthcare). Fasting blood samples were collected from the antecubital vein into lithium-heparin (for plasma) or fluoride oxalate (for glucose) vacutainers, before centrifugation at 3500 rpm, at 4 °C for 20 minutes, wherein the plasma was then rapidly frozen and stored at − 80 °C.
Dietary management
VLCD study participants (n = 10), were instructed to maintain their usual levels of physical activity and prescribed a meal replacement diet designed to aid in weight management (Lighter Life, Harlow, Essex, U.K). This consisted of 4 meals per day, providing ~ 600 kcal/day, with an allowance for an extra 200 kcal/day in the form of fruit, vegetables or meat. The meals provided approximately 50 g protein, 50 g carbohydrate and 17.3 g fat, complete with 100% RDA of vitamins and minerals.
Analytical methods
To determine plasma BCAA and BCKA concentrations, samples were spiked with internal standards (Norleucine and α-Ketovaleric acid) and prepared according to our routine methods15. Briefly, plasma proteins were precipitated in 100% ice-cold ethanol, then pelleted by centrifugation at 10,000 rpm for 3 min at 4 °C; the supernatant was dried under N2 at 90 °C in a Techne Dri-Block. The Quinoxalinol derivative of the BCKA and KVA (internal standard) were prepared using acidified 0.15% ortho-phenylenediamine (OPD) in 1.3 M HCl, at 90 °C for 60 min, then allowed to cool. Lipids and the BCKA-quinoxalinol derivatives were removed by extraction into ethyl acetate. The ethyl acetate layer and the remaining aqueous layer (containing the BCAA), were dried down separately and the N-tert-butyldimethyl-silyl-N-methyl-trifluoracetamide (MTBSTFA) derivatives of each fraction (BCKA and KCAA) were prepared, and their concentrations were then determined separately by GC–MS. This involved using selected ion-monitoring (SIM) approaches, monitoring m/z 288 (Val), 302 (Leu, Ile and Norleu), and m/z 245 (KIV and KVA) and 259 (KIC and KMV). Concentrations of plasma BCAA and BCKA were determined with reference to a standard curve of known concentrations. A pooled plasma quality control (QC) sample (study-specific sample) was prepared and analysed throughout each batch to monitor instrument performance.
GC–MS conditions
Approximately 0.5 µl of each fraction was injected into an ISQ Trace 1300 single quadrupole GC–MS (ThermoFisher Scientific, Hemel Hempstead, UK). Split injection mode (1:10) was used, with an initial oven temperature of 100 °C, held for 1 min, then ramped at 12 °C/min to 300 °C, held for 5 min to ensure elution of higher boiling compounds. Helium was the carrier gas at a flow rate of 1.5 mL/ min, and separation was achieved on a 30 m Rxi-5MS (0.25 mm internal diameter, 0.25 µm thickness) fused-silica column (Restek, Bellafonte, Pennsylvania).
Insulin and glucose concentrations
Plasma insulin and glucose, were assessed in duplicate23. Insulin was assessed via a high-sensitivity human insulin ELISA (DRG Instruments GmbH) according to manufacturer’s instructions. Glucose was measured using a clinical chemistry analyser (YSI 2950 Biochemistry analyser, YSI LifeSciences, Ohio, USA) against commercial standards. IS was calculated via HOMA-IR, according to the formula:
Statistical analysis
Based on normality of data or transformation where required, BCAA and BCKA concentrations were compared between OW and NW controls using Student’s unpaired t-tests. Changes in BCAA concentrations in OW participants who underwent 6-weeks of VLCD were compared using Student’s paired t-test. The relationship between HOMA-IR and BCAA at baseline and following VLCD was investigated using Pearson’s correlation. All data are presented as mean ± SEM with significance at p < 0.05. Analyses were performed using GraphPad Prism v8.3 (La Jolla, CA, USA).
Results
Effects of VLCD on body composition and circulating BCAA levels
Six weeks VLCD elicited reductions in whole-body mass (baseline 103.9 ± 12.3 kg, post-VLCD 93 ± 9.6 kg; p < 0.001) and BMI (baseline 32.2 ± 4, post-VLCD 28.9 ± 3.6 kg/m2; p < 0.001), with concomitant declines in whole-body lean mass (baseline 65.2 ± 6 kg, post-VLCD 60.9 ± 4.8; p < 0.001), Table 1.
Correlation between changes in fasting BCAA’s and HOMA-IR values
VLCD reduced HOMA-IR (1.2 ± 0.62 AU, p = 0.01; Fig. 3A). There was no correlation between changes in HOMA-IR and BCAA at baseline (Leu, R2: 2.498e−005, p = 0.98, Ile R2: 1.211−e006, p = 0.99, Val R2: 0.004, p = 0.85, sum BCAA R2 0.001, p = 0.93), nor following VLCD (Leu, R2: 0.003, p = 0.86, Ile R2: 0.006, p = 0.82, Val R2: 0.02, p = 0.65, sum BCAA R2: 0.004, p = 0.85), Fig. 3B–E. To increase statistical power, the association between HOMA-IR and BCAA was investigated in an additional 32 individuals (total including OW participants, N = 58) to determine if a relationship existed, however Pearson’s correlation revealed no association (R2: 0.01, p = 0.31, Fig. 3F).
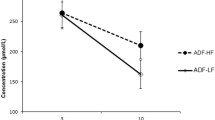
Circulating BCAA in OW compared with NW volunteers
First, an unpaired t-test revealed no gender differences in baseline BCAA concentrations between our NW female (mean 349 ± 35 µM) and male (mean 372 ± 91 µM, p = 0.51) participants. BCAAs in our OW participants (457 ± 85 µM) were higher than in NW counterparts (365 ± 78 µM; p = 0.0002; Fig. 1D). Despite no changes in leucine concentrations (Fig. 1A), these differences were driven primarily by valine (OW 253 ± 38 µM, NW 193 ± 45 µM; p < 0.0001; Fig. 1C) and isoleucine (OW 70 ± 20 µM, NW 53 ± 18 µM; p = 0.002; Fig. 1B). Despite reductions in body weight, fat, and lean mass, as well as HOMA-IR, plasma BCAA concentrations were largely unchanged (baseline: total BCAA 471 ± 98 µM, leucine 141 ± 36 µM; isoleucine 71 ± 17 µM or valine 259 µM ± 47, Fig. 2A–D) following VLCD (sum BCAA 439 ± 75 µM, p = 0.35; leucine 131 ± 27 µM, p = 0.41; isoleucine 76 ± 22 µM, p = 0.55; or valine 231 ± 32 µM, p = 0.14). Similarly, BCKA concentrations at baseline (KIC 47 ± 18 µM, KMV 22 ± 13 µM, KIV 24 ± 14 µM, sum BCKA 94 ± 42 µM) were not significantly changed following six weeks of VLCD (KIC 40 ± 13 µM p = 0.31, KMV 19 ± 10 µM, p = 0.52, KIV 15 ± 4 µM, p = 0.13, sum BCKA 75 ± 25 µM, p = 0.21, Fig. 2E–H), nor were they associated with IS at baseline or following VLCD (Fig. 3G–J).
Comparison of individual BCAA’s and sum BCAA of OW (n = 26; mean BMI 32.2 ± 2.9 kg/m2) volunteers to NW, age-matched controls (n = 26; mean BMI 25.4 ± 3 kg/m2). There was a significant increase in total BCAA (D) in OW individuals compared to NW. The differences were driven primarily by isoleucine (B) and valine (C). Leucine (A) however remained unchanged.
HOMA-IR (A) of individuals with obesity pre and post VLCD (A, P = 0.01) and correlations of HOMA-IR to individual and sum BCAA at baseline and post-VLCD (B–E). The baseline association between HOMA-IR and BCAA across a broader age and BMI range and mixed genders (F) with a greater N = 58 are displayed. The association between HOMA IR to individual BCKA (G–I) and total BCKA (J) are also displayed.
Discussion
We investigated relationships between plasma BCAA/BCKA concentrations and measures of IR in OW men following a 6-week low calorie dietary intervention in the form of a ~ 600 kcal/day VLCD. Calorie restriction remains the most effective primary care step in treating obesity due to the rapid reduction in whole body mass and subsequent improvement in glycaemic control in both men and women24,25 The magnitude of weight loss (~ 11%) was comparable to that observed in other calorie restriction studies (~ 9.5–16%);26,27 and was also accompanied by significant reductions in HOMA-IR, fat mass, visceral fat and lean body mass—indicative of compliance with the intervention, assuring efficacy of VLCD.
Previously, robust correlations between IR and BCAA have been well-documented4,10,11,28, and BCAAs have been proposed as prognostic biomarkers for populations at risk of developing T2DM5. In accordance with numerous other studies10,11,28,29, including in monozygotic twins30, and including both men and women participants11,31, BCAAs were higher in our OW participants compared to those of a NW. Further, baseline comparison of our mixed gender NW cohort revealed no within group differences (p = 0.5), suggesting that plasma BCAA concentrations are unaffected by sex in healthy individuals and thus validating our test group comparison. Indeed, further modelling reveals that BCAA alone or in combination with other metabolites5, such as aromatic amino acids (AA;Phe/Tyr) and acylcarnitine species11 alanine and proline32 may hold value as metabolic ‘signatures’ of obesity and as predictors of T2DM. Nonetheless, relationships between plasma BCAAs and other prototype metabolic ‘signatures’ have been shown to vary across the lifespan. For example, elevated BCAAs are not associated with obesity in adolescents33, indicating that any relationship with plasma BCAAs may be context-dependant29. Furthermore, these associations have also been shown to differ between sexes. Reflecting this, in females, it was shown that BCAAs, phenylalanine, and the BCAA metabolite, 3-methyl-2-oxovalerate34 when combined revealed the strongest associations with IR. Conversely, in males it was BCAA, alanine, proline, glutamine and aromatic AAs that associated most strongly32. Therefore, elevations in BCAAs alone do not indicate underlying metabolic dysfunction and show variability across the lifespan and between genders.
Contrary to previous observations between food over-consumption and higher BCAA25, we did not observe lowering of BCAA concentrations or in BCKAs, following 6-weeks of VLCD-induced weight loss. Our observations are in-line with some other VLCD studies of similar duration35,36 but contrast to other reports of BCAA lowering induced by calorie restriction induced weight loss following bariatric surgery31,37. While it is possible that individual subject characteristics may account for these contrasting results, other evidence suggests that reductions in BCAAs occur directly as a result of bariatric surgery per se, independent of weight loss. This may be due to increased BCAA catabolic gene expression in adipose tissue38, or due to the altered AA metabolism and reduced gastric capacity following operative procedures39,40. Therefore, while the causes of higher plasma BCAAs are not fully elucidated (i.e. the impact of age, caloric and protein intake, or impaired catabolism;41,42), our study suggests improvements in body composition and HOMA-IR occur independently of changes in fasting plasma BCAAs. Further, a relationship between BCAAs and IR was not apparent at baseline, in our OW participants, nor when we combined OW/NW cohorts (n = 58) to increase statistical power. This illustrates the lack of simplicity of relationships between plasma BCAAs and metabolic health; indeed in a previous study43, we demonstrated that fasting BCAAs positively correlate with lean mass and strength outcomes, as opposed to IR, following resistance exercise training.
Recent studies suggest a ‘clogging’ model of impaired BCAA catabolism, including increased accumulation of 3-hydroxyisobutyrate (3-HIB) a valine catabolite42. These authors reported increased muscle 3-HIB secretion in IR facilitates fatty acid uptake resulting in lipid accumulation42, a ‘synergistic’ relationship supported by other studies13. Genomic markers (e.g. reduced BCAA dehydrogenase complex and its regulatory enzyme protein phosphatase 1 K [PPM1K] in obese individuals)44,45 have also been proposed as possible mechanisms. In terms of BCAA catabolites, we measured each BCAA-derived BCKA as markers of altered BCAA metabolism. Similar to BCAAs, we observed neither a change in plasma BCKA concentrations (plasma biomarkers of muscle BCAA flux) or correlations between BCKAs and IS before/after VLCD. While of a preliminary nature, these findings do not support gross BCKA mis-handling in obese men. That being said, these data match those of BCAAs, thus suggesting more distal metabolites42 of BCAA metabolism may instead be implicated in tissue-level IR. Future work could adopt BCAA metabolomic and fluxomic approaches, including human muscle tissue, to address this. The lack of correlation between reductions in IR and BCAAs seen herein, despite improved metabolic health i.e. significant weight/ fat loss, suggests that reductions in BCAAs per se is not required to increase IS, but rather a metabolic reprogramming of insulin-sensitive tissue(s) in response to VLCD causes improvement in IS, preceding detectable changes in plasma BCAAs, particularly since no correlation was observed between total mass/fat loss and indices of IS.
The sample size of the VLCD cohort was a potential limitation of our study, future studies may benefit from enrolling a larger cohort in identifying robust links between plasma BCAAs and IR, as per the literature. An additional limitation of the present study may be the ‘low level’ IR of participants as a potential a confounding factor. HOMA-IR measures of ~ 3.5–5.5 have been reported in obesity11,32 compared to ~ 1.19 here. Furthermore, while VLCD elicited reductions in BMI (29 ± 4 kg/m2; ~ 10%), this improvement did not bring volunteers within the normal weight range (~ 25 kg/m2), with longer time-frames of VLCD likely required to achieve this46. A means to mitigate the loss of lean tissue or muscle mass in interventions of this nature are important to maximise the potential therapeutic benefits, with the increased protein intake being one such option. Undoubtedly, protective factors against IR and development of obesity/ T2DM include exercise participation since direct beneficial effects on β-cell function47 and liver function induced by exercise have been reported48, independent of changes in body mass.
In summary, despite VLCD resulting in weight loss and improved IS and despite higher BCAAs in OW participants, neither reductions in BCAAs nor correlations in BCAA/BCKA to HOMA-IR were observed following VLCD. We conclude that higher fasting BCAAs in obesity are unlikely a consequence of calorie over-consumption and are more likely to be genetically and/or metabolically programmed. Our findings do not rule out interventions aimed at driving BCAA/BCKA catabolism to improve IS in obesity/T2DM.
Data availability
The datasets used during the current study are available from the corresponding author on request.
References
Kelly, T., Yang, W., Chen, C. S., Reynolds, K. & He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 32(9), 1431–1437 (2008).
Shaw, J. E., Sicree, R. A. & Zimmet, P. Z. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 87, 4–14 (2010).
Cai, Q. et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care 43(7), 1392–1398 (2020).
Lynch, C. J. & Adams, S. H. Banched-chain amino acids in metabolic signalling and Insulin resistance. Nat. Rev. Endocrinol. 10(12), 723–736 (2014).
Wang, T. J. et al. Metabolite profiles and the risk of developing diabetes. Nat. Med. 17(4), 448–453 (2011).
Biswas, D. et al. Branched-chain ketoacid overload inhibits insulin action in the muscle. J. Biol. Chem. 295(46), 15597–15621. https://doi.org/10.1074/jbc.RA120.013121 (2020).
Tricò, D. et al. Elevated a-hydroxybutyrate and branched-chain amino acid levels predict deterioration of glycemic control in adolescents. J. Clin. Endocrinol. Metab. 102(7), 2473–2481 (2017).
White, P. J. et al. Branched-chain amino acid restriction in Zucker-fatty rats improves muscle insulin sensitivity by enhancing efficiency of fatty acid oxidation and acyl-glycine export. Mol. Metab. 5(7), 538–551. https://doi.org/10.1016/j.molmet.2016.04.006 (2016).
White, P. J. et al. The BCKDH kinase and phosphatase integrate BCAA and lipid metabolism via regulation of ATP-citrate lyase. Cell Metab. 27(6), 1281–1293. https://doi.org/10.1016/j.cmet.2018.04.015 (2018).
Felig, P., Marliss, E. & Cahill, G. F. Plasma amino acid levels and insulin secretion in obesity. N. Engl. J. Med. 1(9), 39–42 (1969).
Newgard, C. B. et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 9(4), 311–326. https://doi.org/10.1016/j.cmet.2009.02.002 (2009).
Tobias, D. K. et al. Fasting status and metabolic health in relation to plasma branched chain amino acid concentrations in women. Metabolism 117, 154391. https://doi.org/10.1016/j.metabol.2020.154391 (2021).
Newgard, C. B. Interplay between lipids and branched-chain amino acids in development of insulin resistance. Cell Metab. 15(5), 606–614. https://doi.org/10.1016/j.cmet.2012.01.024 (2012).
Kubacka, J., Cembrowska, P., Sypniewska, G. & Stefanska, A. The association between branched-chain amino acids (Bcaas) and cardiometabolic risk factors in middle-aged caucasian women stratified according to glycemic status. Nutrients 13(10), 3307 (2021).
Wilkinson, D. J. et al. Effects of leucine and its metabolite β-hydroxy-β-methylbutyrate on human skeletal muscle protein metabolism. J. Physiol. 591(11), 2911–2923 (2013).
Hernández-Alvarez, M. I. et al. Early-onset and classical forms of type 2 diabetes show impaired expression of genes involved in muscle branched-chain amino acids metabolism. Sci. Rep. 7(1), 1–12 (2017).
David, J., Dardevet, D., Mosoni, L., Savary-Auzeloux, I. & Polakof, S. Impaired skeletal muscle branched-chain amino acids catabolism contributes to their increased circulating levels in a non-obese insulin-resistant fructose-fed rat model. Nutrients 11(2), 1–13 (2019).
Crossland, H. et al. Exploring mechanistic links between extracellular branched-chain amino acids and muscle insulin resistance: An in vitro approach. Am. J. Physiol. Cell Physiol. 319(6), C1151–C1157 (2020).
Lim, E. L., Lim, K., Hollingsworth, K. G. & Aribisala, B. S. Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 (2011).
Lean, M. E. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomised trial. Lancet 391(10120), 541–551. https://doi.org/10.1016/S0140-6736(17)33102-1 (2018).
Hong, K., Li, Z., Wang, H. J., Elashoff, R. & Heber, D. Analysis of weight loss outcomes using VLCD in black and white overweight and obese women with and without metabolic syndrome. Int. J. Obes. 29(4), 436–442 (2005).
Willi, S. M., Martin, K., Datko, F. M. & Brant, B. P. Treatment of type 2 diabetes in childhood using a very-low-calorie diet. Diabetes Care 27(2), 348–353 (2004).
Phillips, B., Williams, J. P., Greenhaff, P. L., Smith, K. & Atherton, P. J. Physiological adaptations to resistance exercise as a function of age. JCI Insight 2(17), 1–16 (2017).
Muscogiuri, G. et al. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 17(1), 1–9. https://doi.org/10.1186/s12967-019-2104-z (2019).
Goday, A. et al. Short-Term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus. Nutr. Diabetes 6(9), e230 (2016).
Colleluori, G. et al. Aerobic plus resistance exercise in obese older adults improves muscle protein synthesis and preserves myocellular quality despite weight loss. Cell Metab. 30(2), 261-273.e6 (2019).
La Vignera, S. et al. The ketogenic diet corrects metabolic hypogonadism and preserves pancreatic ß-cell function in overweight/obese men: A single-arm uncontrolled study. Endocrine https://doi.org/10.1007/s12020-020-02518-8 (2020).
Siddik, M. A. B. & Shin, A. C. Recent progress on branched-chain amino acids in obesity, diabetes, and beyond. Endocrinol. Metab. 34(3), 234–246 (2019).
Le Couteur, D. G. et al. Branched chain amino acids, cardiometabolic risk factors and outcomes in older men: The concord health and ageing in men project. J. Gerontol. Ser. A 75(10), 1–6 (2019).
Pietiläinen, K. H. et al. Global transcript profiles of fat in monozygotic twins discordant for BMI: Pathways behind acquired obesity. PLoS Med. 5(3), 0472–0483 (2008).
Shah, S. H. et al. Branched-chain amino acid levels are associated with improvement in insulin resistance with weight loss. Diabetologia 55(2), 321–330 (2012).
Tai, E. S. et al. Insulin resistance is associated with a metabolic profile of altered protein metabolism in Chinese and Asian-Indian men. Diabetologia 53(4), 757–767 (2010).
Mihalik, S. J. et al. Metabolomic profiling of fatty acid and amino acid metabolism in youth with obesity and type 2 diabetes: Evidence for enhanced mitochondrial oxidation. Diabetes Care 35(3), 605–611 (2012).
Menni, C. et al. Biomarkers for type 2 diabetes and impaired fasting glucose using a nontargeted metabolomics approach. Diabetes 62(12), 4270–4276 (2013).
Lips, M. A. et al. Roux-en-Y gastric bypass surgery, but not calorie restriction, reduces plasma branched-chain amino acids in obese women independent of weight loss or the presence of type 2 diabetes. Diabetes Care 37(12), 3150–3156 (2014).
Laferrère, B. et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 93(7), 2479–2485 (2008).
Magkos, F. et al. Effect of roux-en-y gastric bypass and laparoscopic adjustable gastric banding on branched-chain amino acid metabolism. Diabetes 62(8), 2757–2761 (2013).
She, P., Reid, T., Huston, S., Cooney, R. & Lynch, C. Obesity-related elevations in plasma leucine are associated with alterations in enzymes involved in branched chain amino acid (BCAA) metabolism. Am. J. Physiol. Endocrinol. Metab. 293(1), 1–7 (2007).
Steenackers, N., Gesquiere, I. & Matthys, C. The relevance of dietary protein after bariatric surgery: What do we know?. Curr. Opin. Clin. Nutr. Metab. Care 21(1), 58–63 (2018).
Ferreira Nicoletti, C. et al. Protein and amino acid status before and after bariatric surgery: A 12-month follow-up study. Surg. Obes. Relat. Dis. 9(6), 1008–1012. https://doi.org/10.1016/j.soard.2013.07.004 (2013).
Elshorbagy, A. K. et al. Food overconsumption in healthy adults triggers early and sustained increases in serum branched-chain amino acids and changes in cysteine linked to fat gain. J. Nutr. 148(7), 1073–1080 (2018).
Jang, C. et al. A branched-chain amino acid metabolite drives vascular fatty acid transport and causes insulin resistance. Nat. Med. 22(4), 421–426 (2016).
Sayda, M. H. et al. Associations between plasma branched chain amino acids and health biomarkers in response to resistance exercise training across age. Nutrients 12(10), 3029 (2020).
She, P. et al. Disruption of BCATm in mice leads to increased energy expenditure associated with the activation of a futile protein turnover cycle. Cell Metab. 6(3), 181–194 (2007).
Wang, Q., Holmes, M. V., Smith, G. D. & Ala-Korpela, M. Genetic support for a causal role of insulin resistance on circulating branched-chain amino acids and inflammation. Diabetes Care 40(12), 1779–1786 (2017).
Hammer, S. et al. Prolonged caloric restriction in obese patients with type 2 diabetes mellitus decreases myocardial triglyceride content and improves myocardial function. J. Am. Coll. Cardiol. 52(12), 1006–1012 (2008).
Heiskanen, M. A. et al. Exercise training decreases pancreatic fat content and improves beta cell function regardless of baseline glucose tolerance: A randomised controlled trial. Diabetologia 61(8), 1817–1828 (2018).
Keating, S. E., Hackett, D. A., George, J. & Johnson, N. A. Exercise and non-alcoholic fatty liver disease: A systematic review and meta-analysis. J. Hepatol. 57(1), 157–166. https://doi.org/10.1016/j.jhep.2012.02.023 (2012).
Acknowledgements
The authors thank the participants who participated in this study. The authors also thank Kate Hession for assistance on study days.
Funding
This research was supported by the MRC-Versus Arthritis Centre for Musculoskeletal Ageing Research (Grant Nos. MR/R502364/1, MR/P021220/1) and the National Institute for Health Research (NIHR) Nottingham Biomedical Research Centre. M.H.S. is funded by The National Centre for Sport and Exercise Medicine–East Midlands.
Author information
Authors and Affiliations
Contributions
P.J.A., K.S., I.I., B.E.P., D.J.W., and P.L.G. conceptualised the study. H.A. and N.G. performed study interventions and undertook sample collection. M.H.S., H.A. and N.G. performed laboratory analysis. M.H.S., P.J.A., K.S., B.E.P., D.J.W., and I.I., analysed and visualised the data. All contributed to drafting the manuscript and have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sayda, M.H., Abdul Aziz, M.H., Gharahdaghi, N. et al. Caloric restriction improves glycaemic control without reducing plasma branched-chain amino acids or keto-acids in obese men. Sci Rep 12, 19273 (2022). https://doi.org/10.1038/s41598-022-21814-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-21814-z
- Springer Nature Limited