Abstract
To alleviate anti-cancer treatment burden in advanced breast cancer, patient-clinician communication strategies based on nocebo-effect mechanisms are promising. We assessed distinct/combined effects on psychological outcomes (e.g. anxiety; main outcome) and side-effect expectations of (1) nocebo information about the (non)pharmacological origin of side effects, and (2) clinician-expressed empathy through reassurance of continuing support. Furthermore, we explored whether information and empathy effects on side-effect expectations were mediated by decreased anxiety. In a two-by-two experimental video-vignette design, 160 cancer patients/survivors and healthy women watched one of four videos differing in level of nocebo information (±) and empathy (±). Regression and mediation analysis were used to determine effects of information/empathy and explore anxiety’s mediating role. Anxiety was not influenced by empathy or information (Stai-state: p = 0.281; p = 0.410, VAS p = 0.387; p = 0.838). Information improved (specific) side-effect coping expectations (p < 0.01). Empathy improved side-effect intensity expectations (p < 0.01 = specific; p < 0.05 = non-specific/partial) and specific side-effect probability expectations (p < 0.01), and increased satisfaction, trust, and self-efficacy (p < 0.001). No mediating effects were found of anxiety on expectations. Mainly empathy, but also nocebo information improved psychological outcomes and—mainly specific—side-effect expectations. Exploring the power of these communication elements in clinical practice is essential to diminish the anti-cancer treatment burden in advanced breast cancer.
Similar content being viewed by others
Introduction
While anti-cancer treatment in advanced illness, such as incurable breast cancer, may prolong patients’ quantity of life, it may also be associated with impaired quality of life. Many patients experience considerable psychological and physical symptoms and side effects, with 30–74% experiencing symptoms such as anxiety, nausea, insomnia, and fatigue1. Treatment side effects are, apart from disease progression, key factors in the decision to stop treatment2 and may contribute to poorer overall quality of life3.
In a quest to find better ways to alleviate burdensome symptoms and side effects, we may need to look beyond merely pharmacological treatments and focus on communication strategies based on nocebo-effect mechanisms. In the context of side effects, nocebo effects are those side effects that are not solely attributable to pharmacological substances of the anti-cancer treatment4,5 but are due to, or exacerbated by, patient expectations, past experiences6, or the therapeutic context7. It is thought that nocebo effects play a greater role in the non-specific (non-dose-dependent) side effects of treatments, such as insomnia4, although they can also aggravate specific (dose-dependent) side effects, such as hair loss8.
Indeed, there is abundant evidence that manipulating patients’ expectations of treatments is a mechanism that elicits nocebo effects9,10. Merely informing patients about possible treatment side effects can increase the numbers who report those side effects and can intensify worry and concern4,11,12,13. In contrast, intriguing new studies (including open-label placebo studies14) seem to indicate that informing patients about the existence and functioning of the nocebo effect can actually reduce side effects15,16,17. These studies indicate that educating patients about the non-pharmacological origin of side effects may strengthen their perceived control over, primarily non-specific effects15,17, and (for patients with advanced cancer) may even decrease side-effect occurrence16 and severity (Michnevich et al., submitted). In these studies, psycho-education occurred outside the medical consultation; it is not yet known whether the same results would be found if clinician-expressed information about the nocebo effect were integrated into the doctor-patient consultation.
Another mechanism potentially capable of alleviating nocebo effects is clinician-expressed empathy. There is evidence that clinician-expressed empathy can reduce pain18 and improve patient satisfaction and quality of life19,20,21,22,23. In advanced cancer, a particularly powerful empathic behaviour is to reassure patients that they will receive continuing support and will be well taken care of: this has been found—mainly in experimental studies—to reduce feelings of anxiety and increase self-efficacy and information recall7,20,24,25. However, it has not yet been determined whether clinician-expressed reassurance of continuing support may lessen—expected—side effects.
Moreover, it is important to explore the pathways through which clinician-expressed nocebo-effect information and empathy may alleviate the—expected—side effects of anti-cancer treatment. In general, clinician-expressed empathy is often thought to alleviate patient anxiety20,21. Furthermore, anxiety sensitivity has also been found to positively correlate with nocebo responses26,27 and has been associated with patients’ physical impairment28. Therefore it might be promising to examine whether the potential effects of clinician-expressed information and empathy on expected specific and/or non-specific side effects might be routed via a decrease in patients’ anxiety.
Against this background, the aims of this experimental study conducted in the setting of advanced breast cancer are twofold. First, we investigate how nocebo information and clinician-expressed empathy may affect patients’ psychological outcomes (e.g., anxiety; main outcome) and expectations regarding side effects. Specifically, we will examine the distinct and combined effects of (1) nocebo information about the non-pharmacological origin of side effects, and (2) clinician-expressed empathy through reassurance of continuing support. Second, we explore whether the effect of information and empathy on side-effect expectations may be mediated by a decrease in participants’ anxiety. We will include expectations regarding occurrence, intensity, and coping in relation to both specific (dose-dependent) and non-specific (non-dose-dependent) side effects. Pursuing these aims can provide insight into the causal effect of communication strategies in the setting of advanced cancer and may pave the way towards alleviating patients’ psychological symptoms and side effects.
Methods
Design
An experimental video-vignette study was employed, with a 2 × 2 design. Four role-played video vignettes were developed, depicting a consultation between an oncologist and a patient with advanced breast cancer, in which potential treatments (chemotherapy) were discussed. All video vignettes were equal in communication and content; the only variations concerned the level of nocebo information (with (+) or without (−) a nocebo explanation) and empathy (with (+) or without (−) added reassurance of continuing support) (see Table 1 for the design). Reporting conformed to CONSORT guidelines29.
Script and video development
The videos were developed following the steps postulated by Hillen et al.30. The scripts were created by the research group (researchers, clinicians, and patient representatives). Content and manipulations were based on clinical observations25, a qualitative preparatory study31, previous experimental video-vignette20,21,25,32,33 and open-label studies15,34, and research/clinical/patient expertise of the research group. To ensure the internal (i.e., manipulation success) and external (e.g., realism) validity of the videos, an expert group of clinicians, researchers, patients/survivors, and healthy women were involved in creating/piloting the videos (see Online Appendix 1 for the development procedures, including internal/external validity evaluations). The final scripts were role-played by professional actors. The exact manipulations are displayed in Table 2; the total final scripts are displayed in Online Appendix 2.
Ethics
The study was approved by the Ethics Committee of Leiden University, Department of Psychology [2021-01-27-L.M. van Vliet-V1-2909], and was registered at the Dutch Trial Registration (NTR NL8992, on 21/10/2020). All methods were performed in accordance with relevant guidelines and regulations, and all participants signed informed consent at the time of participation.
Participants and sample size
Adult (18 > older) female cancer patients/survivors and healthy women with sufficient command of Dutch could participate. All participants (cancer patients, cancer survivors and healthy women) acted as Analogue Patients (APs) when viewing the video, putting themselves in the shoes of the patient with advanced breast cancer in the video. The validity of the AP methodology has been shown35,36, and previous studies found no differences in response between healthy women and cancer patients20,33. We included only female participants as it might be more difficult for male participants to identify with the female actor-patient.
In line with previous studies20,21 we used anxiety as a primary outcome. Based on a previous study21 using a similar experimental design that found a medium effect size (Cohen’s d = 0.28) for the primary outcome (i.e. anxiety), it was estimated20 that a sample size of 144 was required to attain 80% power for detecting two main effects and one interaction effect at p < 0.05. To obtain valid responses of 144 participants, we aimed to recruit up to 160 participants.
Recruitment and procedures
Participants were recruited online via patient organizations (e.g., Dutch Breast Cancer Society (BVN)) or social media (e.g. LinkedIn, Twitter), and through advertisements in shops, requests to former participants in our studies on cancer communication who consented to be contacted again, personal contacts, and snowballing procedures. Particular efforts were made to recruit women from non-western migrant backgrounds (e.g., via patient organization Mammarosa and key contact persons), as they are often underrepresented in research37. After reading an online advertisement text, participants could access a webpage (hosted via Qualtrics) containing the information letter and electronic consent form. After providing informed consent, they entered the experiment webpage. First, background characteristics were assessed. Next, Qualtrics stratified participants into (1) current cancer patients and (2) cancer survivors and healthy women, and assigned them equally and randomly to one of the four videos. We monitored inclusion to ensure both groups were sufficiently represented. Next, final outcome measures were assessed, and at study end participants were debriefed and could receive $5.90 (5 euro) reimbursement. All data were collected anonymously. Participants could contact the research team for questions and emotional support and could leave the study at any time without consequences.
For non-western participants recruited via patient organizations, participation was supported by the research team in person or via video conference (Zoom.us). If necessary, patients were assisted with completing the questionnaires.
Measures
Questionnaires were composed in collaboration with patient representatives. The following measures were assessed.
Pre-video
Demographics
Sociodemographic and cancer-related characteristics using self-created questionnaires.
Personality characteristics
(1) Trait anxiety (STAI-trait)38 (2) Optimism (LOT-R39), (3) Coping styles monitoring (attending to threatening information) and blunting (avoiding threatening information) (TMSI shortened version40); (4) Coping information needs (Degree to which patients want to be informed about (a) proposed medical treatment, (b) potential side effects of proposed treatment (0–10 Numerical Rating Scale (NRS) ‘no information at all’ to ‘as much information as possible’), adapted from a previous study15);
Psychological outcome
Anxiety: (a) State anxiety (STAI-state)SPS:refid::bib3838 (main outcome), (b) current anxiety levels (0–100 Visual Analogue Scale (VAS), ‘not at all’ to ‘very much’22,41).
Anticipated side effects
(a) General side-effect expectations, (b) general side-effect experiences16,42, (c) current side effects (0–100 VAS ‘not at all ‘to ‘very much’), all adapted from previous studies16,43.
Post-video
Psychological outcomes
-
i.
Anxiety: (a) State anxiety (STAI-state)38 (main outcome), (b) current anxiety levels (0–100 VAS, ‘not at all’ to ‘very much’22,41); The post–pre video anxiety difference scores were used for all analysis.
-
ii.
Satisfaction with the communication in the consultation (0–10 NRS ‘not satisfied at all’ to ‘extremely satisfied’), adapted from previous study21,22;
-
iii.
Trust in the doctor (0–10 NRS ‘no trust at all’ to ‘full trust’, self-created);
-
iv.
self-efficacy (i.e. the feeling of being able to handle the future) (0–10 NRS ‘very little’ to ‘very great’)20;
Side-effect (coping) expectations
For a list of 13 pre-defined side effects (determined in collaboration with the oncologists involved and divided into the groups ‘specific’ (i.e., hair loss, nausea, diarrhea, impaired immune system functioning, neuropathy), ‘non-specific’ (i.e., loss of interest/apathy, insomnia, being abrupt/irritability) and ‘partially specific/non-specific’ (i.e. cognitive impairment, fatigue, headache, concentration problems, rash), we assessed participants’ expectations regarding: (a) probability: probable occurrence of side effects (0–10 NRS scale, ‘not probable at all’ to ‘very probable’, self-created question adapted from16,43, (b) intensity: intensity (severity) of side effects (0–10 NRS scale, ‘not at all intense’ to ‘very intense’ using a modified version of the GASE44, adapted from15), (c) Coping: coping with side effects (0–10 NRS scale, ‘not handling at all’ ‘handling very well’, using a modified version of the GASE44 adapted from15).
Manipulation success
Participants assessed the extent to which the oncologist a. provided information about the non-pharmacological origin of side effects, and b. provided reassurance of continuing support (0–10 NRS scales ‘not at all’ to ‘completely’).
Analysis
First, background characteristics were described. One-way ANOVA and χ2 tests were performed to compare the background characteristics between the four conditions. Variables that differed between groups were included as covariates (i.e., control variables) in subsequent analysis. Second, manipulation successes were determined with independent t-tests. Third, to assess whether data from current cancer patients and cancer survivors/healthy women could be pooled, we compared their responses to the four conditions on the anxiety and side-effect outcomes. Fourth, using regression analysis, the influence of the following pre-video characteristics on anxiety and side-effect outcomes was assessed (as they might influence communication preferences): age45, education45, trait anxiety46, optimism47, (in)direct chemotherapy experiences48, migrant background49, coping20,50, treatment and side-effect information need, general side-effect expectations51 and side-effect experiences, current side effects. The three characteristics (number chosen due to power limits) with the strongest effects (p < 0.01) were used as control variables in, fifth, hierarchical regression analysis to assess the main and interaction effects of ‘information’ and ‘empathy’ (using contrast coding, − 0.5 and 0.5) on all outcome measures. Interaction effects were eliminated from the model if insignificant. We applied an appropriate transformation for negatively skewed data (the log10 of the inverse). For independent variables, migration background was transformed into two dummy variables (with native Dutch as reference group). To ease interpretation, the raw (uncontrolled) mean scores and Cohen’s d were described for nocebo information and empathy. Lastly, using PROCESS52 mediation analysis, we explored the effects on side-effect expectations of information and empathy via anxiety-reduction. Analyses were conducted using SPSS Version 25.0 at p < 0.01 (p < 0.05 trend significance).
Results
Sample
When we reached our required sample size of 160 participants (at April 19th), 60 other participants already dropped-out due to one of the reasons as mentioned in Fig. 1 (p. 10). At the end, one participant chose to opt out (data were removed). The 160 women who completed the main outcome (STAI-state anxiety) were included in our analysis (Fig. 1). These 160 participants had a mean age of 52.93 years (SD 12.14), had mainly attended higher education (67%), and were mainly of Dutch origin (81%). There were no significant differences in background characteristics between the conditions (see Table 3).
CONSORT diagram showing randomization assignment and participant flow by the group. *Randomization took place after background characteristics had been provided. Drop-out during background characteristics provision was n = 33; drop-out after randomization was n = 28. Data collection took place between February 8 and April 19, 2021.
Manipulation success
The manipulations succeeded. In the videos with added nocebo information, the clinician was more strongly perceived as providing an explanation that side effects can have both pharmacological and non-pharmacological (psychological) origins (present: M = 8.06, SD = 1.77; absent: M = 2.05, SD = 2.05, p < 0.001). In the videos with the empathy manipulations, the clinician was perceived as providing more reassurance of continuing support than in the videos without empathy (present: M = 8.64, SD = 1.40; absent: M = 5.11, SD = 2.60, p < 0.001).
Pooling of data
As current patients and healthy women/survivors responded the same to all but one video (information+/empathy+ for anxiety Stai-state, Online Appendix 3), data were pooled for the main analysis.
Control variables
The three participant characteristics that had the strongest association (p- < 0.001, data not shown) with outcome measures were pre-video trait anxiety, migrant background, and treatment information needs. These variables were included as control variables in the subsequent regression model (Model 2, Table 4).
Main and interaction effects of nocebo information and empathy
Nocebo information
As demonstrated in Table 4, in controlled models the nocebo explanation did not influence APs’ anxiety levels (Stai-state: p = 0.410, VAS p = 0.838), or their feelings of satisfaction, trust, and self-efficacy (p > 0.05). The nocebo explanation improved coping expectations regarding specific side effects but this effect was dependent on the level of empathy (the interaction effect was significant; p < 0.01). This interaction effect revealed that when empathy was present the nocebo explanation improved coping expectations but without empathy the information decreased the expectations (see Fig. 2). Nocebo information did not influence expectations concerning the intensity or probability of side effects (p > 0.10). Outcomes for present and absent nocebo explanation are displayed in Table 5, demonstrating that apart from specific coping, for which the effect size (uncontrolled) was 0.40, all other effects were small.
Empathy
As demonstrated in Table 4, in controlled models reassurance of continuing support did not influence anxiety levels (Stai-state: p = 0.281, VAS p = 0.387) but did increase feelings of satisfaction, trust, and self-efficacy (p < 0.001). Following reassurance, APs also expected side effects to be less intensive (p < 0.01 = specific; p < 0.05 = non-specific and partial), and specific side effects less probable to occur (p < 0.01; non-specific and partial probability were p > 0.05); however, their coping expectations did not improve (p > 0.05). APs’ outcomes for with and without added reassurance are displayed in Table 5, demonstrating that all the significant effects of empathy represent a medium effect size (ranging from d = 0.49 for specific intensity to d = 0.66 for self-efficacy).
Control variables
While most associations between control variables and outcomes were insignificant, it did emerge that after the videos, APs with higher trait anxiety were less anxious than those with lower trait anxiety; and those with higher information needs were more satisfied than those with lower information needs. APs with a non-western background tended to expect somewhat worse side-effect outcomes (Table 4).
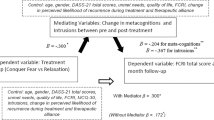
Mediating role of anxiety
In no case was the effect of nocebo information and empathy on side-effect expectations mediated by APs’ state anxiety levels (for direct, indirect, and total effects see online Appendix 4). The direct effects of information and empathy on side effects were in line with the results of the regression analyses.
Discussion
In this online experimental video-vignette study—among Aps—we explored how nocebo information and clinician-expressed empathy affect patients’ general psychological well-being and expectations of experiencing side effects. Specifically, we aimed to determine how psychological outcomes (e.g., anxiety, main outcome) and side-effect expectations were affected by the clinician providing nocebo information about the non-pharmacological origin of side effects, and/or expressing empathy through reassurance of continuing support: we examined the distinct and combined effects of these two variables. In addition, we explored whether the effect of information and empathy on APs’ side-effect expectations might be mediated by a decrease in their anxiety.
Results indicated that neither information nor empathy had an effect on APs’ anxiety levels; only empathy improved other psychological outcomes. Empathy also led APs to expect that specific side effects were less probable and would be less intense. Information improved APs’ expectations of being able to cope with specific side effects. No mediating role of anxiety was found.
In our study, the nocebo explanation had little influence overall on APs’ expected side-effect occurrence and intensity. This finding contradicts previous studies in which nocebo explanations led to actual symptom reduction among patients with weekly headaches16, and to increased feelings of perceived control17 and decreased severity of side effects among cancer patients (Michnevich et al., under review). This contradiction might be due to our experimental design incorporating the nocebo explanation into the oncologist-patient encounter, as opposed to longer psycho-education conducted in clinical practice15,16,17; however, it also brings to light some peculiarities. First, our finding that nocebo information improved (only) APs’ coping expectations regarding specific side effects contradicts the thinking of the previous studies that nocebo information affects the experience of more non-specific side effects of treatments15,17 (Michnevich et al., under review). Given our results, we can only speculate that, when it came to coping expectations, the specific side effects may have been more readily known to our APs, since the term ‘side effects’ usually refers to pharmacological effects16. Second, we should note that although the clinical study of Michnevich et al. did find an effect on side-effect experiences, it too failed to find an effect on side-effect expectations, which raises the question whether expectations even are the pathway via which nocebo explanations influence actual side effects. Clinical follow-up studies are needed to better understand the pathway(s) of how a nocebo explanation may affect experiences of side effects (whether specific or non-specific).
The finding that information did not influence APs’ psychological outcomes (anxiety (main outcome); satisfaction with the communication; trust in the doctor; self-efficacy), may seem less surprising, as cognitive and affective communication serve different patient needs48,53. At the same time, it should not be overlooked that a clinician explaining the non-pharmacological origin of side effects did not increase psychological distress. Especially since it can be argued that the majority of the nocebo expectations in (particularly cancer) patients comes from the necessities for transparency about the options and consequences of treatment. While clinicians are legally and morally imperative to convey side-effect information, this exact information might also harm. Qualitative comments from our pilot studies and consultations with patients showed that there is a fine line between the realization that side effects have a non-pharmacological component and the idea that side effects are all in one’s head, which our intervention successfully seemed to balance.
Unlike previous studies21,32,42,48, in the present research empathy did not affect patient anxiety, and although it is acknowledged that empathy is no magic bullet54, this finding remains difficult to explain. While we could argue that discussion of a relatively young mother’s incurable cancer may evoke anxiety independently of communication style, this is not in line with previous video-vignette studies20,21. That being said, empathy did, in line with other studies, influence psychological outcomes such as trust33,55 and satisfaction20,23, providing further evidence that short empathic statements can influence psychological outcomes for the better32,56.
At the same time, also somewhat unexpectedly, empathy led to APs’ expecting specific side effects (as opposed to non-specific, as discussed above) to be less intensive and less probable to occur. This finding raises questions about the active ingredients in current nocebo-explanation interventions, in which information provision is often combined with an empathic attitude15,16,17. Indeed, the few studies that have disentangled clinician-provided positive information from an empathic attitude have found that it is only when positive clinician-information is provided in a warm and caring manner that psychological outcomes such as anxiety, satisfaction, and stress are improved21,57,58. These studies’ suggestion that physician empathy is of utmost importance for patients, and essential for information provision, is in line with our notable effect sizes for the enhanced empathy condition. By comparison, clinical studies have found similar small to moderate effect sizes of patients’ response expectancies on overall cancer treatment-related side effects (r = 0.153–0.431)59,60. This adds to the evidence that empathy may decrease patients’ physical experiences and symptoms19,23,61, and may also facilitate information provision in advanced cancer settings31,32. As such we may assume that integrating empathy into the doctor-patient consultation could be a—clinically relevant, factor for alleviating the burden of anti-cancer treatment.
While it is important—in the interests of increasing the evidence base of communication—to disentangle the pathways via which various communication elements operate, our study did not find that anxiety plays a mediating role between information and empathy and side-effect expectations. Although anxiety has been associated with nocebo effects26,27, there are also previous studies which failed to find that clinician-expressed empathy improves patient outcomes via a decrease in anxiety32,56,62. Given the effect sizes in our study for trust (d = 0.52), self-efficacy (d = 0.66) and satisfaction (d = 0.52), future studies might consider investigating the potential mediating roles of these outcome measures.
Lastly, our study suggests that some people may be more prone to experience side effects than others depending on their personality traits (e.g., neuroticism)63,64, and (although this is relatively underexplored) that patients from non-western groups may expect worse outcomes than those of western origin 65,66, showing that communication strategies are no one-size-fits-all. Our findings showed that patients with higher trait anxiety, with greater treatment information needs, and with a non-western migration background expected to experience more side effects. Interestingly, there is some indication that both anxious patients67 and those with high information needs20 may actually benefit the most from empathy. It is important to explore how patients with a non-western background may benefit from empathy, especially since non-western minority groups may receive less empathy than western patients68,69.
Our study has limitations. First, despite efforts to recruit patients from non-western migrant backgrounds, the majority of our participants were native Dutch, highly educated women. Given the online format, people without internet access (3% in the NL, mainly third-grade educated elderly > 65)70 could not participate easily. Furthermore, we did not explore demographic differences between the 60 participants who dropped out and the 160 who completed the study as stated in our rules for data handling as within the informed consent. This limits the generalizability of our results54. Second, caution is needed towards the significant effects found for our secondary outcome variables (Table 4) because we did not correct for multiple testing, and therefore the overall significance level was inflated. Third, scripted studies remain proxies for clinical interactions, especially as we only assessed side-effect expectations and did not measure actual experiences, so results can only with caution be generalized to clinical patients. However, video vignettes provide an ethically and methodologically sound opportunity to test causal effects of specific communication elements before follow-up studies in clinical practice. Future clinical follow-up studies with a representative sample are needed to determine the effects of nocebo explanations and reassurance of continuing support in clinical practice and should explore through which underlying mechanisms information and empathy may operate.
To conclude, as a first step we have demonstrated that empathy—and to a lesser extent nocebo information—can improve psychological outcomes and side-effect expectations in APs in an experimental setting. Exploring the power of these communication elements in clinical practice is essential to reduce the burden of anti-cancer treatment in advanced breast cancer.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
29 September 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-42781-z
References
Teunissen, S. C. et al. Symptom prevalence in patients with incurable cancer: A systematic review. J. Pain Symptom Manag. 34, 94–104 (2007).
Clarke, G., Johnston, S., Corrie, P., Kuhn, I. & Barclay, S. Withdrawal of anticancer therapy in advanced disease: A systematic literature review. BMC Cancer 15, 1–9 (2015).
Cramarossa, G. et al. Predictive factors for overall quality of life in patients with advanced cancer. Supportive Care Cancer 21, 1709–1716 (2013).
Barsky, A. J., Saintfort, R., Rogers, M. P. & Borus, J. F. Nonspecific medication side effects and the nocebo phenomenon. JAMA 287, 622–627 (2002).
Finniss, D. G., Kaptchuk, T. J., Miller, F. & Benedetti, F. Biological, clinical, and ethical advances of placebo effects. Lancet 375, 686–695 (2010).
Marchant, J. Placebos: Honest fakery. Nature 535, S14–S15 (2016).
Di Blasi, Z., Harkness, E., Ernst, E., Georgiou, A. & Kleijnen, J. Influence of context effects on health outcomes: A systematic review. Lancet 357, 757–762 (2001).
Nestoriuc, Y. et al. Is it best to expect the worst? Influence of patients’ side-effect expectations on endocrine treatment outcome in a 2-year prospective clinical cohort study. Ann. Oncol. 27, 1909–1915 (2016).
Tracey, I. Getting the pain you expect: Mechanisms of placebo, nocebo and reappraisal effects in humans. Nat. Med. 16, 1277–1283 (2010).
Petersen, G. L. et al. The magnitude of nocebo effects in pain: A meta-analysis. Pain 155, 1426–1434 (2014).
Cocco, G. Erectile dysfunction after therapy with metoprolol: The Hawthorne effect. Cardiology 112, 174–177 (2009).
Barsky, A. J. The iatrogenic potential of the physician’s words. JAMA 318, 2425–2426 (2017).
Jacobs, W., Das, E. & Schagen, S. Increased cognitive problem reporting after information about chemotherapy-induced cognitive decline: The moderating role of stigma consciousness. Psychol. Health 32, 78–93 (2017).
von Wernsdorff, M., Loef, M., Tuschen-Caffier, B. & Schmidt, S. Effects of open-label placebos in clinical trials: A systematic review and meta-analysis. Sci. Rep. 11, 1–14 (2021).
Quidde, J. et al. Preventing adverse events of chemotherapy by educating patients about the nocebo effect (RENNO study)–study protocol of a randomized controlled trial with gastrointestinal cancer patients. BMC Cancer 18, 1–8 (2018).
Pan, Y., Kinitz, T., Stapic, M. & Nestoriuc, Y. Minimizing drug adverse events by informing about the nocebo effect—An experimental study. Front. Psychiatry 10, 504 (2019).
Shedden-Mora, M. C. et al. Optimizing expectations about endocrine treatment for breast cancer: Results of the randomized controlled psy-breast trial. Clin. Psychol. Europe 2, 1–20 (2020).
Howick, J. et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J. R. Soc. Med. 111, 240–252 (2018).
Mistiaen, P. et al. The effect of patient-practitioner communication on pain: A systematic review. Eur. J. Pain (Lond. Engl.). https://doi.org/10.1002/ejp.797 (2015).
Van Vliet, L. M., Van Der Wall, E., Plum, N. M. & Bensing, J. M. Explicit prognostic information and reassurance about nonabandonment when entering palliative breast cancer care: Findings from a scripted video-vignette study. J. Clin. Oncol. 31, 3242–3249 (2013).
van Osch, M., van Dulmen, S., van Vliet, L. & Bensing, J. Specifying the effects of physician's communication on patients’ outcomes: A randomised controlled trial. Patient Educ. Couns. 100, 1482–1489 (2017).
Hoffstädt, H. et al. Patients’ and clinicians’ perceptions of clinician-expressed empathy in advanced cancer consultations and associations with patient outcomes. Pal. Med. Rep. 1, 76–83 (2020).
Howick, J., Mittoo, S., Abel, L., Halpern, J. & Mercer, S. W. A price tag on clinical empathy? Factors influencing its cost-effectiveness. J. R. Soc. Med. 113, 389–393 (2020).
Back, A. L. et al. Abandonment at the end of life from patient, caregiver, nurse, and physician perspectives: Loss of continuity and lack of closure. Arch. Inter. Med. 169, 474–479 (2009).
Van Vliet, L. M. et al. The use of expectancy and empathy when communicating with patients with advanced breast cancer; an observational study of clinician-patient consultations. Front. Psychiatry. 10, 464 (2019).
Corsi, N. & Colloca, L. Placebo and nocebo effects: The advantage of measuring expectations and psychological factors. Front. Psychol. 8, 308 (2017).
Whitford, H. S. & Olver, I. N. When expectations predict experience: The influence of psychological factors on chemotherapy toxicities. J. Pain Symptom Manag. 43, 1036–1050 (2012).
Stark, D. P. H. & House, A. Anxiety in cancer patients. Br. J. Cancer 83, 1261–1267 (2000).
Schulz, K. F., Altman, D. G. & Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ (Clin. Res. Ed.) 340(c332), 2010. https://doi.org/10.1136/bmj.c332 (2010).
Hillen, M. A., van Vliet, L. M., de Haes, H. C. & Smets, E. M. Developing and administering scripted video vignettes for experimental research of patient–provider communication. Patient Educ. Couns. 91, 295–309 (2013).
van Vliet, L. M. et al. Addressing challenges in information-provision: A qualitative study among oncologists and women with advanced breast cancer. BMC Palliat. Care 20, 1–12 (2021).
van Osch, M., Sep, M., van Vliet, L. M., van Dulmen, S. & Bensing, J. M. Reducing patients’ anxiety and uncertainty, and improving recall in bad news consultations. Health Psychol. 33, 1382 (2014).
Hillen, M. A. et al. All eyes on the patient: the influence of oncologists’ nonverbal communication on breast cancer patients’ trust. Breast Cancer Res. Treat. 153, 161–171 (2015).
Crichton, F. & Petrie, K. J. Health complaints and wind turbines: The efficacy of explaining the nocebo response to reduce symptom reporting. Environ. Res. 140, 449–455 (2015).
Van Vliet, L. M. et al. The validity of using analogue patients in practitioner–patient communication research: Systematic review and meta-analysis. J. Gen. Intern. Med. 27, 1528–1543 (2012).
Blanch-Hartigan, D. et al. Effects of communication about uncertainty and oncologist gender on the physician-patient relationship. Patient Educ. Couns. 102, 1613–1620 (2019).
Torensma, M. et al. How to help researchers in palliative care improve responsiveness to migrants and other underrepresented populations: Developing and testing a self-assessment instrument. BMC Palliat, Care 18, 1–11 (2019).
Van der Ploeg, H. Validity of the Zelf-Beoordelings-Vragenlijst (A Dutch version of the Spielberger State-Trait Anxiety Inventory). Ned. Tijdschr. Psychol. Grensgeb. 35, 243–249 (1980).
Scheier, M. F., Carver, C. S. & Bridges, M. W. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J. Pers. Soc. Psychol. 67, 1063 (1994).
Ong, L. M. et al. Cancer patients’ coping styles and doctor-patient communication. Psychooncology 8, 155–166. https://doi.org/10.1002/(sici)1099-1611(199903/04)8:2%3c155::aid-pon350%3e3.0.co;2-a (1999).
Henselmans, I. et al. A randomized controlled trial of a skills training for oncologists and a communication aid for patients to stimulate shared decision making about palliative systemic treatment (CHOICE): Study protocol. BMC Cancer 18, 55 (2018).
van Vliet, L. M. et al. Examining the effects of enhanced provider-patient communication on postoperative tonsillectomy pain: Protocol of a randomised controlled trial performed by nurses in daily clinical care. BMJ Open 7, e015505. https://doi.org/10.1136/bmjopen-2016-015505 (2017).
Labrie, N. et al. Effective information provision about the side effects of treatment for malignant lymphoma: Protocol of a randomized controlled trial using video vignettes. JMIR Res. Protoc. 8, e12453. https://doi.org/10.2196/12453 (2019).
von Blanckenburg, P., Schuricht, F., Albert, U.-S., Rief, W. & Nestoriuc, Y. Optimizing expectations to prevent side effects and enhance quality of life in breast cancer patients undergoing endocrine therapy: Study protocol of a randomized controlled trial. BMC Cancer 13, 426. https://doi.org/10.1186/1471-2407-13-426 (2013).
Parker, S. M. et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: Patient/caregiver preferences for the content, style, and timing of information. J. Pain Symptom Manag. 34, 81–93 (2007).
Graugaard, P. K. & Finset, A. Trait anxiety and reactions to patient-centered and doctor-centered styles of communication: An experimental study. Psychosom. Med. 62, 33–39. https://doi.org/10.1097/00006842-200001000-00005 (2000).
Wong, F. et al. Men with prostate cancer: Influence of psychological factors on informational needs and decision making. J. Psychosom. Res. 49, 13–19. https://doi.org/10.1016/s0022-3999(99)00109-9 (2000).
van Vliet, L. M. & Epstein, A. S. Current state of the art and science of patient-clinician communication in progressive disease: Patients’ need to know and need to feel known. J. Clin. Oncol. 32, 3474 (2014).
de Graaff, F. M., Francke, A. L., van den Muijsenbergh, M. E. & van der Geest, S. “Palliative care”: A contradiction in terms? A qualitative study of cancer patients with a Turkish or Moroccan background, their relatives and care providers. BMC Palliat. Care 9, 19. https://doi.org/10.1186/1472-684x-9-19 (2010).
Miller, S. M. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer 76, 167–177. https://doi.org/10.1002/1097-0142(19950715)76:2%3c167::aid-cncr2820760203%3e3.0.co;2-k (1995).
Sommer, M. et al. Prevalence and predictors of postoperative pain after ear, nose, and throat surgery. Arch. Otolaryngol. Head Neck Surg. 135, 124–130 (2009).
Hayes, A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach (Guilford Publications, 2017).
De Haes, H. & Bensing, J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Educ. Couns. 74, 287–294 (2009).
van Vliet, L. M. & Back, A. L. The different faces of empathy in cancer care: From a desired virtue to an evidence-based communication process. Cancer https://doi.org/10.1002/cncr.33833 (2021).
Peerdeman, K. J., Hinnen, C., van Vliet, L. M. & Evers, A. W. M. Pre-consultation information about one’s physician can affect trust and treatment outcome expectations. Patient Educ. Couns. 104, 427–431. https://doi.org/10.1016/j.pec.2020.07.021 (2021).
Visser, L. N. C., Tollenaar, M. S., van Doornen, L. J. P., de Haes, H. & Smets, E. M. A. Does silence speak louder than words? The impact of oncologists’ emotion-oriented communication on analogue patients’ information recall and emotional stress. Patient Educ. Couns. 102, 43–52. https://doi.org/10.1016/j.pec.2018.08.032 (2019).
Gaab, J., Kossowsky, J., Ehlert, U. & Locher, C. Effects and components of placebos with a psychological treatment rationale–three randomized-controlled studies. Sci. Rep. 9, 1–8 (2019).
Verheul, W., Sanders, A. & Bensing, J. The effects of physicians’ affect-oriented communication style and raising expectations on analogue patients’ anxiety, affect and expectancies. Patient Educ. Couns. 80, 300–306 (2010).
Devlin, E. J., Denson, L. A. & Whitford, H. S. Cancer treatment side effects: A meta-analysis of the relationship between response expectancies and experience. J. Pain Symptom Manag. 54, 245-258.e242 (2017).
Fletcher, C., Wilson, C., Hutchinson, A. D. & Grunfeld, E. A. The relationship between anticipated response and subsequent experience of cancer treatment-related side effects: A meta-analysis comparing effects before and after treatment exposure. Cancer Treat. Rev. 68, 86–93 (2018).
Sep, M. S., van Osch, M., van Vliet, L. M., Smets, E. M. & Bensing, J. M. The power of clinicians’ affective communication: How reassurance about non-abandonment can reduce patients’ physiological arousal and increase information recall in bad news consultations. An experimental study using analogue patients. Patient Educ. Couns. 95, 45–52. https://doi.org/10.1016/j.pec.2013.12.022 (2014).
Westendorp, J. et al. The power of clinician-expressed empathy to increase information recall in advanced breast cancer care: An observational study in clinical care, exploring the mediating role of anxiety. Patient Educ. Couns. 104, 1109–1115 (2021).
Kern, A., Kramm, C., Witt, C. M. & Barth, J. The influence of personality traits on the placebo/nocebo response: A systematic review. J. Psychosom. Res. 128, 109866 (2020).
Feldhaus, M. H., Horing, B., Sprenger, C. & Büchel, C. Association of nocebo hyperalgesia and basic somatosensory characteristics in a large cohort. Sci. Rep. 11, 1–12 (2021).
Kim, Y., Yen, I. H. & Rabow, M. W. Comparing symptom burden in patients with metastatic and nonmetastatic cancer. J. Palliat. Med. 19, 64–68 (2016).
Smith, Z. L., Eggener, S. E. & Murphy, A. B. African–American prostate cancer disparities. Curr. Urol. Rep. 18, 1–10 (2017).
Lelorain, S., Brédart, A., Dolbeault, S. & Sultan, S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology 21, 1255–1264 (2012).
Roberts, B. W., Puri, N. K., Trzeciak, C. J., Mazzarelli, A. J. & Trzeciak, S. Socioeconomic, racial and ethnic differences in patient experience of clinician empathy: Results of a systematic review and meta-analysis. PLoS ONE 16, e0247259 (2021).
Ferguson, W. J. & Candib, L. M. Culture, language, and the doctor-patient relationship. FMCH Public. Present. 61 (2002).
CBS. Internet; toegang, gebruik en faciliteiten; 2012–2019. https://www.cbs.nl/nl-nl/cijfers/detail/83429NED (reviewed on 07-09-2021).
Acknowledgements
We would like to thank the expert panel for their help in the development of the videos. We are grateful to the following patient organizations for their help with recruitment: Dutch Breast Cancer Society (BVN), Dutch Federation of Cancer Patients Organisations (NFK), Head-Neck Patient Organisation (PVHH), Lung Cancer Netherlands (Longkanker NL), hemato-oncological Patient Organisation (Hematon), Mammarosa foundation, Network of Organisations of Elder Migrants (NOOM), the Netherlands Comprehensive Cancer Organisation (IKNL), cancer.nl (kanker.nl), Foundation for Optimal Support for Cancer (Stichting OOK), Pink Ribbon, Psycho-oncological centre ‘Het Behouden Huys’, Pain by Cancer foundation (Stichting Pijn bij Kanker), IPSO (Institutes for Psychosocial Oncology).
Funding
The project was funded by a Young Investigator Grant of the Dutch Cancer Society (number 10392, 02/04/2016), awarded to LV.
Author information
Authors and Affiliations
Contributions
M.M.: script-and-video development, data collection, data analyses, writing—original draft. E.D.: script-and-video development, data collection, data analyses, writing—review and editing. S.J.: script-and-video development, data collection, data analyses, writing—review and editing. J.S., A.E., H.D., A.F., N.P., E.W., Y.N.: script-and-video development, writing—review and editing. E.D.: data analysis, interpretation results. L.V. conceptualization, script-and-video development, data collection, data analyses, writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained errors in the dataset. Modifications have been made to the Abstract, Table 3, Table 4 and the Results section. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meijers, M.C., Stouthard, J., Evers, A.W.M. et al. Possible alleviation of symptoms and side effects through clinicians’ nocebo information and empathy in an experimental video vignette study. Sci Rep 12, 16112 (2022). https://doi.org/10.1038/s41598-022-19729-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19729-w
- Springer Nature Limited
This article is cited by
-
The influence of written medication reminder on patient experience among older adult patients: a repeat cross-sectional study
BMC Geriatrics (2024)
-
Identifying the psychological effects of nocebo education: results from two pre-registered experiments
Journal of Behavioral Medicine (2024)