Abstract
Cannabis is the main illicit psychoactive substance used by pregnant women in France. The aim of the present national survey was to describe adverse events (AEs) of recreational cannabis use during pregnancy reported to the French Addictovigilance Network (FAN). Spontaneous reports (SRs) of AEs related to recreational cannabis use during pregnancy were collected by the FAN between 01/01/2011 and 31/01/2021 (excluding cannabidiol and synthetic cannabinoids). Over the study period, 160 SRs involved cannabis use alone or in association with tobacco (59% of all SRs) which increased. Among the 175 maternal AEs, the most commons were psychiatric AEs experienced by 96 (64.9%) women, in particular cannabis use disorders (n = 89, 60.1%), dependence (n = 54, 36.5%) and abuse (n = 21, 14.2%). Among the 57 fetal AEs, the most common were heart rhythm disorders that affected 25 (16.9%) fetuses and intrauterine growth restriction (IUGR) (n = 20, 13.5%). Among the 140 neonatal AEs, the most common were IUGR experienced by 39 (26.3%) newborns and prematurity (n = 32, 21.6%). Twelve cases of congenital malformations were observed and 4 intrauterine/neonatal deaths. Furthermore, some of these AEs (n = 13) were unexpected. Cannabis use during pregnancy has problematic consequences for both mothers and infants who need close monitoring.
Similar content being viewed by others
Introduction
Cannabis is the main illicit psychoactive substance used by women of childbearing age in France. In 2017, 4% of women aged 18 to 34 years reported consuming cannabis at least ten times a month1.
Cannabis contains over 120 cannabinoids, the best characterized is delta-9-tetrahydrocannabinol (THC). THC crosses the placenta during the embryonic and fetal periods but there is still scarce knowledge about the pharmacokinetic properties of cannabis during pregnancy. Its distribution in the fetal compartment has not yet been studied. It is detected in meconium, urine and hair of infants exposed in utero. Blackard et al. measured THC and 9-carboxy-THC simultaneous in cord blood and maternal blood and showed concentrations in cord blood 3 and 6 times lower than in the maternal blood2. Furthermore, Boskovic et al. measured different THC content in the meconium and the hair of dizygotic twins, which suggested that some fetal and placental factors may modulate the fetal exposure3.
Very few data on the prevalence of cannabis use and its complications are available in France. According to the last national perinatal survey 2016, 2.1% of women interviewed in postpartum care reported using cannabis during pregnancy, almost half more than three times a month4. Furthermore, the French pharmaco-epidemiological survey OPPIDUM (Observation of illegal drugs and misuse of psychotropic medications) showed a significant rise in cannabis consumption among pregnant women seen in specialized addiction care centers from 1.2% in 2005–2006 to 17.8% in 2017–20185.
In France, the potential for abuse and dependence of psychoactive substances is assessed by the French Addictovigilance Network (FAN) in collaboration with the National Agency for the Safety of Medicines and Health Products (Agence Nationale de Sécurité du Médicament et des Produits de Santé). This surveillance system regulated by law is based on spontaneous reporting by healthcare professionals, collaborators and patients completed by specific pharmaco-epidemiological surveillance programs6,7,8.
A previous national survey showed a wide variety of adverse events (AEs) of recreational cannabis use reported to the FAN over the period 2012–2017, including some perinatal AEs (n = 55, 1.7% of all AEs). They were mainly dependence (21.8% of the perinatal AEs), IUGR (21.8% of the perinatal AEs), prematurity/premature rupture of membranes (n = 7, 12.7% of perinatal AEs)9. Five of them were unexpected: three cases of congenital malformations (cardiopathy, horse kidney and duodenal atresia), one case of oligohydramnios and one case of bartholinitis9. Given the recent increase in Addictovigilance signals, an overview was necessary.
The aim of the present national survey was to described AEs of recreational cannabis use during pregnancy by exploring cases reported to the FAN the ten last years.
Methods
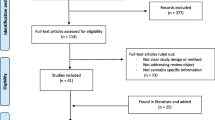
According to French law, any serious cases of abuse and dependence involving psychoactive substances (with the exception of alcohol and tobacco) must be reported by health professionals to the FAN. The FAN consists of 13 addictovigilance centers implemented in university hospital throughout France. Practitioners from the FAN are pharmacologists who answer to health professionals about the risks of psychoactive substances use, who investigate spontaneous reports (SRs) to complete and analyze them in order to identify or confirm public health signals. After their analysis, SRs are recorded over time in the addictovigilance database by respecting the anonymity of the patients and the notifiers.
We identified all SRs of AEs related to recreational cannabis use during pregnancy collected by the FAN between January 1, 2011 and January 31, 2021 (excluding cannabidiol and synthetic cannabinoids).
All cases were reviewed by an expert pharmacologist. The addictovigilance database was approved by the French Data Protection Agency (CNIL), and data were recorded anonymously, therefore there was no direct clinical responsibility for patients, no required informed consent and no research ethics committee approval.
Events were classified in three categories: maternal, fetal and neonatal events. They were coded using the Medical Dictionary for Regulatory Activities (MedDRA).
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Classification of Diseases and Related Health Problems (ICD-10), abuse was defined as an excessive and intentional use, occasional or persistent with harmful physical and/or psychological effects and dependence as a craving, an inability to reduce or control cannabis use despite health problems caused by its use, a withdrawal syndrome, a phenomenon of tolerance resulting in a consumption of larger amounts that were intended or spending a lot of time to get, use or recover from effects10,11. In mid-2013, DSM-V replaced DSM-IV and abuse and dependence were combined under the terminology cannabis use disorders12. Thus, the coded terms were abuse and dependence until mid-2013, and then cannabis use disorders.
Problematic use was defined by a punctual, regular or chronic use resulting in negative medical and social consequences. It differs from abuse because there is not necessary excessive consumption.
Intrauterine growth restriction was defined as a birth weight for gestational age less than the 10th percentile.
Events were considered unexpected if they had been described in the literature only rarely or not at all.
Exposures were classified in three categories: during the first, the second and the third trimester of pregnancy. When consumption was related in number of joints or number of times a day during pregnancy, it was considered that cannabis was consumed throughout pregnancy.
In some cases, toxicological tests were performed in the context of medical care.
The analysis of congenital malformations focused on cases exposed to cannabis at least in the first trimester of pregnancy. The analysis of neonatal withdrawal syndromes focused on cases exposed to cannabis at least in the third trimester of pregnancy.
To describe the evolution of reports, the percentage of all SRs on cannabis use during pregnancy among the total number of national SRs was calculated for each year. The rate of reported cases per 100,000 live births was estimated using the French national institute of statistics and economic studies (Institut National de la Statistique et des Etudes Economiques—INSEE) data on live births13.
The characteristics of cannabis pregnant users, cannabis use during pregnancy and the main AEs were described and then compared between two groups exposed to “cannabis alone or in association with tobacco” and “cannabis and others psychoactive substances/medicinal products”. The means and frequencies were reported for quantitative and qualitative variables, respectively. Chi-square test and Student test were performed to compare the two groups when relevant, using the statistical software R (version 3.6.2, R Core Team, 2019).
To assess AEs related to cannabis use during pregnancy, we focused only on cases involving cannabis alone or in association with tobacco due to their frequent concomitant use. Those involving concomitant use of alcohol, other substances or drugs such as cocaine or methadone were excluded because of the risk of bias related to their use.
Results
Characteristics of SRs
A total of 271 SRs of one or more events involving cannabis use during pregnancy were included in the study. They occurred in 242 pregnancies, some of them concerning both the mother and the fetus and/or the newborn. The proportion of SRs involving cannabis use during pregnancy represented a small proportion of the total national SRs. It significantly increased from 0.16% in 2011 to 1.10% in 2020 (p < 0.001). This corresponds to a notified rate multiplied by 7 whereas the total national number of SRs increased by around 2.5-fold over the same period (data not shown). The estimated reporting rate of SRs related to cannabis use during pregnancy per 100,000 live births increased from 0.49 reports per 100,000 live births in 2011 to 8.38 reports per 100,000 live births (p < 0.0001).
Characteristics of pregnant women
The mean age of pregnant women was 27.8 years (range 16–44 years) and three were minors. A history of substance abuse was reported in 59.5% of them and a psychiatric history in 27.7% of them (Table 1).
The characteristics of pregnant women who reported cannabis use alone or in association with tobacco were different from those who used cannabis and other psychoactive substances/medicinal products: they were younger (mean age: 26.6 versus 30.2 years, p < 0.001) and had fewer psychiatric history (21.6% versus 37.2%, p = 0.01).
Characteristics of cannabis use during pregnancy
Table 2 shows the characteristics of cannabis use during pregnancy. When the route of administration was specified, it was always inhaled (59.9%) (Table 2). Cannabis use in the first trimester of pregnancy was chronic in 64.5% of cases (daily in 58.3% of cases and greater than ten times a day in 9.5% of cases). Pregnant women who used cannabis alone or in association with tobacco reported more frequently a chronic use in the first trimester of pregnancy (69.6% versus 56.4% among those who reported cannabis and other substances/medicinal products use), in particular a daily use (63.5% versus 50.0% among those who reported cannabis and other substances/medicinal products use, p = 0.04) (Table 2).
Few pregnant women (6.2%) stopped consuming cannabis during pregnancy (2.5% in the first trimester, 1.2% in the second trimester and 2.1% in the third trimester). A decrease in cannabis use was reported by 10.3% of them and an increase in cannabis use by 1.2% of them (Table 2).
A concomitant use of tobacco was reported in 47.1% of cases in the first trimester, in 46.5% of cases in the second trimester and in 45.2% of cases in the third trimester (Table 2). A concomitant use of alcohol was mentioned in 12.4% of cases in the first trimester, in 8.7% of cases in the second trimester and in 7.5% of cases in the third trimester. Concomitant uses of other psychoactive substances were mainly cocaine (12.8% in the first trimester, 9.1% in the second trimester, 9.5% in the third trimester) and heroin (5% in the first trimester, 5.8% in the second trimester and 4.6% in the third trimesters). Concomitant uses of medicinal products were mainly opioid substitution treatments (13.6% in the first trimester, 14.1% in the second trimester, 13.7% in the third trimester), in particular methadone (9.9% in the first trimester, 10% in the second trimester, 9.5% in the third trimester). Benzodiazepines and benzodiazepine-like agents were placed in second position (9.1% in the first and second trimesters, 10% in the third trimester) and then antipsychotics (2.5% in the first and second trimesters, 2.9% in the third trimester), serotonin reuptake inhibitors (2.1% in the first trimester, 1.7% in the second and third trimesters) and anticonvulsants (1.2% in the first trimester, 0.8% in the second and third trimesters) (data not shown).
In 35 (14.5%) of cases, a toxicological test was positive for cannabis in the pregnant women or newborns. They were less frequent in women who reported cannabis use alone or in association with tobacco than in those who reported cannabis and other substances/medicinal products use (Table 2).
Among the 38 pregnant women (15.7%) who described the reasons for their cannabis consumption, 28 (73.7%) indicated consuming it for its anxiolytic/sedative effects, 4 (10.5%) for occupational effects, 3 (7.9%) ex-aequo for hypnotic effects, disinhibition, pleasure, motivation help, recreational use, as a substitute of alcohol and 2 (5.3%) for its anti-emetic effect (data not shown).
Adverse events related to cannabis use alone or in association with tobacco
Over the study period, 160 of the 271 SRs involved cannabis use alone or in association with tobacco and they concerned 148 pregnancies (Table 3).
The number of maternal AEs (n = 175) related to cannabis use alone or in association with tobacco increased significantly from 0 in 2011 to 5 (2.9% of AEs, 95% CI 0.4–5.3%) in 2012 and 25 (13.7%, 95% CI 8.6–18.8%) in 2020 (data not shown). Some of them were AEs usually described in cannabis users. Women who reported cannabis use alone or in association with tobacco presented more frequently psychiatric AEs than those who reported cannabis and other psychoactive substances/medicinal products use (n = 96, 64.9% versus n = 44, 46.8%, p = 0.006) (Table 3). They experienced cannabis use disorders (n = 89, 60.1%), dependence (n = 54, 36.5%), abuse (n = 21, 14.2%) and problematic use (n = 6, 4.0%) (Table 3). Furthermore, five women (3.4%) suffered from cannabinoid hyperemesis syndrome (Table S1). The other most common AEs were threat of premature membranes that were experienced by 13 (8.8%) women and premature rupture of membranes experienced by 12 (8.1%) women (Table 3).
Some women presented unexpected AEs (n = 8, 5.4%): anhydramnios/oligohydramnios (n = 6, 4.0%), preeclampsia (n = 1, 0.7%) and bartholinitis (n = 1, 0.7%) (Table S1).
The number of fetal AEs (n = 57) related to cannabis use alone or in association with tobacco significantly increased from 0 in 2011 to 1 in 2012, 5 (8.8%, 95% CI 1.4–16.1) in 2015 and 23 (40.3%, 95% CI 27.6–53.1) in 2020. Fetus presented most often heart rhythm disorders (n = 25, 16.9%), IUGR (n = 20, 13.5%), congenital malformations diagnosed prenatally (n = 8, 5.4%), and two (1.3%) intrauterine fetal deaths (Table S1).
The number of neonatal AEs (n = 140) related to cannabis use alone or in association with tobacco significantly increased from 0 in 2011 to 4 (2.8%, 95% CI 0.1–5.6) in 2012 and 55 (39.3%, 95% CI 31.2–47.4) in 2020. Infants presented mainly IUGR (n = 39, 26.3%, some of them diagnosed prenatally), prematurity (n = 32, 21.6%), Apgar score ≤ 7 at 1 min (n = 11, 7.4%), withdrawal syndromes (n = 11, 7.4%), congenital malformations (n = 9, 6.1%) and respiratory failure (n = 7, 4.7%). Fifteen newborns (10.1%) were admitted in intensive care. Furthermore, two (1.3%) neonatal deaths were reported in very preterm infants: in one case it was a twin pregnancy and the cause of death was unknown, in the other case, the newborn had intraventricular hemorrhage, leukomalacia, obstructive hydrocephalus, pulmonary arterial hypertension, acute renal failure, congenital malformation to type of arthrogyrosis, inches of bilateral adductus, low set ears, hypospadias in a context of prolonged anhydramnios and he died on the eighth day of life (Table S1). Some infants presented unexpected AEs (n = 5, 3.4%): sacrococcygeal teratoma (n = 1, 0.7%), crossed renal ectopia (n = 1, 0.7%), horseshoe kidney (n = 1, 0.7%), duodenal atresia (n = 1, 0.7%) and hypospadias (n = 1, 0.7%).
Focus on congenital malformations
Twelves of the nineteen cases of congenital malformations occurred in fetuses/newborns whose mothers reported cannabis use alone or in association with tobacco (8.1% of pregnancies). They were limb malformations (n = 4, arthrogyrosis, inches of bilateral adductus in a context of anhydramnios, bilateral equine varus feet, short femur), microcephaly (n = 3, including one case with dolicocephalia), kidney malformations (n = 2, crossed renal ectopia, horseshoe kidney), congenital malformation of the face (n = 2, low set ears, philtrum elongated with thin upper lip and small chin), hypospadias (n = 1), sacrococcygeal teratoma (n = 1), cardiopathy (n = 1), omphalocele (n = 1) and duodenal atresia (n = 1) (Table 4).
Maternal age was less than 35 years old in 8 cases (66.7%). Cannabis was consumed during the whole pregnancy, most often regularly (when this data was available), nevertheless in two cases it was punctual (data not shown). Congenital malformations were associated with IUGR in 6 cases (4.0% of pregnancies exposed to cannabis alone or in association with tobacco), and with anhydramnios/oligohydramnios in 3 cases (2% of pregnancies exposed to cannabis alone or in association with tobacco). In most of the cases, several congenital anomalies were present without however being able to define a specific pattern of malformation (Table 4).
Discussion
The proportion of SRs involving cannabis use during pregnancy reported to the FAN was low and represented a small proportion of the total national SRs. It increased sevenfold between 2010 and 2020 whereas the total national number of SRs increased by around 2.5-fold over the same period and the reporting rate in France of all AEs related to cannabis use alone or in association with tobacco and/or alcohol tripled between 2012 and 20179. This increase may result from a rise in the prevalence of cannabis use during pregnancy, from a normalization of cannabis use leading pregnant women to confess it or because pregnant women were more likely to be questioning about their cannabis use.
The characteristics of women who used cannabis alone or in association with tobacco were different from those who were poly-consumers of psychoactive substances because they were younger, had less psychiatric history and reported more frequently chronic cannabis use.
The maternal events related to cannabis use alone or in association with tobacco were in the first place psychiatric, in particular use disorders and dependence, which is consistent with previous results observed more generally in cannabis users9. These conditions may complicate the management of the pregnancy, in particular in women with past-history of sustained daily cannabis use. Furthermore, nine maternal AEs were unexpected such as anhydramnios/oligohydramnios, pre-eclampsia/eclampsia and bartholinitis. The last two cases have always been mentioned in our previous study9.
Fetal events related to cannabis use alone or in association with tobacco were mainly fetal heart rhythm disorders, intrauterine growth restriction and congenital malformations diagnosed prenatally. It is also noteworthy that two cases of intrauterine fetal deaths were also reported.
Neonatal events related to cannabis use alone or in association with tobacco were mainly intrauterine growth restriction and prematurity, which was expected. A previous study more than ten years ago had shown an increased risk of growth restriction in infants whose mothers used cannabis during pregnancy compared with those whose mothers smoked tobacco14 and an increased risk of preterm birth in pregnant women who used cannabis, notably among those who also smoke tobacco15. Other frequent effects were Apgar score ≤ 7 at 1 min, withdrawal syndromes, congenital malformations and respiratory failure. Five AEs were unexpected such as sacrococcygeal teratoma, crossed renal ectopia, horseshoe kidney, duodenal atresia and hypospadias and three of them have always been described in our previous study9. In most of cases, several congenital malformations were associated without being able to define a specific pattern of malformation. Furthermore, two neonatal deaths were reported in very preterm infants.
France is the only European country with a national specifically proactive addictovigilance surveillance system to evaluate the potential of abuse and dependence of psychoactive substances. The present study is the first to give a national overview of AEs related to recreational cannabis use alone or in association with tobacco during pregnancy these ten last years. The choice of excluding cases related to cannabis use in association with other substances was intended to provide an overall description of the potential events related only to the use of cannabis frequently associated with tobacco smoking during pregnancy.
This study based on spontaneous reporting is subject to underreporting16. Furthermore, cannabis use during pregnancy is frequently underreported by pregnant women due to the stigma associated with it. Consequently, these findings do not reflect all AEs related to cannabis use during pregnancy in general population. It cannot be excluded that birth anomalies were likely to reflect differential reporting of cannabis use in women whose infant suffered from them. But these results provide hypotheses that need to be tested in large representative samples of women who have been asked about their cannabis use before birth and confirmed by biomarkers of cannabis use. In addition, one addictovigilance center collected nearly 40% of SRs resulting from hospital consultations specialized in addictology that is likely to induce a bias in the severity of the effects. Pregnant women were more likely to be questioning by these practitioners about their cannabis use and to report it, which in turn can increase the risk of reporting bias, thus making it difficult to interpret the increased reporting of AEs. This analysis of SRs did not allow to compare cases to those that occurred in pregnant women not exposed to cannabis so that causality could not be assessed. Unfortunately, some of the data that were collected from spontaneous notifications were likely to be missing and tobacco use was not always provided.
The endocannabinoid system is involved in different stages of reproduction and for early pregnancy and maintenance17. Thus an imbalance secondary to the use of cannabis at key moments is likely to induce deleterious effects. Moreover, the mean THC content of cannabis products has increased over the past 10 years worldwide18,19. In France, it rose for cannabis resin from 10% in 2009 to 28% in 2019 and for herbal cannabis, it maintained around 12% in 2019 compared to 7% in 200918,20. This may result in an increased in utero exposure to THC and risk of AEs.
When women reported consuming cannabis alone, it was difficult to absolutely exclude the role of tobacco due to the frequent concomitant use, notably by inhalation. Tobacco is also known to induce perinatal adverse effects, notably preterm births and intrauterine growth restriction with a dose–response effect21,22,23. Kyrklund-Blomberg et al. reported an increased risk of prematurity by 1.2 [1.1–1.2] among pregnant women smoking 1 to 9 cigarettes/day and by 1.4 [1.3–1.5] among those smoking more than 10 cigarettes/day compared to nonsmoker pregnant women21. Another retrospective study showed an increased risk of prematurity by 1.41 [1.37–1.44] among cigarettes smoking pregnant women22. According to a meta-analysis of 210 studies, the rate of small for gestational age was nearly twice in cigarette smoking pregnant women (pooled aOR 1.95 [1.76–2.16]), the rate of shorter length was lower (pooled mean difference = 0.43 [0.41–0.44]), as well as smaller head circumference (pooled mean difference = 0.27 [0.25–0.29])23. Maternal smoking appears to be associated with a lower risk of preeclampsia. A meta-analysis of 70 prospective studies reported that smoking pregnant women was inversely associated with the incidence of preeclampsia (RR = 0.67 [0.60–0.75])24. However, co-use of cannabis and tobacco seems to be associated with an increased risk of preeclampsia25. Furthermore, Shobeiri et al. showed that smoking during pregnancy was associated with a higher risk of placenta previa (OR 1.42 [1.30–1.54], RR = 1.27 [1.18–1.35])26.
Nevertheless, experimental data are particularly interesting because they allow to overcome biases observed in clinical studies and to analyze the effects of cannabis and/or THC alone. They have shown that cannabis and THC exposure during gestation resulted in reduced birth weight and increased embryonic and fetal mortality27,28. This may be explained by the role of cannabis on placental insufficiency29, lower placental GLUT1 expression that may decrease the availability of glucose which is the primarily energy source for the fetus27. Furthermore, THC reduces the invasion of extravillous trophoblasts in vitro HTR-8/SV neo cells in a spheroid invasion model30,31, which suggests its role in the occurrence of preeclampsia.
Regarding the six cases of anhydramnios/oligohydramnios, one had no other contributing factor than a chronic cannabis use (6 joints/day at the beginning of the pregnancy reduced at 3 joints/day). For the five other cases, premature rupture of membranes, intra-uterine growth restriction and renal congenital malformation were also present.
Indeed, in published studies about the risk of congenital malformations, it was very often difficult to ruled out the role of concomitant substances32. Cases reported in this study did not allow to conclude to an increased risk, but some of them were unexpected (sacrococcygeal teratoma, crossed renal ectopia, horseshoe kidney, duodenal atresia and hypospadias). To date no increased risk is retained for tobacco, even if a weak association is discussed for specific malformations such as facial clefts, musculoskeletal defects, limb reduction, malposition of the foot, gastrointestinal defects and cardiopathies33. However, experimental studies have shown epigenetic disruptions related to cannabis exposure during pregnancy28,34. Moreover, chronic THC exposure may decrease the level of plasma folic acid, which plays an important role in preventing congenital malformation, in particular neural tube defects but also cardiac malformations, urinary tract anomalies, oro-facial clefts and limb reductions35. Animal studies on teratogen risk showed congenital anomalies (limb and extremity defects, encephalocele, eventration of abdominal visceral) in 57% of descendants of pregnant rats exposed to intraperitoneal emulsion of resin (4.2 mg/kg/day from day 1 to day 6 of gestation)36 but they have not been confirmed later37,38.
Conclusion
Cannabis use during pregnancy, alone or in association with tobacco, has problematic consequences for both mothers and children who need close monitoring. Some of the reported events in this study were unexpected, such as anhydramnios/oligohydramnios, preeclampsia, bartholinitis and some congenital malformations (sacrococcygeal teratoma, crossed renal ectopia, horseshoe kidney, duodenal atresia and hypospadias). Even if the risks of smoking during pregnancy are serious, they are well-documented for tobacco much less for cannabis. Interestingly, experimental studies have showed effects of cannabis and/or THC alone on fetal growth and mortality as well as on epigenetic disruption and decreased levels of folic acid.
In our study, few women have discontinued their cannabis use during pregnancy. In the light of the normalization of recreational cannabis use, it seems therefore important to inform women of childbearing age, pregnant women, health professionals and policy makers about the deleterious effects of exposure to cannabis during pregnancy.
Data availability
The datasets generated or analyzed during the current study are not publicly available due to restrictions. According to the French Laws (Articles R.5132-113, R5132-114) each case was recorded in the French Addictovigilance database, in an anonymous format and are under the authority of the French National Agency for Medicines and Health Products Safety (ANSM). The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
References
Observatoire Français des Drogues et Toxicomanies. Santé Publique France. Les niveaux d’usages des drogues illicites en France en 2017, Tendances 128, Novembre 2018. https://www.ofdt.fr/publications/collections/periodiques/lettre-tendances/les-niveaux-dusages-des-drogues-illicites-en-france-en-2017-tendances-128-novembre-2018/. Accessed 3 December 2021. (2018).
Blackard, C. & Tennes, K. Human placental transfer of cannabinoids. N. Engl. J. Med. 311, 797. https://doi.org/10.1056/NEJM198409203111213 (1984).
Boskovic, R., Klein, J., Woodland, C., Karaskov, T. & Koren, G. The role of the placenta in variability of fetal exposure to cocaine and cannabinoids: A twin study. Can. J. Physiol. Pharmacol. 79, 942–945 (2001).
Institut National de la Santé et de la Recherche Médicale – Direction de la Recherche, des Etudes, de l’Evaluation et des Statistiques. Enquête Nationale Périnatale. Rapport 2016. Les naissances et les Etablissements. Situation et Evolution Depuis 2010. http://www.xn--epop-inserm-ebb.fr/wp-content/uploads/2017/10/ENP2016_synthese_rapport.pdf. Accessed 5 November 2021. (2017).
Blayac, L., Micallef, J. & Lapeyre-Mestre, M. Evolution des comportements de consommation de produits psychoactifs illicites ou détournés de leur usage médicamenteux chez les femmes enceintes en France: Analyse des données OPPIDUM de 2005 à 2018. Therapies 76, 169 (2021).
Légifrance. Décret n°99–249 du 31 mars 1999 relatif aux substances vénéneuses et à l’organisation de l’évaluation de la pharmacodépendance, modifiant le code de la santé publique (deuxième partie: Décrets en Conseil d’Etat). https://www.legifrance.gouv.fr/loda/id/JORFTEXT000000393106/. Accessed 5 November 2021. (1999).
Jouanjus, E., Gibaja, V., Kahn, J. P., Haramburu, F. & Daveluy, A. Signal identification in addictovigilance: The functioning of the French system. Therapies 70, 113–131. https://doi.org/10.2515/therapie/2015011 (2015).
Micallef, J. & Mallaret, M. Twenty-five years of the French Addictovigilance Network (FAN). Therapies 71, 375–378. https://doi.org/10.1016/j.therap.2016.05.001 (2016).
Bouquet, E. et al. Adverse events of recreational cannabis use reported to the French Addictovigilance Network (2012–2017). Br. J. Clin. Pharmacol. 87, 3925–3927. https://doi.org/10.1111/bcp.14812 (2021).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th edn. (APA, 1994).
World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. https://apps.who.int/iris/handle/10665/37958. Accessed 17 June 2021. (1992)
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn. (APA, 2013).
Institut National de la Statistique et des Etudes Economiques. Naissances et taux de Natalité—Données annuelles de 1982 à 2020. https://www.insee.fr/fr/statistiques/2381380#tableau-figure1. Accessed 17 June 2021. (2021).
El Marroun, H. et al. Intrauterine cannabis exposure affects fetal growth trajectories: The Generation R Study. J. Am. Acad. Child Adolesc. Psychiatry 48, 1173–1181. https://doi.org/10.1097/CHI.0b013e3181bfa8ee (2009).
Saurel-Cubizolles, M. J., Prunet, C. & Blondel, B. Cannabis use during pregnancy in France in 2010. BJOG 121, 971–977. https://doi.org/10.1111/1471-0528.12626 (2014).
Jouanjus, E., Pourcel, L., Saivin, S., Molinier, L. & Lapeyre-Mestre, M. Use of multiple sources and capture-recapture method to estimate the frequency of hospitalizations related to drug abuse. Pharmacoepidemiol. Drug Saf. 21, 733–741. https://doi.org/10.1002/pds.3280 (2012).
Kozakiewicz, M. L., Grotegut, C. A. & Howlett, A. C. Endocannabinoid system in pregnancy maintenance and labor: A mini-review. Front. Endocrinol. 12, 699951. https://doi.org/10.3389/fendo.2021.699951 (2021).
Dujourdy, L. & Besacier, F. A study of cannabis potency in France over a 25 years period (1992–2016). Forensic Sci. Int. 272, 72–80. https://doi.org/10.1016/j.forsciint.2017.01.007 (2017).
World Health Organization. Expert Committee on Drug Dependence Pre-review. Cannabis Plant and Cannabis Resin. Section 5: Epidemiology. https://www.who.int/medicines/access/controlled-substances/Section5.CannabisPlant.Epidemiology.pdf?ua=1. Accessed 5 November 2021. (2018).
Gérome, C. & Gandilhon, M. Psychoactive Substances, Users and Markets. Recent Trends (2019–2020). Bulletin TREND. OFDT. https://en.ofdt.fr/publications/tendances/psychoactive-substances-users-and-markets-recent-trends-2019-2020-tendances-141-december-2020/. Accessed 5 November 2021. (2020).
Kyrklund-Blomberg, N. B. & Cnattingius, S. Preterm birth and maternal smoking: Risks related to gestational age and onset of delivery. Am. J. Obstet. Gynecol. 179, 1051–1055. https://doi.org/10.1016/s0002-9378(98)70214-5 (1998).
Lawder, R., Whyte, B., Wood, R., Fischbacher, C. & Tappin, D. M. Impact of maternal smoking on early childhood health: A retrospective cohort linked dataset analysis of 697 003 children bom in Scotland 1997–2009. BMJ 9, e023213 (2019).
Quelhas, D. et al. The association between active tobacco use during pregnancy and growth outcomes of children under five years of age: A systematic review and meta-analysis. BMC Public Health 18, 1372. https://doi.org/10.1186/s12889-018-6137-7 (2018).
Wei, J., Liu, C. X., Gong, T. T., Wu, Q. J. & Wu, L. Cigarette smoking during pregnancy and preeclampsia risk: A systematic review and meta-analysis of prospective studies. Oncotarget 6, 43667–43678 (2015).
Cajachagua-Torres, K. N., El Marroun, H., Reiss, I. K. M. & Jaddoe, V. W. V. Maternal preconception and pregnancy tobacco and cannabis use in relation to placental developmental markers: A population-based study. Reprod. Toxicol. 1, 70–77. https://doi.org/10.1016/j.reprotox.2022.03.015 (2022).
Shobeiri, F. & Jenabi, E. Smoking and placenta previa: A meta-analysis. J. Matern Fetal Neonatal Med. 30, 2985–2990 (2017).
Natale, B. V. et al. Δ9-tetrahydrocannabinol exposure during rat pregnancy leads to symmetrical fetal growth restriction and labyrinth-specific vascular defects in the placenta. Sci. Rep. 10, 544. https://doi.org/10.1038/s41598-019-57318-6 (2020).
Zumbrun, E. E., Sido, J. M., Nagarkatti, P. S. & Nagarkatti, M. Epigenetic regulation of immunological alterations following prenatal exposure to marijuana cannabinoids and its long term consequences in offspring. J. Neuroimmune Pharmacol. 10, 245–254. https://doi.org/10.1007/s11481-015-9586-0 (2015).
Benevenuto, S. G. et al. Recreational use of marijuana during pregnancy and negative gestational and fetal outcomes: An experimental study in mice. Toxicology 376, 94–101. https://doi.org/10.1016/j.tox.2016.05.020 (2017).
Meakin, C., Barrett, E. S. & Aleksunes, L. M. Extravillous trophoblast migration and invasion: Impact of environmental chemicals and pharmaceuticals. Reprod. Toxicol. 107, 60–68 (2022).
Wong, M. K., Wahed, M., Shawky, S. A., Dvorkin-Gheva, A. & Raha, S. Transcriptomic and functional analyses of 3D placental extravillous trophoblast spheroids. Sci. Rep. 9, 12607 (2019).
Corsi, D. J. The potential association between prenatal cannabis use and congenital anomalies. J. Addict. Med. 14, 451–453 (2020).
Hackshaw, A., Rodeck, C. & Boniface, S. Maternal smoking in pregnancy and birth defects: A systematic review based on 173 687 malformed cases and 11.7 million controls. Hum. Reprod. Update 17, 589–604. https://doi.org/10.1093/humupd/dmr022 (2011).
DiNieri, J. A. et al. Maternal cannabis use alters ventral striatal dopamine D2 gene regulation in the offspring. Biol. Psychiatry 70, 763–769. https://doi.org/10.1016/j.biopsych.2011.06.027 (2011).
Araújo, J. R., Gonçalves, P. & Martel, F. Effect of cannabinoids upon the uptake of folic acid by BeWo cells. Pharmacology 83, 70–76. https://doi.org/10.1159/000192587 (2009).
Persaud, T. V. & Ellington, A. C. Teratogenic activity of cannabis resin. Lancet 2, 406–407. https://doi.org/10.1016/s0140-6736(68)90626-0 (1968).
Gianutsos, G. & Abbatiello, E. R. The effect of pre-natal Cannabis sativa on maze learning ability in the rat. Psychopharmacologia 27, 117–122. https://doi.org/10.1007/BF00439370 (1972).
Martin, P. A. Cannabis and chromosomes. Lancet 1, 370 (1969).
Author information
Authors and Affiliations
Consortia
Contributions
This study was conducted in the context of a national Addictovigilance follow-up for which the Addictovigilance center of Poitiers was appointed by the French National Agency for the Safety of Medicines and Health Products. E.B., C.P. contributed to conception of the study. E.B., C.E., B.F., S.P., M.C.P.P., FAN were involved in the acquisition of data. E.B. analyzed data. E.B., C.E., B.F., S.P., M.C.P.P. interpreted data. All authors contributed to the preparation of the manuscript and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bouquet, E., Eiden, C., Fauconneau, B. et al. Adverse events of recreational cannabis use during pregnancy reported to the French Addictovigilance Network between 2011 and 2020. Sci Rep 12, 16509 (2022). https://doi.org/10.1038/s41598-022-19197-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19197-2
- Springer Nature Limited
This article is cited by
-
Association Between Preconception Maternal Mental Health-Related Hospitalisation (MHrH) and Outcomes During Pregnancy: A Population-Based Cohort Study in the Northern Territory, Australia
International Journal of Mental Health and Addiction (2024)