Abstract
Possible mechanisms by which maternal pre-pregnancy body mass index (BMI) programs offspring mental disorders in late childhood are not fully clarified. To assess the association between maternal BMI and mental health problems at 11 years old, we used data from the 2004 Pelotas birth cohort which comprised 4231 newborns. Maternal pre-pregnancy BMI was analyzed as underweight (< 18.5), normal (18.5–24.9), overweight (25.0–29.9), and obesity (≥ 30.0). Mental health problems were assessed at the child’s age of 11 years by the Strengths and Difficulties Questionnaire, total difficulties score and subscale scores (emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems), dichotomized into normal/borderline and abnormal category. The associations between maternal pre-pregnancy BMI and mental health problems in the whole sample and stratified by sex were estimated using crude and adjusted linear and logistic regression. Both linear and logistic regression showed that pre-pregnancy weight was associated with mental problems in early adolescents. Maternal pre-pregnancy obesity was associated with increased odds of total difficulty score among the whole sample. Boys whose mothers were pre-pregnancy overweight had higher odds of conduct problems (OR = 1.56; 95% CI: 1.13, 1.95), when compared to children of normal pre-pregnancy weight mothers, even after adjustments. Maternal pre-pregnancy obesity was associated with mental health problems in early adolescents; specifically, pre-pregnancy overweight increased the risk for conduct problems in 11 years old boys.
Similar content being viewed by others
Introduction
Obesity is a worldwide public health problem, even among women of reproductive age1. In a Brazilian pooled cohort, more than 30% of women started pregnancy overweight or obese2. Several studies have observed associations between maternal obesity before and during pregnancy with other intrauterine risk factors and pregnancy complications, such as gestational diabetes and pre-eclampsia3. Infants born to obese women have higher rates of neural tube defects4 and an increased risk of obesity5 and asthma6 later in life.
Recent studies concerning long-term child mental health outcomes suggest pre-pregnancy obesity is associated with numerous neurodevelopmental and neuropsychiatric events7,8. Compared to children of normal-weight mothers, children whose mothers were obese were more likely to have behavioral or emotional problems9, developmental delay9, peer problems10, internalizing and externalizing problems11, attention deficit hyperactivity disorder (ADHD) or autism spectrum disorder (ASD)8,9,12. Also, severe obesity at pre-pregnancy was associated with worse problem-solving and poorer executive functioning in areas of attention, inhibitory control, and working memory in children13.
Nevertheless, the association between maternal pre-pregnancy obesity and child mental health is inconsistent across the studies14,15. Hence, this study aimed to assess the association between maternal pre-pregnancy BMI and children’s mental health at 11.
Results
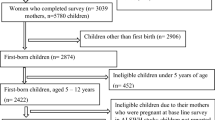
Information about pre-pregnancy BMI was available for 3875 mothers and SDQ scores data for 3563 participants. A total of 3385 cohort participants (80.0% of the original sample), comprising 1644 girls and 1741 boys, had complete information on maternal pre-pregnancy BMI on SDQ and were included in the analyses. Mothers of participants who kept in this study were generally 20–34 years old, more educated, more likely to live with a husband or partner, multiparous and nonsmokers during pregnancy, as compared to those who were not included (Supplementary Table 1).
The distribution of maternal pre-pregnancy BMI according to co-variables is presented in Table 1. Overall, before pregnancy, 2.3% (95% CI: 1.8–2.9) of the mothers were underweight, 54.7% (95% CI: 53.1–56.4) were normal weight, 29.0% (95% CI: 27.5–30.6) were overweight and 13.9% (95% CI: 12.8–15.1) were obese. The prevalence of obesity was higher among mothers aged ≥ 35 years, from the lowest socioeconomic strata, with a low level of formal education, and who lived without a husband or partner.
Table 2 shows the prevalence of mental health problems with 95% CI, according to maternal pre-pregnancy BMI. The prevalence of any difficulty was higher among children of pre-pregnancy underweight (21.8%) and obese mothers (17.2%) than among children of pre-pregnancy normal-weight mothers (13.1%). Prevalence of hyperactivity was also higher among children of pre-pregnancy underweight (19.2%) and obese mothers (17.4%) as compared to children of normal-weight mothers (16.9%).
When stratified by sex, the proportion of girls of pre-pregnancy underweight and obese mothers who had any difficulty (18.9% and 14.9%, respectively) and conduct problems (16.2% and 14.9%, respectively) was higher than among girls of pre-pregnancy normal weight mothers (11.5% and 11.1%, respectively). Boys from pre-pregnancy underweight and obese mothers had higher proportions of hyperactivity (26.8% and 23.0%, respectively) when compared to boys from pre-pregnancy normal-weight mothers (21.7%) (Table 2).
In unadjusted linear analyses, there was a significant increase of 0.05 SDs in peer relationship problems with every SD increase in pre-pregnancy weight (p = 0.03). (Table 3). The logistic regression analysis orientated the results to other findings. Children of pre-pregnancy obese mothers had increased odds of having any difficulty (OR = 1.38, 95% CI: 1.05–1.81) and conduct problems (OR = 1.33, 95% CI: 1.00–1.78) compared with children of pre-pregnancy normal weight mothers. Boys of pre-pregnancy overweight mothers had increased odds of conduct problems (OR = 1.44, 95% CI: 1.07–1.95) compared with their counterparts of pre-pregnancy normal weight mothers. On the other hand, we did not find any association between girls of pre-pregnancy obese mothers and any mental health problems. (Table 4).
The strength of the associations of pre-pregnancy maternal overweight and obesity with mental health problems increased after adjusting for confounders for linear regression. For logistic regression, the association increased specifically for conduct problems.
There was a significant increase of 0.02, 0.04 and 0.04 SDs in emotional symptoms, conduct problems and peer relationships problems with every SD increase in pre-pregnancy weight, respectively (p < 0.01). In boys, the increase was 0.03 SDs in conduct problems score and 0.02 SDs in peer relationship problems with every SD increase in pre-pregnancy weight, respectively (p < 0.01). In contrast, there was a decrease of -0.02 SDs in hyperactivity score with every SD increase in pre-pregnancy weight (p < 0.01) (Table 3). On the other hand, the associations of pre-pregnancy maternal obesity with any difficulty (OR = 1.42, 95% CI: 1.06–1.91) and conduct problems (OR = 1.42, 95%CI: 1.04–1.93) increased after adjusting for confounders, even among boys whose mothers were overweight in pre-pregnancy (OR = 1.56, 95% CI: 1.13–2.16) (Table 4).
Discussion
In this study, maternal pre-pregnancy overweight and obesity were associated with having any difficulty among children at eleven years of age. Maternal pre-pregnancy weight was found associated with emotional problems, conduct problems, peer relationship problems, hyperactivity/inattention problems among children at eleven years. Regardless of the type of analysis, boys of pre-pregnancy overweight mothers had higher odds of presenting conduct problems even after adjustment for confounders compared to children of normal pre-pregnancy weight mothers.
Our findings are in concordance with previously published studies. Kong et al. found that maternal pre-pregnancy obesity was associated with an increased risk of offspring’s psychiatric and mild neurodevelopmental disorders, primarily conduct disorders16. Similar results were demonstrated in the study by Menting et al. carried out on children from Amsterdam17. In this study, the authors assessed child behavioral problems with the maternal and teacher version of the SDQ, finding that maternal pre-pregnancy overweight and obesity were associated with increased children's behavior problems. Teachers reported peer relationship problems for children whose mothers were obese before pregnancy17. Another study of 1311 mother–child pairs reported that children of obese class II/III mothers had increased odds of emotional symptoms, peer relationship problems, total psychosocial difficulties, ADHD diagnosis, autism, or developmental delay diagnosis. In addition, they were more likely to need speech-language therapy, psychological services, and any special needs service compared with children of normal weight mothers10. Others have reported associations between maternal pre-pregnancy obesity and lower cognitive performance18, intellectual disability19,20, ADHD21, and autism22. Although the specific outcomes differed, the findings are generally consistent with those observed in our study. Only one study, based on two European pregnancy cohorts-ALSPAC (UK) and Generation R (Netherlands) found no evidence between maternal pre-pregnancy overweight and offspring cognitive development and behavioral problems14.
Some mechanisms to explain the association between maternal obesity and offspring mental disorders have been explored. Using sibling comparisons, Chen et al. studied high maternal pre-pregnancy body mass index associated with increased risk of offspring Attention-deficit/hyperactivity disorder. They observed the associations between pre-pregnancy overweight/obese mothers with an increased risk of ADHD no longer remained when complete sibling comparisons were performed. Their results suggested that the association between maternal pre-pregnancy overweight/obesity and offspring ADHD could be ascribed to unmeasured familial confounding, which might reflect genetic origin.
On the other hand, the association of pre-pregnancy overweight and obesity with maternal and neonatal adverse outcomes could lead to changes in altered maternal and neonatal physiology, as reported in the meta-analysis by Vats and colleagues23. They included 86 cohort studies of pregnant women and found that pre-pregnancy overweight and obese mothers were associated with cesarean delivery, emergency cesarean delivery, gestational diabetes, gestational hypertension, labor induction, postpartum hemorrhage, pre-eclampsia and pre-term premature rupture of membrane. The fetus and neonates of overweight and obese mothers have a higher risk for admission to the newborn intensive care unit, low APGAR score, large for gestational age, macrosomia, preterm birth. These adverse outcomes directly contribute to malprogramming23.
Furthermore, altered maternal physiology may result in increased inflammation24, lipotoxicity25, and oxidative stress in the fetoplacental unit. These changes in the in-utero environment may contribute to the malprogramming of the fetal brain, pancreas, skeletal muscle, and adipose tissue, among other organs. Peripheral inflammation and insulin resistance lead to central insulin resistance and aberrant central glucose metabolism and transport. Moreover, elevated leptin levels and leptin resistance are prominent in obese mothers26. Considered a critical neurotrophic factor, leptin may signal abnormalities during fetal development, such as decreased neuronal stem cell differentiation and growth27, and the regulation of synaptic plasticity and neurotransmitter receptor trafficking28. Thus, during crucial developmental periods, leptin signaling is considered a potential mechanism underlying abnormal neurodevelopment in fetuses of obese women29. Thus, resulting in an increased risk for offspring mental health problems12.
Strengths and limitations
Our study has some strengths and limitations. The large population-based sample, face-to-face interviews with adolescents and their caregivers, and the use of an internationally recognized instrument to screen mental health problems are among the study’s strengths. Being validated in Brazil and applied by trained psychologists resulted in high-quality data acquisition. On the other hand, the SDQ was applied only to the mothers/caregivers. It would have been interesting to use the SDQ to the teachers and the children’s pairs, too, to obtain a more accurate profile of the cohort participant’s mental health. Another limitation is the presence of attrition in our sample, which could potentially lead to selection bias. Nonetheless, the sample loss was at-random, and the follow-up rates were higher among non-LBW children, from highly educated mothers and non-smokers mothers during pregnancy. These characteristics are commonly associated with adequate child mental health30,31. Therefore, it is unlikely that the observed associations were due to attrition bias.
Our findings evidence associations of maternal pre-pregnancy obesity with children’s mental health problems at eleven years of age. Specifically, boys of pre-pregnancy obese mothers had a higher risk of developing conduct problems when compared with children of normal pre-pregnancy weight mothers. This study highlights that pre-pregnancy obesity may have long-term mental health effects on early adolescents, supporting previous evidence that recommends preventive preconception health care.
Methods
The 2004 Pelotas birth cohort is a population-based birth cohort of individuals born to women living in the urban area of Pelotas, a southern city of Brazil, from January 1st to December 31st, 2004. A total of 4231 live births from all five city hospitals visited daily were enrolled in the study (99.2% of the eligible population). Trained personnel conducted structured interviews containing questions about the demographic, socioeconomic, behavioral, and biological characteristics of mothers and children at different stages. These included the perinatal study (within the first 24 h after delivery); at 3, 12, 24, and 48 months; and at 6 and 11 years of age. Detailed method information can be found elsewhere32,33.
For this study, we used information collected at birth and the 11-year follow-up. In the perinatal study, the interviews and newborn examinations were carried out in maternity hospitals. The response rate of the 11-year follow-up was 87%. All evaluations of this follow-up were performed at the research clinic of the Postgraduate Program in Epidemiology of the Federal University of Pelotas and, we used RedCap as the instrument for data collection34.
Maternal pre-pregnancy BMI
The primary exposure was maternal pre-pregnancy BMI. To construct this variable, the mother pre-pregnancy weight was collected via antenatal record card (n = 3270) when available or by the maternal report (n = 3911) during the perinatal study. Height was collected during the 3-month follow-up visit by our trained field team using an aluminum stadiometer with 1 mm precision (n = 3974). Pre-pregnancy BMI was calculated in kg/m2 and categorized according to the World Health Organization standards. These categories were underweight (BMI < 18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), and obesity (BMI ≥ 30.0)35.
Children mental health assessment
At the 11-year follow-up, trained psychologists interviewed participants’ mothers or caregivers using the Strengths and Difficulties Questionnaire (SDQ), a brief screening instrument designed to assess mental health problems in children and adolescents in the last six months. Developed by Goodman R., the SDQ was validated by Fleitlich-Bilyk and colleagues for use in Brazilian population36,37.
The instrument was composed of 25 questions divided into five subscales: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior. Each question was scored on a three-point scale (not true = 0; somewhat true = 1; certainly true = 2). The total difficulty score (any difficulty), calculated by adding the results of the subscales (except prosocial behavior), ranged from 0 to 40. The subscale scores ranged from 0 to 10. We used the total SDQ score and the four subscales (emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems) dichotomized into normal/borderline and abnormal categories. We adopted the suggested cutoff points for parents’ responses available on the SDQ website (https://sdqinfo.org/py/sdqinfo/c0.py): ≥ 14 for any difficulty, ≥ 4 for emotional symptoms, ≥ 3 for conduct problems, ≥ 6 for hyperactivity/inattention, and ≥ 3 for peer relationship problems.
Co-variables
The variables considered potential confounders were collected at the perinatal study and chosen a priori, based on previous research exploring associations between maternal weight and child development. From the mother, we used the following items: family monthly income (in Brazilian Real), later analyzed in quintiles (1st quintile comprised the poorest and 5th the wealthiest group); maternal schooling (0–4, 5–8 and ≥ 9 years of formal education); mother´s age (≤ 19, 20–34 and ≥ 35 years); the presence of a husband or partner (yes, no); self-referred skin color (White, Black, Other); parity (1, 2 and ≥ 3); smoking during pregnancy-at least one cigarette per day, every day, during any trimester of pregnancy (yes, no); alcohol use during pregnancy-regular use at least once a week, regardless of intake amount (yes, no).
From the child, we used low birth weight (LBW) (< 2500 g; yes, no) to describe the children included in this study, and sex (male, female) to test effect modification.
Analysis
The sample distribution and the prevalence of maternal pre-pregnancy BMI categories were analyzed according to maternal and child characteristics. We used the continuous SDQ scores and also compared the proportion of children with total difficulties and each SDQ subscale score (emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems) according to maternal pre-pregnancy BMI by using bivariate analyses and stratifying by sex. We used linear regression to obtain standarised coefficients (βs) indicating the change on the SDQ subcategories score by a change in the mother’s weight. Also, we used logistic regression to obtain odds ratios (OR) with corresponding 95% confidence intervals (95% CI) for the association between maternal pre-pregnancy BMI and child mental health outcomes. A p-value < 0.05 was considered to be statistically significant. All the crude and adjusted analyses were conducted for the sample as a whole. Interaction terms were tested to examine whether the association between maternal pre-pregnancy BMI and child mental health differed by sex. Due to finding interaction between maternal pre-pregnancy BMI and sex (overweight in girls p = 0.003 and overweight in boys p = 0.024), we stratified the analysis by sex. We performed all analyses using Stata program, version 14.0 (StataCorp LP, College Station, TX).
Ethics
The study was approved by the Ethics and Research Committee of the Faculty of Medicine of the Federal University of Pelotas and adhered to the ethical guidelines of clinical and epidemiological research. Mothers or legal guardians of the children signed an Informed Consent Form after having been notified and explained about the study. At the 11-year follow-up, the children also signed an Informed Consent Form.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Chen, C., Xu, X. & Yan, Y. Estimated global overweight and obesity burden in pregnant women based on panel data model. PLoS ONE 13, e0202183. https://doi.org/10.1371/journal.pone.0202183 (2018).
Carrilho, T. R. B. et al. Brazilian maternal and child nutrition consortium: establishment, data harmonization and basic characteristics. Sci. Rep. 10, 14869. https://doi.org/10.1038/s41598-020-71612-8 (2020).
Marchi, J., Berg, M., Dencker, A., Olander, E. K. & Begley, C. Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes. Rev. 16, 621–638. https://doi.org/10.1111/obr.12288 (2015).
Stothard, K. J., Tennant, P. W. G., Bell, R. & Rankin, J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA 301, 636–650. https://doi.org/10.1001/jama.2009.113 (2009).
Drake, A. J. & Reynolds, R. M. Impact of maternal obesity on offspring obesity and cardiometabolic disease risk. Reproduction 140, 387–398. https://doi.org/10.1530/rep-10-0077 (2010).
Reichman, N. E. & Nepomnyaschy, L. Maternal pre-pregnancy obesity and diagnosis of asthma in offspring at age 3 years. Matern. Child Health J. 12, 725–733. https://doi.org/10.1007/s10995-007-0292-2 (2008).
Antoniou, E. E. et al. Maternal pre-pregnancy weight and externalising behaviour problems in preschool children: a UK-based twin study. BMJ Open 4, e005974–e005974. https://doi.org/10.1136/bmjopen-2014-005974 (2014).
Rivera, H., Christiansen, K. & Sullivan, E. The role of maternal obesity in the risk of neuropsychiatric disorders. Front. Neurosci. https://doi.org/10.3389/fnins.2015.00194 (2015).
Sanchez, C. E. et al. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: a meta-analysis. Obes. Rev. 19, 464–484. https://doi.org/10.1111/obr.12643 (2018).
Jo, H. et al. Maternal prepregnancy body mass index and child psychosocial development at 6 years of age. Pediatrics 135, e1198–e1209. https://doi.org/10.1542/peds.2014-3058 (2015).
Van Lieshout, R. J., Robinson M Fau-Boyle, M. H. & Boyle, M. H. Maternal pre-pregnancy body mass index and internalizing and externalizing problems in offspring.
Edlow, A. G. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn 37, 95–110. https://doi.org/10.1002/pd.4932 (2017).
Mina, T. H. et al. Prenatal exposure to maternal very severe obesity is associated with impaired neurodevelopment and executive functioning in children. Pediatr. Res. 82, 47–54. https://doi.org/10.1038/pr.2017.43 (2017).
Brion, M.-J. et al. Intrauterine effects of maternal prepregnancy overweight on child cognition and behavior in 2 cohorts. Pediatrics 127, e202–e211. https://doi.org/10.1542/peds.2010-0651 (2011).
Bilder, D. A. et al. Maternal prenatal weight gain and autism spectrum disorders. Pediatrics 132, e1276–e1283. https://doi.org/10.1542/peds.2013-1188 (2013).
Kong, L., Norstedt, G., Schalling, M., Gissler, M. & Lavebratt, C. The risk of offspring psychiatric disorders in the setting of maternal obesity and diabetes. Pediatrics 142, e20180776. https://doi.org/10.1542/peds.2018-0776 (2018).
Menting, M. D. et al. The association between pre-pregnancy overweight/obesity and offspring’s behavioral problems and executive functioning. Early Human Dev. 122, 32–41. https://doi.org/10.1016/j.earlhumdev.2018.05.009 (2018).
Basatemur, E. et al. Maternal prepregnancy BMI and child cognition: a longitudinal cohort study. Pediatrics 131, 56–63. https://doi.org/10.1542/peds.2012-0788 (2013).
Heikura, U. et al. Variations in prenatal sociodemographic factors associated with intellectual disability: a study of the 20-year interval between two birth cohorts in Northern Finland. Am. J. Epidemiol. 167, 169–177. https://doi.org/10.1093/aje/kwm291 (2007).
Mann, J., McDermott, S., Hardin, J., Pan, C. & Zhang, Z. Pre-pregnancy body mass index, weight change during pregnancy, and risk of intellectual disability in children. BJOG: Int. J. Obstet. Gynaecol. 120, 309–319. https://doi.org/10.1111/1471-0528.12052 (2013).
Li, L. et al. Maternal pre-pregnancy overweight/obesity and the risk of attention-deficit/hyperactivity disorder in offspring: a systematic review, meta-analysis and quasi-experimental family-based study. Int. J. Epidemiol. 49, 857–875. https://doi.org/10.1093/ije/dyaa040 (2020).
Krakowiak, P. et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 129, e1121. https://doi.org/10.1542/peds.2011-2583 (2012).
Vats, H., Saxena, R., Sachdeva, M. P., Walia, G. K. & Gupta, V. Impact of maternal pre-pregnancy body mass index on maternal, fetal and neonatal adverse outcomes in the worldwide populations: a systematic review and meta-analysis. Obes. Res. Clin. Pract. 15, 536–545. https://doi.org/10.1016/j.orcp.2021.10.005 (2021).
Huleihel, M., Golan, H. & Hallak, M. Intrauterine infection/inflammation during pregnancy and offspring brain damages: possible mechanisms involved. Reprod. Biol. endocrinol. 2, 17. https://doi.org/10.1186/1477-7827-2-17 (2004).
Jarvie, E. et al. Lipotoxicity in obese pregnancy and its potential role in adverse pregnancy outcome and obesity in the offspring. Clin. Sci. 119, 123–129. https://doi.org/10.1042/cs20090640 (2010).
Hauguel-de Mouzon, S., Lepercq, J. & Catalano, P. The known and unknown of leptin in pregnancy. Am. J. Obstet. Gynecol. 194, 1537–1545. https://doi.org/10.1016/j.ajog.2005.06.064 (2006).
Desai, M., Li, T. & Ross, M. G. Fetal hypothalamic neuroprogenitor cell culture: preferential differentiation paths induced by leptin and insulin. Endocrinology 152, 3192–3201. https://doi.org/10.1210/en.2010-1217 (2011).
Cordner, Z. A. & Tamashiro, K. L. K. Effects of high-fat diet exposure on learning and memory. Physiol. Behav. 152, 363–371. https://doi.org/10.1016/j.physbeh.2015.06.008 (2015).
Dodds, L. et al. The role of prenatal, obstetric and neonatal factors in the development of autism. J. Autism Dev. Disord. 41, 891–902. https://doi.org/10.1007/s10803-010-1114-8 (2011).
Jami, E. S., Hammerschlag, A. R., Bartels, M. & Middeldorp, C. M. Parental characteristics and offspring mental health and related outcomes: a systematic review of genetically informative literature. Transl. Psychiatry 11, 197. https://doi.org/10.1038/s41398-021-01300-2 (2021).
Indredavik, M. S. et al. Psychiatric symptoms and disorders in adolescents with low birth weight. Arch. Dis. Child. Fetal and Neonatal Ed. 89, F445–F450. https://doi.org/10.1136/adc.2003.038943 (2004).
Santos, I. S. et al. Cohort profile: the 2004 Pelotas (Brazil) birth cohort study. Int. J. Epidemiol. 40, 1461–1468. https://doi.org/10.1093/ije/dyq130 (2011).
Santos, I. S. et al. Cohort Profile Update: 2004 Pelotas (Brazil) birth cohort study. Body composition, mental health and genetic assessment at the 6 years follow-up. Int J Epidemiol 43, 1437–1437f. https://doi.org/10.1093/ije/dyu144 (2014).
Harris, P. A. et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 (2009).
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series 894, i-xii, 1–253 (2000).
Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 40, 1337–1345. https://doi.org/10.1097/00004583-200111000-00015 (2001).
Fleitlich-Bilyk, B. & Goodman, R. Prevalence of child and adolescent psychiatric disorders in Southeast Brazil. J. Am. Acad. Child. Adolesc. Psychiatry 43, 727–734. https://doi.org/10.1097/01.chi.0000120021.14101.ca (2004).
Funding
This article is based on data from the 2004 Pelotas birth cohort study, conducted by the Postgraduate Program in Epidemiology of the Federal University of Pelotas, Brazil, with the support of the Brazilian Public Health Association (ABRASCO). From 2009 to 2013, the 2004 Pelotas birth cohort was supported by the Wellcome Trust (Grant no. 086974/Z/08/Z). Previous phases of the study were supported by the World Health Organization (Grant no. 03014HNI), National Support Program for Centres of Excellence (PRONEX) (Grant no. 04/0882.7), Brazilian National Research Council (CNPq) (Grant nos. 481012-2009-5; 484077-2010-4; 470965-2010-0; 481141-2007-3), Brazilian Ministry of Health (Grant no. 25000.105293/2004-83) and Children's Pastorate. The 11-year follow-up was also funded by the São Paulo Research Foundation (FAPESP; Grant No. 2014/13864-6). I.S.S., and A.M. are supported by the CNPq.
Author information
Authors and Affiliations
Contributions
G.C.Q. undertook the analysis, interpreted the results, and drafted the first version of the article. T.M., I.S.S. and A.M. Participated in the design and analysis of the study and collaborated with the interpretation of the findings and writing of the article. All authors approved the final version of the manuscript submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Quinte, G.C., Munhoz, T.N., Matijasevich, A. et al. Maternal pre-pregnancy body mass index and mental health problems in early adolescents from the 2004 Pelotas birth cohort. Sci Rep 12, 14437 (2022). https://doi.org/10.1038/s41598-022-18032-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18032-y
- Springer Nature Limited