Abstract
The effect of induction chemotherapy on liver function in patients with acute lymphoblastic leukemia is not well documented in Ethiopia. This study assessed hepatotoxicity in patients with acute lymphoblastic leukemia who were undergoing induction chemotherapy in Ethiopia. A 1-month cohort study was undertaken in forty patients with acute lymphoblastic leukemia, with measurements taken at the baseline, second, and fourth weeks. A Log 10 transformation was done because of the skewed distribution of liver function tests. Descriptive statistics such as mean and proportion were calculated. A mixed model ANOVA and Bonferroni post hoc test were computed. A p value < 0.05 was declared to determine statistical significance. Clinically significant hepatotoxicity was observed in 15% of patients. Mild liver injury occurred in 5% of patients. The mean of all liver function tests increased significantly from pre-induction to post-induction. ALT levels were significantly higher in patients who received blood transfusions, but not in those who did not. Regardless of other factors, ALP level in children is significantly higher than in adults, although total bilirubin in adults is higher than in children. A significant proportion of patients had hepatotoxicity. During chemotherapy induction, the mean of all liver function tests rose significantly, but this elevation of serum liver function tests may be transient. Chemotherapy drugs should be given without causing a significant alteration in serum liver function tests. Continuous monitoring of patients should be required.
Similar content being viewed by others
Introduction
Acute lymphoblastic leukemia (ALL) is the most frequent childhood cancer, but adults can be affected as well1,2,3, and it is caused by hereditary links and genetic abnormalities4. Chemotherapy induction for acute lymphocytic leukemia (ALL) is used to clear immature white blood cells from the blood and bone marrow and achieve full remission or response. The induction phase of treatment lasts a month5,6. Chemotherapy is divided into three phases: the induction phase, the consolidation (or intensification) phase, and the maintenance phase. The goal of treatment is to achieve remission, which is usually defined as a reduction of less than 5% of blast cells in the bone marrow7. Induction treatment (protocol 1) began with one week of prednisone and intrathecal methotrexate (protocol 1/phase 1) and was followed by a 4-week regimen of daily prednisone, intrathecal methotrexate on days 15 and 29, weekly vincristine and daunorubicin, and three times per week l-asparaginase8. Hepatotoxicity is defined as a liver injury caused by medication exposure that result in altered liver function. Hepatocellular liver injury is a prominent initial elevation of the alanine aminotransferase level, cholestatic, as evidenced by an increase in serum alkaline phosphatase levels, or mixed if both enzymes are elevated. ALT levels exceeding three times the upper limit of normal values and total bilirubin concentrations greater than twice the upper limit are defined as clinically significant abnormalities on liver tests9,10,11,12. Patients who received four or more chemotherapy drugs were at risk of experiencing adverse medication reactions13. In the absence of other more likely causes of elevated liver tests, post-chemotherapy liver test results were defined as drug-induced liver injury if ALT was > 3 times the upper limit of normal and total bilirubin (TB) was > 2–3 times the upper limit of normal14,15. Chemotherapy hepatotoxicity often occurs unexpectedly or in an idiosyncratic manner, and previous liver disease increases the risk16. During the treatment of acute leukemia, serum total bilirubin, ALT, and AST levels rise in response to chemotherapy drugs17,18. The anti-leukemic therapy given for the induction of remission did not induce hepatotoxicity except that the serum SGPT was transiently increased during the induction of remission. Elevation in serum enzyme levels is taken as an indicator of liver injury, whereas increases in bilirubin levels, albumin concentration, and prothrombin time are measures of overall liver function12. In Singapore19 and the United States20, 10.7% and 53.9% of patients with acute lymphoblastic leukemia who received L-asparaginase had hepatic transaminase and grade 3/4 transaminitis, respectively. In a study from the Netherlands, in patients treated according to ALL-1, grade 3/4 hyperbilirubinemia and elevated ALT occurred in 10% and 26% of patients, respectively. Hepatotoxicity occurred in 9.76% of patients treated with the Dana Farber Consortium Protocol (DFCP) in Egypt. Adolescents and young adults had favorable outcomes with DFCP but more toxicity21. Greater asparaginase activity levels resulted in statistically significant increases in ALT and bilirubin22. Genetic variations in genes that are linked to hepatotoxicity and cardiotoxicity could influence the safety of standard induction therapy in pediatric patients with acute lymphoblastic leukemia23. Hepatotoxicity was significantly associated with obesity and hypofibrinogenemia, but not to L-asparaginase doses24. Adolescents and young adults are highly susceptible to developing asparaginase liver toxicity25. L-asparaginase treatment was associated with acute liver toxicity in patients with acute lymphoblastic leukemia in a Sudanese study. Adults receiving L-asparaginase treatment are more likely than children to develop acute liver toxicity26.
Chemotherapy induction associated with hepatotoxicity during the induction phase has never been studied in Ethiopia. Clinicians will be able to use these findings to better monitor and manage patients in the future. Thus, the study aimed to determine whether chemotherapy induction is associated with hepatotoxicity in patients with acute lymphoblastic leukemia in Black Lion Hospital, Ethiopia.
Methods
Study area and design
The study was conducted at Black Lion Hospital in Addis Ababa, Ethiopia. The Black Lion Specialized Hospital is affiliated with Addis Ababa University. It is the largest tertiary hospital in the country. From July 1 to September 30, 2019, a cohort study was conducted to evaluate chemotherapy-induced hepatotoxicity in patients with acute lymphoblastic leukemia.
Patient information
Patients over the age of one year who were newly diagnosed with acute lymphoblastic leukemia at Black Lion Hospital between July 1 and September 30, 2019, were included. The same study group is divided into three groups based on the dosages of induction chemotherapy drugs. These were the baseline study group, the second-week induction study group, and the fourth-week induction study group.
Eligible criteria
Patients have been admitted for at least one month and have not yet started induction therapy.
Variables and operational definition
Dependent variables: Hepatotoxicity.
Independent variables: Age, sex, alcohol intake, weight, blood transfusion and chemotherapy induction drugs.
Induction protocol: All patients were treated in Modified Berlin-Frankfurt-Munster 95 dose schedule in Phase A induction chemotherapy27 (Table 1).
Children are defined as those who are under the age of 18 years28.
Hepatotoxicity is defined as any of the following: ALT levels greater than or equal to a fivefold increase above the baseline, or ALT levels greater than or equal to a threefold increase, with a simultaneous increase in bilirubin concentration greater than twofold of the baseline (Table 2)29.
Measurements
The same groups' liver function tests were performed three times a month at baseline, the second week after induction, and the fourth week after induction.
Sample size and sampling method
Each of the three measurements included 40 patients, totaling 120. Purposive sampling was used to select study participants.
Data collection and blood sampling procedures
Data collection
During the data collection period, all participants who were willing to receive chemotherapy induction were included indiscriminately. Informed consent was obtained from each study participant after a brief explanation of the study aim. Background information was collected by structured interview questionnaires. Then, serum blood samples were taken.
Blood sample data collection and processing
Blood samples were taken from participants in 5 ml serum separator tubes once before induction and twice after chemotherapy induction in the 2nd and 4th weeks. After keeping the tube for 20 min to clot, the specimen was centrifuged at 1500 rpm for 5 min, and the serum was separated and stored at 40° until an assay was conducted. The liver function tests were conducted on serum at the Ethiopian Public Health Institute.
Test analysis
The principle of a spectrophotometer analyzed the liver function test to measure the absorption spectrum of the analyst at every wavelength. A Roche-COBAS Integra® 400 automated chemistry analyzer was used. All tests were performed based on the manufacturer's protocol.
Data quality assurance
There was a fair procedure for the selection of study participants and measurement of outcomes.
Data analysis
The data were entered into a database sheet in SPSS version 23. The Shapiro–Wilk test showed that the distributions of all liver function tests were skewed. As a result, a log 10 transformation was computed. The mean and standard deviation were calculated using a log 10 transform. The mean and standard deviations (SD) were then back-transformed. A mixed ANOVA model is used to examine the relationship between independent factors and times (baseline, second week of induction, and fourth week of induction). Greenhouse–Geisser was applied when the assumption of sphericity was violated. A Bonferroni post hoc test was conducted when the F-test was significant. If there is an interaction between the independent variables and the dependent variable, a splitting method was used to determine which group the association occurred in. A p value < 0.05 was declared to determine whether the difference was statistically significant.
Ethical consideration
Ethical clearance was obtained from the ethics review board (ERB) of Addis Ababa University's health science college. All methods were performed in accordance with the relevant guidelines and regulations. No one was harmed because of participating in this study. After a brief explanation of the study objective, informed consent was obtained from adults and the child’s guardian. In addition to parental informed consent, the child’s informed assent was obtained as much as the child’s ability. The right of participants to withdraw at any time was respected. By eliminating identifiers from questionnaires, confidentiality was preserved.
Results
Socio-demographic characteristics of patients with acute lymphoblastic leukaemia
A total of forty patients with acute lymphoblastic leukemia were included in this study. Out of these, 55% of them were males. The median age of patients was 14 years (range 2–52 years). Most of the participants were children, with 40% of those aged 1–9 years. Over 85% of patients had blood transfusions. About 17.5% of patients were underweight. Around thirteen percent (12.5%) of adults were alcohol drinkers (Table 3).
The incidence of chemotherapy drug-induced hepatotoxicity in patients with acute lymphoblastic leukemia
In each of the three measurements (at baseline, second and fourth weeks), a total of forty patients were involved for up to four weeks. Clinically significant hepatotoxicity, including moderate drug-induced liver injury, occurred in 15% of patients. Five percent of patients had mild drug-induced liver injuries. At the baseline and second-week measures, no patients were found to fulfill the criteria for drug-induced liver injury. There were no cases of severe or fatal drug-induced liver injury (Table 4).
The effect of induction chemotherapeutic drugs on the alanine aminotransferase (ALT) enzyme in patients with acute lymphoblastic leukemia
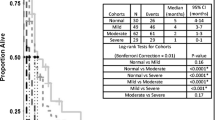
The assumption of sphericity was not met by Mauchly’s sphericity test (p = 0.002). A Greenhouse–Geisser correction was thus used (ɛ = 0.77). The ALT levels differed between those who received blood transfusions and those who did not receive blood transfusions during chemotherapeutic induction (F(1.6, 59) = 4.2, p = 0.029). The ALT level in patients who received blood transfusions increased significantly from pre-induction to 2-week induction and 4-week induction (p < 0.01), but not between 2-week induction and 4-week induction (p = 0.151). The elevation in ALT levels in those who did not get blood transfusions was not statistically significant (p = 0.99) (Table 5). Figure 1 depicts the interaction nature of chemotherapeutic-induced ALT levels in patients with and without blood transfusion.
The effect of induction chemotherapeutic drugs on aspartate aminotransferase (AST) enzyme in patients with acute lymphoblastic leukaemia
The assumption of sphericity was violated (p = 0.004). Therefore, the Greenhouse–Geisser adjustment was used (ɛ = 0.793). A statistically significant difference was observed between the three mean AST enzymes (F(1.6, 60.3) = 8.8, p = 0.001). The mean AST level significantly differed between pre-induction and 2 weeks of induction (p = 001), as well as between pre-induction and 4 weeks of induction (p = 0.014), but not statistically significant between 2-weeks and 4-weeks of induction (p = 0.99) (Table 6).
The effect of induction chemotherapy on alkaline phosphate (ALP) enzyme in patients with acute lymphoblastic leukemia
The Mauchly’s sphericity test indicates that the condition of sphericity was not met (p = 0.001). Thus, the Greenhouse–Geisser correction was applied (ɛ = 0.687). There is a significant difference between the three mean ALP enzymes (F(1.4, 52.2) = 9.03, p = 0.002). A significant difference was seen between pre-induction ALP enzyme and 4-weeks of induction ALP enzyme (p = 0.006), and also between 2-week induction and 4-week induction (p = 0.029). However, no statistically significant difference was found between the pre-induction ALP enzyme and the 2-week induction ALP enzyme (p = 0.05). Ignoring all other factors, the mean ALP differs significantly between children and adults (F(1, 38) = 8.07, p = 0.007) (Table 7).
The effect of chemotherapy induction on total bilirubin in patients with acute lymphoblastic leukemia
The variance homogeneity (p = 0.001) was violated. The Greenhouse–Geisser correction (ɛ = 0.72) was used. At least one significant difference exists between the three total bilirubin measures (baseline, 2-week induction, and 4-week induction) (F(1.4, 54.5) = 5.4, p = 0.014). Only total bilirubin differs significantly between pre-induction and 4 weeks of induction (p = 0.043). Controlling all other factors, total bilirubin in adults is significantly higher than in children (F(1, 38) = 7.1, p = 0.011) (Table 8).
The effect of chemotherapy induction on direct bilirubin in patients with acute lymphoblastic leukaemia
The assumption of sphericity was met (p = 0.81). A mixed model ANOVA revealed that there is at least one statistically significant difference between the three mean direct bilirubin levels (F(2, 76) = 19, p = 0.001). The Bonferroni post hoc test indicated that direct bilirubin levels differed significantly between pre-induction and post-induction (2 and 4 weeks of induction) (p < 0.01), but not between 2-weeks and 4-weeks of induction (p = 0.99) (Table 9).
Discussion
This study was the first to evaluate the side effects of chemotherapeutic drugs on the liver during induction in Ethiopia. After chemotherapy induction, the mean of all liver function tests increased. The cause of the abnormal rise of these liver functions could be exposure to chemotherapy induction. This evidence supports the previous studies9,12,16,17,25. The incidence of chemotherapeutic drug-induced hepatotoxicity, which included moderate drug-induced liver injury, occurred in 15% of patients. These patients fully meet the criteria for clinically significant abnormalities in liver function tests11,12,13,14, indicating hepatocellular injury10,12. The mild drug-induced liver injury occurred in 5% of patients. The incidence of hepatotoxicity in this study is higher than in a prior studies in Egypt21 and Singapore18 but lower than in studies in the United States19 and the Netherlands20 for patients who received L-asparaginase as a chemotherapy induction. The difference could be attributed to the administration of four chemotherapy drugs in the current study, variations in hepatotoxicity grading criteria, the health status of patients, standard care of hospitals, and sample size. Furthermore, genetics can play a role in a significant difference in pancreatitis incidence23. ALT levels increased significantly in those who received blood transfusions from pre-induction to two weeks and four weeks of induction but not between two and four weeks of induction. For those without a blood transfusion, ALT levels have not increased significantly. Elevated levels of ALT in patients who have received blood transfusions may be caused by patients bleeding before donating blood, as these bleeding patients may have hepatotoxicity23. The levels of AST, direct bilirubin, and children's ALT differed significantly between pre-and post-induction but not between two and four weeks. This evidence suggests that chemotherapeutic drugs exposure triggers the production of AST, ALT and direct bilirubin, but increasing cumulative chemotherapy drug dosages may not increase the level of AST, ALT and direct bilirubin. This finding is also in line with a prior study that showed L-asparaginase dosages had no effect on liver toxicity23 and another study that found asparaginase activity-induced statistically significant increases in ALT and bilirubin20. ALP levels increased significantly from pre-induction to four weeks of induction, as well as from two weeks to four weeks of induction. Total bilirubin levels differed only significantly between pre-induction and four-week induction. This showed that increasing the cumulative chemotherapy drug dosages increased ALP and total bilirubin levels. These findings contradicted the previous finding23. Ignoring all other factors, children's ALP levels are significantly higher than those of adults, but the total bilirubin of adults is higher than that of children. The cause of the difference between ALP and total bilirubin may be biological; that is, for children, the concentration of ALP correlates with bone growth and the occurrence of a high concentration of total bilirubin in adults may be associated with increased age. According to the current studies, chemotherapy-induced hepatotoxicity was not significantly different between children and adults. This finding is against with the previous findings that reported L-asparaginase-induced hepatotoxicity differs between children and adults24,25. Genetic variation23 and sample size could be the contributing factors to these contradicting results. Although elevated serum liver enzymes and bilirubin showed liver injury, this hepatocellular injury may be transient due to the absence of additional liver parameters such as albumin and prothrombin, which indicated the overall liver function12.
Despite the fact that logistic regression was not used to control for confounding due to the small sample size, a mixed model ANOVA statistical test can aid in determining the relationship or interaction of independent variables with the dependent variable. Measuring the same group three times and comparing results can help to avoid variations between groups. This study helped clinicians understand chemotherapy drug induction-hepatotoxicity and the development of early preventive measures to limit the progression of drug-induced liver injury. However, patients with acute lymphoblastic leukemia are treated with combination chemotherapy, making it difficult to identify the specific drug causing the hepatic injury. The study is a baseline for future research to identify a precise drug agent causing liver injury with large sample size and a long follow-up period.
Conclusion
A significant proportion of patients had clinically significant hepatotoxicity. The mean rise of liver function tests from baseline to post-induction is statistically significant. The ALT level increased significantly in those who received blood, but not in those who did not donate blood. ALP and total bilirubin levels differ between children and adults, regardless of other factors. The increase in liver enzymes during chemotherapy induction may be transient, resulting in no long-term liver injury. During induction, the chemotherapeutic drugs should be given without causing significant changes in liver function, and patients should be closely monitored.
Data availability
All materials and data were in the manuscript and supplementary material table (Table S1).
Abbreviations
- ANOVA:
-
Analysis of Variance
- SPSS:
-
Statically Package for Social Science
- S.D:
-
Standard deviation
- AST:
-
Aspartate amino transferase
- ALT:
-
Alanine amino transferase
- ALP:
-
Alkaline phosphate
- ULN:
-
Upper limit normal
References
Pui, C.-H. & Evans, W. E. Treatment of acute lymphoblastic leukemia. N. Engl. J. Med. 354(2), 166–178 (2006).
Lopez-Santillan, M., Iparraguirre, L., Martin-Guerrero, I., Gutierrez-Camino, A. & Garcia-Orad, A. Review of pharmacogenetics studies of L-asparaginase hypersensitivity in acute lymphoblastic leukemia points to variants in the GRIA1 gene. Drug Metab. Pers. Ther. 32(1), 1–9 (2017).
Mohseni, M., Uludag, H. & Brandwein, J. M. Advances in biology of acute lymphoblastic leukemia (ALL) and therapeutic implications. Am. J. Blood Res. 8(4), 29 (2018).
Redaelli, A., Laskin, B., Stephens, J., Botteman, M. & Pashos, C. A systematic literature review of the clinical and epidemiological burden of acute lymphoblastic leukaemia (ALL). Eur. J. Cancer Care 14(1), 53–62 (2005).
Society CC. Induction Treatments for Acute Lymphocytic Leukemia. https://cancer.ca/en/cancer-information/cancer-types/acute-lymphocytic-leukemia-all/treatment/induction#:~:text=Induction%20treatment%20is%20also%20called,complete%20remission%2C%20or%20complete%20response.
Booklet ACC. Understanding Chemotherapy. https://www.cancer.org.au/assets/pdf/understanding-chemotherapy-booklet.
medicine P. All About Adult Acute Lymphocytic Leukemia (ALL). https://www.oncolink.org/cancers/leukemia/leukemia-acute-lymphocytic-leukemia-all/all-about-adult-acute-lymphocytic-leukemia-all.
Panzer-Grümayer, E. R., Schneider, M., Panzer, S., Fasching, K. & Gadner, H. Rapid molecular response during early induction chemotherapy predicts a good outcome in childhood acute lymphoblastic leukemia. Blood J. Am. Soc. Hematol. 95(3), 790–794 (2000).
Vagace, J. M. & Gervasini, G. Chemotherapy Toxicity in Patients with Acute Leukemia. Acute Leukemia-The Scientist’s Perspective and Challenge (Intechopen, 2011).
Sharma, A. et al. Chemotherapy induced liver abnormalities: An imaging perspective. Clin. Mol. Hepatol. 20(3), 317 (2014).
Panel CPG, Liver EAftSot. EASL clinical practice guidelines: Drug-induced liver injury. J. Hepatol. 70(6), 1222–1261 (2019).
Jannat, M., Morshed, A. A., Anwer, S. & Islam, S. Effect of chemotherapy on liver function during induction of remission in children with acute lymphoblastic leukemia receiving standard protocol. J. Dhaka Med. Coll. 29(1), 33–37 (2020).
Workalemahu, G., Abdela, O. A. & Yenit, M. K. Chemotherapy-related adverse drug reaction and associated factors among hospitalized paediatric cancer patients at hospitals in North-West Ethiopia. Drug Healthc. Patient Saf. 12, 195 (2020).
Azad, A. et al. Real world experience of drug induced liver injury in patients undergoing chemotherapy. J. Clin. Gastroenterol. Hepatol. 2(3), 18 (2018).
Abboud, G. & Kaplowitz, N. Drug-induced liver injury. Drug Saf. 30(4), 277–294 (2007).
Grigorian, A. & O’Brien, C. B. Hepatotoxicity secondary to chemotherapy. J. Clin. Transl. Hepatol. 2(2), 95 (2014).
Satter, A., Khanam, A., Ibad, S. & Iftikhar, A. Drug induced hepatotoxicity after induction phase of chemotherapy in acute lymphoblastic leukemia patients. Eur. J. Biomed. Pharm. Res. 3, 111–115 (2016).
Islam, T. et al. Liver function tests in patients of acute leukemia before and after induction chemotherapy. J. Biosci. Med. 8(02), 110 (2020).
Yeang, S. H., Chan, A., Tan, C. W., Lim, S. T. & Ng, H. J. Incidence and management of toxicity associated with LAsparaginase in the treatment of ALL and NK/Tcell lymphoma: An observational study. Asian Pac. J. Cancer Prev. 17(7), 3155–3160 (2016).
Aldoss, I. et al. Toxicity profile of repeated doses of PEG-asparaginase incorporated into a pediatric-type regimen for adult acute lymphoblastic leukemia. Eur. J. Haematol. 96(4), 375–380 (2016).
Elashtokhy, H. E. A., Elgohary, H. E., Eldeep, B. B., Gaber, S. M. & Elbedewy, T. A. Retrospective study of Dana Farber Consortium Protocol in newly diagnosed Egyptian adolescents and young adults with acute lymphoblastic leukemia: Tanta experience. J. Egypt. Natl. Canc. Inst. 33(1), 1–10 (2021).
Kloos, R. Q. et al. Individualized asparaginase dosing in childhood acute lymphoblastic leukemia. J. Clin. Oncol. 38(7), 715–724 (2020).
Aslam, S., Ameer, S., Shabana, N. & Ahmed, M. Pharmacogenetics of induction therapy-related toxicities in childhood acute lymphoblastic leukemia patients treated with UKALL 2003 protocol. Sci. Rep. 11(1), 1–8 (2021).
Christ, T. N., Stock, W. & Knoebel, R. W. Incidence of asparaginase-related hepatotoxicity, pancreatitis, and thrombotic events in adults with acute lymphoblastic leukemia treated with a pediatric-inspired regimen. J. Oncol. Pharm. Pract. 24(4), 299–308 (2018).
Boissel, N. & Sender, L. S. Best practices in adolescent and young adult patients with acute lymphoblastic leukemia: A focus on asparaginase. J. Adolesc. Young Adult Oncol. 4(3), 118–128 (2015).
Jahalla, A. & Alameen, A. Assessment of liver function before and after L-asparaginase therapy in acute lymphoblastic leukemia. Eur. J. Biomed. Pharm. Sci. 4, 510–513 (2017).
Gupta, S. et al. Effect of dose and schedule of L-asparaginase administration on early minimal residual disease in acute lymphoblastic leukemia. Indian J. Med. Paediatr. Oncol. 40(4), 496–500 (2019).
Child TACotRaWot. Overarching Definition of the Child in Africa, 1990. http://www.africanchildforum.org/clr/Harmonisation%20of%20Laws%20in%20Africa/other-documents-harmonisation_1_en.pdf.
Aithal, G. P. et al. Case definition and phenotype standardization in drug-induced liver injury. Clin. Pharmacol. Ther. 89(6), 806–815 (2011).
Acknowledgements
The authors like to thank all study participants and other individuals involved in any process of this study.
Author information
Authors and Affiliations
Contributions
Both authors made significant contributions to the conception and design, data acquisition, data analysis, and interpretation, drafted the article or critically revised manuscript for important intellectual content, agreed to submit the manuscript to the current journal and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mekonnen, A.T., Wondmeneh, T.G. Evaluation of liver function tests to identify hepatotoxicity among acute lymphoblastic leukemia patients who are receiving chemotherapy induction. Sci Rep 12, 13215 (2022). https://doi.org/10.1038/s41598-022-17618-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17618-w
- Springer Nature Limited