Abstract
The role of metformin (MET) in the treatment of patients with advanced HFrEF and type 2 diabetes mellitus (DM) is not firmly established. We studied the impact of MET on metabolic profile, quality of life (QoL) and survival in these patients. A total of 847 stable patients with advanced HFrEF (57.4 ± 11.3 years, 67.7% NYHA III/IV, LVEF 23.6 ± 5.8%) underwent clinical and laboratory evaluation and were prospectively followed for a median of 1126 (IQRs 410; 1781) days for occurrence of death, urgent heart transplantation or mechanical circulatory support implantation. A subgroup of 380 patients (44.9%) had DM, 87 of DM patients (22.9%) were treated with MET. Despite worse insulin sensitivity and more severe DM (higher BMI, HbA1c, worse insulin resistance), MET-treated patients exhibited more stable HF marked by lower BNP level (400 vs. 642 ng/l), better LV and RV function, lower mitral and tricuspid regurgitation severity, were using smaller doses of diuretics (all p < 0.05). Further, they had higher eGFR (69.23 vs. 63.34 ml/min/1.73 m2) and better QoL (MLHFQ: 36 vs. 48 points, p = 0.002). Compared to diabetics treated with other glucose-lowering agents, MET-treated patients had better event-free survival even after adjustment for BNP, BMI and eGFR (p = 0.035). Propensity score-matched analysis with 17 covariates yielded 81 pairs of patients and showed a significantly better survival for MET-treated subgroup (p = 0.01). MET treatment in patients with advanced HFrEF and DM is associated with improved outcome by mechanisms beyond the improvement of blood glucose control.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (DM) is a common and severe comorbidity in patients with heart failure with reduced ejection fraction (HFrEF), but optimal treatment modality has not yet been clarified. Biguanides including metformin (MET) had long been considered contraindicated in HF patients due to concerns about lactic acidosis, that was observed with phenformin, an older biguanide with less favorable pharmacological profile1. Large meta-analysis, however, has not demonstrated an association between MET therapy and increased risk of lactic acidosis2, so MET has been used even in HF population. Observational studies showed not only MET safety in HF subjects3,4,5 but some studies even suggested a survival benefit associated with this drug6,7,8. However, there is only one study analyzing MET specifically in patients with HFrEF9 and the absence of a randomized trial is a major limitation for MET use. Moreover, registry-based retrospective studies lack a precise characterization of analyzed patients (echocardiography, laboratory analysis including metabolic profile). Therefore, the mechanism of MET action in this population is speculative.
The aim of the present study was to evaluate the association between MET treatment and metabolic profile, quality of life and outcome in prospectively followed advanced HFrEF patients.
Methods
Patients
Patients with stable HFrEF (LVEF < 40%) of least 6-month duration receiving a stable medication for at least 3 months were enrolled in the study between 2008 and 2016 in a prospectively defined registry. Subjects with potentially reversible LV dysfunction (planned valve surgery, revascularization, or tachycardia-induced cardiomyopathy) were excluded. Patients were followed until July 2019. DM was diagnosed according to current recommendation10. The investigation conforms with the principles outlined in the Declaration of Helsinki, the study protocol was approved by the Institutional Ethics Committee and all subjects signed an informed consent. At the study enrollment, patients completed a Minnesota Living with Heart Failure Questionnaire (MLHFQ) and had anthropometric tests and underwent an echocardiographic study (Vivid-7; General Electric, Milwaukee, Wisconsin). LV function and dimensions were measured according to recommendations11. RV dysfunction was quantified in four grades (0–3). Mitral and tricuspid regurgitations were assessed semiquantitatively and expressed in 3 grades (mild, moderate, significant). An adverse outcome was defined as the combined endpoint of death, urgent heart transplantation (HTx) or mechanical circulatory support (MCS) implantation12. Patients who received a non-urgent HTx were censored as having no adverse event at the day of HTx.
Statistical analysis
Data are presented as mean ± standard deviation, median with interquartile ranges (IQRs), or frequency (percent). Unpaired t-test or Mann–Whitney test were used to compare continuous variables between groups as appropriate. The effect of biomarker concentration on prognosis was tested using univariate and multivariable Cox model. Event-free survival of patients was analyzed by Kaplan–Meier analysis with log-rank test comparison between groups. Propensity score matching was used to account for differences in characteristics of patients with and without MET. The propensity score for each patient was calculated using a multivariable logistic regression model in which the MET use was regressed on 17 characteristics (see “Results” section) that might influence the selection of MET therapy or that have been shown to influence prognosis of patients with advanced HF. All tests were 2-sided, and p values < 0.05 were considered significant. Calculations were performed using JMP 11 (SAS Institute Inc., Cary, NC) and R (Vienna, Austria). Methods in detail can be found in the Online Supplement.
Ethics approval and consent to participate
The ethical committee of the Institute for Clinical and Experimental Medicine-IKEM and Thomayer hospital in Prague approved the study protocol. Written, informed consent for participation in the study was obtained from all the subjects. The study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments.
Results
Patients
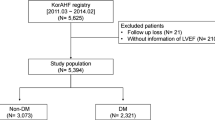
A total of 847 advanced HFrEF patients (67.7% were in with NYHA III/IV, average LV-ejection fraction was 23.6%, 44.9% had moderate/severe RV dysfunction), were enrolled in the study (Fig. 1 in the Online supplement). Enrolled patients achieved high level of guideline-recommended HF pharmacotherapy and device therapy (Table 1). Patients were prospectively followed for a median of 1126 (IQRs 410; 1781) days. During follow-up, 515 patients (60.8%) experienced an adverse outcome.
A total of 380 patients (44.9%) were found to have DM, 467 patients (55.1%) were DM free. All DM patients had type 2 DM; none of the patients had type 1 DM. DM patients were older, had more often CAD as underlying HF etiology, larger body mass index, worse renal function (Table 1) and worse cumulative survival—269 (70.8%) DM vs. 246 (52.7%) non-DM patients experienced an adverse outcome, median time to event was 879 days (IQRs 312; 1631) for DM patients compared with 1270 (IQRs 467; 2010) days for non-DM counterparts. Kaplan–Meier curves are provided in Fig. 2 in the Online Supplement.
Diabetes treatment
Out of 380 DM patients, 153 patients (40.3%) were treated with diet only, 87 patients (22.9%) with MET, 67 patients (17.6%) with sulfonylurea (SU) derivatives, 108 patients (28.4%) with insulin, 26 patients (6.8%) with DPPIV-inhibitors, 3 patients (0.8%) with repaglinide and 1 patient (0.3%) was treated with liraglutide. In 3 patients the information about the treatment was missing. None of the patients was treated with thiazolidinediones, acarbose or SGLT2-inhibitors. 31 patients (8.2%) were treated with more than one peroral antidiabetics (PAD), 26 patients (6.8%) with the combination of PAD and insulin. More detailed information about DM treatment is given in Table 1 and Fig. 3 in the Online Supplement.
In patients treated with MET, the most widely used MET dose was 1000 mg (29 patients, 33.3%). 18 patients (20.7%) were taking a dose lower than 1000 mg, 14 patients (16.1%) a dose between 1000 and 2000 mg and 25 patients (28.8%) were taking 2000 mg daily or higher. The information about MET daily dose was missing in 1 patient (1.1%). Distribution of MET daily dose is in Fig. 4 in the Online Supplement.
Compared with MET-free counterparts, MET-treated DM patients had better LV function (LVEF), RV function and lower both mitral and tricuspid regurgitation severity, better renal function and larger BMI. They were using smaller diuretic doses but achieved similar level of guideline-recommended HF pharmacotherapy, had comparable rate of ICD and CRT treatment and similar hemodynamic profile (Table 1). MET-treated patients were more often treated with SU derivatives and DPPIV-inhibitors; no significant difference was found for insulin treatment.
Metabolic profile of MET-treated patients
Analysis of metabolic parameters revealed that compared with MET-free counterparts, MET-treated patients had similar levels of fasting glycemia and insulin secretion (C-peptide level), but larger Hb1Ac level, higher insulin and glucagon level and more pronounced insulin resistance (HOMA-IR), Table 1 and Fig. 1. Further, MET-treated patients had higher level of beta-hydroxybutyrate but similar level of GDF-15 (Fig. 1).
Diabetes treatment and quality of life
No significant difference was found in QoL between patients with and without DM (Table 1). In DM subgroup, pharmacotherapy with neither insulin, SU derivatives nor with DPPIV-inhibitors was associated with better QoL (Table 1 in the Online Supplement). On the contrary, MET treatment was associated with a better QoL (Table 1).
Multivariable regression analysis identified MET treatment together with BNP and BMI, but not eGFR, SU derivatives treatment, DPPIV-inhibitors treatment or insulin treatment to be independently associated with MLHFQ score (Table 2 in the Online Supplement). Similar results were obtained for the somatic component of MLHFQ whereas no association of MET treatment with emotional component of the MLHFQ score was found (data not shown).
Diabetes treatment and outcome
Kaplan–Meier analysis showed that MET-treated diabetic patients had better survival compared to MET-free counterparts. Other therapeutic regimes were not associated with any difference in event-free survival (Fig. 2). Similarly, Cox proportional hazard model identified MET treatment to be associated with improved outcome. No such relationship was observed for therapy with insulin, SU derivatives or DPPIV-inhibitors (Table 3 in the Online Supplement).
Next, we have analyzed whether there was any subgroup having altered benefit from MET treatment. No significant interaction was found between MET therapy and NYHA functional class, LVEF, RV dysfunction grade, BNP level, eGFR, ACEi/ARB treatment, beta-blocker treatment, presence of ICD, or CRT (all p for interaction ≥ 0.20, Table 4 in the Online Supplement). This suggests that the benefit from MET therapy is preserved regardless of HF severity and independent of HF treatment. Similarly, no significant interaction was found between MET therapy and insulin or DPPIVi treatment (p for interaction = 0.35 and 0.95, respectively). However, borderline interaction was found for SU derivatives treatment (p for interaction = 0.054). Kaplan–Meier analysis showed borderline worse survival of patients treated with MET and SU derivatives compared with MET without SU derivatives (p (log-rank) = 0.08).
Adjustment for confounders, propensity score-matched analysis
Although MET-treated DM patients had better cardiac function, renal function and larger BMI, Cox proportional hazard model analysis revealed that MET treatment was associated with a significantly better outcome even after the adjustment for BNP, eGFR and BMI (Table 2).
Finally, we have performed propensity score matched analysis that matched the patients for 17 variables that might influence the selection of MET therapy or that have been shown to influence prognosis of patients with advanced heart failure (age, sex, NYHA functional class, BMI, estimated glomerular filtration rate, LVEF, RV dysfunction grade, mitral and tricuspid regurgitation severity, BNP level, beta-blockers use, renin-angiotensin system inhibitors use, ICD therapy, CRT therapy, uric acid levels, treatment with other PAD/incretins and treatment with insulin). Propensity score matching yielded 81 pairs of patients. Standardized mean differences of matched covariates ranged from 0 to 0.23, with a standardized median difference of 0.06 (IQR 0.029–0.076). Significantly better survival for MET-treated group was showed both using the McNemar (p = 0.04), as well as Cox proportional hazard model (p = 0.01, Fig. 3).
Survival of MET-treated patients, propensity-score matched analysis. BMI body mass index, eGFR estimated glomerular filtration rate, LVEF left ventricle ejection fraction, RV right ventricle, BNP B-type natriuretic peptide, RAAi renin-angiotensin system inhibitors, ICD implantable cardioverter/defibrillator, CRT cardiac resynchronization, therapy, PAD peroral antidiabetics.
Discussion
The results of this study can be summarized as follows: (i) despite worse insulin sensitivity and worse DM compensation in MET-treated patients, MET-treatment was independently associated with both better quality of life and improved outcome in advanced HFrEF patients with DM; (ii) MET treatment was associated with better outcome regardless of HF severity or compensation of diabetes.
Optimal treatment modality in patients with advanced HF and DM is not well established, which is mirrored by the large variability of treatment strategies observed in our study.
Only 22.9% of our patients were treated with MET, which is likely a consequence of previous recommendations to avoid this drug in HF because of concerns regarding lactic acidosis risk13. Nevertheless, MET was used in clinical practice and data on MET use in HF patients with DM eventually emerged. One recently published study showed lower risk of hospitalization for HF in MET-treated DM patients14. Thirteen studies have been published describing the association between MET treatment on outcome in patients with established HF and DM6,7,9,15,16,17,18,19,20,21,22,23,24. However, the majority of studies are retrospective and based on administrative or disease records7,17,18,19,20,21,23,24. Only five of them reported LV-ejection fraction6,7,9,17,22 and only one study focused specifically on patients with LVEF < 40%9. Although meta-analyses of these studies reported mostly better outcome in patients treated with MET3,4, the heterogeneity of studied populations and approaches leave many questions unanswered. None of the studies focused specifically on patients with advanced HF and no study HFrEF patients employed propensity-matching approach. As large randomized controlled trials with MET in HF patients with DM are unlikely to be carried out25, our data offering a prospective observational design of well-characterized cohort employing propensity matching analysis offers the strongest evidence possible. In the propensity matching analysis, we have adjusted the cohort for seventeen possible confounders and our data thus strongly suggest that despite differences between MET-treated and MET-free patients, observed difference in outcome between these groups is indeed attributable to MET therapy.
The mechanism of action of MET is a subject of intense debate. Beneficial effect of MET was first explained by an inhibition of mitochondrial complex I26,27 and by an increase in ADP/ATP ratio that activates AMP-dependent protein kinase (AMPK). However, the mechanism of action of MET is likely to be more pleiotropic; MET enhances cardiac autophagy28, improves myocardial efficiency and reduces myocardial energy consumption29, and directly modulates the growth and function of gut microbiota30. MET has been also shown to have potent effect on cancer prevention and recurrence31,32 and its anti-cancer effect might be also clinically relevant in HF patients as they are consistently reported to have higher risk of malignancies33,34.
Although our study was not designed to unveil the mechanism responsible for overall benefit from MET therapy, our data suggest that the cardioprotection of MET is independent on glycemic control. This is in line with results of the post UKPDS-trial follow-up that showed significant risk reduction by MET in diabetes-related endpoints despite of the loss of between-group differences in glycated hemoglobin35. Experimental studies have similarly shown anti-inflammatory properties of MET irrespective of DM status36.
Metabolic abnormalities are observed early in the course of cardiac pathologies. When subjected to pressure overload, the ventricular myocardium shifts from fatty acids to glucose as its main source for energy; this precedes the development of LV hypertrophy36. The excessive glucose metabolism in the cardiomyocytes causes glucose-6-phosphate (G6P) accumulation. G6P activates mammalian target of rapamycin complex 1 (mTORC1), which induces hypertrophy. MET activates AMPK, which inhibits mTROC1, thus preventing LV hypertrophy36. This explains that MET treatment has also been shown to induce regression of LV-hypertrophy and exert anti-oxidant effects even in non-diabetic patients37. Similarly, LV reverse remodeling has been observed in other drugs that activate AMPK such as SGLT2-inhibitors38.
In non-HF subjects, MET was shown to mediate its effect on body weight and energy balance through GDF-1539. We have not observed increased GDF-15 level in MET-treated compared with MET-free patients in our study, which can be explained by worse cardiac and renal function in MET-free patients. Both cardiac as well as renal dysfunction are associated with higher GDF-15 levels40. MET-treated patients have increased ketone body beta-hydroxybutyrate, a metabolic substrate that is readily utilized by failing heart and that may have favorable effects on bioenergetics41. Infusion of ketone bodies in HFrEF patients was shown to improve cardiac output and LV-ejection fraction42. Interestingly, despite patients on MET had lower neurohumoral activation, we observed higher levels of stress hormone glucagon in MET-treated patients. Is was shown that MET administration to prediabetic subjects resulted in an increase of glucagon43. Higher glucagon in MET-treated patients may be protective against hypoglycemia that is a feared complication of DM treatment and was linked to arrhythmias and increased mortality44.
Although QoL was independent of DM status in our study, we have observed a better QoL in MET-treated DM patients and MET was significantly associated with QoL also in multivariable linear regression suggesting its independent effect on QoL. To our best knowledge, this is the first study that analyzed the QoL with respect to MET treatment using a validated tool45. It has been recently demonstrated that QoL in HF patients is driven by HF itself, not by associated comorbidities46. MET-induced improvement in myocardial efficiency29 suggests that the effect of MET on QoL in HF is rather due to an improvement in HF, not due to improvement in blood glucose control.
Beneficial effects of MET documented in high risk advanced HF population suggest that MET should be more widely used in management of HF. Even in studies with SGLT2 inhibitors in HF patients, a substantial proportion of DM+ patients were treated with biguanides (metformin). In DAPA-HF trial, 41.8% of patients had DM and 51% of DM+ patients were treated by biguanides (predominantly MET)47. EMPEROR-Reduced trial reports also a 49.8% prevalence of DM and 46.4% of DM+ patients were treated with biguanides48,49. Our data strongly suggest that MET should be a frontline drug for the treatment of diabetic patients with HFrEF. Combination therapy with MET and SGLT2i has been shown safe and efficacious in patients with DM50. Combined therapy of these patients with MET and SGLT2 inhibitors warrants further research.
Limitations
Our study was performed in a heart center offering a complex cardiovascular program including MCS implantation and HTx. Since this could introduce bias related to the analysis of prognostic value, urgent HTx and MCS implantation were considered adverse outcomes, while the patients receiving non-urgent HTx were censored as having no adverse outcome on the day of transplantation12. In addition, it was a single-center study with a substantial predominance of males. Our study cohort included patients with advanced HFrEF, the results thus might not be fully applicable to patients with milder HF or to older patients. Data about HF re-hospitalizations were not available in all patients so this endpoint could have not been included in the analysis. The information about DM duration and MET exposure time before entering the study were not available in all subjects, therefore it was not possible to address these variables in the propensity-matching analysis. The cause of death was not available in all patients, so we were not able to distinguish between cardiovascular and non-cardiovascular mortality. QoL was analyzed only at baseline and is likely a result of a various time of preceding MET therapy; the time of MET treatment before baseline exam or during follow-up is unknown. Data about plasmatic MET concentration are not available; similarly, lactate was not measured. None of the patients was treated by sacubitril-valsartan or SGLT2 inhibitors. Therefore, it is impossible to analyze potentially additional effect of MET and these agents. Only a subset of patients had serial echocardiographic examinations, so it was not possible to analyze the impact of MET-treatment of cardiac reverse remodeling.
Conclusion
Metformin treatment in advanced HFrEF patients with DM is associated with better outcome by mechanisms beyond the improvement of blood glucose control. Metformin should stay among frontline drugs for the management of HFrEF patients with DM.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request (jan.benes@ikem.cz).
References
Lu, H. C., Parikh, P. P. & Lorber, D. L. Phenformin-associated lactic acidosis due to imported phenformin. Diabetes Care 19, 1449–1450. https://doi.org/10.2337/diacare.19.12.1449 (1996).
Salpeter, S. R., Greyber, E., Pasternak, G. A. & Salpeter, E. E. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2010, CD002967. https://doi.org/10.1002/14651858.CD002967.pub4 (2010).
Eurich, D. T. et al. Comparative safety and effectiveness of metformin in patients with diabetes mellitus and heart failure: Systematic review of observational studies involving 34,000 patients. Circ. Heart Fail. 6, 395–402. https://doi.org/10.1161/circheartfailure.112.000162 (2013).
Crowley, M. J. et al. Clinical outcomes of metformin use in populations with chronic kidney disease, congestive heart failure, or chronic liver disease: A systematic review. Ann. Intern. Med. 166, 191–200. https://doi.org/10.7326/m16-1901 (2017).
Dludla, P. V. et al. Metformin and heart failure-related outcomes in patients with or without diabetes: A systematic review of randomized controlled trials. Heart Fail. Rev. 26, 1437–1445. https://doi.org/10.1007/s10741-020-09942-y (2021).
Aguilar, D., Chan, W., Bozkurt, B., Ramasubbu, K. & Deswal, A. Metformin use and mortality in ambulatory patients with diabetes and heart failure. Circ. Heart Fail. 4, 53–58. https://doi.org/10.1161/circheartfailure.110.952556 (2011).
MacDonald, M. R. et al. Treatment of type 2 diabetes and outcomes in patients with heart failure: A nested case-control study from the U.K. general practice research database. Diabetes Care 33, 1213–1218. https://doi.org/10.2337/dc09-2227 (2010).
Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352, 854–865 (1998).
Shah, D. D., Fonarow, G. C. & Horwich, T. B. Metformin therapy and outcomes in patients with advanced systolic heart failure and diabetes. J. Cardiac Fail. 16, 200–206. https://doi.org/10.1016/j.cardfail.2009.10.022 (2010).
Cosentino, F. et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 41, 255–323. https://doi.org/10.1093/eurheartj/ehz486 (2020).
Lang, R. M. et al. Recommendations for chamber quantification. Eur. J. Echocardiogr. 7, 79–108. https://doi.org/10.1016/j.euje.2005.12.014 (2006).
Aaronson, K. D. et al. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation 95, 2660–2667. https://doi.org/10.1161/01.cir.95.12.2660 (1997).
Inzucchi, S. E., Masoudi, F. A. & McGuire, D. K. Metformin in heart failure. Diabetes Care 30, e129. https://doi.org/10.2337/dc07-1686 (2007).
Tseng, C. H. Metformin use is associated with a lower risk of hospitalization for heart failure in patients with type 2 diabetes mellitus: A retrospective cohort analysis. J. Am. Heart Assoc. 8, e011640. https://doi.org/10.1161/jaha.118.011640 (2019).
Bergmark, B. A. et al. Metformin use and clinical outcomes among patients with diabetes mellitus with or without heart failure or kidney dysfunction: Observations from the SAVOR-TIMI 53 trial. Circulation 140, 1004–1014. https://doi.org/10.1161/circulationaha.119.040144 (2019).
Inzucchi, S. E. et al. Insulin-sensitizing antihyperglycemic drugs and mortality after acute myocardial infarction: Insights from the National Heart Care Project. Diabetes Care 28, 1680–1689. https://doi.org/10.2337/diacare.28.7.1680 (2005).
Masoudi, F. A. et al. Thiazolidinediones, metformin, and outcomes in older patients with diabetes and heart failure: An observational study. Circulation 111, 583–590. https://doi.org/10.1161/01.cir.0000154542.13412.b1 (2005).
Eurich, D. T., Majumdar, S. R., McAlister, F. A., Tsuyuki, R. T. & Johnson, J. A. Improved clinical outcomes associated with metformin in patients with diabetes and heart failure. Diabetes Care 28, 2345–2351. https://doi.org/10.2337/diacare.28.10.2345 (2005).
Evans, J. M. et al. Effect of Metformin on mortality in patients with heart failure and type 2 diabetes mellitus. Am. J. Cardiol. 106, 1006–1010. https://doi.org/10.1016/j.amjcard.2010.05.031 (2010).
Roussel, R. et al. Metformin use and mortality among patients with diabetes and atherothrombosis. Arch. Intern. Med. 170, 1892–1899. https://doi.org/10.1001/archinternmed.2010.409 (2010).
Andersson, C. et al. Metformin treatment is associated with a low risk of mortality in diabetic patients with heart failure: A retrospective nationwide cohort study. Diabetologia 53, 2546–2553. https://doi.org/10.1007/s00125-010-1906-6 (2010).
Romero, S. P. et al. Metformin therapy and prognosis of patients with heart failure and new-onset diabetes mellitus. A propensity-matched study in the community. Int. J. Cardiol. 166, 404–412. https://doi.org/10.1016/j.ijcard.2011.10.141 (2013).
Tinetti, M. E., McAvay, G., Trentalange, M., Cohen, A. B. & Allore, H. G. Association between guideline recommended drugs and death in older adults with multiple chronic conditions: Population based cohort study. BMJ (Clin. Res. Ed.) 351, h4984. https://doi.org/10.1136/bmj.h4984 (2015).
Weir, D. L., McAlister, F. A., Senthilselvan, A., Minhas-Sandhu, J. K. & Eurich, D. T. Sitagliptin use in patients with diabetes and heart failure: A population-based retrospective cohort study. JACC. Heart Fail. 2, 573–582. https://doi.org/10.1016/j.jchf.2014.04.005 (2014).
Eurich, D. T. et al. Metformin treatment in diabetes and heart failure: When academic equipoise meets clinical reality. Trials 10, 12. https://doi.org/10.1186/1745-6215-10-12 (2009).
Owen, M. R., Doran, E. & Halestrap, A. P. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem. J. 348(Pt 3), 607–614 (2000).
El-Mir, M. Y. et al. Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J. Biol. Chem. 275, 223–228. https://doi.org/10.1074/jbc.275.1.223 (2000).
Kanamori, H. et al. Metformin enhances autophagy and provides cardioprotection in δ-sarcoglycan deficiency-induced dilated cardiomyopathy. Circ. Heart Fail. 12, e005418. https://doi.org/10.1161/circheartfailure.118.005418 (2019).
Larsen, A. H. et al. A randomised, double-blind, placebo-controlled trial of metformin on myocardial efficiency in insulin-resistant chronic heart failure patients without diabetes. Eur. J. Heart Fail. 22, 1628–1637. https://doi.org/10.1002/ejhf.1656 (2020).
Wu, H. et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat. Med. 23, 850–858. https://doi.org/10.1038/nm.4345 (2017).
He, K. et al. The effect of metformin therapy on incidence and prognosis in prostate cancer: A systematic review and meta-analysis. Sci. Rep. 9, 2218. https://doi.org/10.1038/s41598-018-38285-w (2019).
Anselmino, L. E. et al. Repositioning metformin and propranolol for colorectal and triple negative breast cancers treatment. Sci. Rep. 11, 8091. https://doi.org/10.1038/s41598-021-87525-z (2021).
Meijers, W. C. et al. Heart failure stimulates tumor growth by circulating factors. Circulation 138, 678–691. https://doi.org/10.1161/circulationaha.117.030816 (2018).
Banke, A. et al. Incidence of cancer in patients with chronic heart failure: A long-term follow-up study. Eur. J. Heart Fail. 18, 260–266. https://doi.org/10.1002/ejhf.472 (2016).
Holman, R. R., Paul, S. K., Bethel, M. A., Matthews, D. R. & Neil, H. A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 359, 1577–1589. https://doi.org/10.1056/NEJMoa0806470 (2008).
Cameron, A. R. et al. Anti-inflammatory effects of metformin irrespective of diabetes status. Circ. Res. 119, 652–665. https://doi.org/10.1161/circresaha.116.308445 (2016).
Mohan, M. et al. A randomized controlled trial of metformin on left ventricular hypertrophy in patients with coronary artery disease without diabetes: The MET-REMODEL trial. Eur. Heart J. 40, 3409–3417. https://doi.org/10.1093/eurheartj/ehz203 (2019).
Santos-Gallego, C. G. et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J. Am. Coll. Cardiol. 73, 1931–1944. https://doi.org/10.1016/j.jacc.2019.01.056 (2019).
Coll, A. P. et al. GDF15 mediates the effects of metformin on body weight and energy balance. Nature 578, 444–448. https://doi.org/10.1038/s41586-019-1911-y (2020).
Benes, J. et al. The role of GDF-15 in heart failure patients with chronic kidney disease. Can. J. Cardiol. 35, 462–470. https://doi.org/10.1016/j.cjca.2018.12.027 (2019).
Monzo, L. et al. Myocardial ketone body utilization in patients with heart failure: The impact of oral ketone ester. Metab. Clin. Exp. 115, 154452. https://doi.org/10.1016/j.metabol.2020.154452 (2021).
Nielsen, R. et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation 139, 2129–2141. https://doi.org/10.1161/circulationaha.118.036459 (2019).
Konopka, A. R. et al. Hyperglucagonemia mitigates the effect of metformin on glucose production in prediabetes. Cell Rep. 23, 2532. https://doi.org/10.1016/j.celrep.2018.05.027 (2018).
Landstedt-Hallin, L., Englund, A., Adamson, U. & Lins, P. E. Increased QT dispersion during hypoglycaemia in patients with type 2 diabetes mellitus. J. Intern. Med. 246, 299–307. https://doi.org/10.1046/j.1365-2796.1999.00528.x (1999).
Rector, T. S., Kubo, S. H. & Cohn, J. N. Validity of the Minnesota living with heart failure questionnaire as a measure of therapeutic response to enalapril or placebo. Am. J. Cardiol. 71, 1106–1107. https://doi.org/10.1016/0002-9149(93)90582-w (1993).
Benes, J. et al. The effect of three major co-morbidities on quality of life and outcome of patients with heart failure with reduced ejection fraction. ESC Heart Fail. https://doi.org/10.1002/ehf2.13227 (2021).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008. https://doi.org/10.1056/NEJMoa1911303 (2019).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424. https://doi.org/10.1056/NEJMoa2022190 (2020).
Anker, S. D. et al. Effect of empagliflozin on cardiovascular and renal outcomes in patients with heart failure by baseline diabetes status: Results from the EMPEROR-reduced trial. Circulation 143, 337–349. https://doi.org/10.1161/circulationaha.120.051824 (2021).
Gebrie, D., Getnet, D. & Manyazewal, T. Cardiovascular safety and efficacy of metformin-SGLT2i versus metformin-sulfonylureas in type 2 diabetes: Systematic review and meta-analysis of randomized controlled trials. Sci. Rep. 11, 137. https://doi.org/10.1038/s41598-020-80603-8 (2021).
Funding
This work was supported by Ministry of Health, Czech Republic—conceptual development of research organization (Institute for Clinical and Experimental Medicine—IKEM) [IN 00023001] and by Grants NV19-02-00130, NV 19-09-00125, NU21-02-00402 and by the project National Institute for Research of Metabolic and Cardiovascular Diseases (Programme EXCELES, Project No. LX22NPO5104) - Funded by the European Union - Next Generation EU.
Author information
Authors and Affiliations
Contributions
J.B., M.K. and K.K. participated in the enrollment of patients, performed echocardiography, analyzed the data and wrote the manuscript. P.W. analyzed the data and revised the manuscript for important intellectual content. J.K., J.F. and P.J. performed laboratory analyses and revised the manuscript. M.H., L.H. and E.H. participated in the enrollment of patients and performed follow-up. T.P., J.K. and V.M. designed the study, participated in data analysis, interpretation and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
Josef Kautzner is a member of Advisory Boards for Bayer, Boehringer Ingelheim, Daiichi Sankyo, Biosense Webster, Medtronic and St Jude Medical (Abbott). He has received speaker honoraria from the above-mentioned companies and from Biotronik, Mylan, Pfizer and Pro Med. Petr Jarolim received research support from Abbott Laboratories, Amgen Inc., AstraZeneca LP, Beckman Coulter, Daiichi Sankyo, Inc., GlaxoSmithKline, Merck & Co., Inc., Roche Diagnostics Corporation, Takeda Global Research and Development Center and Waters Technologies Corporation and speaker honoraria from Roche Diagnostics Corporation. All other authors have no competing interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Benes, J., Kotrc, M., Kroupova, K. et al. Metformin treatment is associated with improved outcome in patients with diabetes and advanced heart failure (HFrEF). Sci Rep 12, 13038 (2022). https://doi.org/10.1038/s41598-022-17327-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17327-4
- Springer Nature Limited