Abstract
Over the last two decades, we have tracked the national burden of cancer and its trends in Ethiopia, providing estimates of incidence, death, and disability adjusted life years. In Ethiopia, there were an estimated 53,560 (95% UI 52,480–55,540) new incident cases, 39,480 deaths (95% UI 32,640–46,440), and 1.42 million (95% UI 1.16–1.68) DALYs of cancer 2019. Cancer incidence, death, and DALYs counts increased by 32% (95% UI 11–55%), 29% (95% UI 12–44%), and 19% (95% UI − 2 to 44%) between 2010 to 2019, respectively, while age-standardised incidence, death, and DALYs rates increased by 5% (95% UI − 7 to 18%), 2% (95% UI − 9 to 14%), and − 2% (95% UI − 15 to 12%) respectively. In 2019, the leading incidence cases were leukemia, cervical cancer, breast cancer, colon and rectum cancer, and stomach cancer, while leukemia, breast cancer, cervical cancer, and stomach cancer were the most common killer cancers in Ethiopia. According to the findings of this study, tobacco-related cancers such as pancreatic, kidney, and lung cancer have increased in Ethiopian females over the last decade, while genitourinary cancer has increased in Ethiopian males. Another significant finding was that infection-related cancers, such as stomach cancer and Hodgkin lymphoma, have been rapidly declining over the last decade.
Similar content being viewed by others
Introduction
Cancer is a newly evolved noncommunicable global disease burden that accounts for a significant portion of global morbidity, mortality, and economic loss. Cancer is the first or second leading cause of premature death in 134 of the world's 183 countries, and it ranks third or fourth in 45 more for people under the age of 701,2,3. According to WHO, cancer caused 4.5 million (29.8 percent) of the 15.2 million premature deaths from noncommunicable diseases worldwide in 2016, while cardiovascular diseases caused 6.2 million (40.8 percent)1. Cancer caused approximately 24 million new cases, 10.0 million deaths, and 250 million DALYs globally in 20194. Because of demographics, epidemiological transitions, advanced diagnostic tools, and screening programs, these global records revealed that the burden of cancer is increasing while the burden of infectious diseases is decreasing. Because of the rapid rise in cancer cases, the United Nations (UN) Sustainable Development Goals (SDGs) include cancer burden reduction as a goal. According to 3.4, noncommunicable disease premature mortality should have been reduced by one-third through prevention and treatment, as well as promotion of mental health and well-being5. Global integrated and cooperative efforts on prevention and control of cancer lead by the WHO initiative focused breast Cancer6, Cervical cancer7, childhood cancer8, and Third United Nations high Level meeting on NCDs including cancer9. Cancer incidence is higher in developing countries, which may be due to epidemiological transitions as well as ineffective preventive and control health policies. Ethiopia has created a National Cancer Control Plan for 2016–2020, with the goal of promoting cancer prevention, early detection, improved diagnosis and treatment, palliative care, cancer surveillance, registration, and research10. The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 (GBD 2019) provides the most recent and concise evidence of cancer burden and trends in terms of incidence, mortality, and DALYs11.
Result
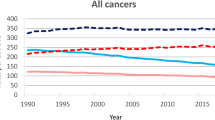
In 2019, there were an estimated 53,560 new incident cases of cancer in both sexes (95% UI 52,480–55,540), with an age-standardised incidence rate of 104.3 (95% UI 98.1–113.3) per 100,000 in Ethiopia. In 2019, cancer accounted for 39,480 deaths (95% UI 32,640–46,440) in both sexes, with an age-standardised death rate of 87.5 (71.6–105) per 100,000. In 2019, there were 1.42 million (95% UI 1.16–1.68) DALYs in both sexes in Ethiopia, with age-standardised rates of 2300 (95% UI 1900–2700) per 100,000. Year life loss (YLL) accounted for more than 98 percent of DALYs, with YLD accounting for the remainder (Table 1). Between 2010 and 2019, cancer incident cases, death counts, and DALYs counts increased by 32% (95% UI 11–55%), 29% (95% UI 12–44%), and 19% (95% UI − 2 to 44%), respectively, while incident, death, and DALY rates changed by 5% (95% UI − 7 to 18%), 2% (95% UI − 9 to 14%), and − 2% (95% UI 15–12%), respectively (Table 2). Between 2010 and 2019, the absolute number of years lived with disability (YLD) and years of life lost (YLL) increased by 36% (95% UI 12–64%) and 19% (95% UI − 24.4%), respectively. However, the age standardized rate of YLD increased by 9% (95% UI − 4 to 24%), while the age standardized rate of YLL decreased by − 2% (95% UI 15–12%). We made comparisons with neighboring countries as well as at the global level (Table 3).
Burden of cancer type
In Ethiopia, the five most common cancer incidence cases were leukemia (8310 [95% UI 4270–12440]), cervical cancer (6570 [95% UI 4470–10640]), breast cancer (5900 [95% UI 4640–7420]), colon and rectum cancer (3200 [95% UI 2400–4460]), and stomach cancer (2580 [95% UI 2100–3230]). In 2019, the highest age-standardised incidence rate was observed in breast (12.5 [95% UI 10.1–15.3]), cervical cancer (12.1 [95% UI 8.4–19.3]), leukemia (9.5 [95% UI 5.3–13.4]), CRC (7.7 [95% UI 5.8–10.7]), and prostate cancer 7.5 (95% UI 4–12.3) per 100,000, while the lowest age-standardised incidence rate was noted in malignant skin melanoma 0.5 (95% UI 0.4–0.7), mesothelioma 0.3 (95% UI 0.1–0.8), other pharynx cancer 0.3 (95% UI 0.2–0.5), and testicular cancer 0.2 (95% UI 0.19–0.4) per 100,000 (Table 1). From 2010 to 2019, the highest change of age-standardised incidence rates was recorded in testicular cancer 33% (95% UI − 12 to 104%), kidney 26% (95% UI 6–56%), ovarian 24% (95% UI − 10 to 68%), and CRC 21% (95% UI − 1 to 42%), while the lowest changes of age- standardised incident rates were observed in leukemia-11% (95% UI − 31 to 11%), Hodgkin lymphoma-14% (95% UI − 28 to 5%), and stomach cancer-16% (95% UI − 26 to − 4%) (Table 2).
Leukemia (5270 [95% UI 2910–7250]), breast cancer (4110 [95% UI 3300–4960]), cervical cancer (3870 [95% UI 2680–6290]), CRC (2850 [95% UI 2130–4000]), and stomach cancer (2640 [95% UI 2160–3370] were the four most lethal cancers in Ethiopia in 2019. In 2019, breast cancer 9.7 (95% UI 8–11.6), cervical cancer 8.2 (95% UI 5.7–13.3), leukemia 7.7 (95% UI 4.5–10.9), and CRC 7.7 (95% UI 5.5–10.4) per 100,000 had the highest age-standardised death rates in Ethiopia (Table 1). From 2010 to 2019, the highest percentage change of death counts was observed in ovarian cancer 61% (95% UI 20–117%), pancreatic cancer 59% (95% UI 32–102%), CRC 56% (95% UI 30–83%), and non-melanoma skin cancer 55% (95% UI 32–83%), while the lowest death count changes were seen in stomach cancer 12% (95% UI − 3 to 27%), Hodgkin's lymphoma 6% (95% UI − 12 to 31%), and leukemia 3% (95% UI − 23 to 38%) (Table 2).
In 2019, leukemia, breast cancer, cervical cancer, colorectal cancer, and stomach cancer had the highest age-standardised DALYs rate (Table 1). From 2010 to 2019, the highest DALYs count changes were observed in ovarian cancer 60% (95% UI 16–123%), pancreatic cancer 56% (95% UI 27–81%), colon and rectum cancer 54% (95% UI 27–81%), non-melanoma skin cancer 47% (95% UI 23–76%), while lowest change of DALYs counts documented in stomach cancer 8% (95% UI − 8 to 26%), Hodgkin's lymphoma 4% (95% UI − 16 to 32%), and leukemia-6% (95% UI − 33 to 37%). The highest age-standardised rate of DALYs change from 2010 to 2019 has been seen in pancreatic cancer 18% (95% UI − 5 to 35%), and colon and rectum cancer 15% (95% UI − 5 to 35%), while the lowest changes have been seen in Hodgkin's lymphoma-2% (95% UI − 24 to 27%), and leukemia-19% (95% UI − 33 to − 1%) (Table 2).
Burden of cancer in female
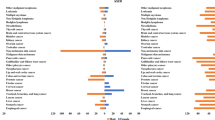
In 2019, the leading incident cases of cancer in females were cervical cancer (6570 [95% UI 4470–106400], breast cancer (5450 [95% UI 4210–6860]), leukemia (3980 [95% UI 1890–6390]), thyroid (1990 [95% UI 1360–2790]), and CRC (1440 [95% UI 1020–2120]), while the lowest incident cases were larynx cancer (60 [95% UI 50–80]), mesothelioma (60 [95% UI 20–90]) and other pharynx cancer (50 [95% UI 40–80]). Cervical cancer 24.6 (95% UI 17.1–39.2), breast cancer 23 (95% UI 18.4–28.1), leukemia 8.7 (95% UI 4.9–12.4), and CRC 7 (95% UI 5–10.2) per 100,000 Ethiopian females had the highest age-standardised incidence rate in 2019. From 2010 to 2019, the highest percentage of change of incidence cases in females was observed in pancreatic 79% (95% UI 42–128%), kidney cancer 72% (95% UI 33–115%), tracheal, bronchus, and lung cancer 69% (95% UI 36–114), ovarian cancer 67% (95% UI 16–134%), and CRC 64% (95% UI 32–104), while the lowest change was observed in stomach 15% (95% UI − 7 to 44%) and leukemia-7% (95% UI − 39 to 43%) (Fig. 1).
Stomach cancer, leukemia, larynx cancer, nasopharynx cancer, esophageal cancer, Hodgkin's lymphoma, gallbladder and biliary tract cancer, and mesothelioma have decreased age-standardised incidence rate from 2010 to 2019, ranging from − 1 to − 14%, and other malignant cancers have seen an increment in age-standardised incidence rate, ranging from 1 to 30%.
In 2019, the leading causes of cancer related mortality were cervical cancer 3870 (95% UI 2680–6290), breast cancer 3700 (95% UI 2970–4510), leukemia 2150 (95% UI 1260–3060), CRC 1270 (95% UI 900–1870), and stomach cancer 1230 (95% UI 950–2030), while the lowest causes of death were non-melanoma skin cancer 60 (95% UI 30–90), mesothelioma 50 (95% UI 20–70), and other pharynx cancer 50 (95% UI 30–70). From 2010 to 2019, the highest percentage change of death was observed in pancreatic cancer at 81% (95% UI 43–128), tracheal, bronchus, and lung cancer 70% (95% UI 39–112), kidney cancer 66% (95% UI 33–100), ovarian cancer 61% (95%), and CRC 59% (95% UI 30–93%), while the lowest change of death was seen in Hodgkin's lymphoma 19% ( 95% UI − 10 to 58%), stomach cancer 17% (95% UI − 4 to 43%), and leukemia 1% (95% UI − 28 to 46%) (Fig. 2).
Burden of cancer in males
In 2019, the leading causes of incident cases of cancer among males were leukemia (4330 [95% UI 2110–6470]), prostate cancer (2570 [95% UI 1350–4300]), CRC (1760 [95% UI 1230–2690]), tracheal, bronchial, and lung cancer (1690 [95% UI 1160–2280]). In 2019, the highest age-standardised incidence rate was observed in prostate cancer (14.5 [95% UI 7.7–23.9]), leukemia (10.3 [95% UI 5.3–15.6]), tracheal, bronchus, and lung cancer (8.6 [95% UI 5.9–11.6]), and CRC (8.4 [95% UI 5.9–12.7]) per 100,000, while the lowest age-standardised incidence rate was observed in testicular cancer 0.5 (95% UI 0.3–0.7), other pharynx cancer (0.4 [95% UI 0.3–0.7]), and mesothelioma (0.2 [95% UI 0.1–01.3]) per 100,000. Testicular cancer (67% [95% UI 2–180]), colon and rectum cancer (61% [95% UI 19–105]), prostate cancer (57% [95% UI 28–90]), and thyroid cancer (53% [95% UI 19–103]) had the highest percentage change in incident cases from 2010 to 2019, while Hodgkins lymphoma (8% [95% UI 14–36%]), stomach cancer (7% [95% UI − 14 to 32%]), and leukemia (2% [95% UI − 29 to 51%]) had the lowest change of incident cases (Fig. 3).
In 2019, the five most lethal cancers in Ethiopian males were leukemia (3120 [95% UI 1540–4540]), prostate cancer (2290 [95% UI 1210–3740]), tracheal, bronchus, and lung cancer (1820 (95% UI 1240–2480]), colon and rectum cancer (1580 [95% UI 1090–2450]), and stomach cancer (1410 [95% UI 1050–1840]). Prostate cancer had the highest age-standardised death rate in Ethiopia in 2019, with 13.8 (95% UI 7.5–22), tracheal, bronchus, and lung cancer (9.5 [95% UI 6.5–12.90]), leukemia (9 [95% UI 4.7–14]), and colon and rectum cancer (8 [95% UI 5.5–12.3]). Kidney cancer (19% [95% UI − 14 to 67%]), colon and rectum cancer (18% [95% UI − 11 to 50%]), non-melanoma skin cancer (17% [95% UI − 4 to 41%]), other pharynx cancer (15% [95% UI − 13 to 50%]), and pancreatic cancer (15% [95% UI − 14 to 59%]) had the greatest percentage change in age-standardised death rate in males between 2010 and 2019, while decreased age-standardised death rate in males was observed in breast cancer (− 3% [95% UI − 27 to 27%]), esophageal cancer (− 4% [95% UI − 26 to 25%]), leukemia (− 7% [95% UI − 28 to 23%]), larynx cancer (− 9% [95% UI − 29 to 14%)), stomach cancer (− 16% [95% UI − 33 to 2%), and Hodgkin's lymphoma (− 19% [95% UI − 35 to 0%]) (Fig. 4).
In 2019, the leading causes of highest DALYs counts and age-standardised DALYs rates in males were leukemia, prostatic cancer, CRC, and tracheal, bronchus, and lung cancer, while the lowest DALYs counts were non-melanoma skin cancer, other pharynx cancer, and mesothelioma. From 2010 to 2019, the most significant percentage change in DALYs counts was observed in colon and rectum cancer (53% [95% UI 13–97%]), non-melanoma skin cancer (49% [95% UI 19–85%], other pharynx cancer (49% [95% UI 12–97%]), pancreatic cancer (47% [95% UI 10–103%]), testicular cancer (45% [95% UI 10–91%]), and prostate cancer (15% [95% UI:15–74%]) (Fig. 3). From 2010 to 2019, a decreased age-standardised DALYs rate was identified in lip and oral cavity cancer, nasopharynx cancer, gallbladder and biliary tract cancer, brain and central nervous system cancer, breast cancer, esophageal cancer, larynx cancer, leukemia, stomach cancer, and Hodgkin lymphoma, ranging from − 1 to − 22% (Fig. 4).
Discussion
Between 2010 and 2019, the absolute number of cancer incidence cases, mortality, and DALYs increased significantly in Ethiopia. However, the age-standardised rate of cancer incidence, death, and DALYs shows erratic trends. From 2010 to 2019, we found that the trends in the age-standardised cancer incidence rate were fairly stable. Similarly, neighboring countries such as Djibouti, Eritrea, Kenya, Somalia, South Sudan, and Sudan have seen similar trends. However, there were contrast trend in high income countries and global4. Cancer is becoming more prevalent around the world, particularly in low and middle-income countries. According to WHO projections, low and middle income (LMIC) countries will bear two-thirds of the cancer burden in 20403.The main reasons for the rapid rise in cancer in low and middle income countries are population growth, aging, sociodemographic, and epidemiological transitions (LMICs)1.
The change in the incidence of cancer cases in Ethiopia, on the other hand, was primarily driven by population growth and aging. The stable age-standardised cancer incidence rate suggests that epidemiological and sociodemographic transitions play a minor role in cancer pathogenesis in Ethiopia. In 2019, behavioral risks, metabolic, occupational exposure, and air pollutions were attributed to approximately 20% (17–26%) of cancer in Ethiopia; however, changes in overall risk factors were less than 10% between 2010 and 2019.From 2010 to 2019, the age-standardised rate of cancer death in Ethiopia increased. The findings of this study stand in stark contrast to the age-standardised cancer rates in high-income countries12 and global trends4.
The increased age-standardised cancer death rate calls into question national policy in terms of progress in treatment and management, primary prevention, and secondary prevention modality implementation. Cancer is responsible for one out of every six deaths worldwide, according to a WHO report3. Many global initiatives have been launched to address the cancer burden. However, global, regional, and national efforts for cancer prevention in low and middle-income countries remain insufficient and inequitable4. In high-income countries, a strong health-care system, a large human resource capacity, and effective primary and secondary prevention methods are responsible for lower mortality12 whereas the main causes of increased cancer related mortality are a lack of workforce capacity, poor cancer care infrastructure, a lack of cancer centers for diagnosis and treatment, a lack of financial security, and a lack of universal health coverage3,13. Despite an increase in the age-standardised death rate of overall cancer, some cancer types had decreased age-standardised death rates, such as thyroid cancer, gall bladder and biliary tract cancer, cervical cancer, Nasopharynx cancer, esophageal cancer, leukemia, larynx cancer, stomach cancer, and Hodgkin lymphoma, which ranged from − 1 to − 18% over the last one decades. The main agent for lowering mortality rates will be progress in human resource capacity building, adoption of diagnostic imaging and pathological laboratories, early detection and treatment, surgical advancement, and adaptation of an effective cervical cancer screen. Most infection-related cancers, such as cervical, stomach, nasopharynx, and Hodgkin lymphoma, have steadily declined in Ethiopia over the last one decade.
Cancer trends and outcomes are disproportionately high in low and middle-income countries1,3,4. Low health care budgets14, overburdened health-resources with communicable diseases, child and maternal health, low universal health coverage15, and an increased burden of cancer all contribute to significant universal health-care disparities and inequity in low and middle-income countries. According to current evidence, primary and secondary prevention strategies could prevent more than half of all cancers16. A screening program based on guidelines has shown a reduction in cancer-related mortality in cervical, breast, prostate, and colorectal cancer16. Screening has been primarily responsible for lower rates of death and disability-adjusted life years (DALYs) for cervical cancer in Ethiopia. Currently, evidence-based modification of primary risk factors such as smoking (lung, kidney, pancreatic, and larynx cancer), H.pylori (stomach cancer), reduced alcohol consumption (liver cancer), and salted and western diets (colorectal and other GI malignancy) have aided in cancer prevention12,17. Global organizations advocate for and implement National Cancer Control Plans (NCCP) to address the cancer burden in low-income countries18. WHO leads the Global Action Plan for the Prevention and Control of NCDs 2013–2020, which aims to reduce overall mortality from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases by 25% by 2025, as well as premature mortality from noncommunicable diseases between the ages of 30 and 7019. Ethiopia has one cancer center that offers chemoradiotheraphy with few oncologists and radiotherapy wait times of 15–17 months and surgery wait times of 6–12 months. Ethiopia's cancer health policy in terms of prevention and control is deplorable. Ethiopia should have adopted WHO recommendations for cancer prevention, diagnosis, and management, as well as for strength national cancer control plan3. Low setting countries like Ethiopia should have learnt a lesson on cancer care policy development, cancer care infrastructure development, human resource capacity building, and principle of cancer prevention and control program from Rwanda13.
Limitation
Although GBD studies provide qualitative and compressive evidence for policymakers, researchers, and planners, the quality and quantity of data sources available for estimation is dependent on the quality and quantity of data sources available for estimation. Cancer mortality is primarily estimated using the cancer registry, vital registration, and, to a lesser extent, other data sources. Ethiopia has only one population-based cancer registry, which only covers 3–5 percent of the total population.
Conclusion
Overall cancer related mortality and incidence rates increased in Ethiopia. Disparities in cancer prevention, care, and control are the primary causes of these trends. Researchers, health care professionals, and policymakers must work together to develop screening guidelines and protocols, improve cancer care infrastructure, capacity building, surgical and chemoradiotheray policy, and maximize primary cancer prevention, secondary cancer prevention, early diagnosis, treatment, and rehabilitative care to reduce cancer-related mortality and disability.
Methods
We extracted data from the GBD 2019 results too (http://ghdx.healthdata.org/gbd-results-tool). The method and data sources are described in detail in GBD 2019 publications and previous GBD publications11,20,21. The Guideline for Accurate and Transparent Health Estimated Reporting (GATHER) statement was used to create GBD 2019. In summary, the 2019 Global Burden of Disease, Injury, and Risk Factors Study reported national estimates of cancer incidence, mortality, and DALYs from 1990 to 2019. Estimates for GBD 2019 were analyzed and evidence for 363 non-fatal diseases, 302 deaths, and 87 risk factors were reported in 204 countries and 21 regions11. To calculate disease incidence, mortality, and DALYs, the GBD study collects data from vital registration, verbal autopsy, cancer registry, sample vital registry, censes, demographic and health surveys, published and unpublished health data, and other sources. GBD produced sound and up-to-date evidence of trends at the global, regional, and national levels as a result of the shift in the global agenda and increased focus on noncommunicable disease and injury. GBD studies used three main standardised modeling tools to process data, model, and generate each estimation of disease by age, location, sex, and year-Cause of Death Ensemble (CODEm), DisMod-MR, and Spatiotemporal Gaussian Process Regression (ST-GPR). Cancer registry incidence data were used to calculate the mortality rate. The first model was MIR, which is based on a cancer registry and includes both mortality and incidence. MIR is a liner-step mixed-effects model that includes a logit link function, HAQ, age, and gender as covariates. Spatiotemporal Gaussian process regression was used to smooth and adjust the final model. The final model CODEm was built using observed mortality data and MIR model estimated mortality. To estimate cancer incidence, the final cancer specific mortality estimates are divided by MRI. DisMod-MR is a Bayesian meta-regression tool that uses all available data to estimate the incidence and prevalence of each disease over time. Years lived with disability (YLDs) are calculated by dividing 10-year cancer prevalence into four categories: (1) diagnosis/treatment, (2) remission, (3) metastasis/dissemination, and (4) terminal phase. Years of life lost (YLLs) are calculated by multiplying the estimated number of deaths by age by the age's standard life expectancy. The sum of YLDs and YLLs yields disability-adjusted life-years (DALYs). For age standardised rates and all rates reported per 100,000, the GBD world population is used. All estimates have 95 percent confidence intervals (UI). The GBD2019 publications contain detailed descriptions of methodology, modeling, and data sources. The GBD2019 publications contain detailed descriptions of methodology, modeling, and data sources11,20,21. We focused on the national burden of cancer in Ethiopia, estimating the burden in terms of incidence, DALYs, and mortality for 29 cancer categories.
Data availability
Data available in GBD2019 result tool (http://ghdx.healthdata.org/gbd-results-tool).
References
Wild, C. P. et al. (eds) World Cancer Report: Cancer Research for Cancer Prevention (International Agency for Research on Cancer, 2020).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
World Health Organization. WHO Report on Cancer: Setting Priorities, Investing Wisely and Providing Care for All (World Health Organization, 2020).
Global Burden of Disease Cancer Center, Kocarnik, J. M. et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol. 8, 420–444 (2021).
UN: Sustainable Developments Goals 2015–2030, accessed September 12 2021; https://sdgs.un.org/goals/goal6.
Anderson, B. O. et al. The Global Breast Cancer Initiative: a strategic collaboration to strengthen health care for non-communicable diseases. Lancet Oncol. 22(5), 578–581 (2021).
WHO. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. World Health Organization; 2020, accessed 12 September 2021; https://www.who.int/publications/i/item/9789240014107.
WHO. Global Initiative for Childhood Cancer 2020, accessed 12 September, 2021; https://www.who.int/publications/m/item/global-initiative-for-childhood-cancer.
General Assembly of the United Nations. Prevention and control of non-communicable diseases; 2018, accessed 12 September 2021; https://www.un.org/pga/72/event-latest/prevention-of-non-communicable-diseases/.
FMOH. National Cancer Control plan2016–2020. AA, Ethiopia; 2015 https://www.iccpportal.org/sites/default/files/plans/NCCP%20Ethiopia%20Final%20261015.pdf, accessed 25 April 2021.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 396(10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020). Erratum in: Lancet. 396(10262), 1562 (2020).
Bosetti, C. et al. National burden of cancer in Italy, 1990–2017: A systematic analysis for the global burden of disease study 2017. Sci. Rep. 10(1), 22099. https://doi.org/10.1038/s41598-020-79176-3 (2020).
Stulac, S. et al. Capacity building for oncology programmes in sub-Saharan Africa: The Rwanda experience. Lancet Oncol. 16(8), 979–989 (2015).
Chang, A. Y. et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. The Lancet 393(10187), 2233–2260 (2019).
GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 396(10258), 1250–1284. https://doi.org/10.1016/S0140-6736(20)30750-9 (2020).
Franceschi, S. & Wild, C. P. Meeting the global demands of epidemiologic transition: The indispensable role of cancer prevention. Mol. Oncol. 7(1), 1–13 (2013).
Bray, F., Jemal, A., Grey, N., Ferlay, J. & Forman, D. Global cancer transitions according to the Human Development Index (2008–2030): A population-based study. Lancet Oncol. 13(8), 790–801 (2012).
Romero, Y. et al. National cancer control plans: A global analysis. Lancet Oncol. 19(10), e546–e555 (2018).
WHO. WHO Global Action Plan for the Prevention and Control of NCDs 2013–2020 (World Health Organization, 2012).
Global cancer collaborator 2017. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: A systematic analysis for the global burden of disease study. JAMA Oncol. 5(12), 1749–1768. https://doi.org/10.1001/jamaoncol.2019.2996 (2019). Erratum in: JAMA Oncol. 6(3), 444 (2020). Erratum in: JAMA Oncol. 6(5), 789 (2020). Erratum in: JAMA Oncol. 7(3), 466 (2021).
James, S. L. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858 (2018).
Author information
Authors and Affiliations
Contributions
A.F. and Z.A. conceptualized of the study, A.F. and W.B. drafted the manuscript, A.F. generate all data from GBD 2019 tools, A.F., Z.A., W.B. write the result, Z.A. and A.F. write discussion, A.F. and W.B. table and Figure preparation, A.F., Z.A., W.B. finalized the final paper. All authors approved the final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awedew, A.F., Asefa, Z. & Belay, W.B. National Burden and Trend of Cancer in Ethiopia, 2010–2019: a systemic analysis for Global burden of disease study. Sci Rep 12, 12736 (2022). https://doi.org/10.1038/s41598-022-17128-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17128-9
- Springer Nature Limited
This article is cited by
-
Mortality rate and predictors of colorectal cancer patients in Ethiopia: a systematic review and meta-analysis
BMC Cancer (2024)
-
Factors influencing the uptake and utilization of cervical cancer screening services among women attending public health centers in Addis Ababa, Ethiopia: mixed methods study
BMC Women's Health (2024)
-
Precancerous lesion determinants in women attending cervical cancer screening at public health facilities in North Shoa Zone, Amhara, Ethiopia: an unmatched case-control study
BMC Women's Health (2024)
-
Knowledge, attitude, and uptake of human papillomavirus vaccine among adolescent schoolgirls in Ethiopia: a systematic review and meta-analysis
BMC Women's Health (2023)