Abstract
Risk stratification plays a key role in identifying acute myocardial infarction (AMI) patients at higher risk of mortality. However, current AMI risk scores such as the Global Registry of Acute Coronary Events (GRACE) score were derived from predominantly Caucasian populations and may not be applicable to Asian populations. We previously developed an AMI risk score from the national-level Singapore Myocardial Infarction Registry (SMIR) confined to ST-segment elevation myocardial infarction (STEMI) patients and did not include non-STEMI (NSTEMI) patients. Here, we derived a modified SMIR risk score for both STEMI and NSTEMI patients and compared its performance to the GRACE 2.0 score for predicting 1-year all-cause mortality in our multi-ethnic population. The most significant predictor of 1-year all-cause mortality in our population using the GRACE 2.0 score was cardiopulmonary resuscitation on admission (adjusted hazards ratio [HR] 6.50), while the most significant predictor using the SMIR score was age 80–89 years (adjusted HR 7.78). Although the variables used in the GRACE 2.0 score and SMIR score were not exactly the same, the c-statistics for 1-year all-cause mortality were similar between the two scores (GRACE 2.0 0.841 and SMIR 0.865). In conclusion, we have shown that in a multi-ethnic Asian AMI population undergoing PCI, the SMIR score performed as well as the GRACE 2.0 score.
Similar content being viewed by others
Introduction
Mortality and morbidity remain significant in patients with acute myocardial infarction (AMI)1. As patients vary in prognosis, it is crucial to determine which patients are expected to perform poorly so that aggressive treatment can be targeted towards that group of patients2,3. Risk stratification plays a key role in identifying the high-risk patients. Several risk scores have been developed, including the Global Registry of Acute Coronary Events (GRACE) and Thrombolysis In Myocardial infarction (TIMI) scores, but these scores were primarily derived from and validated in mainly Caucasian populations2,3,4. A previous study performed in Singapore showed that the GRACE score underestimated in-hospital mortality after AMI in a multi-ethnic Asian population1.
The most recent American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommended the use of GRACE and TIMI scores for risk stratification5,6, and there are emerging studies evaluating whether these scores apply to ethnically homogenous Asian populations7,8. The Korean Acute Myocardial Infarction Registry (KAMIR) score was created to risk stratify the Korean AMI population9. However, the performance of the scores developed for the Caucasian and Korean populations may not be applicable to the Singaporean population as the latter population is multi-ethnic2. Furthermore, it is uncertain how the previously developed SMIR risk score for ST-segment elevation myocaridal infarction (STEMI) patients compares to the guideline-recommended GRACE score in predicting 1-year all-cause mortality2. The SMIR risk score was previously used for predicting in-hospital, 30-day and 1-year cardiac mortality, as well as 1-year heart failure rehospitalization, but not for 1-year all-cause mortality. The previous SMIR risk score was also not meant to risk stratify non-ST segment elevation myocardial infarction (NSTEMI) patients.
As such, we sought to develop a new SMIR score and evaluate the performance of both the modified SMIR and GRACE 2.0 scores in predicting 1-year all-cause mortality among a population-based real-world multi-ethnic Asian STEMI and NSTEMI population with percutaneous coronary intervention (PCI).
Methods
Data collection
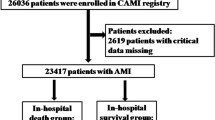
We utilized data from the Singapore Myocardial Infarction Registry (SMIR) for this study. SMIR is a national, ministry-funded registry run by the National Registry of Diseases Office (NRDO). The local ethics committee granted an exemption review for this study (SingHealth CIRB Reference No: 2016/2480) with a waiver of need for informed consent as the study utilised de-identified data. The study was performed in accordance with the Declaration of Helsinki. The statistician could access the anonymised individual-level data, while the rest of the co-authors could only access the analysed aggregated data.
SMIR obtains clinical data of all AMI patients from the public and private hosptials in Singapore10,11,12,13,14. Healthcare practitioners are mandated by law to notify the registry of the AMI cases, based on the International Classification of Diseases, 10th Revision (Australian Modification) codes I21 and I22. Patients’ were notified through medical claim listings, patient discharge summaries and laboratory results, while patients’ data were extracted from their medical records by the registry co-ordinators. These clinical data were then merged with the death data from the Registry of Births and Deaths. The Registry of Births and Deaths captures all mortality outcomes in Singapore through mandatory reporting. The registry data was subject to annual audits for accuracy and inter-rater reliability. Outlier and illogical data were flagged for review. We looked at STEMI patients who underwent primary percutaneous coronary intervention (PPCI) and NSTEMI patients who underwent PCI. AMI patients treated medically without PCI were excluded as their clinical characteristics were heterogenous.
Derivation of GRACE 2.0 score and SMIR score
The GRACE 2.0 score, derived from the GRACE registry involving 94 hospitals from 14 countries, was an improved and preferred version refined from the original GRACE score. This score was validated in the French registry of STEMI and NSTEMI (FAST-MI). A higher GRACE 2.0 score is associated with a higher mortality risk up to 3 years after the initial acute coronary syndrome event3. We chose to study the GRACE 2.0 score instead of the original GRACE score as this improved version could predict mortality beyond the initial hospitalization3.
Using SMIR data of STEMI patients with PPCI and NSTEMI patients with PCI in January 2017 to June 2018 and the same method previously used to derive the original SMIR score for STEMI patients2, we developed the modified SMIR score whereby a random sample of 70% of the cases (n = 3960) were used to derive the score and the remaining 30% (n = 1698) were used to validate the score. The components in the modified SMIR score were: age at onset of AMI, history of diabetes, Killip class on admission, cardiopulmonary resuscitation (CPR) on admission, systolic blood pressure on admission, creatinine on admission, haemoglobin on admission and left ventricular ejection fraction (LVEF) during hospitalization. Supplementary Table 1 shows the score allocation of the components and the predicted risk from the modified SMIR score. While the derivation of the modified SMIR score was largely driven by the SMIR data, it also used empirical evidence to categorize the numeric variables in the score. While using continuous functions to handle the numeric variables like the GRACE 2.0 score might yield better predictive ability, we handled the numeric variables in the modified SMIR score using a categorical approach so that the interpretation of the predicted risk contributed by each variable in the score would be easier. Unlike the previous study by Chan et al.1, we did not re-calibrate the GRACE 2.0 score to fit the local AMI population as we were keen to consider other variables that might be crucial in risk prediction.
Statistical analysis
As the modified SMIR score was validated on a randomly selected 30% of the STEMI patients with PPCI and NSTEMI patients with PCI in January 2017 to June 2018 from SMIR (n = 1698), we calculated the GRACE 2.0 score on the same group of patients and compared the performance of the two scores. We did not look at patients with PCI prior to January 2017 as SMIR only started to capture heart rate and blood pressure, variables included in the GRACE 2.0 score, from 2017 onwards. We also did not apply the scores on patients with PCI after June 2018 as the death data available at the point of analysis was until June 2019 and our outcome of interest was 1-year all-cause mortality.
The demographics and clinical chracteristics of all the AMI patients included in this study were expressed as frequency with percentages for categorical variables and median with interquartile range continuous variables. Cox regression was performed to determine the hazards ratios of the components of the GRACE 2.0 and modified SMIR scores. Patients were divided into groups based on their predicted risk of 1-year all-cause mortality from the GRACE 2.0 and modified SMIR scores. Actual mortality among the patients in each group was calculated to see if the observed mortality were close to the predicted mortality estimated from the two scores. The receiver operator chracteristic (ROC) curve of each score was plotted and the area under the curves were compared to see how well each score predicted 1-year all-cause mortality. The same analyses were replicated for each of the three main ethnic groups in Singapore to see if the performance of the two scores differed by ethnic group. Missing data were excluded from the analyses through case deletion without imputation to maintain data in its original form. All statistical analyses were performed using Stata (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). All statistical tests were 2-tailed and results were deemed to be statistically significant if p < 0.05.
Results
Baseline characteristics
Our study included 5658 patients from January 2017 to June 2018. Baseline characteristics of the included patients are described in Table 1. The median age of the patients was 61.2 years (IQR 54.0, 69.6), and they were predominantly male (81.1%). Our study consisted of a multi-ethnic Asian population, whereby the majority of patients were Chinese (62.4%). The most common co-morbidity among the patients was hypertension (61.8%), followed by hyperlipidaemia (58.4%) and then diabetes (37.6%). There were more smokers (current 38.9%, former 17.7%) than non-smokers (43.3%). Most patients were Killip Class I on admission (83.8%). The majority of patients were on evidence-based therapies for AMI during hospitalization.
Comparison of GRACE 2.0 and modified SMIR scores based on patients in SMIR
The unadjusted and adjusted hazard ratios (HR) of the individual components of the GRACE 2.0 and modified SMIR scores are shown in Table 2. For the GRACE 2.0 score, the three most significant predictors of 1-year all-cause mortality were CPR on admission (adjusted HR 6.50, 95% CI 3.82–11.06), high Killip Class on admission (adjusted HR for Class IV 4.98, 95% CI 3.14–7.91) and increasing age per 10 years (adjusted HR 1.70, 95% CI 1.45–1.99). Increasing systolic blood pressure per 20 mmHg on admission was protective (adjusted HR 0.84, 95% CI 0.75–0.95). For the modified SMIR score, the three most significant predictors of 1-year all-cause mortality were old age (adjusted HR for 70–79 years 3.53, 95% CI 1.27–9.81; adjusted HR for 80–89 years 7.78, 95% CI 2.68–22.57), CPR on admission (adjusted HR 6.34, 95% CI 3.35–12.00) and high Killip Class on admission (adjusted HR for Class IV 3.02, 95% CI 1.72–5.31). A higher LVEF during hospitalization was protective.
The predicted risk of 1-year all-cause death was < 10% for most of the patients based on the GRACE 2.0 and modified SMIR scores (Supplementary Table 2). To reduce statistical variability, we collapsed the patients into broader groups based on their predicted risk and looked at the actual observed mortality in each group. The observed mortality generally increased with the predicted mortality from both the GRACE 2.0 and modified SMIR scores, indicating positive correlation between the scores and actual outcome (Fig. 1). There was no statistically significant difference between the area under the curves for the two scores in predicting 1-year all-cause mortality (p = 0.075) (Fig. 2). The area under the ROC curve for the GRACE 2.0 score was 0.841 (95% CI 0.802–0.880) and that for the modified SMIR score was 0.865 (95% CI 0.833–0.898). Stratifying by the three main ethnic groups in Singapore, the performance of the two scores remained similar without statistically significant difference in area under the curves for predicting 1-year all-cause mortality (Supplementary Tables 3 and 4).
Observed 1-year all-cause mortality and predicted risk from the GRACE 2.0 and modified SMIR scores. The predicted mortality from the GRACE 2.0 (blue) and modified SMIR (red) scores were compared with the actual 1-year all-cause mortality observed among the AMI patients in SMIR. GRACE Global Registry of Acute Coronary Events, SMIR Singapore Myocardial Infarction Registry.
Receiver operator characteristics curves of the GRACE 2.0 and modified SMIR scores. The areas under the curve of the GRACE 2.0 (blue) and modified SMIR (red) scores were plotted and estimated to compare the performance of the two scores among the AMI patients in SMIR. AUC (95% CI) of GRACE 2.0 score: 0.841 (0.802–0.880). AUC (95% CI) of modified SMIR score: 0.865 (0.833–0.898). No statistically significant difference in AUC between the two scores: p = 0.075. AUC area under the curve, CI confidence interval, GRACE Global Registry of Acute Coronary Events, SMIR Singapore Myocardial Infarction Registry.
Discussion
In this real-world population-based study, we showed that the modified SMIR score performed similarly to the GRACE 2.0 score in a multi-ethnic Asian population in predicting 1-year all-cause mortality following STEMI and NSTEMI.
Inter-ethnic differences in the outcomes of STEMI patients have been published previously. Previous studies performed both locally15,16,17 and abroad18 have suggested inter-ethnic differences in terms of outcomes such as mortality. While there are established coronary risk factors, such as smoking, hypertension, hyperlipidaemia and diabetes mellitus, these risk factors cannot fully account for the observed inter-ethnic variations in outcomes19. Ethnic differences also existed in possible pathophysiological factors such as economic, lifestyle, anthropometric, and patient susceptibility to cerebrovascular diseases16,18. Of note, these factors are not included in contemporary risk scores such as the TIMI and GRACE 2.0 scores3,4, and are also difficult to ascertain in the acute setting. As such, there is a need to assess the relevance of contemporary risk scores in predicting outcomes among multi-ethnic or ethnic-specific population.
The GRACE registry initially consisted of 123 hospitals from 14 countries in Europe, North and South America, Australia and New Zealand20. This registry initially did not have participation from Asian countries, and consequently the derived original GRACE score was not obtained from Asian patient data2. The subsequently updated GRACE 2 registry expanded recruitment to involve 154 hospitals, this time including hospitals from Asia (including China)20. Nevertheless, the updated GRACE 2.0 score was only derived from the older registry and was validated in a French cohort3. In the Asian context, studies on the GRACE 2.0 score have been performed in ethnically homogenous populations such as in the Japanese7, Vietnamese8 and Chinese21 populations. The Japanese study was a single centre validation study of 412 STEMI patients who had undergone PPCI. This study showed a good AUC of 0.92 in predicting 360-day mortality7. The Vietnamese study was performed on 217 patients from a single centre diagnosed with unstable angina, NSTEMI and STEMI. The authors used the score to stratify their patients, but did not specifically study the predictive performance of the GRACE 2.0 score8. Fu et al. in China developed the CAMI-NSTEMI score based on 5775 patients from the China Acute Myocardial Infarction (CAMI) registry. They showed that the CAMI-NSTEMI score was superior to that of the GRACE score (AUC 0.81 vs 0.72, p < 0.01) in predicting in-hospital mortality in their Chinese population21. We found that the performance of the GRACE 2.0 and modified SMIR scores were similar, be it among all or ethnic-specific AMI patients.
In the modified SMIR score, we found that a higher LVEF was associated with a reduced 1-year all-cause mortality. LVEF is currently not one of the components of the TIMI and GRACE 2.0 scores. LVEF has previously been shown to be associated with an increased mortality in post-MI patients22. Therefore, it was worthwhile considering the use LVEF as a variable in risk prediction for AMI patients. Previously, it was difficult to perform a dedicated transthoracic echocardiogram study in the acute setting due to time constraints. However, with the advent of point-of-care echocardiography with portable handheld devices, the LVEF of the patient can be rapidly obtained by the bedside23. Future risk scores may consider the use of variables that were previously not readily available.
In addition, notably there are emerging risk stratification tools for AMI patients beyond published risk scores. Emerging approaches, such as metabolomics-based risk stratification, may have a role in future risk stratification beyond current clinically available variables24,25. Identified soluble biomarkers, such as those for myocardial fibrosis, may play a role in determining the severity of acute myocardial infarction26. Authors have also reported machine-learning based methods for risk stratification of AMI patients using big data approaches, with results that seem to outperform traditional risk models27,28. It is not improbable that in the future, risk prediction would incorporate a combination of clinical, haematological, biochemical, echocardiographic and electronic health records-based information, customized to the local context, to provide personalized risk stratification for each AMI patient. Nevertheless, until such technology becomes mature and widely available, and also in areas of practice with resource constraints29, traditional risk scores will remain relevant.
Strengths and limitations
This study used a large national-level database of AMI patients based on mandatory reporting to ensure near-complete case coverage. This also minimized selection bias. Data linkage with the national Death Registry ensured accurate and objective ascertainment of outcomes. Another strength of this study is that this scoring system is based on the contemporaneous treatment population, both in terns of secondary prevention and revascularization.
Nevertheless, we acknowledge several limitations of this study. While Singapore’s ethnically diverse population is ideal for this study, no superiority in using the modified SMIR score compared to the popular and validated GRACE tool was demonstrated. Thus, the scientific and clinical contributions of our findings seem not to be high. Nevertheless, this study fills the literature gap by studying the GRACE 2.0 score in a multi-ethnic Asian population which is currently lacking and demonstrating that GRACE 2.0 is likely to be applicable to other Asian populations that are primarily of Chinese, Malay or Indian origin. As our study focused exclusively on PCI patients alone, our findings cannot be extrapolated to patients without PCI such as the thrombolysis population. However, thrombolysis as a reperfusion strategy is seldom used, at least in Singapore. Although we found that the GRACE 2.0 and modified SMIR scores were able to correctly classify patients broadly into low (< 10%), mid (10–20% and 20–40%) and high (40–60% and > 60%) risk, we were unable to compare the observed mortality for finer subgroups at different predicted risk level due to small sample sizes. Clinicians would need to apply their own clinical judgement should they need more granular risk stratification. Further studies are needed to optimize the performance of the stated scores in predicting 1-year all-cause mortality. Moreover, the points corresponding to categories of some prognostic components, such as age at onset of acute myocardial infarction and the Killip class, are nonlinear, but these components were used for regression models. Therefore, the clinical interpretability of these components needs to be done with cautions.
Conclusion
In conclusion, we have shown that in a multi-ethnic Asian AMI population with PCI, the modified SMIR score performed similarly to the GRACE 2.0 score.
Data availability
The datasets used in this study are property of the National Registry of Diseases and were collected primarily for internal use. De-identified data can be accessed for public health research purposes after appropriate approval is obtained from the Institutional Review Board and Ministry of Health.
References
Chan, M. Y. et al. Recalibration of the Global Registry of Acute Coronary Events risk score in a multiethnic Asian population. Am. Heart J. 162, 291–299 (2011).
Bulluck, H. et al. Independent predictors of cardiac mortality and hospitalization for heart failure in a multi-ethnic Asian ST-segment elevation myocardial infarction population treated by primary percutaneous coronary intervention. Sci. Rep. 9, 1–14 (2019).
Fox, K. A. A. et al. Should patients with acute coronary disease be stratified for management according to their risk? Derivation, external validation and outcomes using the updated GRACE risk score. BMJ Open 4, e004425 (2014).
Morrow, D. A. et al. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 102, 2031–2037 (2000).
Ibanez, B. et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 39, 119–177 (2018).
O’Gara, P. T. et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 61, e78–e140 (2013).
Fujii, T. et al. Diagnostic accuracy of Global Registry of Acute Coronary Events (GRACE) risk score in ST-elevation myocardial infarction for in-hospital and 360-day mortality in Japanese patients. Circ. J. 78, 2950–2954 (2014).
Minh, T. et al. Performance of the GRACE risk score 2.0 for predicting mortality and Medication Use in Acute Coronary Syndrome patients in Ho Chi Minh city. Pharm. Sci. Asia 46, 88–97 (2019).
Lee, K. H. et al. New horizons of acute myocardial infarction: From the Korea Acute Myocardial Infarction Registry. J. Korean Med. Sci. 28, 173–180 (2013).
Ho, A. F. W. et al. Emergency medical services utilization among patients with ST-segment elevation myocardial infarction: Observations from the Singapore Myocardial Infarction Registry. Prehosp. Emerg. Care 20, 454–461 (2016).
National Registry of Diseases Office. Singapore Myocardial Infarction Registry Annual Report 2007–2013. (2014).
Sia, C. H. et al. The Lipid Paradox is present in ST-elevation but not in non-ST-elevation myocardial infarction patients: Insights from the Singapore Myocardial Infarction Registry. Sci. Rep. 10, 1–3 (2020).
Sia, C. H. et al. Association between smoking status and outcomes in myocardial infarction patients undergoing percutaneous coronary intervention. Sci. Rep. 11, 1–9 (2021).
Zheng, H. et al. Ethnic differences and trends in ST-segment elevation myocardial infarction incidence and mortality in a multi-ethnic population. Ann. Acad. Med. Singap. 48, 75–85 (2019).
Maka, K. H. et al. Ethnic differences in acute myocardial infarction in Singapore. Eur. Heart J. 24, 151–160 (2003).
Hughes, K., Lun, K. C. & Yeo, P. P. B. Cardiovascular diseases in Chinese, Malays, and Indians in Singapore. I. Differences in mortality. J. Epidemiol. Community Health 44, 24–28 (1990).
Kenneth Bk Tan, M., Aaron, M. & Wong, S. L. Mortality and neurological outcomes in out-of-hospital cardiac arrest patients with and without targeted temperature management in a multiethnic Asian population. Ann. Acad. Med. Singap. 49, 127–136 (2020).
Bhopal, R. et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: Cross sectional study. BMJ 319, 215–220 (1999).
Forouhi, N. G. & Sattar, N. CVD risk factors and ethnicity—A homogeneous relationship?. Atheroscler. Suppl. 7, 11–19 (2006).
Fox, K. A. A., Eagle, K. A., Gore, J. M., Steg, P. G. & Anderson, F. A. The global registry of acute coronary events, 1999 to 2009–GRACE. Heart 96, 1095–1101 (2010).
Fu, R. et al. CAMI-NSTEMI Score—China Acute myocardial infarction registry-derived novel tool to predict in-hospital death in non-ST segment elevation myocardial infarction patients. Circ. J. 82, 1884–1891 (2018).
Hall, T. S. et al. Relationship between left ventricular ejection fraction and mortality after myocardial infarction complicated by heart failure or left ventricular dysfunction. Int. J. Cardiol. 272, 260–266 (2018).
Arntfield, T. R. & Millington, J. S. Point of care cardiac ultrasound applications in the emergency department and intensive care unit—A review. Curr. Cardiol. Rev. 8, 98–108 (2012).
Vignoli, A. et al. NMR-based metabolomics identifies patients at high risk of death within two years after acute myocardial infarction in the AMI-Florence II cohort. BMC Med. 17, 1–9 (2019).
Vignoli, A. et al. Differential network analysis reveals metabolic determinants associated with mortality in acute myocardial infarction patients and suggests potential mechanisms underlying different clinical scores used to predict death. J. Proteome Res. 19, 949–961 (2020).
Gerber, Y. et al. Contemporary risk stratification after myocardial infarction in the community: Performance of scores and incremental value of soluble suppression of tumorigenicity-2. J. Am. Heart Assoc. 6, e005958 (2017).
Kwon, J. M. et al. Deep-learning-based risk stratification for mortality of patients with acute myocardial infarction. PLoS One 14, e0224502 (2019).
Weiss, J. C., Page, D., Natarajan, S., Peissig, P. L. & McCarty, C. Statistical relational learning to predict primary myocardial infarction from electronic health records. Proc. Innov. Appl. Artif. Intell. Conf. 2012, 2341 (2012).
Sheikh, K. & Bullock, C. Urban-rural differences in the quality of care for medicare patients with acute myocardial infarction. Arch. Intern. Med. 161, 737–743 (2001).
Acknowledgements
We would like to thank the registry coordinators of SMIR for upkeeping the quality of the registry data.
Funding
CHS was supported by the National University of Singapore Yong Loo Lin School of Medicine’s Junior Academic Faculty Scheme and the Singapore Population Health Improvement Centre (SPHERiC) Fellowship. JK was supported by the SingHealth Medical Student Talent Development Award (SMSTDA). AFWH was supported by Khoo Clinical Scholars Programme, Khoo Pilot Award (KP/2019/0034), Duke-NUS Medical School and National Medical Research Council (NMRC/CS_Seedfd/012/2018). DJH was supported by the Duke-National University of Singapore Medical School, Singapore Ministry of Health’s National Medical Research Council under its Clinician Scientist-Senior Investigator scheme (NMRC/CSA-SI/0011/2017) and Collaborative Centre Grant scheme (NMRC/CGAug16C006). This article is based upon work from COST Action EU-CARDIOPROTECTION CA16225 supported by COST (European Cooperation in Science and Technology).
Author information
Authors and Affiliations
Contributions
C.H.S., H.B., and D.J.H. designed this study; H.Z. contributed to this study by obtaining and analyzing the data of SMIR; C.H.S. and D.J.H. contributed to interpreting the data. C.H.S., H.Z., and J.K. wrote the manuscripts. A.F.H., D.F., L.F., P.Z.L., B.W.L., P.C., T.Y., H.T., T.C., M.Y.C., K.A.A.F., and J.W.C.T. contributed to this paper by providing constructive comments and insights. D.J.H. and H.B. supervised and provided critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sia, CH., Zheng, H., Ko, J. et al. Comparison of the modified Singapore myocardial infarction registry risk score with GRACE 2.0 in predicting 1-year acute myocardial infarction outcomes. Sci Rep 12, 14270 (2022). https://doi.org/10.1038/s41598-022-16523-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16523-6
- Springer Nature Limited